Abstract
Recent estimates suggest that as many as 1 in 200 adults may be trans (transgender, transsexual, or transitioned). Knowledge about dimensions of sex and gender in trans populations is crucial to development of inclusive policy, practice, and research, but limited data have been available, particularly from probability samples. The Trans PULSE community-based research project surveyed trans Ontarians (n = 433) in 2009–2010 using respondent-driven sampling. Frequencies were weighted by recruitment probability to produce estimates for the networked Ontario trans population. An estimated 30% of trans Ontarians were living their day-to-day lives in their birth gender, and 23% were living in their felt gender with no medical intervention. In all, 42% were using hormones, while 15% of male-to-female spectrum persons had undergone vaginoplasty and 0.4% of female-to-male spectrum persons had had phalloplasty. Of those living in their felt gender, 59% had begun to do so within the past four years. A minority of trans Ontarians reported a linear transition from one sex to another, yet such a trajectory is often assumed to be the norm. Accounting for this observed diversity, we recommend policy and practice changes to increase social inclusion and service access for trans persons, regardless of transition status.
Health researchers increasingly recognize the need to understand, measure, and distinguish among the impacts of gender relations, gendered identity, and sex-linked biology in order to support the development of effective policy, programmatic, and clinical interventions (Johnson, Greaves, & Repta, 2009; Krieger, 2003). Similarly, sex researchers have been called on to more carefully consider both sociocultural and biological dimensions of gender, sex, and their interplay as they relate to sexuality (Tolman & Diamond, 2001). Trans (transgender, transsexual, and transitioned) individuals represent a gender/sex-minority population that has been excluded from much population health and sexuality research (Bauer, 2012), though new evidence suggests that trans persons, broadly defined, may comprise 0.5% of the adult population (Conron, Scott, Stowell, & Landers, 2012). The field of trans health and sexuality research has burgeoned in the past two decades (Melendez, Bonem, & Sember, 2006). Yet we know little about how biological sex and social gender are understood, lived, and embodied within the broad trans population and the concrete practice and policy problems related to sex and gender diversity within trans communities.
We use the term trans to describe those who identify with a sex/gender other than that assigned at birth, and cisgender for individuals who identify with the sex/gender assigned at birth or raised in (Tate, Ledbetter, & Youssef, 2013). Trans persons can be classified as MTF (male-to-female/feminine) or FTM (female-to-male/masculine) spectra (Bauer, Travers, Scanlon, & Coleman, 2012). Trans is used to encompass a wide range of gender-variant or nonconforming identities (Kuper, Nussbaum, & Mustanski, 2012)—from transsexuals, who identify with the opposite sex to that assigned at birth, to genderqueers, who identify outside of the male/female gender binary (Bauer et al., 2012).
Genderqueer people (variously referred to as gender fluid, gender nonconforming, or nonbinary) have gained visibility in recent years (Hansbury, 2005; Kuper et al., 2012). Although such individuals may seek medical transition, they are less likely to do so (Grant et al., 2011; Kuper et al., 2012), and they may not feel that the concept of transitioning across the categories of male and female is applicable to them. Of respondents to the U.S. National Transgender Discrimination Survey (NTDS), 13% reported a gender identity other than male, female, or part time in both roles; most of these individuals wrote in “genderqueer” (Harrison, Grant, & Herman, 2011). Emerging information regarding the unique demographic and health-related profile of this group highlights the importance of their inclusion in research and of comprehensive measures of gender identity and expression (Kuper et al., 2012; Tate et al., 2013).
Although sex and gender are complex across populations, trans identities and bodies draw particular attention to the multidimensionality of these constructs. Researchers studying trans people and others who did not conform to expectations of dimorphic sex and binary gender were first to draw the conceptual distinction between biological sex and social gender. According to Money and Ehrhardt (1972), sex refers to physical characteristics, while gender encompasses the belief that one is male, female, or “ambivalent,” and one's public expression of that belief. In addition to distinguishing between sex and gender, Money's (1995) work led to a more complicated picture of sex differentiation, with five prenatal determinants: chromosomes, gonads, internal morphology, external morphology, and hormonal milieu. Without medical intervention, chromosomal, hormonal, genital, and secondary sex characteristics are usually, but not always, aligned as male or female (Fausto-Sterling, 2000). Those who are not genotypically and phenotypically male or female can be described as intersex or as having a disorder of sex development. It has been estimated that intersex infants comprise up to 2% of all live births (Blackless et al., 2000).
In the 1960s and 1970s, scholars further disaggregated gender into domains of identity (i.e., core or felt gender) and role (i.e., social expression of masculinity and femininity; Zucker & Bradley, 1995). More recently, Bauer (2012) distinguished between felt gender (the gender an individual understands himself or herself to be), lived or social gender (how an individual presents his or her gender socially), and conventional masculinity or femininity (Bauer, 2012). Transsexualism/transgenderism can be considered a third axis of gender/sex difference, encompassing trans status (whether an individual falls under the umbrella of trans, i.e., gender identity does not equate to birth sex) and trans identity (Bauer, 2012). In addition, dimensions of sex and gender are temporal. For instance, hormonal milieu changes over the life span as a consequence of endogenous and exogenous processes (Fausto-Sterling, 2000); lived gender can change with social gender transition; and some dimensions of sex (hormonal milieu, genital organs, and secondary characteristics) can change with medical transition. Trans identity can also change with transition; for example, some identify as trans only until they complete social and medical gender/sex transition, after which they identify solely as male or female (Hansbury, 2005).
Not all trans persons transition gender and/or sex. But for those who do, Bockting (2008) argued that transition is primarily a psychosocial process. Social transition can include disclosing one's gender identity to others; change in gender presentation through clothing, hairstyle, and methods of de-emphasizing sex characteristics (e.g., breast binding or padding); use of a new name and/or gender pronoun; and change of name and/or sex marker on government-issued identification (Coleman, Bockting, et al., 2011). The NTDS, the largest convenience sample of trans persons in the United States to date (n = 6,456), found that 55% lived full time in a gender different from that assigned at birth, 27% were not living full time but wanted to, and 18% did not want to live full time in a different gender (Grant et al., 2011). Trans people differ regarding the goals of social transition, with many not wanting to be perceived as cisgender (nontrans) men or women, or realizing that such a goal may not be realistic (Bockting, 2008). Nevertheless, visibility as a trans person may increase exposure to discrimination and marginalization (Lombardi, 2009), while lack of visibility has been associated with depression among MTF-spectrum trans Ontarians (Rotondi et al., 2011). In the NTDS, 21% of trans persons reported never being perceived as transgender (unless they disclosed), 56% report being perceived as trans sometimes or occasionally, and 22%, most of the time or always (Grant et al., 2011).
Medical transition, or changing one's sex characteristics, is increasingly individualized and does not require making all possible changes to sex characteristics (Coleman, Bockting, et al., 2011). Hormone therapy is the most common medical intervention for transitioning sex, and aims to reduce endogenous hormone levels to eliminate secondary sex features of one's birth sex and to replace those hormones with typical levels of the target sex (Hembree et al., 2009). However, some trans persons choose to take low doses of hormones, or to block endogenous hormones, in an effort to achieve a small amount of masculinization or feminization. In convenience samples of trans persons in the United States, the majority of participants reported hormone use (Clements-Nolle, Marx, Guzman, & Katz, 2001; Factor & Rothblum, 2008; Forshee, 2008; Grant et al., 2011; Newfield, Hart, Dibble, & Kohler, 2006; Rachlin, Green, & Lombardi, 2008; Sanchez, Sanchez, & Danoff, 2009). Fewer data are available regarding prevalence of specific surgeries. The U.S. NTDS provided such data only for participants who identified as transgender (excluding gender-nonconforming individuals). Among transgender women, 20% to 25% had undergone each of the following: breast augmentation, orchiectomy (removal of testicles), and vaginoplasty (surgical construction of a vagina; Grant et al., 2011). Among such transgender men, 43% had a mastectomy, 21% had a hysterectomy, and 6% had any genital surgery.
Attending to the multidimensionality of gender and sex, and the increasingly visible diverse subgroups of trans persons, the current study sought to describe sex, gender, and transition-related characteristics among trans Ontarians and to identify their implications for policy, practice, and research. Empirical data are scarce with respect to the diversity of gender and sex characteristics and transition trajectories among trans persons, and no research published to date has described these characteristics in a probability or population-based sample of trans persons. This limits the ability of policymakers, health practitioners, and social service providers to adopt evidence-based approaches to health care, service provision, social inclusion, and civil rights initiatives for all segments of the trans population. For clinicians who may be called upon to provide health care and counseling for trans persons, understanding of sex and gender diversity within this population may improve their ability to provide care that is both culturally competent and individualized. For sexuality researchers, the validity and applicability of research may be strengthened through consideration and measurement of gender and sex heterogeneity, across trans and nontrans populations.
