Abstract
We report the case of a 32-year-old man with Myotonic Dystrophy type 1 showing adenosine-induced sinus tachycardia during transesophageal electrophysiological evaluation.
Key words: sinus tachycardia, adenosine, proarrhythmic effect, myotonic dystrophy
Case report
A 32 year old man with Myotonic Dystrophy type 1 (DM1) was referred to our observation for recurrent palpitations at rest, lasting a few minutes. The medical history was negative for family sudden death, dizziness or syncope. Physical examination revealed a blood pressure of 120/70 mmHg, clear lungs and normal heart sounds. Haematological examination, except for CK values, urinary analysis and thyroid function were all normal. He had no other medical pathologies in the past, and denied intake of alcohol, tobacco or any medications.
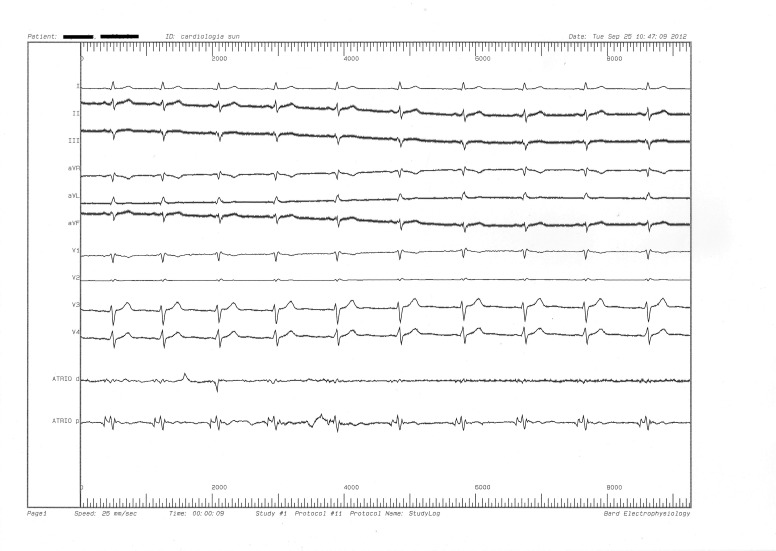
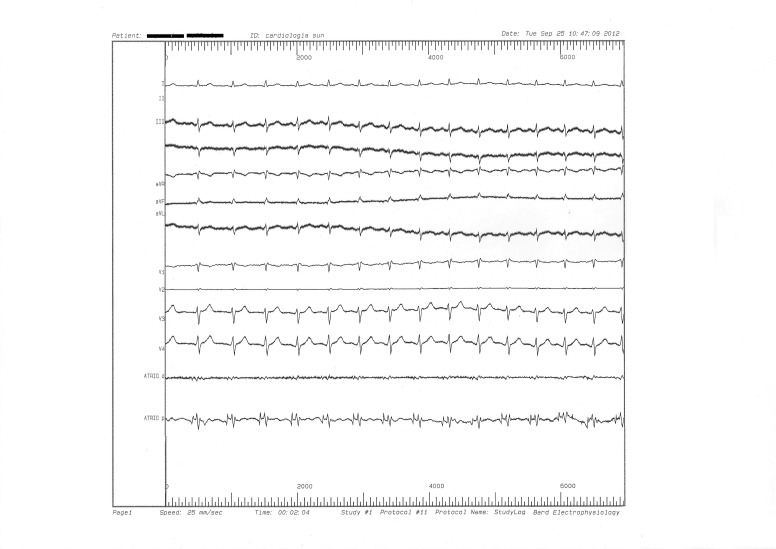
Muscle involvement was characterized by slight weakness and atrophy of facial, axial, semi-distal, and distal compartments. No abnormalities of other organs and systems including eye, endocrine system, central nervous system, gastrointestinal system, respiratory apparatus and heart were present. Electrocardiographic (ECG) examination showed a sinus rhythm of 75 bpm, normal atrioventricular conduction (PR: 160 ms), mild slurred QRS upstroke in leads V3-V4, no ST segment or T wave changes (Fig. 1). Neither chest x-ray nor colordoppler echocardiography revealed any cardiac structural or functional abnormality. 24-hours ECG Holter monitoring and treadmill stress test did not show arrhythmias. He underwent transesophageal electrophysiological evaluation: the atrioventricular node refractory period was 240 msec. During the test was not used anesthesia. The patient was conscious during the entire test and his O2 saturation, measured by a pulse oximeter, was consistently 98-99%. Programmed atrial stimulation up to triple extrastimuli did not induce supraventricular arrhythmias. Intravenous adenosine (12 mg) was performed to slow AV conduction and unmask unapparent pathways. After a single-bolus, rapidly followed by saline flush, a sinus tachycardia at a frequency of 145 beats/min, was observed, self-terminating in approximately 50 seconds, without any change in QRS morphology (Fig. 2). After the second adenosine bolus, carried out about 5 minutes later, a similar effect was observed. The patient remained conscious and asymptomatic during the entire period of tachycardia.
