Abstract
Personality is relatively stable in adulthood but could change in response to life transitions, such as caring for a spouse with a terminal illness. Using a case-control design, spousal caregivers (n=31) of patients with terminal lung cancer completed the NEO-FFI twice, 1.5 years apart, before and after the patient’s death. A demographically-matched sample of community controls (n=93) completed the NEO-FFI on a similar timeframe. Based on research and theory, we hypothesized that bereaved caregivers would experience greater changes than controls in interpersonal facets of extraversion (sociability), agreeableness (prosocial, nonantagonistic), and conscientiousness (dependability). Consistent with hypotheses, bereaved caregivers experienced an increase in interpersonal orientation, becoming more sociable, prosocial, and dependable (Cohen’s d = .48−.67), though there were no changes in nonantagonism. Changes were not observed in controls (ds ≤ .11). These initial findings underscore the need for more research on the effect of life transitions on personality.
Keywords: Bereavement adjustment, Caregiving, Personality change
Spousal caregivers of patients with terminal illnesses simultaneously experience transitions to new roles and often-unprecedented stressors surrounding loss. Recognizing that spousal caregivers are susceptible to elevated morbidity and mortality, they have been described as “hidden patients” (Löckenhoff, Duberstein, Friedman, & Costa, 2011). Transitions can lead to increased depression and anxiety, and some caregivers experience prolonged grief during bereavement (Braun, Mikulincer, Rydall, Walsh, & Rodin, 2007; Prigerson et al., 2009). Caregivers may also experience existential changes, such as finding a greater sense of meaning and purpose (Kim, Carver, Schulz, Lucette, & Cannady, 2013). It has been suggested that during the bereavement process some caregivers may experience broad changes in personality (Caspi & Moffitt, 1993; McCrae & Costa, 1993), particularly in terms of how they interact with others (Shapiro, 2001; Shear & Shair, 2005). As the first study of which we are aware to quantify longitudinal changes in the five established domains of personality in a sample of bereaved caregivers, this study has implications for understanding the malleability of personality in response to life transitions in middle and older adulthood and efforts to enhance family-centered end-of-life care.
The Five Factor Model (Costa & McCrae, 1992) provides a useful taxonomic frame for describing human dispositional variation along five broad personality domains: neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. A meta-analysis of 150 longitudinal studies showed that most personality development occurs prior to age 30, becoming highly crystallized in middle and older adulthood with 5-year longitudinal correlations surpassing r = .70 (Roberts & DelVecchio, 2000). Even during this peak of stability, however, personality can change due to life transitions, such as starting a job or getting married, and success or failure in making these transitions (Hill, Turiano, Mroczek, & Roberts, 2012; Hudson, Roberts, & Lodi-Smith, 2012; Roberts & Mroczek, 2008; Specht, Egloff, & Schmukle, 2013).
Despite the importance of caregiver personality for mental health and physical functioning (Kim, Duberstein, Sorensen, & Larson, 2005; Löckenhoff et al., 2011), existing studies have provided inconclusive evidence that spouses experience any personality change surrounding the death of their partner (McCrae & Costa, 1993; Specht, Egloff, & Schmukle, 2011). One study (McCrae & Costa, 1993) found no differences between bereaved and married spouses on extraversion and openness, but the other three traits were not examined. Another showed that experiencing the death of a spouse was associated with less stable longitudinal correlations for agreeableness (Specht et al., 2011). Neither study could explore the influence of the caregiving-bereavement transition on personality change. In both studies, the samples of bereaved spouses were quite heterogeneous – not all were involved with caregiving, and the causes of death varied considerably (i.e., various chronic and acute illnesses, accidents, suicide, and homicide).
It has been suggested that life transitions that are characterized by relatively clearer social norms and rituals are more likely to engender personality change and that transitions characterized by relatively unclear norms are more likely to foster personality continuity (Caspi & Moffitt, 1993). Consistent with this view, the Sociogenomic Model of Personality (Roberts, 2009) emphasizes that repeated reinforcement of state changes in constituent components of personality (i.e., thought, behavior, and affect) is needed to foster personality development incrementally over time, and social norms are an important source of ongoing reinforcement. Acknowledging that social norms surrounding death from natural illness in the United States continue to evolve (Carr, 2012), these norms are arguably somewhat better established for terminal illnesses with a predictable course (e.g., lung cancer) than for sudden deaths by accident, homicide, or suicide (Aldred, Gott, & Gariballa, 2005; Cerel, Jordan, & Duberstein, 2008). Therefore, we focused this initial investigation on terminal lung cancer and hypothesized that the process of losing one’s partner to lung cancer would lead spousal caregivers to experience personality change.
