Abstract
Undernutrition in infants and young children is a global health priority while overweight is an emerging issue. Small‐scale studies in low‐ and middle‐income countries have demonstrated consumption of sugary and savoury snack foods and soft drinks by young children. We assessed the proportion of children 6–23 months of age consuming sugary snack foods in 18 countries in Asia and Africa using data from selected Demographic and Health Surveys and household expenditures on soft drinks and biscuits using data from four Living Standards Measurement Studies (LSMS). Consumption of sugary snack foods increased with the child's age and household wealth, and was generally higher in urban vs. rural areas. In one‐third of countries, >20% of infants 6–8 months consumed sugary snacks. Up to 75% of Asian children and 46% of African children consumed these foods in the second year of life. The proportion of children consuming sugary snack foods was generally higher than the proportion consuming fortified infant cereals, eggs or fruit. Household per capita daily expenditures on soft drinks ranged from $0.03 to $0.11 in three countries for which LSMS data were available, and from $0.01 to $0.04 on biscuits in two LSMS. Future surveys should include quantitative data on the purchase and consumption of snack foods by infants and young children, using consistent definitions and methods for identifying and categorising snack foods across surveys. Researchers should assess associations between snack food consumption and stunting and overweight, and characterise household, maternal and child characteristics associated with snack food consumption.
Keywords: child feeding, complementary feeding, complementary foods, infant and child nutrition, low‐income countries, child public health
Introduction
Older infants and young children in high‐income countries often consume snack foods such as cookies, sweetened cereals, soft drinks, salty crisps and candy (Smithers et al. 2012). This is concerning given the rapid increase in child overweight and obesity observed in these countries and the association between consumption of energy‐dense, nutrient‐poor foods that are high in fat, sugar and salt and elevated risks of non‐communicable diseases (World Health Organization & Food and Agriculture Organization 2003). The World Health Organization recently convened a meeting ‘to scope the science around early dietary influences on non‐communicable disease, including breastfeeding and complementary feeding, and to identify key issues and future research directions’ (Branca & Caroli 2012).
Processed snack food consumption is also becoming a common occurrence in low‐ and middle‐income countries of Asia, Latin America (Woo et al. 2013) and Africa (Faber & Benadé 2007) where undernutrition is still prevalent and overweight rates in young children are on the rise (de Onis et al. 2010). In Asia and Africa, the prevalence of overweight in children under 5 years was 5% and 7%, respectively, in 2011 and is expected to reach 7% and 11% by 2025 (Black et al. 2013). Stunting prevalence in 2011 was 27% in Asia and 36% in Africa (Black et al. 2013). Infant and young child feeding practices, particularly consumption of nutrient‐poor diets and unhealthy snacks, may contribute to both stunting and overweight.
Snacks for young children are defined as foods eaten between meals – usually self‐fed, convenient and easy to prepare (WHO 2005). For the purposes of this paper, we define snack foods as unhealthy if they usually contain added sugar (referred to as ‘sugary snack foods’ including sweet biscuits, cookies, candy and soft drinks), are high in salt (referred to ‘savoury snack foods’ including chips, crisps or biscuits/crackers) are low in nutrient content or contain trans fats (WHO 2010). Biscuits are a particular concern because frequent consumption of refined carbohydrates is a risk factor for dental caries (Selwitz et al. 2007), they accustom the child to sweet or salty flavours (Adair 2012; Stein et al. 2012) and they often contain trans fats.
To assess how widespread the problem of sugary snack food consumption is in low‐ and middle‐income countries, we examined data from recent selected Demographic and Health Surveys (DHS) on intake of sugary snack foods and compared this with intake of other commercial infant foods and selected healthy foods that could be used as snacks (eggs, as they can be served hardboiled, and fruits such as papaya and mangos). The DHS however do not explicitly assess consumption of soft drinks or savoury snack foods, suggesting that this data source underestimates the magnitude of unhealthy snack consumption in these populations. There is a widespread perception that poor families in the developing world do not have sufficient income to purchase special foods for young children, either healthy or unhealthy, but this may not be the case (Banerjee & Duflo 2012). Nationally representative data on foods specifically purchased for children are largely unavailable. To better understand household purchasing patterns, we analysed data from recent Living Standards Measurement Studies (LSMS) to assess household expenditures on commercially produced snack foods including soft drinks and biscuits (sweet, savoury or plain).
Key messages
Even in low‐ and middle‐income countries, a considerable proportion of children 6–23 months of age consume sugary snack foods.
Higher rates are seen in Asia than in Africa, among 12–23‐month‐olds compared with infants, among urban compared with rural children and among children living in wealthier than poorer families.
Changing food consumption behaviours will require understanding caregivers' motivations for purchasing snack foods and beverages for their young children.
Future surveys should include quantitative data on the purchase and consumption of snack foods by infants and young children, using consistent methods for defining, categorising and measuring snack food consumption across surveys.
Future research should assess associations between young children's snack food consumption, and stunting and overweight.
