Abstract
Objective
To construct a virtual space of common adolescent psychiatric disorders, spanned by factors reflecting major psychopathological dimensions, and locate psychiatric disorders in that space; examine whether the major psychopathological dimensions can be hierarchically organized; and determine the distribution of the latent scores of individuals in the space spanned by those dimensions.
Method
Exploratory factor analyses of data from the National Comorbidity Survey Adolescent Supplement (NCS-A) using the psychiatric diagnoses as indicators were used to identify the latent major psychopathological dimensions. The loadings of the disorders on those dimensions were used as coordinates to calculate the distance among disorders. The distribution of individuals in the space was based on the latent scores on the factors reflecting the major psychopathological conditions.
Results
A model with three correlated factors provided an excellent fit (Comparative Fit Index [CFI]=0.97, Tucker-Lewis Index [TLI]=0.95, the root mean squared error of approximation [RMSEA]=0.008) for the structure of disorders and a 4-factor model could be hierarchically organized, ultimately yielding a general psychopathology factor. Distances between disorders ranged from 0.079 (between social phobia and generalized anxiety disorder [GAD]) and 1.173 (between specific phobia and conduct disorder [CD]). At the individual level, there were 546 distinct liabilities observed (22% of all 2,455 potential liabilities).
Conclusion
A novel way of understanding psychiatric disorders in adolescents is as existing in a space with a limited number of dimensions with no disorder aligning along one single dimension. These dimensions are hierarchically organized, allowing for analyses at different levels of organization. Furthermore, individuals with psychiatric disorders present with a broad range of liabilities, reflecting the diversity of their clinical presentations.
Keywords: space of psychiatric disorders, latent structure of psychiatric disorders, psychiatric liability
Introduction
Publication of the DSM-51 and initiatives to develop alternative conceptualizations of psychopathology2 have stimulated renewed interest in the nosology of psychiatric disorders. This interest extends to a consideration of similarities and differences among disorders,3, 4 the structure of their relationships,5, 6 and reconciliation of the relatively low number of common psychiatric disorders with the diversity of patients’ clinical presentations.2 Providing an empirical basis to address these questions can advance research into shared and disorder-specific risk factors of mental disorders and investigations of their underlying neurobiology.4
Studies examining the latent structure of psychiatric disorders in children5, 7–9 and adults6, 10–15 have found that two to four underlying factors representing predispositions to internalizing or externalizing psychopathology explain well the patterns of co-occurrence of psychiatric disorders. However, to date, no study using a nationally representative sample has examined whether those factors can be further refined into lower order, more specialized factors or subsumed into a higher order, more general psychopathological factors. Those factors would represent fundamental, core dimensions of psychopathology that could be the target of etiological studies as well as preventive and treatment interventions.16, 17 Similarly, no national study has developed or applied a formal measure of the relationships among disorders,18 examined the distribution of latent liabilities for psychiatric disorders among individuals in the community, or investigated how variation in liabilities is related to the fundamental dimensions of psychopathology.
A recent study using the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) presented a new measure of similarity between psychiatric disorders by identifying a limited number of underlying dimensions.18 The authors assigned to each disorder a coordinate in each dimension based on the role that each dimension played in the occurrence of the disorder. Comparing the location of disorders to one another along these dimensions provided a formal measure of their proximity to one another and allowed for a visual representation of those distances. This proximity served as a multivariate measure of similarity among disorders, highlighted their interrelationships, and provided an intuitive way to represent those relationships. However, that study focused on adults and did not examine the distance among disorders or the distribution of liabilities among adolescents.
The onsets of several psychiatric disorders peak during adolescence.19 Moreover, adolescence is characterized by critical changes in neural systems that control higher cognitive functions including cognitive regulation of emotions, interpersonal and social judgment, and assessment of risk versus reward.20 To assess whether the structure of psychiatric disorders during this key neurodevelopmental period resembles the previously described structure of adult psychiatric disorders,18 we used data from a large, nationally representative sample of US adolescents, the National Comorbidity Survey Adolescent Supplement (NCS-A).9 A previous report indicated the latent structure of the lifetime comorbidity in the NCS-A sample included four factors, two representing internalizing disorders (fear and distress) and two representing externalizing (behavior and substance use) disorders.9 We sought to build on those findings by addressing four important, unanswered questions: 1) identifying the latent dimensions underlying 12-month common psychiatric disorders in adolescents; 2) developing a space of psychiatric disorders based on those dimensions; 3) investigating whether the dimensions could be hierarchically organized; and 4) examining the distribution of latent scores in the space spanned by those dimensions.