Figure 1.
Basal electrocardiogram.
Figure 2.
Adenosine induced synus tachycardia.
Discussion
Myotonic dystrophy type 1 (DM1) is a serious autosomal- dominant hereditary disease with an estimated incidence of 1 in 8000 births. The phenotype is characterized by myotonia and muscle weakness, but a multisystemic involvement with highly variable clinical manifestations is very frequent. Cardiac involvement, that often precedes the skeletal muscle one, occurs in 80% of DM1 patients and represents the second most common cause of death, after respiratory causes (1). Arrhythmic risk in DM1 patients may be related to the heterogeneity of ventricular repolarization (2, 3), expressing by an increase in QTc and JTc dispersion, as reported in other congenital (4-8) or acquired (9-11) heart diseases and in neuromuscular diseases (12-16). Adenosine is an endogenous nucleoside whose actions were first investigated by Drury & Szent-Gyorgyi in 1929 (17). They described a slowing of sinus rate and a reduction of conduction through the atrioventricular node in the hearts of laboratory mammals. The adenosine test seems to have a good sensitivity for unmasking accessory pathways (18), because it extends the atrioventricular node refractory period, favoring the anterograde conduction. The electrophysiologic effects of adenosine on a specific AV bypass tract, depend on the type of cell that characterize the tract: nodal type cells (with decremental conduction) or atrial myocytes. In sinu-atrial nodal cells, the activation of a potassium outward current, results in a reduced rate of phase IV depolarization, thereby slowing sinu-atrial node automaticity. In the AV node, adenosine prolongs post-repolarization refractoriness and suppresses excitability of cells in the N region of the node, resulting in an AV nodal conduction block of variable degree.
Some authors reported serious adverse events related to the adenosine infusion, including supraventricular and life threatening ventricular arrhythmias (19, 20). To date, while the association between adenosine infusion and ventricular arrhythmias is well known (21), little is known about the adenosine induced supraventricular arrhythmias. The possible mechanisms underlying pro-arrhythmic effect of adenosine are summarized in Table 1.
Table 1.
Mechanisms underlying pro-arrhythmic effect of adenosine.
| Type of arrhythmia | Underlying mechanisms |
|---|---|
| Atrial fibrillation/atrial flutter | Shortening of atrial refractoriness Sympathetic activation |
| Rapidly conducted atrial flutter/atrial fibrillation | Sympathetic activation |
| Orthodromic atrioventricular reentry tachycardia | Critical prolongation of anterograde AV nodal and retrograde activation of the atrium via an accessory pathway |
| Pre-excited atrial fibrillation/atrial flutter | Critical prolongation of anterograde AV nodal and retrograde activation of the atrium via an accessory pathway |
| Sinus tachycardia/atrial tachycardia | Reflex sympathetic discharge Direct sympathetic activation by stimulation in the carotid body chemoreceptors |
The most common pro-arrhythmic effect of adenosine is the induction of atrial fibrillation (AF) (19). This is probably owing to the shortening of atrial refractoriness, that favours the induction of reentrant arrhythmias. Because the signal transduction pathways activated by adenosine and acetylcholine, converge on the same potassium channels and produce similar electrophysiologic effects in the atrial myocardium, adenosine-induced and vagus nerve–dependent AF are mechanistically similar.
Both adenosine and vagus nerve activation cause a spatially and temporally heterogeneous shortening of atrial refractoriness (22).