Drawing upon bereavement research and theory (Shapiro, 2001; Shear & Shair, 2005), we hypothesized that bereaved spousal caregivers would be particularly likely to experience changes in interpersonal facets of personality spanning extraversion, agreeableness, and conscientiousness. Caregivers may seek additional social support during bereavement (Ownsworth, Henderson, & Chambers, 2010), and the loss of a spouse could lead to significant restructuring of social networks (Bergman & Haley, 2009), perhaps with implications for the sociability component of extraversion. As well, bereaved caregivers commonly engage in “benefit finding” (Kim et al., 2013), such as developing a greater sense of tender-mindedness, compassion, responsibility, and character growth, perhaps reflected in aspects of agreeableness and the dependability facet of conscientiousness. In contrast to these changes in social behavior, bereavement research and theory makes no explicit predictions about openness to experience and suggests that changes in emotional stability are more commonly acute than enduring (Prigerson et al., 2009).
The current study is the first to examine personality change during the caregiving-bereavement transition in spouses of patients with terminal illnesses. A case-control design was used to examine personality changes over approximately 1.5 years in 31 spousal caregivers of patients with terminal lung cancer and a demographically-matched control group of 93 continuously-married adults in the community. Our primary hypothesis was that spousal caregivers would be more likely than community controls to experience personality change, as demonstrated by a higher percentage of participants experiencing reliable changes (Reliable Change Index ≥ 1.96; Jacobson & Truax, 1991) across the NEO-FFI personality facets. Second, based on research (Bergman & Haley, 2009; Kim et al., 2013; Ownsworth et al., 2010; Specht et al., 2011) and theory (Shapiro, 2001; Shear & Shair, 2005), we expected change to be confined primarily to interpersonal aspects of personality. Thus, we hypothesized that bereaved spousal caregivers would experience greater mean shifts and less stable longitudinal correlations than controls for interpersonal facets.
Method
Participants and procedures
Self-reported personality data were collected longitudinally from a sample of spousal caregivers of patients with terminal lung cancer. For relatively rare events such as mortality, “case-control” study designs are often used (Rothman, Greenland, & Lash, 2008). Such designs assess individuals experiencing a relatively rare event and compare them to a generally similar control group. We utilized a control group of continuously-married adults in the same community. As advocated in guidelines for case-control studies, we selected a control group larger than the number of cases to provide reliable estimates and increased power for comparisons. A control group three to four times the size of controls is typically recommended, with larger control groups generally showing only small improvements in power. The control group was frequency matched1 (Rothman et al., 2008) on age, gender, education level, and marital status at study entry (see Table 1), meaning that these variables were comparable across the two groups and thus could not account for observed group differences on any study outcome variables.
Table 1.
Baseline Characteristics for Bereaved Spousal Caregivers and Matched Community Controls
| Caregivers (n = 31) |
Controls (n = 93) |
|
|---|---|---|
| Variable |
n (%) or M (SD) |
n (%) or M (SD) |
| Gender, female | 23 (74%) | 69 (74%) |
| Married a | 31 (100%) | 93 (100%) |
| Race, white | 31 (100%) | 87 (94%) |
| Age, years | 64.6 (9.3) | 67.6 (4.2) |
| Education, years | 13.7 (2.0) | 14.0 (2.4) |
| Personality, 1–5 scales | ||
| Big Five Domains | ||
| Neuroticism | 2.41 (0.65) | 2.24 (0.64) |
| Extraversion | 3.28 (0.59) | 3.40 (0.54) |
| Openness | 3.29 (0.50) | 3.22 (0.44) |
| Agreeableness | 3.89 (0.39) | 3.95 (0.41) |
| Conscientiousness | 4.04 (0.44) | 3.88 (0.53) |
| Interpersonal Orientation | 3.80 (0.34) | 3.86 (0.36) |
| Sociability | 3.18 (0.68) | 3.39 (0.65) |
| Prosocial Orientation | 4.02 (0.50) | 4.18 (0.43) |
| Nonantagonistic Orientation | 3.84 (0.44) | 3.83 (0.45) |
| Dependability | 4.15 (0.40) | 4.06 (0.54) |
Note All caregivers experienced the death of their partner during the study, whereas all controls remained continuously married throughout the duration of the study.
The sample of spousal caregivers (n = 31) consisted of all participants who completed personality measures, before and after the patient’s death, as a part of a broader psycho-oncology study of 120 caregivers conducted with IRB approval at the University of Rochester cancer center (Kim et al., 2005). They first completed the NEO Five Factor Inventory (NEO-FFI, Costa & McCrae, 1992) at study enrollment, which was 8.15 (SD = 14.14) months after the patient’s diagnosis, and again 18.00 (SD = 7.47) months later, which was 6.91 (SD = 1.35) months after the patient’s death. In this sample, mean survival was 1.59 (SD = 1.50) years after diagnosis. Data on mortality in the entire cohort are unavailable but refusal to participate in the post-loss interview was believed to be exceedingly rare. Nearly half the inception cohort had Stage I disease (Kim et al., 2005) and most of these patients were alive 18 months after study entry. In contrast, most of the patients in this post-mortem sample had either Stage III (35%) or Stage IV (42%) disease at the time of study entry. Moreover, in comparison to caregivers who only completed assessments at study entry, those in the present analyses were higher on openness (p = .02) but were otherwise comparable with respect to personality and demographics (all ps >.20).