Materials and methods
The DHS are intended to be nationally representative, cross‐sectional household surveys conducted in low‐ and middle‐income countries to collect information on fertility, family planning, child health, child mortality, reproductive health and nutrition (Pullum 2006). Standardised questionnaires are used to obtain information on which foods were consumed by the youngest child living with the mother in the household ages 0–23.9 months (or up to 35.9 months) on the day or night prior to the interview. The most recent version of the DHS model questionnaire collects information on 18 categories of foods and liquids: juice and juice drinks; clear broth; milk; yogurt; food made from grains (such as rice, bread, maize, porridge, noodles); yellow/orange vegetables; white potatoes, yams, cassava, manioc, and yuca; dark green leafy vegetables; vitamin A‐rich fruits; other fruits and vegetables; meat or poultry; organ meat, fish or seafood; eggs; beans/peas/nuts and lentils; cheese; and only two clearly commercial products (infant formula and fortified complementary foods) (ICF International 2011). The food category ‘sugary snack foods’, defined as biscuits, sweets, candies, chocolates, pastries or cakes, was added to the survey in 2003 and is no longer in the latest version, but many countries continued to include this question. Country researchers may add or delete questions from the standard questionnaire (e.g. some countries have added oil, fats or butter and condiments to the list of foods consumed).
Questionnaires from the DHS conducted between 2005 and 2011 in Asia and in continental sub‐Saharan Africa were reviewed to determine which surveys included a specific question on consumption of sugary snack foods. This process yielded data from surveys in 18 countries (5 in Asia and 13 in Africa). Data were available for two surveys in this time period for Cambodia and Uganda. For this analysis, the only criterion for selection was whether the dataset included questions on sugary food consumption, and all surveys in Asia and sub‐Saharan Africa that met this criterion were included. There were 20 countries (7 in Asia and 13 in Africa) with DHS surveys during this time period that did not collect information on sugary snack food intake. Permission to use country datasets was obtained from the Measure DHS web site (accessed 2013). Sugary snack food consumption was tabulated for children 6.0–23.9 months of age, as rates of consumption among children less than 6 months were low. Cross‐tabulations were conducted by child's age, household wealth and urban/rural residence. Pearson chi‐square statistics were calculated to determine whether differences in proportions of children consuming these foods were statistically significantly different from one another. The proportion of children consuming sugary snack foods was compared with the proportions consuming infant formula, fortified infant cereals, eggs and vitamin A‐rich fruits (such as mangoes and papaya).
Household wealth quintiles generated using principal components analysis and provided in the DHS datasets were used. The wealth index is based on data collected on the household's ownership of items such as a television or car, dwelling characteristics such as flooring material, type of drinking water source, toilet facilities, and other characteristics that are related to wealth status that were specific to each country (Rutstein & Johnson 2004). Sampling weights provided in the datasets were used to ensure that the results are representative at the national and regional levels. These sampling weights account for differences in urban and rural sampling (Ghana Statistical Service (GSS), Ghana Health Service (GHS) & ICF Macro 2009).
The LSMS was established by the World Bank in 1980 to explore ways of improving the type and quality of household data collected by government statistical offices in low‐ and middle‐income countries (Grosh & Glewwe 1995). Information is collected at the household level from a nationally representative sample on foods consumed, expenditures on those foods and on non‐food expenditures. Food expenditure data are collected from the best‐informed household member, the household member who shops for food. This person is asked if a particular food item was consumed by any household members in the preceding week and the amount spent on each food. Food items and terms used to express them often differ among countries.
To obtain information on expenditures for snack foods, we identified LSMS conducted between 2005 and 2011 in Asia and Africa and available on the World Bank LSMS web site (2013) as of January 2013 (World Bank 2013). There were five countries in Africa (Ethiopia, Malawi, Nigeria, Tanzania and Uganda) and two in Asia (Nepal and Timor‐Leste) that met these criteria. The questionnaires for these surveys were reviewed to determine if they contained food items for soft drinks/soda, biscuits, candies or crisps/chips. In Ethiopia, none of these products was in the questionnaire. In Tanzania, separate categories were not provided for soft drinks and biscuits and chips/crisps and candy were not included in the questionnaires. In Nepal, no separate category was given for soft drinks/soda, biscuits or candies, and crisps/chips were not included in the questionnaire. Malawi was the only country for which the questionnaire listed chips/crisps and candies as separate categories. In other countries, candies were either combined with sugar or sweets or not included at all, and no other questionnaires asked about chips/crisps. In Nigeria, biscuits were not included as a separate category and in Uganda, they were not included at all. Only Malawi and Timor‐Leste had data on biscuits but data on soft drinks were available for Malawi, Nigeria, Uganda and Timor‐Leste.
Preliminary analysis of each dataset was then conducted to assess whether any of the above products included in the questionnaire was consumed by 10% or more of households, in order to select datasets with sufficient numbers of cases to assess average expenditures. Three countries (Malawi, Nigeria and Uganda) out of four countries with data met this criterion for soft drinks while less than 10% of the households purchased soft drinks in Timor‐Leste. Two out of two countries (both Malawi and Timor‐Leste) met this criterion for biscuits. In Malawi, the only country with data on chips/crisps and candy, the percentage of households purchasing chips/crisps and candy was less than 10%. Sampling weights provided in the datasets were used in the analyses to allow the survey data to be representative at the national, regional and urban/rural levels. Analyses were conducted to compare results by urban and rural area of residence.