Method
Sample
The NCS-A is a nationally representative sample of US adolescents aged 13–18 years. Adolescents were interviewed between February 2001 and January 2004 in dual-frame household and school samples described elsewhere.21, 22 The household sample included 904 adolescents from households in the National Comorbidity Survey Replication (NCS-R).23 The household sample included school drop-outs and adolescents residing in areas where schools refused to participate. The school sample included 9,244 adolescents from a representative sample of schools. The conditional adolescent response rate was 86.8% for the household sample and 82.6% for the school sample.21, 22
One parent or surrogate of each participating adolescent was asked to complete a self-administered questionnaire about the adolescent’s developmental history and mental health. The conditional response rate was 82.5–83.7% (household and school samples respectively). This report focuses on the 6,483 adolescent–parent pairs with complete data for both adolescents and parents. Incomplete parent participation was taken into account by weighting procedures discussed in detail elsewhere.21, 22 The protocol was approved by human subjects committees of Harvard Medical School and the University of Michigan. The sample was weighted to be nationally representative on sociodemographic variables.21, 22
Diagnostic assessment
Adolescents were administered the Composite International Diagnostic Interview (CIDI), adapted for adolescents in their homes24 by professional lay interviewers from the Survey Research Center at the University of Michigan. Interviewers were extensively trained in administration of the CIDI and other procedures prior to their participation in the study. The CIDI assessed 12-month DSM-IV mood disorders (major depressive episode/dysthymia, mania/hypomania), anxiety disorders (panic disorder with or without agoraphobia, agoraphobia, social anxiety disorder, specific phobia, generalized anxiety disorder [GAD], posttraumatic stress disorder [PTSD], separation anxiety disorder), behavior disorders (attention-deficit/hyperactivity disorder [ADHD], oppositional defiant disorder [ODD], conduct disorder [CD]), eating disorders and substance use disorders (alcohol and drug abuse and dependence, nicotine dependence). Computer algorithms transformed responses from the CIDI interview into DSM-IV diagnoses.25
Adolescent interviews, which lasted an average of 2.5 hours, assessed each of these disorders.25 Parent questionnaires assessed only disorders for which parent reports have previously been found important in diagnosis: behavior disorders26 and depression/dysthymia.27 Because prior research has indicated that adolescents may be the most accurate informants concerning their emotional symptoms, only adolescent reports were used to assess diagnostic criteria for depression and anxiety disorders. By contrast, parent and adolescent reports were combined at the symptom level using an ‘or’ rule (except in the case of ADHD, where only parent reports were used based on evidence of low validity of adolescent reports), as both improve the validity of the diagnoses.9 A clinical reappraisal study indicated that concordance was good between survey and clinical diagnoses.28
Statistical Analyses
Identification of Dimensions and Location of Disorders
In accordance with previous work,18 we used exploratory factor analysis (EFA), using all disorders assessed in the NCS-A as indicators to identify the latent factors. Factor selection was guided by examination of fit indices and interpretability. Each factor was subsequently interpreted as a latent dimension. Those dimensions were used as axes to span a space that was subsequently used to calculate the distance between each disorder and each axis, as well as between all pairs of disorders.
The loadings of the disorders on the factors were used as the system of coordinates to locate each disorder in the space spanned by the factors. Larger positive values of the coordinates indicate stronger association of a disorder with that dimension, whereas negative values indicate an inverse association with the disorder. To estimate the proximity of two disorders, we calculated the distance between them as the square root of the sum of squares of their coordinates.29 Smaller distances indicate disorders that are closer together; larger distances indicate disorders further apart.
The default estimator for EFA was the weighted least squares (WLSMV), a robust estimator that does not assume normally distributed variables.30 The fit indices used for model evaluation were the Comparative Fit Index (CFI), the Tucker–Lewis Index (TLI), and the root mean squared error of approximation (RMSEA). All analyses were conducted using Mplus 7.1 to correct estimates for the non-independence of the data and sampling weights resulting from the complex sample design of the NCS-A.30
Hierarchical models
Based on the results of the EFA, we fit a confirmatory higher-order factor model that incorporated successively broader dimensions of psychopathology. The fit indices used for model evaluation were the same as in the EFA.