The control group consisted of 93 demographically-matched continuously-married adults from the Rochester community. They were selected from participants recruited through primary care in one of two broader IRB-approved studies of health and aging (Chapman et al., 2009; Lyness, Yu, Tang, Tu, & Conwell, 2009). They completed the NEO-FFI at study enrollment and again 16.06 (SD = 7.42) months later, with all remaining married at follow-up. Controls and caregivers were comparable with respect to basic demographics at study entry (proportion married, female, over age 70, college educated, and white), mean levels on the Big 5 personality traits at study entry, and the duration of the follow-up period between personality assessments.
Measures
The 60-item NEO-FFI (Costa & McCrae, 1992) was used to assess personality. As supported in factor analytic studies (Chapman, 2007; Saucier, 1998), the NEO-FFI measures the Big 5 domains of personality as well as 13 subscales assessing narrower facets. These scales included Neuroticism (self-reproach, negative affect), Extraversion (sociability, positive affect, activity level), Openness to experience (aesthetic interests, intellectual interests, unconventionality), Agreeableness (prosocial orientation, nonantagonistic orientation), and Conscientiousness (dependability, orderliness, goal striving). The NEO-FFI has shown evidence for reliability and validity in studies of personality in middle and older adulthood, including among caregivers of patients with serious illnesses (Chapman, Lyness, & Duberstein, 2007; Patrick & Hayden, 1999). Internal consistency reliability was comparable across time points and samples, with a median Cronbach’s alpha of .81 for domains and .67 for facets, close to the .70 of longer NEO-PI-R facets and in line with reports from general samples (Chapman, 2007; Saucier, 1998). Additional descriptives are available in Table 1 and Table in the Appendix (see Online Supplemental Materials, Table A1). For our secondary hypothesis, we used an overall indicator of Interpersonal Orientation, which was the summated composite of four interpersonal facets: sociability, prosocial orientation, nonantagonistic orientation, and dependability (Saucier, 1998). These interpersonal facets have been shown to correlate with other interpersonal constructs (e.g., warmth, altruism, trust, dutifulness) and have implications for adult social functioning (Chapman, 2007; Hitchcock, 2008; Saucier, 1998). In the present sample, Cronbach’s alpha was .73 and .77 for caregivers and .76 and .79 for controls, at baseline and follow-up respectively (average alpha = .76).
Statistical Analyses
The first hypothesis involved examining the percentage of participants in each sample experiencing reliable change in any of the personality facets. The Reliable Change Index (RCI; Jacobson & Truax, 1991) was used to examine whether observed change in a facet score exceeded the level of change that would be expected due to measurement error, given the standard deviation and reliability of the measure (see Robins Fraley, Roberts, & Trzesniewski, 2001; also McCrae, Kurtz, Yamagata, & Terracciano, 2011). RCIs of 1.96 or greater (corresponding to an alpha level of .05) in absolute magnitude reflected reliable change. A Z-test of proportions was used as an omnibus test to compare the percentage of bereaved spousal caregivers and the percentage of controls experiencing reliable personality change.
The second hypothesis examined the magnitude and direction of changes in interpersonal facets of personality. Change was operationalized using two standard approaches (Roberts & Mroczek, 2008). To quantify mean levels of change, we calculated Cohen’s d, and used independent-samples t-tests and MANOVA as appropriate to evaluate the statistical significance of between-group differences. Greater absolute values for Cohen’s d indicate greater change in a group as a whole. To assess relative change, we calculated Pearson’s r, with lower values reflecting greater change in the rank ordering of a group of persons, regardless of the group’s mean shift. Regression was used to evaluate the statistical significance of between-group differences in correlations, as indicated by a significant group by personality interaction term. When mean and relative changes were present simultaneously, we also examined the proportion of participants experiencing 1 and 2 SD changes, with between-group differences evaluated using Z-tests. The case-control design controlled for demographic differences via frequency matching, and sensitivity analyses provided statistical adjustment for time since diagnosis, the length of the follow-up, and cancer staging. Finally, to guard against Type I errors, the binomial probability test was used to examine whether the number of interpersonal facets with observed differences significantly exceeded the number that would be expected by chance.