To date, research with trans populations has relied almost exclusively on clinical and convenience samples, the former of which likely overrepresents those seeking to medically transition sex (Kuper et al., 2012), and the latter of which overrepresents highly marginalized subgroups of trans populations (Rosser, Oakes, Bockting, & Miner, 2007). The present study overcomes some of the limitations of previous research by providing comprehensive data regarding these characteristics across the networked trans population in Ontario, including individuals who have not transitioned, and those who are not connected to trans community organizations or venues. Specifically, we aimed to describe (1) trans Ontarians who had undertaken various degrees of social and/or medical transition, disaggregated by youth status and ethnoracial group; (2) assigned sex at birth, gender identity, and intersex status; (3) the frequency with which social, administrative, and medical transition options or treatments were taken; and (4) the timing of first awareness of trans status, social transition, and surgeries. Drawing on earlier theorizations that distinguished dimensions of sex and gender, our aim was to quantify this diversity in a trans population.
Method
Trans PULSE Project
The Trans PULSE Project is a community-based research study examining the impacts of social exclusion on the health of trans people in Ontario, Canada. The project began as a partnership between trans community members, community organizations, and academic researchers. Ethics approval was obtained from the University of Western Ontario and Wilfrid Laurier University.
Sampling
Respondent-driven sampling (RDS) was used to recruit participants (n = 433). RDS is a chain-referral sampling and analysis method developed for use with hidden populations (Heckathorn, 1997; Salganik & Heckathorn, 2004). In RDS, recruitment and statistical analyses are designed to limit biases inherent in sampling through social networks. Recruitment quotas (limits to how many new participants each participant may recruit) prevent super-recruitment bias, while recruitment networks are tracked and used along with individual network sizes to weight estimates in analysis based on the probability of recruitment.
Sampling and recruitment for Trans PULSE are described in greater detail elsewhere (Bauer et al., 2012). Beginning with 16 initial participants (“seeds”), each participant was provided with three coupons to recruit up to three additional participants; these additional participants in turn recruited the subsequent wave. A total of 22 additional seeds were added in the first six months of recruitment. Individuals who indicated they were trans, following a broad definition, were eligible to participate; they were not required to have undertaken any social or medical transition, nor to have a desire to. In addition, they needed to be 16 years of age or older and live, work, or receive health care in Ontario. Respondents completed the questionnaire in 60 to 90 minutes via a survey website or through a visually identical paper-and-pencil questionnaire (a toll-free telephone interview with language interpretation was offered but not used by any participants). Participants could maintain anonymity, but recruitment patterns were tracked using coupon numbers, and the number of eligible persons known (degree) was assessed for each participant to use RDS analytic methods. Participants were given a $20 gift card as an honorarium, with the option of donating the honorarium to a trans-related charity. Secondary incentives ($5 gift cards) were added for recruitment of peers in the final two months of the study, with no apparent change in the rate of recruitment.
Measures
As validated measures for gender, sex, and transition-related characteristics of trans persons were not available, these measures were developed by academic and community members of the research team, and pretested for clarity and content validity with the study's Community Engagement Team, a diverse group of 16 trans Ontarians. Measures were revised following pretesting to ensure completeness of response options, clarity of language, and relevance to participants.
Demographics
All measures were based on self-report. Demographic variables included gender spectrum, ethnoracial group, and youth status (age 16 to 24). Participants were asked to indicate their assigned sex at birth, and this information was used to categorize gender spectrum as MTF or FTM. Respondents did not necessarily identify as female or male, but could identify as genderqueer, bigender, or other fluid identities. Ethnoracial group was classified based on responses to multiple check-all-that-apply items. Those who indicated being First Nations, Inuit, or Métis (Canada's Aboriginal groups) or were of other Indigenous ethnicity were coded as Aboriginal, while those who reported only white background(s) were coded as non-Aboriginal whites. Participants were coded as non-Aboriginal racialized if they reported only non-white racialized ethnicities (racialized is a term used to describe people of color which emphasizes the social production of racial difference). Those who reported both white and racialized ethnicities were categorized on a case-by-case basis, based on responses to these items and whether they indicated being perceived as persons of color.
Gender identity
Participants selected gender identity labels from a prespecified list but could also select “Other” and write in their own terms. Those who endorsed only nonbinary gender identities (such as cross-dresser, bigender, genderqueer, or two-spirit) were coded as having a “fluid” gender identity. Participants were asked at what age they first realized that their gender and body were not aligned (i.e., that they were trans); this variable was recoded into categories based on years since this realization.
Social transition and gender characteristics
Social gender variables included the frequency of daily living in one's felt gender, number of years living in one's felt gender, use of a new name or pronoun in daily life, completion of a legal name change, change of sex markers on government-issued identification, frequency perceived as trans by others, and desire to be perceived as trans by others. Participants who were living in their felt gender full or part time were asked how old they were when they first began living in their felt gender (i.e., began social transition); this variable was recoded to reflect the number of years since social transition. Participants were provided with a list of all possible forms of government-issued identification (ID) and asked whether they had each type of ID and, if so, whether it included a male or female sex designation. Those who indicated a sex designation opposite to their assigned sex at birth were coded as having changed their sex on any ID, or as having changed their sex on all ID, if so indicated. Frequency perceived as trans and wanting to be perceived as trans were measured with items about the frequency with which people perceived the respondent as trans without being told, and about whether or not respondents wanted to be perceived as trans without disclosing.
Medical transition and sex characteristics
Medical transition and sex characteristics included having been diagnosed with a medically recognized intersex condition, self-described medical transition status (with respect to hormones and/or surgery), history of hormone use (whether or not prescribed them by a physician), and having undergone each specified transition-related surgery or medical procedure from a list provided (and, if so, the year in which the procedure took place).
Social and medical transition status
Social gender and medical sex transition status (transition status) was classified as “no transition,” where participants were not using hormones and had not had surgery, and were either not living in their felt gender or were living part time but not using a new name or pronoun. Transition status was classified as “social only” if participants had not used hormones or had any surgical treatments but were living in their felt gender full time, or part time while using a new name and/or pronoun. Where participants indicated being in the process of medical transition and living in their felt gender full or part time, transition status was classified as “some social and some medical.” Finally, those who self-reported a complete medical transition and who were living in their felt gender full time were classified as “complete” with respect to transition. Where self-reported medical transition status was not aligned with reported hormone use or surgical history (e.g., someone who answered “planning but not begun” but had had multiple surgeries), overall transition status was recoded to ensure accuracy. Five MTF-spectrum participants who reported no social transition but who were currently using hormones consistent with medical transition were excluded from analyses based on transition status because this group represented a separate transition category that was too small to analyze.
Statistical Analysis
Proportions and associated 95% confidence intervals were estimated for the proportion of all trans Ontarians belonging to each transition status group, and for all trans Ontarians stratified by youth status, and by ethnoracial group. All subsequent analyses were stratified by gender spectrum. Sex, gender, and transition status characteristics were estimated for all MTF- and FTM-spectrum Ontarians, and for MTFs and FTMs within each transition status group.
Proportions and 95% confidence intervals were estimated using RDS I methods with the Respondent-Driven Sampling Analysis Tool version 6.0.1 (Volz, Wejnert, Degani, & Heckathorn, 2010). All estimates were weighted based on probability of recruitment through adjustment for network size (number of eligible participants known) and differential recruitment across groups (Heckathorn, 1997, 2002), and thus are estimates for the networked (i.e., knowing at least one other trans person) Ontario trans population 16 years of age and older. Confidence intervals were generated using a modified bootstrapping procedure with 10,000 resamples through recruitment chains, with an enhanced data smoothing algorithm (Salganik, 2006). In RDS I analyses, data from seeds were included in a limited way, contributing to transition probabilities used to estimate confidence intervals, for example, but not to average network sizes (as they were recruited by the research team rather than a peer). Accounting for the networked data structure, statistical significance of differences between proportions was assessed by constructing confidence intervals around the difference in proportions using the method of variance estimates recovery (MOVER; Zou & Donner, 2008). This method was also used to calculate 95% confidence intervals for prevalence ratios, which are reported in the text.
Results
In total, 433 trans Ontarians participated in the study, including 205 male-to-female spectrum trans persons (MTFs) and 227 female-to-male spectrum trans persons (FTMs). Participants ranged in age from 16 to 77 years old. Two participants identified solely as intersex and did not indicate masculine or feminine gender identity; these participants were classified as MTF spectrum based on their assigned sex at birth. A network diagram showing the recruitment structure of the sample is presented in Figure 1, coded for gender spectrum and social and medical transition status. A total of 10 waves of recruitment were obtained, with participants having a median network size of eight. Under the extremely conservative assumption that all seeds belonged to a particular transition status group (which they did not), between two and five waves would have been required to reach equilibrium for different variables, the point at which the sample characteristics are stable and independent of the seeds. This indicates that equilibrium was reached in the less-extreme case of this analysis.