In Nigeria, the only country in which data were available for per capita total annual expenditure deciles, data for the period August–October 2010 were used (National Bureau of Statistics 2012). Per capita total weekly food expenditures and per capita total annual household expenditures (food and non‐food) were provided in the dataset. Household economic status was assessed by dividing households into quintiles for per capita total annual household expenditure. In Uganda, expenditures in home, out of home, in restaurants and values of gifts received were summed to determine per capita weekly spending on snacks (Uganda Bureau of Statistics 2010). Other surveys did not differentiate where food was consumed (Directorate of National Statistics, Timor‐Leste 2007; National Statistical Office, Malawi, 2012). Exchange rates into US dollars for the midpoint month of the survey months were estimated at 150 Nigerian naira, 1900 Uganda shillings and 150 Malawi kwacha (Trading Economics 2013). Pearson chi‐square statistics were used to calculate the significance of differences in proportions consuming products. Analysis of variance was used to compare mean expenditures.
In contrast to the DHS, LSMS use similar but not standardised questionnaires for data collection and there are many differences in how the fieldwork is conducted and how data are coded, entered, cleaned and compiled into usable files (Fiedler et al. 2008). The LSMS are expected to be nationally representative of households, and the datasets used for food consumption included all household types while the DHS data on food consumption were limited to households with children under age 2 years. SPSS 21 (IBM North America, New York, NY, USA) was used for data analyses.
Results
Demographic and Health Survey data
Sugary snack food consumption varied substantially across regions and countries (Fig. 1). It was less common in Tanzania and Zimbabwe (where 11–13% of children 6–23 months old consumed any sugary snack food on the previous day) and more prevalent elsewhere (range: 34–68% in Asia and 18–40% in other African countries).
Figure 1.
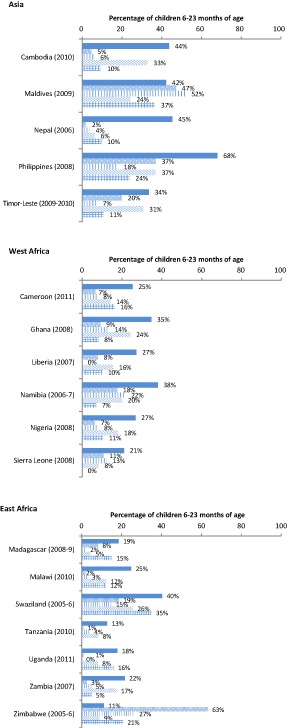
Percentage of children 6–23 months of age who consumed selected types of foods during the day or night preceding the interview.a ( ) Sugary foods, (
) Sugary foods, ( ) infant formula, (
) infant formula, ( ) fortified infant cereals, (
) fortified infant cereals, ( ) eggs, (
) eggs, ( ) vitamin A‐rich fruits. aThe percentage of children who consumed sugary foods differed from the percentage who consumed other foods at P < 0.001 except for Madagascar for fruit (P = 0.01), Maldives for infant formula (P = 0.01) and fortified infant cereal (P = 0.004), Swaziland for fruit (P = 0.03), Timor‐Lester for eggs (P = 0.04), Uganda (2010) for fruit (P = 0.32) and Zimbabwe for eggs (P = 0.05).
) vitamin A‐rich fruits. aThe percentage of children who consumed sugary foods differed from the percentage who consumed other foods at P < 0.001 except for Madagascar for fruit (P = 0.01), Maldives for infant formula (P = 0.01) and fortified infant cereal (P = 0.004), Swaziland for fruit (P = 0.03), Timor‐Lester for eggs (P = 0.04), Uganda (2010) for fruit (P = 0.32) and Zimbabwe for eggs (P = 0.05).
Two countries had two surveys during the time period included. The proportion of Ugandan children 6–23 months of age who ate sugary snack foods increased (from 8.4% to 18.0%, P < 0.001) between the two DHS (2006 and 2011) while in Cambodia, there was a slight decrease (from 50.1% to 43.7%, P = 0.002) between surveys (2005 and 2010).
The proportion of children consuming sugary snacks was higher among 12–23‐month‐old compared with 6–8‐month‐old children in all countries (Fig. 2). In one‐third of countries, >20% of all infants 6–8 months of age had consumed sugary snacks in the day or night preceding the interview. Sugary snack food consumption was especially common in Asia: among 6–8‐month‐olds, 10–44% consumed sugary foods, compared with 28–62% among 9–11‐month‐olds, and 42–75% among 12–23‐month‐olds. In Africa, among 6–8‐month‐old children, 5–29% consumed sugary foods compared with 4–36% among 9–11‐month‐olds and 11–46% among 12–23‐month‐olds.
Figure 2.
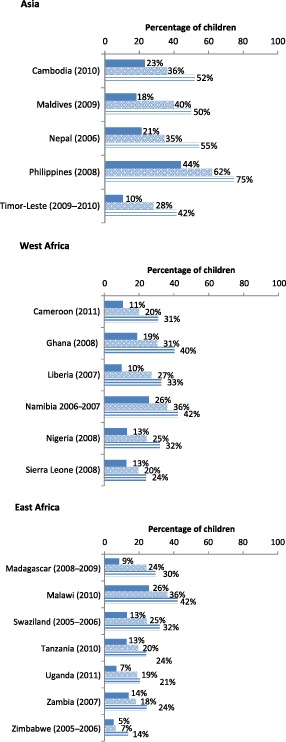
Percentage of children 6–23 months of age who consumed any sugary foods during the day or night preceding the interview, by age category (Demographic and Health Survey).a ( ) 6–8 months, (
) 6–8 months, ( ) 9–11 months, (
) 9–11 months, ( ) 12–23 months. aThe percentage of children who consumed sugary foods differed significantly between ages 6–8 months and 12–23 months at P < 0.001 except for Sierra Leone (P = 0.002).