Results
Omnibus Test of Personality Change
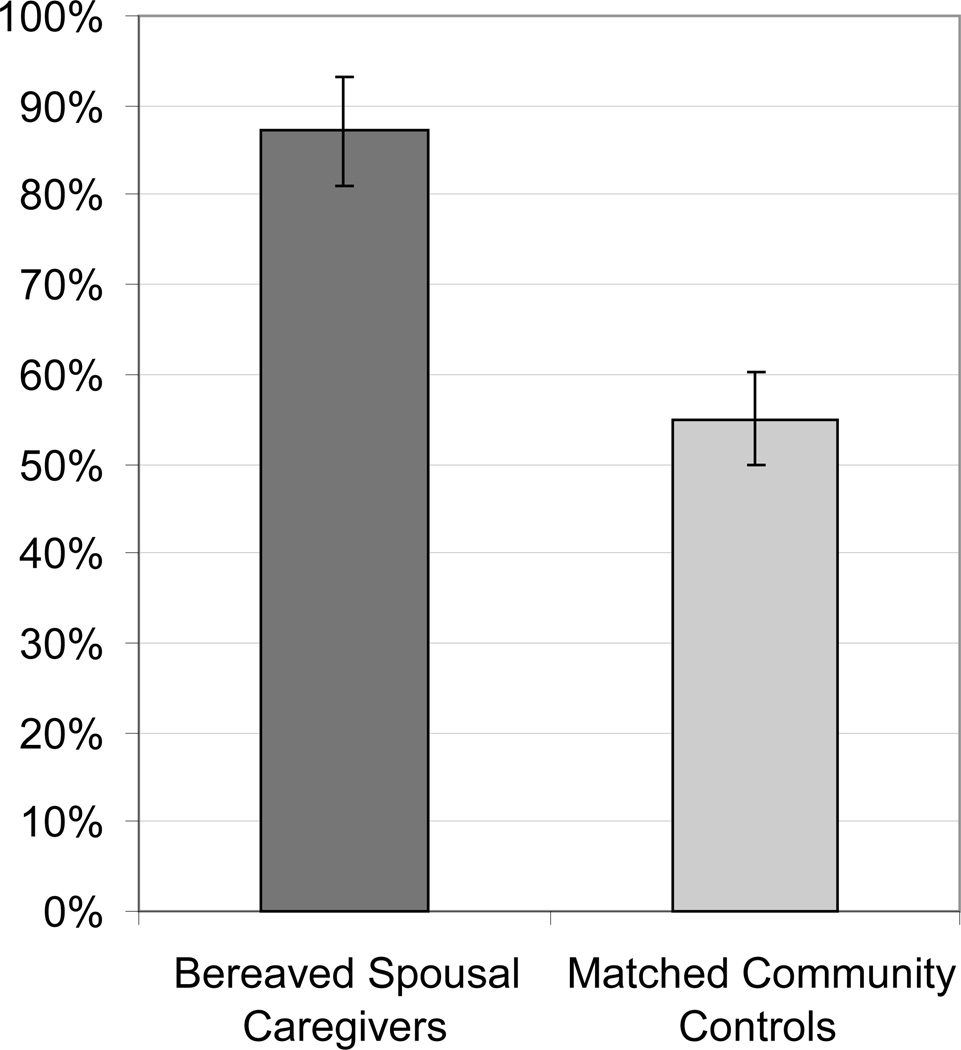
Consistent with our broad first hypothesis, bereaved caregivers were more likely than controls to experience reliable personality change (see Figure 1). Specifically, 87.1% of bereaved caregivers (95% confidence interval [CI] = [75.3%, 98.9%]) experienced reliable personality change, versus 54.8% of controls (CI = [44.7%, 64.9%]), Z = 3.20, p = .001. This difference of 32.3% was qualified by a broad confidence interval [12.7%, 51.9%].
Figure 1.
Percentage of participants experiencing reliable changes (RCI ≥ 1.96) in any of on the NEO-FFI personality facets. Supporting our first hypothesis, bereaved spousal caregivers were significantly more likely to experience personality change than matched community controls over the 1.5-year follow-up period. Error bars indicate the standard error of the mean
Areas of Personality Change
As hypothesized, bereaved spousal caregivers experienced changes in interpersonal orientation, whereas there were no significant changes in controls on any facet. Table 2 shows mean changes and longitudinal correlations. Bereaved caregivers experienced an increase of d = .67 (CI = [.33, 1.01]) on the interpersonal orientation summated composite, indicating an average increase of ⅔-SD in interpersonal orientation. In MANOVA, the overall effect for between group differences in change on the four interpersonal facets was significant, Wilks’ Λ = .884, F(4, 119) = 3.87, p = .005, as were individual effects for sociability, prosocial orientation, and dependability (ds from .48 to .50; see Table 2), but not for nonantagonistic orientation. Thus, relative to controls, bereaved caregivers experienced increases in most but not all aspects of interpersonal orientation.
Table 2.
Bereaved Spousal Caregivers and Matched Community Controls Differ in Amount of Personality Change Experienced During the 1.5-year Longitudinal Study
| Mean Change (Cohen’s d) |
Longitudinal Correlation (r) |
|||
|---|---|---|---|---|
| Personality Measure | Caregivers | Controls | Caregivers | Controls |
| Sociability (E) | .48** b | −.11 | .80*** | .80*** |
| Prosocial Orientation (A) | .50** a | .01 | .25 a | .58*** |
| Nonantagonistic Orientation (A) | −.01 | .03 | .64*** | .72*** |
| Dependability (C) | .50** a | .00 | .58*** | .60*** |
| Interpersonal Orientation | .67*** b | .01 | .60*** | .77*** |
Note. Cohen’s d is the standardized mean difference (change in SD units), with higher scores reflecting increased presence of the trait over time. r is the longitudinal correlation between personality scores at study entry and follow-up; higher correlations indicate greater relative stability. E = extraversion facet, A = agreeableness facet, C = conscientiousness fact, Interpersonal Orientation = the summated composite of the four measures.