Figure 1.
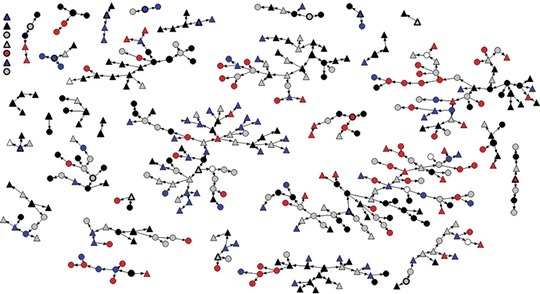
Network structure for sample of 433 trans (transgender, transsexual, transitioned) persons in Ontario, Canada; triangle = female-to-male (FTM) spectrum; circle = male-to-female (MTF) spectrum; red = no transition; blue = social transition only; gray = some social and some medical transition; black = complete social and medical transition.
Social and Medical Transition Status
Information regarding the demographic characteristics of trans Ontarians has been published elsewhere (Bauer et al., 2012). Proportions of trans Ontarians who fell into each social and medical transition status group, disaggregated by youth status, gender spectrum, and ethnoracial group, are presented in Table 1. Overall, 30% (95% CI: 20–35) of trans Ontarians had not undertaken any gender/sex transition, and 23% (95% CI: 18–33) were living in their felt gender with no medical intervention. FTMs were 3.7 times (95% CI: 1.9–9.1) as likely as MTFs to have socially transitioned only, whereas MTFs were 1.7 times (95% CI: 1.1–3.1) as likely to have undergone some social and some medical transition. As compared to adults age 25 and older, youth (16–24 years) were 2.1 times (95% CI: 1.1–3.9) as likely to have socially transitioned only. There were no statistically significant differences in the proportions who indicated they had completed transition. There were no significant differences between ethnoracial groups with respect to social and medical transition status.
Table 1. Social Gender and Medical Sex Transition Status Among Trans a Ontarians.
| Transition Status | Gender Spectrum |
Age |
Ethnoracial Group |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 433) |
MTFs
b
(n = 205) |
FTMs
c
(n = 227) |
Adults (25+) (n = 309) |
Youth (16–24) (n = 123) |
Aboriginal (n = 35) |
Racialized
d
(n = 62) |
White
d
(n = 333) |
|||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| No transition | 30 | (20, 35) | 37 | (23, 46) | 23 | (12, 32) | 33 | (21, 40) | 24 | (12, 36) | 23 | (8, 48) | 27 | (6, 34) | 31 | (21, 38) |
| Social only | 23 | (18, 33) | 10 | (4, 18)† | 35 | (27, 50)† | 18 | (10, 28)* | 37 | (25, 50)* | 11 | (3, 23) | 26 | (12, 52) | 22 | (16, 32) |
| Some social, some medical | 24 | (18, 31) | 31 | (22, 43)† | 18 | (11, 23)† | 24 | (18, 32) | 24 | (12, 35) | 54 | (20, 74) | 17 | (7, 32) | 24 | (18, 32) |
| Complete e | 23 | (17, 31) | 22 | (14, 33) | 24 | (14, 34) | 26 | (18, 36) | 15 | (8, 28) | 13 | (3, 29) | 30 | (12, 53) | 23 | (16, 31) |
aTransgender, transsexual, transitioned.
bMale-to-female or transfeminine spectrum.
cFemale-to-male or transmasculine spectrum.
dNon-Aboriginal.
eComplete transition was self-defined and could include varying combinations of hormones and/or surgeries.
†Indicates statistically significant difference in proportions between MTFs and FTMs at the a = .05 level.
*Indicates statistically significant difference in proportions between youths and adults at the a = .05 level.
Gender Identity
Gender identity characteristics are described in Table 2. While most on the MTF spectrum identified as female or feminine, and most on the FTM spectrum as male or masculine, a sizable proportion (an estimated 27% of MTFs and 14% of FTMs, respectively) were fluid, meaning that they endorsed only nonbinary gender identities (e.g., genderqueer, bigender, two-spirit). In addition, a substantial minority of MTFs identified as cross-dressers (19%; 95% CI: 9–31), including 43% (95% CI: 21–66) of those who had not transitioned. Another 7% of trans Ontarians (95% CI: 4–10) indicated identifying with a gender other than those listed. Gender identities written in included androgyne, butch, human, post gender, work in progress, genderless and gender-creative. An estimated 63% of MTFs and 38% of FTMs had been aware that they were trans or gender incongruent for 20 years or more. The majority of both persons on both gender spectra first realized that they were trans before age 10.
Table 2. Gender Identity Characteristics of Trans a Ontarians.
| Gender Characteristic | Male-to-Female Spectrum (MTF) |
Female-to-Male Spectrum (FTM) |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All MTFs (n = 205) |
No Transition (n = 52) |
Social Only (n = 22) |
Some Social and Some Medical (n = 64) |
Complete Social and Medical (n = 62) |
All FTMs (n = 227) |
No Transition (n = 27) |
Social Only (n = 59) |
Some Social and Some Medical (n = 55) |
Complete Social and Medical (n = 84) |
|||||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Gender identity | ||||||||||||||||||||
| Female or feminine | 73 | (62, 84) | 37 | (19, 58) | 67 | (45, 90) | 94 | (86, 100) | 100 | (100, 100) | 2 | (0, 6) | 9 | (0, 22) | 0 | (0, 0) | 0 | (0, 0) | 0 | (0, 0) |
| Male or masculine | 0 | (0, 0) | — | — | — | — | — | — | — | — | 84 | (73, 92) | 69 | (59, 93) | 71 | (44, 91) | 98 | (95, 100) | 99 | (97, 100) |
| Fluid | 27 | (16, 38) | 63 | (42, 81) | 33 | (10, 55) | 6 | (0, 14) | 0 | (0, 0) | 14 | (7, 25) | 22 | (5, 34) | 29 | (9, 56) | 1 | (0, 5) | 1 | (0, 3) |
| Gender identity label* | ||||||||||||||||||||
| Girl or woman | 41 | (30, 52)† | 7 | (3, 12) | 43 | (10, 75) | 59 | (45, 81) | 73 | (56, 90) | 7 | (1, 13)† | 18 | (0, 21) | 8 | (0, 21) | 0 | (0, 0) | 0 | (0, 0) |
| Boy or man | 8 | (2, 14)† | 20 | (3, 34) | 13 | (0, 31) | 2 | (0, 7) | 1 | (—, —) | 64 | (54, 74)† | 56 | (30, 80) | 58 | (39, 80) | 75 | (56, 90) | 67 | (47, 82) |
| MTF or FTM | 45 | (36, 56)† | 34 | (16, 53) | 32 | (12, 63) | 58 | (35, 71) | 51 | (32, 76) | 58 | (47, 68)† | 61 | (32, 89) | 47 | (30, 67) | 62 | (40, 79) | 64 | (41, 81) |
| Trans girl/woman | 37 | (27, 48)† | 18 | (5, 32) | 30 | (9, 58) | 52 | (29, 68) | 35 | (20, 57) | 0 | (0, 0)† | — | — | — | — | — | — | — | — |
| Trans boy/man | 0 | (0, 0)† | — | — | — | — | — | — | — | — | 52 | (39, 61)† | 28 | (5, 54) | 48 | (25, 66) | 73 | (51, 86) | 55 | (32, 73) |
| T girl | 16 | (8, 24)† | 13 | (2, 25) | 24 | (5, 50) | 28 | (11, 43) | 10 | (2, 23) | 0 | (0, 0)† | — | — | — | — | — | — | — | — |
| Shemale | 8 | (2, 14)† | 10 | (0, 19) | 0 | (0, 0) | 12 | (2, 27) | 4 | (0, 12) | 0 | (0, 0)† | — | — | — | — | — | — | — | — |
| Feel like a girl sometimes | 12 | (6, 20) | 22 | (7, 37) | 29 | (2, 52) | 11 | (0, 20) | 1 | (0, 2) | 7 | (3, 14) | 14 | (0, 16) | 5 | (1, 10) | 2 | (0, 4) | 3 | (—, —) |
| Feel like a boy sometimes | 2 | (1, 5) | — | — | — | — | — | — | — | — | 14 | (8, 24) | 18 | (1, 29) | 16 | (5, 32) | 5 | (0, 16) | 2 | (0, 9) |
| Cross-dresser | 19 | (9, 31)† | 43 | (21, 66) | 16 | (2, 33) | 5 | (0, 18) | 0 | (0,0) | 5 | (1, 9)† | — | — | — | — | — | — | — | — |
| Genderqueer | 10 | (5, 16)† | 9 | (2, 20) | 28 | (7, 56) | 11 | (1, 23) | 9 | (0, 22) | 32 | (22, 43)† | 47 | (23, 72) | 41 | (22, 63) | 19 | (6, 35) | 8 | (3, 16) |