) 12–23 months. aThe percentage of children who consumed sugary foods differed significantly between ages 6–8 months and 12–23 months at P < 0.001 except for Sierra Leone (P = 0.002).
Consumption of sugary snack foods increased with wealth quintile (Fig. 3) in all countries (P < 0.01 comparing lowest to the highest wealth quintile) except the Maldives. Consumption in the lowest wealth quintile ranged from 19.2% to 60.5% in Asia and from 4.5% to 31.5% in Africa, compared with the range in the highest quintile from 35.9% to 69.7% in Asia and from 15.9% to 52.1% in Africa. The levels of income associated with these quintiles differ across countries.
Figure 3.
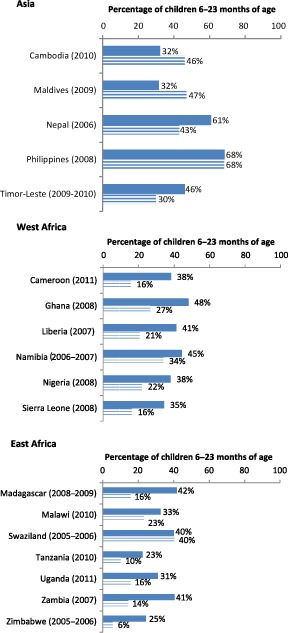
Percentage of children 6–23 months of age who consumed any sugary foods during the day or night preceding the interview, by area of residence (DHS).a ( ) Urban, (
) Urban, ( ) rural. aThe percentage of children who consumed any sugary foods differed significantly by urban vs. rural residence at P < 0.001 except for Philippines (P = 0.71) and Swaziland (P = 0.95).
) rural. aThe percentage of children who consumed any sugary foods differed significantly by urban vs. rural residence at P < 0.001 except for Philippines (P = 0.71) and Swaziland (P = 0.95).
In all countries except Philippines and Swaziland, urban children were more likely than rural children to consume sugary snacks (Fig. 4). In most of the countries, sugary foods were more likely to have been consumed than (1) foods specifically marketed for consumption by older infants and children (fortified infant cereals) and (2) eggs and vitamin A‐rich fruits (Fig. 1). Only in Zimbabwe and the Maldives was the proportion of children consuming fortified infant cereal higher than the proportion of those consuming sugary foods.
Figure 4.
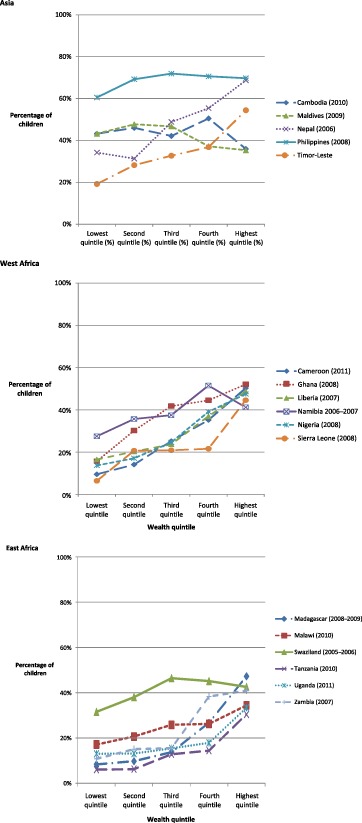
Percentage of children 6–23 months of age who consumed any sugary foods during the day or night preceding the interview, by wealth quintile (DHS).a aProportions differed significantly between the lowest and highest quintiles at P < 0.001, except for the Maldives (P = 0.08).
Living Standards Measurement Studies
Household‐level food expenditure data from the LSMS include purchases for all household members, including young children. In the LSMS in Nigeria, Uganda and Malawi, which met our criterion for inclusion of data on soft drinks, about one‐fourth of urban (23–28%) and 7–16% of rural households reported purchasing any soft drinks in the week preceding the interview (Table 1). Among those purchasing soft drinks, urban households in Nigeria spent $0.25 [standard deviation (SD) $0.32] per capita per week, compared with $0.78 (SD $1.04) in Uganda and $0.48 (SD $0.47) in Malawi. In rural households, the amount spent per capita per week was $0.22 (SD $0.25) in Nigeria, $0.57 (SD$1.00) in Uganda and $0.31 (SD $0.34) in Malawi. In Nigeria (the only country for which data were available for per capita total annual expenditure deciles), as total annual household expenditures increased, the percentage of households purchasing any soft drinks also increased (Fig. 5), with 3% of poorest households purchasing soft drinks compared with 36% of the richest households. The mean per capita weekly expenditures on soft drinks among purchasers also increased with annual total household expenditures (Fig. 6), with those in the lowest decile spending $0.04 per person per week compared with $0.36 per person per week by those in the highest decile.