p < .05
p < .01
p < .001
Differs from the control group, p < .05
Differs from the control group, p < .01
Longitudinal correlations differed by group for prosocial orientation, with caregivers (r = .25, CI = [−.11, .55]) having lower relative stability than controls (r = .58, CI = [.43, .70]) in terms of who was highest to lowest on prosocial orientation (see Table 2). Combined with the mean increase in prosocial orientation, this relative instability meant that some caregivers experienced a larger increase in prosocial orientation than others, with 42% (CI = [26%, 59%]) of caregivers experiencing a 1 SD increase, and 16% (CI = [7%, 33%]) experiencing a 2 SD increase (greater than values of 11% and 2% for controls, Zs ≥ 2.98, ps ≤ .002).
Among the non-interpersonal personality facets measured, both caregivers and controls showed evidence for stability, with no statistically significant differences between groups (see Table A2 of the Online Supplemental Materials). The average magnitude of mean changes was |d| = .10 (from −.24 to .27, all ps ns) for caregivers, and |d| = .08 (from −.17 to .18, all ps ns) for controls. The average longitudinal correlation was r = .67 (from .53 to .87, all ps < .002) for caregivers, and r = .69 (from .57 to .76, all ps < .001) for controls.
The number of interpersonal facets with hypothesized and observed group differences (3 of 4) exceeded the rate expected by chance (.05 × 4 facets = 0.20 facets by chance), p < .001. In summary, bereaved spousal caregivers were hypothesized and observed to experience changes in personality facets associated with social behavior.
Discussion
Bereaved spousal caregivers were more likely than controls to experience personality change, and these changes involved an increase in interpersonal orientation on facets spanning three domains of the Five Factor Model (Costa & McCrae, 1992), namely agreeableness, extraversion, and conscientiousness. In fact, 87% (CI: 75–99%) of bereaved caregivers experienced reliable personality change in at least one facet of personality (see Figure 1). Further, the average increase in interpersonal orientation was sizeable in magnitude, approximately ⅔-SD (see Table 2). Arguably, caregiver changes in agreeableness were most dramatic, with 2 in 5 caregivers experiencing more than a standard deviation increase in prosocial or courteous characteristics. Bereaved caregivers also experienced increased sociability, an extraversion facet, as well as increased dependability, a conscientiousness facet. As the first known study to examine personality changes during the caregiving-bereavement transition, our findings extend prior research (Braun et al., 2007; Kim et al., 2013; McCrae & Costa, 1993; Specht et al., 2011) by showing that interpersonal aspects of personality are sensitive to change during the caregiving-bereavement transitions.
This research has theoretical implications for understanding the impact of life transitions on personality development in the second half of life. Over the past several decades, the stability of personality has been subject to much debate (Roberts, 2009). It is now known that personality is relatively stable in the absence of major life perturbations, but potentially malleable in response to some types of life transitions involving health, relationships, and work (Roberts & Mroczek, 2008; Roberts, Walton, & Viechtbauer, 2006). Prior studies have found little (Specht et al., 2011) to no (McCrae & Costa, 1993) bereavement-related changes in personality. Those studies lumped together heterogeneous causes of death that may have affected personality in different ways and to different degrees (Caspi & Moffitt, 1993), neutralizing group-level effects. Our research suggests that when examining more uniform circumstances – participants were all spousal caregivers of patients with terminal lung cancer – bereavement-related personality changes are observable and can be sizeable and multifaceted.
In contrast to our finding of personality change, some areas of caregiver personality were more stable. For example, trait-level neuroticism may remain stable throughout the bereavement process, despite state-level changes in caregiver emotional distress (Braun et al., 2007). Similarly, findings for openness indicate that caregivers’ preferred styles of thinking are not modified during caregiving-bereavement transitions. Moreover, one aspect of interpersonal orientation, the nonantagonistic facet of agreeableness, also remained stable. Based on item content and criterion correlations of the interpersonal facets in past studies (Chapman, 2007; Saucier, 1998), this suggests that the caregiving-bereavement transition may reflect changes in affiliativeness and altruism more so than hostility and argumentativeness.
Although bereaved spousal caregivers were significantly more likely than controls to experience personality change, many controls were found to experience idiosyncratic personality changes. As a group, controls did not experience mean-level changes in any of the 13 NEO-FFI facets, indicating that while changes were common, the specific nature of change varied from participant to participant. Prior studies have not typically reported the percentage of participants experiencing reliable personality changes, though our results indicate this might be a fruitful area of research.
Future studies can build on these findings by examining the implications of caregiver personality change for family functioning and the grieving process. In the context of terminal illnesses, spousal caregivers are often emotionally burdened by the challenges of treatment decision-making and communicating with clinicians, other family members, and their ill spouses. Following the death of a spouse, widowed individuals must navigate social terrain without their partner. Changes in caregiver personality could complicate or ease these processes. As well, there is a need for research on the implications of personality change for prolonged grief (Prigerson et al., 2009). Further analyses of personality change following other somewhat homogeneous life transitions, such as unplanned early retirement or bereavement following suicide, accident, or sudden natural deaths are also warranted. Research is needed to understand how different types of life transitions affect personality continuity and change (Caspi & Moffitt, 1993).