| Two spirit | 11 | (4, 19) | 18 | (2, 34) | 11 | (2, 29) | 11 | (1, 22) | 1 | (0, 4) | 5 | (2, 10) | — | — | — | — | — | — | — | — |
| Bigender | 7 | (2, 13) | 16 | (3, 30) | 22 | (1, 50) | 1 | (0, 2) | 0 | (0, 0) | 3 | (1, 5) | — | — | — | — | — | — | — | — |
| Years since first aware of trans status | ||||||||||||||||||||
| 9 years ago or less | 16 | (8, 27) | 20 | (6, 42) | 15 | (0, 46) | 16 | (3, 31) | 4 | (0, 12) | 24 | (16, 36) | 28 | (8, 51) | 35 | (13, 56) | 19 | (3, 26) | 11 | (3, 23) |
| 10–19 years ago | 21 | (12, 32)† | 17 | (4, 38) | 5 | (0, 28) | 27 | (12, 48) | 10 | (3, 27) | 38 | (26, 49)† | 26 | (5, 46) | 38 | (16, 58) | 32 | (18, 58) | 35 | (17, 57) |
| 20–29 years ago | 19 | (13, 29) | 4 | (0, 11) | 31 | (12, 69) | 20 | (6, 42) | 30 | (11, 49) | 15 | (8, 23) | 21 | (13, 51) | 11 | (1, 30) | 28 | (8, 48) | 22 | (13, 44) |
| 30 + years ago | 44 | (29, 55)† | 59 | (32, 77) | 49 | (5, 75) | 38 | (17, 53) | 56 | (31, 75) | 23 | (13, 34)† | 25 | (0, 32) | 15 | (4, 39) | 21 | (7, 43) | 31 | (7, 47) |
| Age first aware | ||||||||||||||||||||
| 9 years or under | 60 | (49, 70) | 36 | (15, 56) | 52 | (21, 85) | 58 | (41, 76) | 88 | (76, 95) | 57 | (44, 65) | 55 | (23, 79) | 40 | (20, 61) | 61 | (43, 79) | 74 | (59, 85) |
| 10–14 years | 23 | (14, 32) | 33 | (13, 55) | 11 | (2, 33) | 34 | (17, 51) | 7 | (2, 15) | 21 | (14, 31) | 17 | (2, 39) | 27 | (11, 50) | 23 | (12, 48) | 11 | (5, 21) |
| 15–19 years | 10 | (4, 18) | 21 | (3, 36) | 5 | (0, 18) | 7 | (0, 14) | 3 | (0, 10) | 15 | (9, 25) | 19 | (4, 50) | 28 | (9, 49) | 9 | (0, 16) | 8 | (2, 18) |
| 20 years or older | 7 | (3, 14) | 10 | (2, 35) | 33 | (0, 63) | 2 | (0, 5) | 2 | (0, 8) | 8 | (3, 13) | 9 | (0, 23) | 5 | (0, 12) | 7 | (0, 8) | 7 | (0, 15) |
Note. Proportions may not add up to 100% due to rounding and RDS estimation procedures for stratum-specific estimates. (—, —) = confidence interval could not be calculated.
*Multiple response options were allowed; proportions will not add up to 100%.
aTransgender, transsexual, transitioned.
†Indicates statistically significant difference in proportions between MTFs and FTMs at the a = .05 level.
Social Transition and Gender Characteristics
Table 3 includes social transition and gender characteristics. We estimated that approximately half of trans Ontarians were living full time in their felt gender. MTF-spectrum persons were 1.9 (95% CI: 1.0–4.6) times as likely to report not living in their felt gender, even part time, as compared to FTM-spectrum persons. While we did not collect information about plans to socially transition, planning to medically transition likely implies plans to socially transition as well. Therefore, we note that a majority of nontransitioned FTMs, and a minority of nontransitioned MTFs, were planning to medically transition (75%, 95% CI: 58–95 versus 27%, 95% CI: 11–47). The majority of networked trans Ontarians who were living in their felt gender had begun to do so within the past four years (59%, 95% CI: 50–69). However, approximately 10% had socially transitioned 15 years ago or more, and the number of years since social transition reported by participants ranged from 0 to 56 years.
Table 3. Social Transition and Gender Characteristics of Trans a Ontarians.
| Male-to-Female Spectrum (MTF) |
Female-to-Male Spectrum (FTM) |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All MTFs (n = 205) |
No Transition (n = 52) |
Social Only (n = 22) |
Some Social and Some Medical (n = 64) |
Complete Social and Medical (n = 62) |
All FTMs (n = 227) |
No Transition (n = 27) |
Social Only (n = 59) |
Some Social and Some Medical (n = 55) |
Complete Social and Medical (n = 84) |
|||||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Living in felt gender | ||||||||||||||||||||
| Full time | 46 | (37, 59) | — | — | 52 | (29, 86) | 64 | (51, 87) | 100 | (—, —) | 49 | (38, 61) | — | — | 42 | (27, 64) | 76 | (56, 91) | 100 | (—, —) |
| Part time | 24 | (13, 30) | 17 | (5, 28) | 48 | (14, 71) | 36 | (13, 49) | — | — | 35 | (25, 47) | 38 | (11, 64) | 58 | (36, 73) | 24 | (9, 44) | — | — |
| Not at all | 30 | (21, 42)† | 83 | (72, 95) | — | — | — | — | — | — | 16 | (7, 26)† | 62 | (36, 89) | — | — | — | — | — | — |
| Years since social transition b | ||||||||||||||||||||
| 1 year or less | 20 | (8, 25)† | — | — | 43 | (0, 72) | 28 | (8, 40) | 7 | (0, 15) | 35 | (25, 50)† | — | — | 60 | (53, 85) | 42 | (18, 60) | 4 | (0, 10) |
| 2–4 years | 39 | (27, 52)† | — | — | 17 | (0, 49) | 44 | (29, 70) | 36 | (16, 52) | 23 | (16, 34)† | — | — | 11 | (3, 22) | 34 | (21, 57) | 32 | (27, 62) |
| 5–14 years | 31 | (20, 46) | — | — | 30 | (0, 59) | 16 | (5, 37) | 52 | (37, 73) | 31 | (20, 42) | — | — | 18 | (2, 28) | 19 | (3, 35) | 54 | (26, 63) |
| 15 + years | 10 | (3, 26) | — | — | 10 | (0, 74) | 13 | (0, 33) | 5 | (2, 12) | 12 | (2, 16) | — | — | 11 | (1, 13) | 5 | (0, 13) | 10 | (0, 21) |
| Using new name and/or pronoun | 60 | (50, 73)† | 6 | (1, 15) | 89 | (70, 100) | 82 | (67, 97) | 100 | (100, 100) | 77 | (66, 87)† | 14 | (3, 32) | 97 | (93, 100) | 99 | (—, —) | 99 | (98, 100) |
| Perceived as trans | ||||||||||||||||||||
| Always or very frequently | 18 | (11, 28)† | 6 | (1, 17) | 33 | (0, 76) | 28 | (12, 48) | 17 | (5, 26) | 7 | (2, 12)† | 7 | (0, 21) | 7 | (0, 19) | 4 | (0, 11) | 3 | (0, 7) |
| Occasionally/rarely | 41 | (30, 51) | 33 | (16, 58) | 49 | (13, 80) | 38 | (20, 54) | 45 | (24, 68) | 42 | (33, 53) | 18 | (3, 32) | 64 | (49, 83) | 62 | (45, 82) | 22 | (13, 37) |
| Never or very rarely | 42 | (30, 52) | 61 | (34, 78) | 8 | (3, 46) | 34 | (17, 56) | 39 | (18, 63) | 51 | (40, 61) | 75 | (56, 94) | 28 | (12, 44) | 34 | (17, 51) | 75 | (59, 85) |
| Wants to be perceived as trans | ||||||||||||||||||||
| Yes | 18 | (9, 26) | 16 | (3, 31) | 12 | (0, 22) | 22 | (5, 38) | 1 | (0, 2) | 18 | (10, 27) | 27 | (6, 56) | 28 | (12, 45) | 12 | (1, 27) | 4 | (1, 9) |
| No | 54 | (44, 66) | 53 | (25, 64) | 52 | (13, 85) | 40 | (28, 69) | 79 | (65, 92) | 52 | (41, 62) | 30 | (0, 47) | 36 | (19, 61) | 48 | (33, 71) | 86 | (76, 95) |
| Don't care | 29 | (19, 40) | 31 | (22, 61) | 36 | (12, 76) | 38 | (13, 53) | 21 | (8, 34) | 30 | (21, 41) | 44 | (23, 77) | 37 | (15, 53) | 40 | (18, 55) | 10 | (2, 19) |
| Legal name change | 33 | (23, 44) | 0 | (—, —) | 5 | (0, 15) | 38 | (21, 59) | 86 | (70, 98) | 35 | (25, 46) | 4 | (0, 14) | 19 | (7, 37) | 56 | (40, 80) | 81 | (59, 96) |
| Sex marker change | ||||||||||||||||||||
| On all ID | 11 | (4, 19) | 0 | (0, 2) | 0 | (—, —) | 2 | (0, 5) | 46 | (15, 61) | 10 | (4, 17) | 0 | (—, —) | 0 | (0, 0) | 9 | (0, 34) | 38 | (20, 57) |
| On any ID | 18 | (10, 29) | 0 | (0,0) | 34 | (0, 73) | 24 | (8, 49) | 33 | (19, 62) | 14 | (8, 21) | 0 | (0, 0) | 5 | (0, 13) | 18 | (7, 34) | 37 | (18, 56) |
Note. Proportions may not add up to 100% due to rounding and RDS estimation procedures for stratum-specific estimates; (—, —) = confidence interval could not be calculated.