Table 1.
Percentage of households purchasing any soft drinks and soft drink expenditures in the week preceding the interview in Nigeria (2010–2011), Uganda (2009–2010) and Malawi (2010–2011)*
| Survey | No. of households unweighted n | % of households reporting any expenditures on soft drinks † | % of households reporting any expenditures on soft drinks † | Mean per capita weekly expenditure on soft drinks (for those households that reported any expenditures) US $ (SD) ‡ | ||
|---|---|---|---|---|---|---|
| Urban | Rural | Urban | Rural | |||
| Nigeria (2010–2011) National Bureau of Statistics (2012) | 4 986 | 21 | 27 | 16 | 0.25 (0.32) | 0.22 (0.25) |
| Uganda (2009–2010) Uganda Bureau of Statistics (2010) | 2 975 | 14 | 28 | 9 | 0.78 (1.04) | 0.57 (1.00) |
| Malawi (2010–2011) National Statistical Office (2012) | 12 271 | 10 | 23 | 7 | 0.48 (0.47) | 0.31 (0.34) |
*In Malawi, Nigeria and Uganda, 10% or more of households had purchased soft drinks while less than 10% of the households in Timor‐Leste had done so. †Sampling weights provided in the datasets were used in these analyses. ‡Difference between urban and rural significant at P < 0.001.
Figure 5.
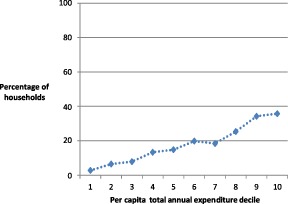
Percentage of households purchasing any soft drinks in the previous week in Nigeria (2010–2011), by annual per capita total household expenditure decile.
Figure 6.
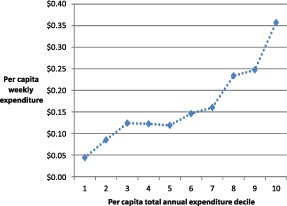
Per capita weekly expenditure ($) on soft drinks among purchasers by annual per capital total household expenditure decile in Nigeria (2010–2011).
LSMS data for Malawi and Timor‐Leste met our inclusion criterion for expenditures on biscuits. In Malawi, 22.9% of urban and 10.2% of rural households purchased any biscuits in the week prior to the interview (Table 2). Mean per capita weekly expenditures on biscuits among purchasers was $0.29 (SD $0.50) in urban households and $0.12 (SD $0.18) in rural households. In Timor‐Leste, 17.2% of urban and 12.6% of rural households purchased biscuits and they spent $0.11 (SD$0.08) and $0.10 (SD$0.08) per person per week, respectively. All differences between urban and rural households were significant at P ≤ 0.001.
Table 2.
Percentage of households purchasing any biscuits and biscuit expenditures in Malawi (2010–2011) and Timor‐Leste (2007)*
| Survey | No. of households unweighted n | % of households reporting any expenditures on biscuits † | % of households reporting any expenditures on biscuits † | Mean weekly per capita expenditure on biscuits (for those households that reported any expenditures) US $ (SD) ‡ | ||
|---|---|---|---|---|---|---|
| Urban | Rural | Urban | Rural | |||
| Malawi (2010–2011) National Statistical Office (2012) | 12 271 | 12 | 23 | 10 | 0.29 (0.50) | 0.12 (0.18) |
| Timor‐Leste (2007) Directorate of National Statistics (2007) | 4 477 | 14 | 17 | 13 | 0.11 (0.08) | 0.10 (0.08) |
*Only Malawi and Timor‐Leste had data on biscuit expenditures and both met the criterion of at least 10% of households purchasing biscuits. †Sampling weights provided in the datasets were used in these analyses. ‡The difference between urban and rural is significant at P < 0.001.
Discussion
DHS data show that sugary snack foods are consumed by a sizeable proportion of children 6–23 months of age (more than 40% in the six Asian countries and more than 20% in 9 out of 13 African countries reportedly consumed such foods on the day before the interview). In several countries, including Cambodia, Nepal, Philippines, Namibia and Swaziland, more than 20% of 6–8‐month‐old infants had consumed some sugary snack foods on the day preceding the interview. The percentage that had eaten a sugary snack food was even higher among toddlers – at least one‐third of children aged 12–23 months in the majority of countries. In nearly all cases, sugary snack food consumption was more common than intake of more nutritious foods such as eggs or vitamin A‐rich fruits, or fortified infant cereals. The assessment of intake by wealth quintiles confirms that sugary snack food consumption by older infants and young children occurs in all income groups and is not just a phenomenon among wealthier families in these countries. The rates of stunting among children under age 5 years in the countries included in this study ranged from 19% in the Maldives to 58% in Timor‐Leste, and prevalence of overweight ranged from 1% in Nepal to 11% in Nigeria (UNICEF 2013). Replacing unhealthy snacks with more nutritious alternatives could be an important means to improve infant and young child feeding and nutritional status.