This research also holds promise for informing interventions in the context of caregiving and other expectable (vs. unpredictable) life transitions. Existing theories of self-knowledge (Hoerger, Chapman, Epstein, & Duberstein, 2012; Wilson, 2009) suggest that people have a limited understanding of how they will be affected by future life transitions. Notably, while individuals acknowledge prior changes in personality, they seem to experience great difficulty imagining future personality change (Quoidbach, Gilbert, & Wilson, 2013). Yet, foreknowledge is instrumental for guiding planning and facilitating adjustment. In the same way that popular education about the “stages” or states of grief has helped many individuals (Maciejewski, Zhang, Block, & Prigerson, 2007), improving caregiver understanding of the potential effects of the caregiving-bereavement transition on personality could ease the adjustment of caregivers to their changing roles. Information about personality change could be embedded within health education materials or psychosocial interventions for caregivers to promote self-care (Hoerger et al., 2013; Maciejewski et al., 2007). Clinicians (psychologists, nurses, physicians) should be aware of the possibility of personality change in the context of the caregiving-bereavement transition.
This study had several strengths, chiefly the uniqueness of the data, the use of a well-validated measure of personality, and the case-control design. Nonetheless, as the first study to examine changes in the five established domains of personality during the caregiver-bereavement transition, there were several limitations. As with any study involving self-reports of personality, the observed changes could be influenced by motivation to see oneself in a particular light. Informant reports of personality have strengths and weaknesses (e.g., Hoerger et al., 2011) but could make a significant methodologic contribution to the burgeoning literature on personality change. Second, the present analyses could underestimate personality changes experienced by bereaved caregivers, as the power to detect significant effects was constrained by the total sample size (n = 124). Third, the investigation included two time points of observation separated by only 18 months and a control sample drawn from primary care. Multiwave studies and different controls (e.g., spouses with minimal roles in caregiving, spouses of terminal patients who survive the follow-up period) would be needed to quantify the duration of personality change and to determine whether change occurs steadily, cyclically, or suddenly, and whether changes are mainly due to the diagnosis of potentially life-limiting illness, the burdens of caregiving, or loss. For example, given that the initial assessment occurred after the patient’s diagnosis, it is possible that the process of personality change had begun by the time spouses were recruited into the study. (If that is the case, the present findings represent underestimates.) Calls for the inclusion of personality data in Electronic Medical Records (Chapman, Roberts, & Duberstein, 2011) and Medicare Welcome packets (Friedman et al., 2013), if heeded, could mitigate this problem in future research. Fourth, definitive mortality data were unavailable for the entire cohort, so while we cannot rule out the possibility that those opting to complete the follow-up were more likely than nonparticipants to become interpersonally oriented, we can definitely conclude that, at least, a subset of bereaved caregivers became decidedly more interpersonally oriented. Finally, with larger samples, future studies could explore whether findings are moderated by caregiver factors (e.g., amount of time spent with the patient, extent of other support, health) or whether there are reliable changes in the personality factor structure during the caregiving-bereavement transition.
In closing, this study makes an initial contribution to the rapidly expanding body of research on personality change. For decades, personality research arguably operated from a defensive posture, focusing on fending off criticisms about cross-situational consistency, behavioral prediction, and construct validity. Acknowledging countervailing views, researchers in the post-Mischelian era are now free to address more nuanced questions about the nature of personality change (Roberts, 2009). By providing preliminary evidence that spouses of terminally ill patients can experience personality changes during the caregiving-bereavement transition, our research consequently sparks curiosity about the mechanisms underlying personality change.
Conclusion
This preliminary study suggest that spousal caregivers of patients with terminal cancer experienced an increase in interpersonal orientation during the caregiver-bereavement transition, as demonstrated by personality change in aspects of extraversion, agreeableness, and conscientiousness. Further research examining the caregiving-bereavement transition and other life transitions (e.g., divorce, retirement, unemployment) in large samples could clarify how life transitions affect personality development.
Supplementary Material
Acknowledgments
FINANCIAL DISCLOSURE/FUNDING:
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: National Institute of Mental Health (T32MH018911, K07MH001135, R01MH061429), National Institute on Aging (K08AG031328), and National Cancer Institute (R01CA106370). The authors have no conflicts of interest.
Biographies
Dr. Hoerger is an assistant professor of psychology and psychiatry at the Tulane Cancer Center and adjunct assistant professor of psychiatry at the University of Rochester Medical Center.
Dr. Chapman is an associate professor of psychiatry at the University of Rochester Medical Center.
Dr. Prigerson is the co-director of the Center for End-of-Lie Research and a professor of geriatrics and sociology in medicine at the Weill Cornell Medical College.
Dr. Fagerlin is an associate professor of internal medicine at the University of Michigan Medical School.