aTransgender, transsexual, transitioned.
bAmong those who had begun to live in felt gender full or part time.
†Indicates statistically significant difference in proportions between MTFs and FTMs at the a = .05 level.
Although most trans persons reported being perceived as trans by others occasionally, rarely, or never, MTFs were more likely to always or frequently be perceived as trans (18%, 95% CI: 11–28 versus 7%, 95% CI: 2–12). Gender spectrum differences with respect to the frequency with which trans persons were socially perceived as trans were especially notable among those who had begun medical transition. In this group, the variable can be interpreted as reflecting “passing” in their felt gender role. MTFs with some social and some medical transition were 7.0 times (95% CI: 1.9, upper limit not calculable) as likely to report always or very frequently being perceived as trans, as compared to FTMs of the same transition status. Similarly, those who had completed transition were about half as likely as completely transitioned FTMs to report never or very rarely being perceived as trans (RR = 0.52, 95% CI: 0.40–0.89). While 60% (95% CI: 50–73) of MTFs and 77% (95% CI: 66–87) of FTMs were using a new name and/or pronoun in daily life, only about one-third of trans persons had legally changed their names. An estimated 29% of MTFs and 24% of FTMs had changed the sex designation on at least one form of government-issued identity document.
Medical Transition and Sex Characteristics
Medical transition and sex characteristics are presented in Table 4. In all, 7% (95% CI: 2–13) of MTF-spectrum persons and 5% (95% CI: 1–10) of FTM-spectrum persons indicated having a medically recognized intersex condition. An estimated 46% (95% CI: 35–60) of MTFs and 39% (95% CI: 28–49) of FTMs were currently using hormones for medical transition.
Table 4. Medical Transition and Sex Characteristics of Trans a Ontarians.
| Medical Transition or Sex Characteristic | Male-to-Female Spectrum (MTF) |
Female-to-Male Spectrum (FTM) |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All MTFs (n = 205) |
No Transition (n = 52) |
Social Only (n = 22) |
Some Social and Some Medical (n = 64) |
Complete Social and Medical (n = 62) |
All FTMs (n = 227) |
No Transition (n = 27) |
Social Only (n = 59) |
Some Social and Some Medical (n = 55) |
Complete Social and Medical (n = 84) |
|||||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Medically recognized intersex condition | ||||||||||||||||||||
| Yes | 7 | (2, 13) | 3 | (0, 9) | 9 | (0, 31) | 3 | (0, 11) | 18 | (2, 31) | 5 | (1, 10) | 9 | (0, 32) | 4 | (0, 10) | 10 | (2, 19) | 1 | (0, 4) |
| Unsure | 17 | (10, 26) | 4 | (1, 9) | 40 | (3, 67) | 37 | (16, 57) | 3 | (0, 7) | 14 | (7, 21) | 18 | (4, 52) | 12 | (1, 26) | 15 | (0, 22) | 7 | (1, 18) |
| Self-described medical transition status b | ||||||||||||||||||||
| Completed | 25 | (17, 39) | — | — | — | — | 10 | (—, —) | 100 | (—, —) | 25 | (15, 35) | — | — | — | — | 9 | (—, —) | 100 | (—, —) |
| In process | 32 | (24, 44)† | — | — | — | — | 88 | (76, 99) | — | — | 16 | (10, 22)† | — | — | — | — | 92 | (76, 100) | — | — |
| Planning but not begun | 15 | (7, 22)† | 27 | (11, 47) | 58 | (29, 86) | — | — | — | — | 38 | (28, 49)† | 75 | (58, 95) | 59 | (37, 78) | — | — | — | — |
| Not planning | 3 | (1, 5) | 6 | (2, 12) | 20 | (2, 46) | — | — | — | — | 6 | (1, 14) | 12 | (0, 29) | 12 | (1, 26) | — | — | — | — |
| Not sure | 13 | (5, 21) | 33 | (—, —) | 21 | (—, —) | — | — | — | — | 6 | (2, 15) | 1 | (—, —) | 11 | (—, —) | — | — | — | — |
| Concept does not apply | 11 | (3, 15) | 28 | (9, 46) | 5 | (0, 12) | — | — | — | — | 9 | (4, 14) | 17 | (2, 29) | 16 | (6, 24) | — | — | — | — |
| Hormone use | ||||||||||||||||||||
| Current | 46 | (35, 60) | — | — | — | — | 69 | (49, 92) | 95 | (80, 100) | 39 | (28, 49) | — | — | — | — | 84 | (70, 98) | 100 | (98, 100) |
| Past | 7 | (3, 13)† | — | — | — | — | 3 | (0, 9) | 5 | (0, 20) | 1 | (0, 3)† | — | — | — | — | 6 | (0, 15) | 1 | (0, 2) |
| Never | 47 | (34, 59) | — | — | — | — | 28 | (3, 48) | 0 | (0, 0) | 60 | (50, 72) | — | — | — | — | 11 | (1, 22) | 0 | (0, 0) |
Note. Proportions may not add up to 100% due to rounding and RDS estimation procedures for stratum-specific estimates; (—, —) = confidence interval could not be calculated.
aTransgender, transsexual, transitioned.
bHormonal and/or surgical treatments.
†Indicates statistically significant difference in proportions between MTFs and FTMs at the a = .05 level.
Medical Treatments and Surgeries
Tables 5 and 6 report the proportions of MTF- and FTM-spectrum persons, respectively, who had undergone particular medical and surgical treatments for transition. Hair removal was the most common medical intervention for MTFs, reported by 56% (95% CI: 42–67) overall, including 18% (95% CI: 5–26) of those who had not otherwise begun social or medical transition and 38% (95% CI: 1–77) of those who had socially transitioned only (data not shown). About one-quarter of MTFs (24%, 95% CI: 14–35) and 30% of FTMs (95% CI: 21–40) had undergone any surgery. Mastectomy was the most commonly reported surgery among FTMs, while an estimated 1.4% had any genital surgery, such as phalloplasty (construction of a penis) or metoidioplasty (a genital surgery in which the clitoris is “released” to form a small phallus). Among MTFs, orchiectomy (removal of the testicles) was the most common surgical procedure, and an estimated 15% had undergone genital reconstruction (vaginoplasty). Among those who had completed a social and medical transition, nearly all were currently using hormones. However, not all had undergone genital surgeries or, in some cases, any surgery at all.
Table 5. Transition-Related Procedures: Male-to-Female Spectrum Trans a Ontarians.
| Procedure | All MTFs (n = 205) |
Some Social and Some Medical (n = 64) |
Complete Social and Medical (n = 62) |
|||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | |
| Hair removal | 56 | (42, 67) | 75 | (61, 93) | 89 | (75, 98) |
| Any surgery b | 24 | (14, 35) | 13 | (3, 26)† | 72 | (46, 86) |
| Vocal cord surgery | 3 | (0, 9) | 0 | (0, 0) | 13 | (0, 27) |
| Facial surgery | 4 | (1, 8) | 3 | (0, 10) | 11 | (1, 23) |
| Adam's apple shave | 10 | (2, 18) | 2 | (0, 0) | 30 | (4, 51) |
| Hair transplant | 2 | (0, 3) | 1 | (0, 4) | 3 | (0, 9) |
| Breast augmentation | 12 | (4, 22) | 3 | (0, 11) | 43 | (15, 62) |
| Orchiectomy | 21 | (11, 33) | 10 | (0, 27) | 67 | (41, 85) |
| Vaginoplasty | 15 | (7, 27) | 0 | (0, 0) | 59 | (32, 80) |
aTransgender, transsexual, transitioned.
bReported any transition-related surgical procedure (not including hair removal).