Distribution of individual liability scores
While the loadings of the disorders on the factors provide information on the structure of psychopathology, they do not provide information on the distribution of individuals in the space of disorders. To provide this information, we used the factor score estimates (i.e. “liability scores”) of each individual on each factor and plotted those scores in the virtual space generated by the EFA. This scatterplot provides a graphical representation of the multivariate distribution of individual liabilities for the psychiatric disorders. Because the prevalence of psychiatric disorders varies by gender,31 we tested whether the mean liability scores also differed by gender.
The variability in the distribution of liability scores is bounded by the number of individuals with at least one disorder as well as by the number of possible combinations of disorders. Thus, we calculated the proportion of distinct liability scores actually relative to both. The number of theoretically possible scores (65,520) can be calculated as ΣC(x,16) where C represents the combinatorial operation and with x ranging from 0 to 16, i.e., all potential combinations of co-occurrence of disorders. Additional details about the statistical modeling are available on request.
Results
12-month prevalence of disorders and Identification of Dimensions
As previously reported,31 the NCS-A was broadly representative of the US population of adolescents aged 13 to 17 years. Females composed 51.1% of the sample. Non-Hispanic whites comprised the largest racial/ethnic group (55.7%), followed by Non-Hispanic blacks (19.3%), Hispanics (18.9%) and others (6.1%). There was a broad range of 12-month prevalence among the disorders examined. The most prevalent disorder was specific phobia (15.8%), followed by ODD (8.3%), social anxiety disorder (8.2%), major depressive disorder (MDD)/dysthymia (8.2%), ADHD (6.5%), drug use disorder (5.7%), CD (5.4%), nicotine dependence (5.1%), alcohol use disorders (4.7%), PTSD (3.9%), eating disorders (2.8%), mania/hypomania (2.1%), panic disorder (1.9%), agoraphobia (1.8%), separation anxiety disorder (1.6%), and GAD (1.1%).
The eigenvalues for the first five factors were 5.6, 2.4, 1.4, 1.2 and 1.1. Fit indices indicated that one- and two-factor models had modest fit (CFI=0.81, TLI=0.78, RMSEA=0.017 and CFI=0.94, TLI=0.92, RMSEA=0.010), whereas models with three (CFI=0.97, TLI=0.95, RMSEA=0.008), four (CFI=0.99, TLI=0.97, RMSEA=0.006), and five (CFI=0.99, TLI=0.97, RMSEA=0.006) factors provided excellent and comparable fit (Table 1). In the three-factor model, factor 1 defined an internalizing dimension, whereas factor 2 subdivided into two externalizing factors, one of which had loadings for all externalizing disorders (i.e., a generalized externalizing factor), whereas the other had additional significant loadings for substance use disorders (i.e., substance-specific liability). The four-factor model was similar to the three-factor model but with the internalizing factor subdividing into two factors including one with loadings on the mood and eating disorders, PTSD, and separation anxiety disorder, and the other with loadings on the specific phobia, agoraphobia, social anxiety disorder, and panic disorder. In the four-factor model, the externalizing factor subdivided into a substance use disorder factor and a factor with loadings on ADHD, CD, and ODD. The five-factor model was similar to the four-factor model, but eating disorders had a large loading on the fifth factor. No other disorder had any meaningful loading on the fifth factor. Because the four-factor model is a refinement of the three-factor model but four dimensions cannot be represented graphically, we present the location of the disorders and the distribution of individuals in the space based on the three-factor model.
Table 1.
Exploratory Factor Analysis of Disorders in National Comorbidity Survey Replication Adolescent Supplement (NCS-A; N=6,483).