Dr. Mohile is an associate professor of medicine at the University of Rochester Medical Center.
Dr. Epstein is the associate dean of education, evaluation, and research, and a professor of professor of family medicine, psychiatry, oncology, and nursing at the University of Rochester Medical Center.
Dr. Lyness is the senior associate dean for academic affairs and a professor of psychiatry at the University of Rochester Medical Center.
Dr. Duberstein is a professor of psychiatry and family medicine at the University of Rochester Medical Center.
Footnotes
DECLARATION OF CONFLICT OF INTEREST:
The author(s) declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
“Frequency matching” differs from “individual matching.” For frequency matching, the researcher ensures that samples match on the percentage of participants with various demographic characteristics, and uses independent-samples analyses. For individual matching, the researcher matches individual participants on all possibly relevant characteristics (using exact matching, propensity scores, etc.) and uses paired-sample or other dependent-sample analyses. We used frequency matching, for which conventional analyses are used. Rothman and colleagues (2009) provide an extensive discussion of these methods.
Contributor Information
Michael Hoerger, Tulane Cancer Center, New Orleans, LA, USA, University of Rochester Medical Center, Rochester, NY, USA.
Benjamin P. Chapman, University of Rochester Medical Center, Rochester, NY, USA
Holly G. Prigerson, Weill Cornell Medical College, New York, NY, USA
Angela Fagerlin, University of Michigan Medical School, Ann Arbor, MI, USA.
Supriya G. Mohile, University of Rochester Medical Center, Rochester, NY, USA
Ronald M. Epstein, University of Rochester Medical Center, Rochester, NY, USA
Jeffrey M. Lyness, University of Rochester Medical Center, Rochester, NY, USA
Paul R. Duberstein, University of Rochester Medical Center, Rochester, NY, USA
References
- Aldred H, Gott M, Gariballa S. Advanced heart failure: impact on older patients and informal carers. Journal of Advanced Nursing. 2005;49:116–124. doi: 10.1111/j.1365-2648.2004.03271.x. [DOI] [PubMed] [Google Scholar]
- Bergman EJ, Haley WE. Depressive symptoms, social network, and bereavement service utilization and preferences among spouses of former hospice patients. Journal of Palliative Medicine. 2009;12:170–176. doi: 10.1089/jpm.2008.0237. [DOI] [PubMed] [Google Scholar]
- Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: spouse caregivers. Journal of Clinical Oncology. 2007;25:4829–4834. doi: 10.1200/JCO.2006.10.0909. [DOI] [PubMed] [Google Scholar]
- Carr D. Death and dying in the contemporary United States: What are the psychological implications of anticipated death? Social and Personality Psychology Compass. 2012;6:184–195. [Google Scholar]
- Caspi A, Moffitt TE. When do individual differences matter? A paradoxical theory of personality coherence. Psychological Inquiry. 1993;4:247–271. [Google Scholar]
- Cerel J, Jordan JR, Duberstein PR. The impact of suicide on the family. Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2008;29:38–44. doi: 10.1027/0227-5910.29.1.38. [DOI] [PubMed] [Google Scholar]
- Chapman BP. Bandwidth and fidelity on the NEO-Five Factor Inventory: replicability and reliability of Saucier's (1998) item cluster subcomponents. Journal of Personality Assessment. 2007;88:220–234. doi: 10.1080/00223890701268082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Lyness JM, Duberstein P. Personality and medical illness burden among older adults in primary care. Psychosomatic Medicine. 2007;69(3):277–282. doi: 10.1097/PSY.0b013e3180313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Roberts B, Duberstein P. Personality and longevity: knowns, unknowns, and implications for public health and personalized medicine. Journal of Aging Research. 2011 doi: 10.4061/2011/759170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Shah M, Friedman B, Drayer R, Duberstein PR, Lyness JM. Personality traits predict emergency department utilization over 3 years in older patients. American Journal of Geriatric Psychiatry. 2009;17:526–535. doi: 10.1097/JGP.0b013e3181a2fbb1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Revised NEO personality inventory and NEO five factor inventory: Professional manual. Odessa, FL: Psychological Assessment; 1992. [Google Scholar]
- Friedman B, Veazie PJ, Chapman BP, Manning WG, Duberstein PR. Is personality associated with health care use by older adults? The Milbank Quarterly. 2013;91:491–527. doi: 10.1111/1468-0009.12024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PL, Turiano NA, Mroczek DK, Roberts BW. Examining concurrent and longitudinal relations between personality traits and social well-being in adulthood. Social Psychological and Personality Science. 2012;3:698–705. doi: 10.1177/1948550611433888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitchcock KM. Attachment and Caregiving in Adults: Global and Relationship-specific Patterns. ProQuest: 2008. [Google Scholar]