†Indicates statistically significant difference in proportions between MTFs and FTMs at the a = .05 level.
Table 6. Transition-Related Procedures: Female-to-Male Spectrum Trans a Ontarians.
| Procedure | All FTMs (n = 227) |
Some Social and Some Medical (n = 55) |
Complete Social and Medical (n = 84) |
|||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | |
| Any surgery b | 30 | (21, 40) | 38 | (20, 60)† | 88 | (72, 96) |
| Breast reduction | 5 | (1, 8) | 6 | (1, 18) | 5 | (1, 12) |
| Mastectomy | 25 | (17, 36) | 31 | (14, 52) | 83 | (70, 94) |
| Hysterectomy | 13 | (6, 19) | 20 | (5, 40) | 36 | (17, 56) |
| Oophorectomy | 12 | (6, 19) | 19 | (3, 40) | 35 | (16, 55) |
| Metoidioplasty c | — | — | — | — | — | — |
| Phalloplasty | 0.4 | (0, 1) | 0 | (0, 0) | 1 | (0, 4) |
aTransgender, transsexual, transitioned.
bReported any transition-related surgical procedure.
cUnable to calculate due to high homophily: 1% of all FTM participants (unweighted) and 4% of FTM participants who had completed social and medical transition (unweighted) reported undergoing metoidioplasty.
†Indicates statistically significant difference in proportions between MTFs and FTMs at the a = .05 level.
Of 153 transition-related surgeries (reported by 124 participants) that would potentially be eligible for full public funding in Ontario (these surgeries are vaginoplasty, phalloplasty, metoidioplasty, hysterectomy, and mastectomy), 78% (unweighted) took place between 1999 and 2008 (data not shown), when such surgeries were not publicly funded.
Discussion
Our findings demonstrate great heterogeneity of sex, gender, and transition status characteristics among trans Ontarians. This wide diversity belies the popular notion that a linear and rapid transition from one binary sex/gender to the other is the norm among trans persons (Serano, 2007). Only an estimated 23% of trans Ontarians had completed social and medical transition, and this did not necessarily include both hormones and surgery.
FTM-spectrum persons were more likely than MTF-spectrum persons, and youth (aged 16–24) were more likely than adults age 25 and over, to have socially transitioned without medical intervention. As FTMs had a younger age distribution than MTFs, gender-spectrum effects also represent age effects and vice versa. That FTMs were more likely to have socially transitioned without medical intervention reflects a cohort effect (60% of this group had begun to socially transition within the past year), and some of these FTMs may have since medically transitioned. However, FTMs were also more likely to identify as genderqueer (consistent with previous research; Factor and Rothblum, 2008; Kuper et al., 2012), and this group may include FTMs who have socially transitioned to a nonbinary gender and do not plan to medically transition.
That MTF-spectrum persons were less likely to be living in their felt gender, and were less likely to socially transition without medical intervention, may be shaped by the heightened levels of transphobia faced by MTFs (Marcellin, Scheim, Bauer, & Redman, 2013). Transmisogyny, the interaction of transphobia with sexism (Serano, 2007), may make it more difficult for MTF-spectrum people to transition, particularly without hormones and/or surgery. In addition, variation in the need or desire to transition may contribute to the higher proportion of MTFs who had not transitioned, as we estimated that the majority (63%; 95% CI: 42–81) of nontransitioned MTFs had nonbinary gender identities (predominantly cross-dresser) and were less likely to report plans to transition. Care should be taken in interpreting these cross-sectional results; current gender identities and transition plans may represent lifelong identities and plans or an evolving stage in a trajectory of identity discovery, coming out, and transition. Previous research has suggested that identifying as a cross-dresser for a period of time may be a common part of the MTF transgender identity development process (Rankin & Beemyn, 2012).
It is clear that diversity in sex characteristics among trans persons abounds, at all states of transition. Although they were not included in this analysis because the group was too small to analyze, five MTF-spectrum participants had begun medical transition while living in their birth-assigned gender. Some trans persons had begun to transition many years ago but still needed access to additional medical transition procedures: an estimated 13% of MTFs and 5% of FTMs who had undergone some social and some medical transition had begun their social transition 15 years ago or more. In addition, while current or past hormone use was universal among those who had completed medical transition, surgery was not. Contrary to the assumption that medical transition begins with hormones, some of those who had undergone some social and some medical transition had surgically but not hormonally transitioned.
Few trans Ontarians in 2009–2010 had undergone genital surgery. Such surgeries were particularly rare among FTM-spectrum trans people, consistent with findings from other regions (Grant et al., 2011; Newfield et al., 2006) and qualitative reports that many FTMs do not seek or desire genital surgery (Schilt & Waszkiewicz, 2006). These data primarily reflect the experiences of trans persons who transitioned, and had surgery, in a context where these procedures were not publicly funded; 78% of reported surgeries occurred during the decade where transition-related surgeries were not covered by the province's universal health plan, and some who planned to medically transition had undoubtedly not accessed surgeries they would otherwise have had during this time.
A total of 6% of trans Ontarians reported having a medically recognized intersex condition (Coleman, Bauer, et al., 2011), and a high proportion reported that they were unsure. The same proportion of NTDS respondents identified as intersex (Grant et al., 2011). Though the prevalence of gender variance among intersex persons is unknown, clinical data suggest that intersex persons are more likely than nonintersex persons to experience gender dysphoria and to transition, with much variation between intersex conditions (Meyer-Bahlburg, 2009; Yang, Baskin, & DiSandro, 2010). That such a high proportion of trans Ontarians reported having intersex conditions or were unsure may reflect increased incidence of gender transition among intersex persons. However, these results could also be attributed to increased scrutiny and screening for potential intersex conditions as part of the medical transition process, or to the belief of some trans people that trans status is a form of intersex (Spurgas, 2009). As most intersex individuals do not identify as trans or gender nonconforming, intersex advocates caution against conflation of intersex and trans issues (Feder, 2009). Nevertheless, our results demonstrate that health researchers and clinicians should avoid making assumptions about what medical information is relayed by classification as male, female, FTM, or MTF. For example, our study included two participants who were not easily coded as MTF or FTM spectrum, who indicated need for medical care and screening services specific to both male and female endogenous anatomy.
The present study collected more detailed information about gender, sex, and transition status among trans persons than any other research published to date, using a method that allows us to generalize to the networked trans population in Ontario (i.e., those who know at least one other trans person). However, a few important limitations must be noted. While RDS analytic methods have been demonstrated to produce unbiased results when assumptions are satisfied (Salganik, 2006), it is possible for biases to be introduced that are not related to network size or differences in recruitment across groups. Such biases are not adjusted for in RDS analyses. For example, a particular group could be over- or under-recruited by all other groups (McCreesh et al., 2012). In the present study, it is plausible that newly transitioning individuals may have been more motivated to participate. However, the recency of social transitions in this study could also be related to decreased survival among trans persons, or to trans persons transitioning in increasing numbers, as well as to differential participation.
Transition status groups were defined based on theoretical and sample size considerations; some groups were quite small. In general, confidence intervals are widest where groups are small and at proportions closer to 50%. All point estimates presented should be interpreted in relation to the range of plausible values represented by (sometimes wide) confidence intervals.
Measures employed were pretested for content validity and clarity but were not otherwise validated for use in trans populations. Due to the heterogeneity of this population, care must be taken in interpretation. For instance, those who reported that they were never perceived as trans may have been consistently socially perceived as their felt gender or as nontrans members of their birth-assigned gender.
Our findings of great sex and gender heterogeneity within and across transition status groups underscore the need for more precise and valid measurement of sex and gender-related variables in health and sexuality research (Bauer, 2012). For instance, in research with broad population samples, measures aiming to identify transgender respondents (such as the recommended two-step method; Tate et al., 2013) should be designed to capture the full spectrum of trans experience, including individuals who not identify with the “opposite” binary gender to that assigned at birth. Moreover, measures of additional dimensions of sex or gender may be required to address specific hypotheses (Bauer, 2012), as demonstrated by the heterogeneity we have observed within broad categories of gender spectrum. Within trans-specific research, it cannot be assumed that measures developed and tested with clinical samples of those seeking medical transition (e.g., Deogracias et al., 2007) will be valid for the trans population more broadly. Our finding of gender-spectrum differences across a number of trans-specific gender characteristics should not be surprising, but highlights the necessity of distinguishing between gender spectra in the design, analysis, and reporting of studies which include trans participants. Overall, empirical trans sexuality research that considers the diverse range of trans experiences evident in our data is necessary. In recent years, nonclinical theoretical work on trans sexuality has begun to emerge (Bettcher, 2013; Edelman & Zimman, 2013), but quantitative and empirical work has primarily focused either on HIV prevention (Melendez et al., 2006) or on sexual behavior and functioning in clinical populations of transsexual persons (Klein & Gorzalka, 2009).