These nationally representative surveys confirm findings of smaller studies reporting both frequent consumption of and a high proportion of daily energy intake from unhealthy foods by infants and young children in low‐income settings around the world. For example, Anderson et al. (2008) reported that ‘non‐nutritious snack foods’ (no definitions given) accounted for 42% of non‐breast milk energy intake among children 12–42 months of age living in poor villages in Phnom Penh. The most commonly eaten snack foods were crisps, plain or sweet biscuits and sponge cake. Lander et al. (2010) reported that ‘inappropriate snacks’ were the source of 27%, 35% and 40% of energy consumed from non‐breast milk sources among 6–8, 9–11 and 12–23‐month‐old Mongolian children; doughnuts and biscuits were most commonly consumed. In a nationally representative study conducted in Cameroon (Engle‐Stone et al. 2012), 69.4% [confidence interval (CI) 65.6–73.1%] of children 12–49 months old consumed biscuits in the last week, with an average frequency of consumption of 4.0 (CI 3.6–4.4) times per week (R. Engle‐Stone and K. Brown, unpublished observations). Soft drinks were consumed by 25.0% (CI 21.2–28.8%) of children with a frequency of consumption of 2.3 (CI 2.0–2.6) times per week (R. Engle‐Stone and K. Brown, unpublished observations). In a study in rural KwaZulu‐Natal, South Africa, where the overweight rate was 23%, 38% of infants 6–12 months of age consumed soft drinks at least once a week (Faber & Benadé 2007).
The LSMS analyses show that daily per capita expenditures averaged between $0.03 and $0.11 for soft drinks and $0.01–$0.04 for biscuits. The long shelf life and practicality of these snack foods vis‐à‐vis other foods may be a factor in food purchase decisions; relative food prices may also play a role. In a South African study, 78% of households reported cost as the most important constraint to consuming fruit on a daily basis (Faber et al. 2013).
The LSMS data include households that may not contain young children; households with children may not reflect consumption patterns of the children within them. Other research in Malawi, restricted largely to rural families of 6–23‐month‐old children, also documents that families spend resources on sugary/savoury snack foods. In a study of 352 households in Mangochi district conducted in 2011, 53% of all households with children 9 or 15 months of age had purchased store‐bought snack foods (buns/scones, biscuits, sweets, candies, chocolate and potato chips) in the preceding week (S. Vosti & M. Reimao, unpublished observations). Daily mean per capita expenditures for store‐bought snack foods (among households that purchased snacks) was US $0.03 (SD $0.04). Households that purchased soft drinks spent on average $0.01 (SD $0.02) per capita per day on these products. A similar household survey in Burkina Faso revealed that 60% of 537 households with children 9 months of age and 329 with children 15 months of age bought snacks (including chocolate/candy, cookies, fritters/cakes and soda) in the preceding week, and daily spent $0.01 on snacks (S. Vosti & Y. Xu, unpublished observations).
Unhealthy snack food consumption by young children is of concern for several reasons. Sugary and salty snack foods are usually low in nutritional value but often high in energy content, added sugar or salt (Moodie et al. 2013). Thus, they may meet the child's energy needs but not other nutrient needs. The World Health Organization recommends a maximum of 10% of energy from free sugars (World Health Organization & Food and Agriculture Organization 2003), but intake among young children in high‐income countries exceeds this level (Niinikoski & Ruottinen 2012). The evidence provided in this paper suggests that consumption of sugary foods may be a concern in low‐ and middle‐income countries, although quantitative data on percentage of energy from free sugars is lacking. High sugar intake increases the risk of high blood triglycerides in children (Niinikoski & Ruottinen 2012) and is associated with a higher incidence of dental caries (Feldens et al. 2007). Salt intake in infancy is directly associated with blood pressure in childhood (Strazzullo et al. 2012) and increased preference for salt at 36–48 months of age (Stein et al. 2012). A greater preference for salt is associated with higher blood pressure in young children in the presence of a positive family history of hypertension (Stein et al. 2012).
Another health concern is that many sweet and salty snack foods are made with partially hydrogenated oils that contain trans‐fatty acids (TFAs). Such oils are still commonly used in snack foods due to their low cost and ability to extend shelf life of products (Uauy & Dangour 2009). TFA intake is associated with inflammation (Mozaffarian et al. 2006) and an increased risk of fatal coronary heart disease, sudden cardiac death, metabolic syndrome and diabetes in adults (Uauy & Dangour 2009), and is considered a toxic component of foods consumed by children (Food and Agriculture Organization 2010). Based on TFA content in biscuits, cakes and wafers from 24 countries (Stender et al. 2006), typical serving amounts of biscuits consumed by young children in low‐income countries (Jani et al. 2009; Gibbs 2010) are likely to exceed the Food and Agriculture Organization (2010) recommended upper level of <1% of total energy from TFA for children.
The analyses presented herein are limited by the data available in nationally representative surveys. The DHS do not collect data on the quantities of foods consumed, and therefore we do not know the extent to which sugary snacks are replacing more nutritious foods. The DHS and the LSMS do not use the same categories of foods. This makes it difficult to determine the most frequent snack foods consumed or expenditures on such foods, which could be useful for informing policy makers considering actions to target specific foods in dietary guidelines and for consumer education. Having a standardised list of categories across surveys would simplify and improve the ability to track trends in the purchase and consumption of different types of foods.