- Hoerger M, Chapman BP, Epstein RM, Duberstein PR. Emotional intelligence: A theoretical framework for individual differences in affective forecasting. Emotion. 2012;12:716–725. doi: 10.1037/a0026724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerger M, Chapman B, Ma Y, Tu X, Useda JD, Hirsch J, Duberstein P. Agreement between informant and self-reported personality in depressed older adults: What are the roles of medical illness and cognitive function? Psychology and Aging. 2011;26:1000–1006. doi: 10.1037/a0023213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerger M, Epstein RM, Winters PC, Fiscella K, Duberstein PR, Gramling R, Kravitz RL. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer. 2013;13 doi: 10.1186/1471-2407-13-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson NW, Roberts BW, Lodi-Smith J. Personality trait development and social investment in work. Journal of Research in Personality. 2012;46:334–344. doi: 10.1016/j.jrp.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kim Y, Carver CS, Schulz R, Lucette A, Cannady RS. Finding Benefit in Bereavement among Family Cancer Caregivers. Journal of Palliative Medicine. 2013 doi: 10.1089/jpm.2013.0049. [DOI] [PubMed] [Google Scholar]
- Kim Y, Duberstein PR, Sorensen S, Larson MR. Levels of depressive symptoms in spouses of people with lung cancer: effects of personality, social support, and caregiving burden. Psychosomatics. 2005;46:123–130. doi: 10.1176/appi.psy.46.2.123. [DOI] [PubMed] [Google Scholar]
- Löckenhoff CE, Duberstein PR, Friedman B, Costa PT. Five-factor personality traits and subjective health among caregivers: The role of caregiver strain and self-efficacy. Psychology and Aging. 2011;26:592. doi: 10.1037/a0022209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyness JM, Yu Q, Tang W, Tu X, Conwell Y. Risks for depression onset in primary care elderly patients: potential targets for preventive interventions. Am J Psychiatry. 2009;166:1375. doi: 10.1176/appi.ajp.2009.08101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejewski PK, Zhang B, Block SD, Prigerson HG. An empirical examination of the stage theory of grief. Journal of the American Medical Association. 2007;297:716–723. doi: 10.1001/jama.297.7.716. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Psychological resilience among widowed men and women: A 10-year follow-up of a national sample. In: Stroebe M, Stroebe W, Hansson R, editors. Handbook of bereavement. New York: Cambridge; 1993. pp. 196–207. [Google Scholar]
- McCrae RR, Kurtz JE, Yamagata S, Terracciano A. Internal consistency, retest reliability, and their implications for personality scale validity. Personality and Social Psychology Review. 2011;15:28–50. doi: 10.1177/1088868310366253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ownsworth T, Henderson L, Chambers SK. Social support buffers the impact of functional impairments on caregiver psychological well-being in the context of brain tumor and other cancers. Psycho-Oncology. 2010;19:1116–1122. doi: 10.1002/pon.1663. [DOI] [PubMed] [Google Scholar]
- Patrick JH, Hayden JM. Neuroticism, coping strategies, and negative well-being among caregivers. Psychology and Aging. 1999;14:273–283. doi: 10.1037//0882-7974.14.2.273. [DOI] [PubMed] [Google Scholar]
- Quoidbach J, Gilbert DT, Wilson TD. The end of history illusion. Science. 2013;339:96–98. doi: 10.1126/science.1229294. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, Maciejewski PK. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS medicine. 2009;6:e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW. Back to the future: Personality and Assessment and personality development. Journal of Research in Personality. 2009;43:137–145. doi: 10.1016/j.jrp.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a review of longitudinal studies. Psychological Bulletin. 2000;126:3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Mroczek D. Personality Trait Change in Adulthood. Current Directions in Psychological Science. 2008;17:31–35. doi: 10.1111/j.1467-8721.2008.00543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: a meta-analysis. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Robins RW, Fraley RC, Roberts BW, Trzesniewski KH. A longitudinal study of personality change in young adulthood. Journal of Personality. 2001;69:617–640. doi: 10.1111/1467-6494.694157. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Lippincott: 2008. [Google Scholar]
- Saucier G. Replicable item-cluster subcomponents in the NEO Five-Factor Inventory. J Personality Assessment. 1998;70:263–276. doi: 10.1207/s15327752jpa7002_6. [DOI] [PubMed] [Google Scholar]
- Shapiro ER. Grief in interpersonal perspective: Theories and their implications. 2001 [Google Scholar]
- Shear K, Shair H. Attachment, loss, and complicated grief. Developmental Psychobiology. 2005;47:253–267. doi: 10.1002/dev.20091. [DOI] [PubMed] [Google Scholar]
- Specht J, Egloff B, Schmukle SC. Stability and change of personality across the life course: The impact of age and major life events on mean-level and rank-order stability of the Big Five. Journal of Personality and Social Psychology. 2011;101:862. doi: 10.1037/a0024950. [DOI] [PubMed] [Google Scholar]
- Specht J, Egloff B, Schmukle SC. Examining Mechanisms of Personality Maturation The Impact of Life Satisfaction on the Development of the Big Five Personality Traits. Social Psychological and Personality Science. 2013;4:181–189. [Google Scholar]
- Wilson TD. Know Thyself. Perspectives on Psychological Science. 2009;4:384–389. doi: 10.1111/j.1745-6924.2009.01143.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.