Approaches to clinical care of trans people in Canada and the United States are increasingly de-emphasizing the psychiatric diagnosis of gender identity disorder (now gender dysphoria; American Psychiatric Association, 2013), moving from a “disease-based” to an “identity-based” model of trans health (Bockting & Coleman, 2007), and recognizing a wider range of gender nonconformity and, consequently, of transition trajectories (Fee, Brown, & Laylor, 2003; Coleman, Bockting, et al., 2011). Our results provide empirical evidence of the diversity increasingly observed by clinicians. This heterogeneity has wide-ranging implications for health care—for instance, in long-term care facilities where trans patients may incorrectly be assumed to have “completed” a linear transition; or in psychological counseling settings where trans persons may require support for navigating social life as gender fluid, or for determining what transition options are most suitable for them. Those who have not transitioned, despite being aware of their trans status for many decades, in some instances, may require mental health care that is attentive to gender identity concerns. Our results indicate that assumptions cannot be made about whether those individuals wish or plan to transition; some may desire support for navigating their gender identity without transitioning. However, for those who are planning to transition but have not yet done so, risk of suicidal thoughts and attempts is particularly pronounced (Bauer, Pyne, Francino, & Hammond, 2013).
Social policies have been slow to respond to the heterogeneity within trans populations. In recent years, some countries have made great advances in adapting policies and practices to accommodate those who transition gender and/or sex. For instance, a requirement that one must have transition-related surgery in order to change one's sex designation on an Ontario birth certificate was eliminated in 2012. Similar restrictions have been lifted in Argentina, Australia, Taiwan, and the United Kingdom. However, less attention has been paid to the needs of nontransitioning, “partially” transitioning, and gender-nonconforming persons. In Ontario, to change the sex designation on identification, individuals must certify that they “are living full-time in that gender identity and intend to maintain it” (Ontario Ministry of Health and Long-Term Care, 2012). Trans persons with nonbinary identities, or who are in process of transition, or who are not perceived in their felt gender despite transitioning may be better served by policies that eliminate gender and sex markers, wherever possible. We question whether there is any need for sex/gender designation on Canadian identification, as sex/gender is rarely used for identity verification and serves no legal purpose since laws based on sex have been equalized (e.g., marriage, property, inheritance, voting). Similar issues arise with gender and sex fields in computerized record systems, which typically do not have simple mechanisms for changing gender and sex markers. This can lead to problems with health records, insurance, and billing; outing in professional and education settings; and denial of commercial services due to suspicion of fraud. These problems could be partially remedied through introduction of options to allow for changes to gender and sex markers in these systems, and by delinking other processes (e.g., ordering of medical tests or procedures) from gender fields (Deutsch et al., 2013). A more comprehensive solution would be to eliminate these markers wherever they are not necessary.
Requiring trans individuals to have taken hormones or undergone transition-related surgeries, or to have changed their sex designation, to access the gender-segregated institution or facility most appropriate to their felt gender will clearly exclude the majority of trans Ontarians. However, even more liberal policies that respect gender self-identification may not address the needs of the substantial proportion of trans persons who do not identify as primarily male or female, or who live part time in their felt gender role. Optional gender-neutral facilities, including mixed-gender and single room options, are crucial to ensure the safety and dignity of all trans persons.
An estimated 59% of networked trans Ontarians had begun to socially transition in the past four years, comparable to findings from the European Union, where data collected in 2007 (n = 1, 964) showed that 57% had started transition within the past five years. This likely reflects the impact of increased information sharing, support, and changes in policy that allow more trans people to move forward. It is increasingly possible for trans persons in Ontario and in other regions to live and express their genders as they understand them, in all their complexity, and thus to more fully participate in and contribute to their communities. Institutions that are currently seeing the “tip of the iceberg” will need to adapt to this reality through proactive policy and practice changes.
Acknowledgments
The authors wish to acknowledge the contributions of the 16 Community Engagement Team members and other Trans PULSE contributors who worked to develop and promote the survey, the 89 first-phase participants, and the 433 survey participants.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders () 5th ed. Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Bauer G. R. (2012). Making sure everyone counts: Considerations for inclusion, identification, and analysis of transgender and transsexual participants in health surveys In Institute of Gender & Health Canadian Institutes of Health Research (Ed.), What a difference sex and gender make (pp. 59–67). Vancouver, Canada: Institute of Gender and Health, Canadian Institutes of Health Research. [Google Scholar]
- Bauer G. R., Pyne J., Francino M. C., & Hammond R. (2013). La suicidabilité parmi les personnes trans en Ontario: Implications en travail social et en justice sociale [Suicidality among trans people in Ontario: Implications for social work and social justice] Service Social, 59, 35–62 10.7202/1017478ar [DOI] [Google Scholar]
- Bauer G. R., Travers R., Scanlon K., & Coleman T. (2012). High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: A province-wide respondent-driven sampling survey BMC Public Health, 12, 292 10.1186/1471-2458-12-292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettcher T. M. (2013). When selves have sex: What the phenomenology of trans sexuality can teach about sexual orientation Journal of Homosexuality Advance online publication. doi:10.1080/00918369.2014.865472 [DOI] [PubMed] [Google Scholar]
- Blackless M., Charuvastra A., Derryck A., Fausto-Sterling A., Lauzanne K., & Lee E. (2000). How sexually dimorphic are we? Review and synthesis American Journal of Human Biology, 12, 151–166 [DOI] [PubMed] [Google Scholar]
- Bockting W. O. (2008). Psychotherapy and the real-life experience: From gender dichotomy to gender diversity Sexologies, 17, 211–224 10.1016/j.sexol.2008.08.001 [DOI] [Google Scholar]
- Bockting W. O., & Coleman E. (2007). Developmental stages of the transgender coming out process: Toward an integrated identity In Ettner R., Monstrey S. & Eyler E. (Eds.), Principles of transgender medicine and surgery (pp. 185–208). Binghamton, NY: Haworth Press. [Google Scholar]
- Clements-Nolle K., Marx R., Guzman R., & Katz M. (2001). HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention American Journal of Public Health, 91, 915–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E., Bockting W., Botzer M., Cohen-Kettenis P., DeCuypere G., Feldman J., … Zucker K. (2011). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7 International Journal of Transgenderism, 13, 165–232 10.1080/15532739.2011.700873 [DOI] [Google Scholar]
- Coleman T., Bauer G. R., Scanlon K., Travers R., Kaay M., & Francino M. (2011, November 30). Challenging the binary: Gender characteristics of trans Ontarians Trans PULSE E-Bulletin, 2(2). Retrieved from http://transpulseproject.ca/wp-content/uploads/2011/12/E4English.pdf [Google Scholar]
- Conron K. J., Scott G., Stowell G. S., & Landers S. J. (2012). Transgender health in Massachusetts: Results from a household probability sample of adults American Journal of Public Health, 102, 118–122 10.2105/AJPH.2011.300315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deogracias J. J., Johnson L. L., Meyer K., Kessler S. J., Schober J. M., & Zucker K. J. (2007). The Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults Journal of Sex Research, 44, 370–379 10.1080/00224490701586730 [DOI] [PubMed] [Google Scholar]
- Deutsch M. B., Green J., Keatley J., Mayer G., Hastings J., & Hall A. M. (2013). Electronic medical records and the transgender patient: Recommendations from the World Professional Association for Transgender Health EMR Working Group Journal of the American Medical Informatics Association, 20, 700–703 10.1136/amiajnl-2012-001472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman E. A., & Zimman L. (2013). Boycunts and bonus holes: Trans men's bodies, neoliberalism, and the sexual productivity of genitals Journal of Homosexuality Advance online publication. doi:10.1080/00918369.2014.870438 [DOI] [PubMed] [Google Scholar]