A dangerous increase of the ventricular rate in patients with atrial flutter (23, 24), atrioventricular reentry tachycardia (25), narrow QRS complex tachycardia (26), and 'mild sinus tachycardia' following a brief period of bradycardia (27) have also been reported. The case here shown is the first report of sinus tachycardia induced by intravenous adenosine infusion in a DM1 patient without previous bradycardia, supporting the hypothesis of Biaggioni el al. (28) that adenosine may be responsible of a direct increase in circulating catecholamine levels and of sympathetic nerve traffic, by sympathetic stimulation in the carotid body chemoreceptors. However, in our patient, no bradycardia during the entire test was observed, as transesophageal electrophysiological evaluation was performed under continuous ECG monitoring. We are aware that the relation between adenosine infusion and sinus tachycardia is anecdotal, but we believe that all possible and unexpected pro-arrhytmic effects of antiarrhytmic drugs should be taken into account in clinical practice, particularly in patients affected by neuromuscular disorders.
References
- 1.Russo AD, Mangiola F, Della Bella P, et al. Risk of arrhythmias in myotonic dystrophy: trial design of the RAMYD study. J Cardiovasc Med (Hagerstown) 2009;10:51–58. doi: 10.2459/jcm.0b013e328319bd2c. [DOI] [PubMed] [Google Scholar]
- 2.Cudia P, Bernasconi P, Chiodelli R, et al. Risk of arrhythmia in type I myotonic dystrophy: The role of clinical and genetic variables. J Neurol Neurosurg Psych. 2009;80:790–793. doi: 10.1136/jnnp.2008.162594. [DOI] [PubMed] [Google Scholar]
- 3.Zabel M, Portnoy S, Franz MR. Electrocardiographic indexes of dispersion of ventricular repolarization: an isolated heart validation study. J Am Coll Cardiol. 1995;25:746–752. doi: 10.1016/0735-1097(94)00446-W. [DOI] [PubMed] [Google Scholar]
- 4.Buja G, Miorelli M, Turrini P, et al. Comparison of QT dispersion in hypertrophic cardiomyopathy between patients with and without ventricular arrhythmias and sudden death. Am J Cardiol. 1993;72:973–976. doi: 10.1016/0002-9149(93)91118-2. [DOI] [PubMed] [Google Scholar]
- 5.Nigro G, Russo V, Rago A, et al. Heterogeneity of ventricular repolarization in newborns with severe aortic coarctation. Pediatr Cardiol. 2012;33:302–306. doi: 10.1007/s00246-011-0132-4. [DOI] [PubMed] [Google Scholar]
- 6.Nigro G, Russo V, Rago A, et al. The effect of aortic coarctation surgical repair on QTc and JTc dispersion in severe aortic coarctation newborns: a short term follow up study. Physiol Res. 2014;63:27–33. doi: 10.33549/physiolres.932491. [DOI] [PubMed] [Google Scholar]
- 7.Russo V, Rago A, Pannone B, et al. Dispersion of repolarization and beta-thalassemia major: the prognostic role of QT and JT dispersion for identifying the high-risk patients for sudden death. Eur J Haematol. 2011;86:324–331. doi: 10.1111/j.1600-0609.2011.01579.x. [DOI] [PubMed] [Google Scholar]
- 8.Nigro G, Russo V, Rago A, et al. Regional and transmural dispersion of repolarisation in patients with Emery-Dreifuss muscular dystrophy. Kardiol Pol. 2012;70:1154–1159. [PubMed] [Google Scholar]
- 9.Nigro G, Russo V, Salvo G, et al. Increased heterogenity of ventricular repolarization in obese nonhypertensive children. Pacing Clin Electrophysiol. 2010;33:1533–1539. doi: 10.1111/j.1540-8159.2010.02889.x. [DOI] [PubMed] [Google Scholar]
- 10.Russo V, Ammendola E, Crescenzo I, et al. Effect of weight loss following bariatric surgery on myocardial dispersion of repolarization in morbidly obese patients. Obes Surg. 2007;17:857–865. doi: 10.1007/s11695-007-9160-9. [DOI] [PubMed] [Google Scholar]
- 11.Santangelo L, Ammendola E, Russo V, et al. Influence of biventricular pacing on myocardial dispersion of repolarization in dilated cardiomyopathy patients. Europace. 2006;8:502–505. doi: 10.1093/europace/eul054. [DOI] [PubMed] [Google Scholar]