Improved data on the extent of and reasons for consumption by young children of snack foods of low nutritional value can provide decision makers with the information they need to assess the importance of this issue and to take the needed action. Many commercially processed foods contain ingredients that extend their shelf life, adding to their convenience in markets and in homes, in contrast to shorter shelf lives for fresh produce and animal products. Changing snack food consumption patterns of young children will require a deeper understanding of caregivers' motivations for purchasing some types of foods and beverages.
Promoting healthier snack choices for infants and young children may require policy action to increase the availability and affordability of healthy snack food alternatives, and the establishment and enforcement of agreed‐upon marketing practices for savoury/sweet snacks. Information on the associations between snack food consumption and stunting and overweight, and the household, maternal and child characteristics associated with consumption of such foods, is also needed.
Source of funding
Funding for this analysis was provided by the Bill & Melinda Gates Foundation.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
SLH was involved in the study design, collection, analysis, interpretation of data and writing of the paper. EGP was involved in study design, interpretation of data and writing the paper. SAV contributed to the study design, provided summary data, and reviewed, edited and provided comments on drafts of the manuscript. KGD was involved in interpretation of data and writing the paper. All authors were involved in the decision to submit the paper for publication.
Acknowledgement
We would like to thank several researchers for sharing unpublished data for inclusion in this report, including Dr. Reina Engle‐Stone, Dr. Kenneth Brown, Maira Emy Reimao, Yingying Xu and the research team associated with the International Lipid‐Based Nutrient Supplements (iLiNS) project. We would also like to thank Dr. Shea Rutstein, Alissa Pries, Lara Sweet and Elizabeth Zehner for their helpful comments and review of previous versions of this paper.
References
- Adair L.S. (2012) How could complementary feeding patterns affect the susceptibility to NCD later in life? Nutrition, Metabolism, and Cardiovascular Diseases 22, 765–769. [DOI] [PubMed] [Google Scholar]
- Anderson V.P., Cornwall J., Jack S. & Gibson R.S. (2008) Intakes from non‐breast milk foods for stunted toddlers living in poor urban villages of Phnom Penh, Cambodia, are inadequate. Maternal & Child Nutrition 4, 146–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee A. & Duflo E. (2012) Poor Economics: A Radical Rethinking of the Way to Fight Global Poverty. Public Affairs: New York. [Google Scholar]
- Black R.E., Victora C.G., Walker S.P. & the Maternal and Child Nutrition Study Group (2013) Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 382, 427–451. [DOI] [PubMed] [Google Scholar]
- Branca F. & Caroli M. (2012) Complementary feeding and dietary prevention of non‐communicable diseases – a gap in the life course approach? Nutrition, Metabolism, and Cardiovascular Diseases 22, 763–764. [DOI] [PubMed] [Google Scholar]
- Directorate of National Statistics (2007) Timor‐Leste Survey of Living Standards. Direcção Nacional de Estatística, Ministério de Finanças: Dili, Timor‐Leste.
- Engle‐Stone R., Ndjebayi A.O., Nankap M. & Brown K.H. (2012) Consumption of potentially fortifiable foods by women and young children varies by ecological zone and socio‐economic status in Cameroon. The Journal of Nutrition 142, 555–565. [DOI] [PubMed] [Google Scholar]
- Faber M. & Benadé S. (2007) Breastfeeding, complementary feeding and nutritional status of 6–12 month‐old infants in rural KwaZulu‐Natal. South African Journal of Clinical Nutrition 20, 16–24. [Google Scholar]
- Faber M., Laubscher R. & Laurie S. (2013) Availability of, access to and consumption of fruits and vegetables in a peri‐urban area in KwaZulu‐Natal, South Africa. Maternal & Child Nutrition 9, 409–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldens C.A., Vítolo M.R. & Drachler Mde L. (2007) A randomized trial of the effectiveness of home visits in preventing early childhood caries. Community Dentistry and Oral Epidemiology 35, 215–223. [DOI] [PubMed] [Google Scholar]
- Fiedler J.L., Smitz M.F., Dupriez O. & Friedman J. (2008) Household income and expenditure surveys: a tool for accelerating the development of evidence‐based fortification programs. Food and Nutrition Bulletin 29, 306–319. [DOI] [PubMed] [Google Scholar]
- Food and Agriculture Organization (2010) Fats and fatty acids in human nutrition. Report on an expert consultation . FAO Food and Nutrition Paper 91, 1–166. [PubMed]
- Ghana Statistical Service (GSS) , Ghana Health Service (GHS) & ICF Macro (2009) Ghana Demographic and Health Survey 2008 . GSS, GHS, and ICF Macro: Accra, Ghana. p. 5.
- Gibbs M. (2010) Manufactured complementary foods for infant and young child feeding in Asia: micronutrient adequacy and improvement Master of Science Thesis. University of Otago. Available at: http://hdl.handle.net/10523/369 (Accessed 17 March 2014).
- Grosh M.K. & Glewwe P. (1995) A guide to living standards measurement study surveys and their data sets. Living standards measurement study (LSMS) working paper LSM 120. The World Bank: Washington, DC. Available at: http://documents.worldbank.org/curated/en/1995/09/697050/guide-living-standards-measurement-study-surveys-data-sets (Accessed 17 March 2014).