- Factor R. J., & Rothblum E. (2008). Exploring gender identity and community among three groups of transgender individuals in the United States: MTFs, FTMs, and genderqueers Health Sociology Review, 17, 235–253 10.5172/hesr.451.17.3.235 [DOI] [Google Scholar]
- Fausto-Sterling A. (2000). Sexing the body: Gender politics and the construction of sexuality. New York, NY: Basic Books. [Google Scholar]
- Feder E. K. (2009). Imperatives of normality: From “Intersex” to “Disorders of Sex Development.” GLQ: A Journal of Lesbian and Gay Studies, 15, 225–247 10.1215/10642684-2008-135 [DOI] [Google Scholar]
- Fee E., Brown T. M., & Laylor J. (2003). One size does not fit all in the transgender community American Journal of Public Health, 93, 899 10.2105/AJPH.93.6.899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forshee A. S. (2008). Transgender men: A demographic snapshot Journal of Gay and Lesbian Social Services, 20, 221–236 10.1080/10538720802235229 [DOI] [Google Scholar]
- Grant J. M., Mottet L. A., Tanis J., Harrison J., Herman J. L., & Keisling M. (2011). Injustice at every turn: A report of the National Transgender Discrimination Survey Washington, DC: National Center for Transgender Equality and National Gay and Lesbian Task Force. [Google Scholar]
- Hansbury G. (2005). The middle men: An introduction to the transmasculine identities Studies in Gender and Sexuality, 6, 241–264 10.1080/15240650609349276 [DOI] [Google Scholar]
- Harrison J., Grant J. M., & Herman J. L. (2011). A gender not listed here: Genderqueers, gender rebels, and otherwise in the National Transgender Discrimination Survey LGBTQ Policy Journal at the Harvard Kennedy School, 2, 13–24. [Google Scholar]
- Heckathorn D. D. (1997). Respondent-driven sampling: A new approach to the study of hidden populations Social Problems, 44, 174–199 10.2307/3096941 [DOI] [Google Scholar]
- Heckathorn D. D. (2002). Respondent-driven sampling II: Deriving valid population estimates from chain-referral samples of hidden populations Social Problems, 49, 11–34 10.1525/sp.2002.49.1.11 [DOI] [Google Scholar]
- Hembree W. C., Cohen-Kettenis P., Delemarre-van de Waal H. A., Gooren L. J., Meyer W. J., Spack N. P., Endocrine Society. (2009). Endocrine treatment of transsexual persons: An Endocrine Society clinical practice guideline Journal of Clinical Endocrinology and Metabolism, 94, 3132–3154 10.1210/jc.2009-0345 [DOI] [PubMed] [Google Scholar]
- Johnson J. L., Greaves L., & Repta R. (2009). Better science with sex and gender: Facilitating the use of a sex and gender-based analysis in health research International Journal for Equity in Health, 8, 14 10.1186/1475-9276-8-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein C., & Gorzalka B. B. (2009). Sexual functioning in transsexuals following hormone therapy and genital surgery: A review Journal of Sexual Medicine, 6, 2922–2939 10.1111/j.1743-6109.2009.01370.x [DOI] [PubMed] [Google Scholar]
- Krieger N. (2003). Genders, sexes, and health: What are the connections—And why does it matter? International Journal of Epidemiology, 32, 652–657 10.1093/ije/dyg156 [DOI] [PubMed] [Google Scholar]
- Kuper L. E., Nussbaum R., & Mustanski B. (2012). Exploring the diversity of gender and sexual orientation identities in an online sample of transgender individuals Journal of Sex Research, 49, 244–254 10.1080/00224499.2011.596954 [DOI] [PubMed] [Google Scholar]
- Lombardi E. (2009). Varieties of transgender/transsexual lives and their relationship with transphobia Journal of Homosexuality, 56, 977–992 10.1080/00918360903275393 [DOI] [PubMed] [Google Scholar]
- Marcellin R. L., Scheim A., Bauer G., & Redman N. (2013, March 7). Experiences of transphobia among trans Ontarians Trans PULSE E-Bulletin, 3(2). Retrieved from http://transpulseproject.ca/wp-content/uploads/2013/03/Transphobia-E-Bulletin-6-vFinal-English.pdf [Google Scholar]
- McCreesh N., Frost S. D. W., Seeley J., Katongole J., Tarsh M. N., Ndunguse R., … White R. G. (2012). Evaluation of respondent-driven sampling Epidemiology, 23, 138–147 10.1097/EDE.0b013e31823ac17c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melendez R., Bonem L., & Sember R. (2006). On bodies and research: Transgender issues in health and HIV research articles Sexuality Research and Social Policy, 3, 21–38 10.1525/srsp.2006.3.4.21 [DOI] [Google Scholar]
- Meyer-Bahlburg H. F. L. (2009). Variants of gender differentiation in somatic disorders of sex development: Recommendations for Version 7 of the World Professional Association for Transgender Health's Standards of Care International Journal of Transgenderism, 11, 226–237 10.1080/15532730903439476 [DOI] [Google Scholar]
- Money J. (1995). Gendermaps: Social constructionism, feminism, and sexosophical history New York, NY: Continuum. [Google Scholar]
- Money J., & Ehrhardt A. A. (1972). Man and woman, boy and girl: The differentiation and dimorphism of gender identity from conception to maturity Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Newfield E., Hart S., Dibble S., & Kohler L. (2006). Female-to-male transgender quality of life Quality of Life Research, 15, 1447–1457 10.1007/s11136-006-0002-3 [DOI] [PubMed] [Google Scholar]
- Ontario Ministry of Health, & Long-Term Care (2012). Ontario Health Insurance Plan questions and answers. Retrieved from http://www.health.gov.on.ca/en/public/programs/ohip/ohipfaq_mn.aspx [Google Scholar]
- Rachlin K., Green J., & Lombardi E. (2008). Utilization of health care among female-to-male transgender individuals in the United States Journal of Homosexuality, 54, 243–258 10.1080/00918360801982124 [DOI] [PubMed] [Google Scholar]
- Rankin S., & Beemyn G. (2012). Beyond a binary: The lives of gender-nonconforming youth About Campus, 17, 2–10 10.1002/abc.21086 [DOI] [Google Scholar]
- Rosser B., Oakes J., Bockting W., & Miner M. (2007). Capturing the social demographics of hidden sexual minorities: An Internet study of the transgender population in the United States Sexuality Research and Social Policy, 4, 50–64 10.1525/srsp.2007.4.2.50 [DOI] [Google Scholar]
- Rotondi N. K., Bauer G. R., Travers R., Travers A., Scanlon K., & Kaay M. (2011). Depression in male-to-female transgender Ontarians Canadian Journal of Community Mental Health, 30, 113–133. [Google Scholar]
- Salganik M. J. (2006). Variance estimation, design effects, and sample size calculations for respondent-driven sampling Journal of Urban Health, 83, i98–i112 10.1007/s11524-006-9106-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salganik M. J., & Heckathorn D. D. (2004). Sampling and estimation in hidden populations using respondent-driven sampling Sociological Methodology, 34, 193–240 10.1111/j.0081-1750.2004.00152.x [DOI] [Google Scholar]
- Sanchez N. F., Sanchez J. P., & Danoff A. (2009). Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City American Journal of Public Health, 99, 713–719 10.2105/AJPH.2007.132035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilt K., & Waszkiewicz E. (2006, August). I feel so much more in my body: Challenging the significance of the penis in transsexual men's bodies. Paper presented at the annual meeting of the American Sociological Association, Montreal, Quebec, Canada. [Google Scholar]
- Serano J. (2007). Whipping girl: A transsexual woman on sexism and the scapegoating of femininity Berkeley, CA: Seal Press. [Google Scholar]
- Spurgas A. K. (2009). (Un)Queering identity: The biosocial production of intersex/DSD In Holmes M. (Ed.), Critical intersex (pp. 97–122). Surrey, UK: Ashgate. [Google Scholar]
- Tate C. C., Ledbetter J. N., & Youssef C. P. (2013). A two-question method for assessing gender categories in the social and medical sciences Journal of Sex Research, 50, 767–776 10.1080/00224499.2012.690110 [DOI] [PubMed] [Google Scholar]
- Tolman D. L., & Diamond L. M. (2001). Desegregating sexuality research: Cultural and biological perspectives on gender and desire Annual Review of Sex Research, 12, 33–74 10.1080/10532528.2001.10559793 [DOI] [PubMed] [Google Scholar]
- Volz E., Wejnert C., Degani I., & Heckathorn D. (2010). Respondent-driven sampling analysis tool version 6.0.1 (RDSAT) Ithaca, NY: Cornell University. [Google Scholar]
- Yang J. H., Baskin L. S., & DiSandro M. (2010). Gender identity in disorders of sex development: Review article Urology, 75, 153–159 10.1016/j.urology.2009.07.1286 [DOI] [PubMed] [Google Scholar]
- Zou G. Y., & Donner A. (2008). Construction of confidence limits about effect measures: A general approach Statistics in Medicine, 10, 1693–1702 10.1002/sim.3887 [DOI] [PubMed] [Google Scholar]
- Zucker K. J., & Bradley S. J. (1995). Gender identity disorder and psychosexual problems in children and adolescents New York, NY: Guilford Press. [DOI] [PubMed] [Google Scholar]