- 12.Russo V, Rago A, Politano L, et al. Increased dispersion of ventricular repolarization in Emery Dreifuss muscular dystrophy patients. Med Sci Monit. 2012;18:CR643–CR647. doi: 10.12659/MSM.883541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nigro G, Russo V, Rago A, et al. Regional and transmural dispersion of repolarisation in patients with Emery-Dreifuss muscular dystrophy. Kardiol Pol. 2012;70:1154–1159. [PubMed] [Google Scholar]
- 14.Nigro G, Nigro G, Politano L, et al. Is the value of QT dispersion a valid method to foresee the risk of sudden death? A study in Becker patients. Heart. 2002;87:156–157. doi: 10.1136/heart.87.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rotundo IL, Faraso S, Leonibus E, et al. Worsening of cardiomyopathy using deflazacort in an animal model rescued by gene therapy. PLoS One. 2011;6:e24729–e24729. doi: 10.1371/journal.pone.0024729. doi: 10.1371/journal.pone.0024729. Epub 2011 Sep 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vitiello C, Faraso S, Sorrentino NC, et al. Disease rescue and increased lifespan in a model of cardiomyopathy and muscular dystrophy by combined AAV treatments. PLoS One. 2009;4:e5051–e5051. doi: 10.1371/journal.pone.0005051. doi: 10.1371/journal.pone.0005051. Epub 2009 Mar 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drury AN, Szent-Györgyi A. The physiological activity of adenine compounds with especial reference to their action upon the mammalian heart. J Physiol. 1929;68:213–237. doi: 10.1113/jphysiol.1929.sp002608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belhassen B, Fish R, Viskin S, et al. Adenosine-5'-triphosphate test for the noninvasive diagnosis of concealed accessory pathway. J Am Coll Cardiol. 2000;36:803–810. doi: 10.1016/s0735-1097(00)00813-5. [DOI] [PubMed] [Google Scholar]
- 19.Mallet ML. Proarrhythmic effects of adenosine: a review of the literature. Emerg Med J. 2004;21:408–410. doi: 10.1136/emj.2004.016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pelleg A, Pennock RS, Kutalek SP. Proarrhythmic effects of adenosine: one decade of clinical data. Am J Ther. 2002;9:141–147. doi: 10.1097/00045391-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Tan HL, Spekhorst HH, Peters RJ, et al. Adenosine induced ventricular arrhythmias in the emergency room. Pacing Clin Electrophysiol. 2001;24:450–455. doi: 10.1046/j.1460-9592.2001.00450.x. [DOI] [PubMed] [Google Scholar]
- 22.Prystowski EN, Naccarelli GV, Jackman WM, et al. Enhanced parasympathetic tone shortens atrial refractoriness in man. Am J Cardiol. 1983;51:96–100. doi: 10.1016/s0002-9149(83)80018-6. [DOI] [PubMed] [Google Scholar]
- 23.Slade AK, Garratt CJ. Proarrhythmic effect of adenosine in a patient with atrial flutter. Br Heart J. 1993;70:91–92. doi: 10.1136/hrt.70.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rankin AC, Rae AP, Houston A. Acceleration of ventricular response to atrial flutter after intravenous adenosine. Br Heart J. 1993;69:263–273. doi: 10.1136/hrt.69.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vora A, Lokhandwala Y. Adenosine-induced tachycardia: what is the mechanism? J Cardiovasc Electrophysiol. 2000;11:491–492. doi: 10.1111/j.1540-8167.2000.tb00349.x. [DOI] [PubMed] [Google Scholar]
- 26.Orebaugh SL, Handy M. Intravenous adenosine therapy accelerating rate of paroxysmal supraventricular tachycardia. Am J Emerg Med. 1992;10:326–330. doi: 10.1016/0735-6757(92)90012-m. [DOI] [PubMed] [Google Scholar]
- 27.Watt AH, Routledge PA. Transient bradycardia and subsequent sinus tachycardia produced by intravenous adenosine in healthy adult subjects. Br J Clin Pharmacol. 1986;21:533–536. doi: 10.1111/j.1365-2125.1986.tb02838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Biaggioni I, Killian TJ, Mosqueda-Garcia R, et al. Adenosine increases sympathetic nerve traffic in humans. Circulation. 1991;83:1668–1675. doi: 10.1161/01.cir.83.5.1668. [DOI] [PubMed] [Google Scholar]