- ICF International (2011) Demographic and Health Surveys Methodology – Questionnaires: Household, Woman's, and Man's. MEASURE DHS Phase III: Calverton, Maryland, USA. Available at: http://www.measuredhs.com/publications/publication-DHSQ6-DHS-Questionnaires-and-Manuals.cfm (Accessed 17 March 2014).
- Jani R., Udipi S.A. & Ghugre P.S. (2009) Mineral content of complementary foods. Indian Journal of Pediatrics 76, 37–44. [DOI] [PubMed] [Google Scholar]
- Lander R., Enkhjargal T.S., Batjargal J., Bolormaa N., Enkhmyagmar D., Tserendolgor U. et al (2010) Poor dietary quality of complementary foods is associated with multiple micronutrient deficiencies during early childhood in Mongolia. Public Health Nutrition 13, 1304–1313. [DOI] [PubMed] [Google Scholar]
- Moodie R., Stuckler D., Monteiro C., Sheron N., Neal B., Thamarangsi T. et al (2013) Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra‐processed food and drink industries. Lancet 381, 670–679. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D., Katan M.B., Ascherio A., Stampfer M.J. & Willet W. (2006) Trans fatty acids and cardiovascular disease. New England Journal of Medicine 354, 1601–1613. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics (2012) Nigeria General Household Survey – Panel. Basic Information Document . National Bureau of Statistics, Federal Republic of Nigeria: Abuja, Nigeria.
- National Statistical Office (2012) Third integrated household survey (IHS3) 2010–2011. Basic information document . National Statistical Office: Zomba, Malawi.
- Niinikoski H. & Ruottinen S. (2012) Is carbohydrate intake in the first years of life related to future risk of NCDs? Nutrition, Metabolism, and Cardiovascular Diseases 22, 770–774. [DOI] [PubMed] [Google Scholar]
- de Onis M., Blössner M. & Borghi E. (2010) Global prevalence and trends of overweight and obesity among preschool children. American Journal of Clinical Nutrition 92, 1257–1264. [DOI] [PubMed] [Google Scholar]
- Pullum T.W. (2006) An assessment of age and date reporting in the DHS surveys, 1985–2003. Methodological Reports no. 5. Macro International Inc.: Calverton, Maryland.
- Rutstein S.O. & Johnson K. (2004) The DHS Wealth Index. DHS comparative reports No. 6. ORC Macro: Calverton, Maryland.
- Selwitz R.H., Ismail A.I. & Pitts N.B. (2007) Dental caries. Lancet 369, 51–59. [DOI] [PubMed] [Google Scholar]
- Smithers L.G., Brazionis L., Golley R.K., Mittinty M.N., Northstone K., Emmett P. et al (2012) Associations between dietary patterns at 6 and 15 months of age and sociodemographic factors. European Journal of Clinical Nutrition 66, 658–666. [DOI] [PubMed] [Google Scholar]
- Stein L.J., Cowart B.J. & Beauchamp G.K. (2012) The development of salty taste acceptance is related to dietary experience in human infants: a prospective study. American Journal of Clinical Nutrition 95, 123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stender S., Dyerberg J., Bysted A., Leth T. & Astrup A. (2006) A trans world journey. Atherosclerosis. Supplements 7, 47–52. [DOI] [PubMed] [Google Scholar]
- Strazzullo P., Campanozzi A. & Avallone S. (2012) Does salt intake in the first two years of life affect the development of cardiovascular disorders in adulthood? Nutrition, Metabolism, and Cardiovascular Diseases 22, 787–792. [DOI] [PubMed] [Google Scholar]
- Trading Economics (2013) Currency. Available at: http://www.tradingeconomics.com/currency (Accessed 24 June 2013).
- Uauy R. & Dangour A.D. (2009) Fat and fatty acid requirements and recommendations for infants of 0–2 years and children of 2–18 years. Annals of Nutrition & Metabolism 55, 76–96. [DOI] [PubMed] [Google Scholar]
- Uganda Bureau of Statistics (2010) The Uganda national panel survey (UNPS) 2009/10. Basic information document . Uganda Bureau of Statistics: Kampala, Uganda.
- UNICEF (2013) Improving child nutrition: The achievable imperative for global progress . New York.
- Woo J.G., Guerrero M.L., Ruiz‐Palacios G.M., Peng Y.M., Herbers P.M., Yao W. et al (2013) Specific infant feeding practices do not consistently explain variation in anthropometry at age 1 year in urban United States, Mexico, and China Cohorts. Journal of Nutrition 143, 166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank (2013) Living Standards Measurement Studies . Available at: http://econ.worldbank.org/WBSITE/EXTERNAL/EXTDEC/EXTRESEARCH/EXTLSMS/0,,menuPK:3359053~pagePK:64168427~piPK:64168435~theSitePK:3358997,00.html (Accessed 25 June 2013).
- World Health Organization (2005) Guiding principles for feeding non‐breastfed children 6–24 months of age . World Health Organization: Geneva.
- World Health Organization (2010) Set of recommendations on the marketing of foods and non‐alcoholic beverages to children . World Health Organization: Geneva.
- World Health Organization & Food and Agriculture Organization (2003) Diet, nutrition and the prevention of chronic diseases . Report no. 916. World Health Organization: Geneva. [PubMed]