| 2- factor model | 3- factor model | 4- factor model | 5- factor model | |
|---|---|---|---|---|
| CFI | 0.94 | 0.97 | 0.99 | 0.99 |
| TLI | 0.92 | 0.95 | 0.97 | 0.97 |
| RMSEA | 0.010 | 0.008 | 0.006 | 0.006 |
| Disorders | Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDE/Dysthymia | 0.546 | 0.376 | 0.505 | 0.436 | 0.009 | 0.631 | 0.092 | 0.126 | 0.088 | 0.643 | 0.080 | 0.150 | 0.028 | 0.170 |
| GAD | 0.653 | 0.065 | 0.638 | 0.107 | 0.035 | 0.603 | 0.221 | 0.024 | −0.145 | 0.591 | 0.230 | −0.012 | −0.105 | −0.011 |
| Mania/Hypomania | 0.365 | 0.343 | 0.334 | 0.407 | −0.100 | 0.516 | −0.003 | 0.011 | 0.210 | 0.491 | 0.012 | 0.081 | 0.205 | −0.171 |
| Specific phobia | 0.580 | −0.082 | 0.568 | −0.019 | −0.128 | 0.297 | 0.447 | −0.165 | 0.059 | 0.300 | 0.455 | −0.146 | 0.068 | −0.111 |
| Agoraphobia | 0.668 | −0.156 | 0.674 | −0.126 | −0.007 | −0.020 | 0.934 | −0.018 | 0.029 | −0.035 | 0.921 | −0.022 | 0.046 | 0.129 |
| Social anxiety disorder | 0.572 | 0.082 | 0.569 | 0.099 | 0.078 | 0.284 | 0.441 | 0.103 | −0.010 | 0.268 | 0.463 | 0.119 | −0.022 | 0.287 |
| Panic disorder | 0.525 | −0.009 | 0.549 | −0.037 | 0.129 | 0.206 | 0.452 | 0.101 | −0.123 | 0.186 | 0.482 | 0.094 | −0.105 | −0.176 |
| Separation anxiety disorder | 0.702 | −0.122 | 0.675 | 0.002 | −0.361 | 0.912 | −0.008 | −0.492 | 0.015 | 0.939 | −0.010 | −0.500 | 0.020 | −0.003 |
| PTSD | 0.647 | 0.168 | 0.627 | 0.219 | −0.004 | 0.785 | 0.029 | 0.016 | −0.106 | 0.787 | 0.029 | 0.006 | −0.111 | −0.017 |
| Eating disorders | 0.390 | 0.143 | 0.338 | 0.258 | −0.195 | 0.493 | −0.006 | −0.101 | 0.118 | 0.509 | −0.008 | −0.020 | 0.039 | 0.761 |
| ADHD | 0.046 | 0.430 | −0.039 | 0.572 | −0.360 | 0.052 | 0.022 | −0.125 | 0.754 | 0.020 | 0.014 | −0.030 | 0.890 | −0.376 |
| ODD | 0.109 | 0.701 | 0.028 | 0.803 | −0.226 | 0.359 | −0.162 | 0.097 | 0.612 | 0.358 | −0.177 | 0.207 | 0.544 | 0.057 |
| CD | 0.023 | 0.720 | −0.065 | 0.805 | 0.009 | −0.042 | 0.103 | 0.394 | 0.610 | −0.042 | 0.082 | 0.505 | 0.539 | 0.007 |
| Drug use disorders | −0.010 | 0.862 | 0.000 | 0.735 | 0.549 | 0.158 | −0.090 | 0.846 | 0.009 | 0.130 | −0.082 | 0.850 | −0.013 | −0.051 |
| Alcohol use disorders | −0.027 | 0.723 | −0.012 | 0.596 | 0.472 | 0.032 | 0.000 | 0.718 | 0.034 | 0.024 | −0.005 | 0.765 | 0.027 | −0.287 |
| Nicotine dependence | −0.001 | 0.790 | 0.014 | 0.671 | 0.445 | 0.029 | 0.049 | 0.741 | 0.107 | 0.006 | 0.049 | 0.787 | 0.055 | 0.083 |
| Factor correlations | ||||||||||||||
| 1.000 | 1.000 | 1.000 | 1.000 | |||||||||||
| 0.312 | 1.000 | 0.279 | 1.000 | 0.348 | 1.000 | 0.352 | 1.000 | |||||||
| 0.125 | −0.011 | 1.000 | 0.454 | 0.109 | 1.000 | 0.471 | 0.116 | 1.000 | ||||||
| 0.312 | 0.053 | 0.363 | 1.000 | 0.272 | 0.035 | 0.269 | 1.000 | |||||||
| −0.006 | −0.028 | 0.092 | 0.256 | 1.000 |
Note: Boldface values indicate loadings ≥0.4 or, if no loading is ≥0.4, highest loading of that disorder. ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; CFI = Comparative Fit Index; GAD = generalized anxiety disorder; MDE = major depressive episode; ODD = oppositional defiant disorder; PTSD = posttraumatic stress disorder; RMSEA = root mean squared error of approximation; TLI = Tucker-Lewis Index.
Based on these results, the three- and four-factor EFA models were further evaluated using CFA in order to build the hierarchical models. The 3-factor EFA model had significant cross loadings between the 2nd and 3rd “externalizing” factors, which did not suggest simple structure, whereas the four-factor model distinctly separated the factors into simple structure. Fixing all non-bolded values in Table 1 to zero, the CFA for the four-factor model had a slightly better fit (CFI=0.96, TLI=0.95, RMSEA=0.008) than the three-factor model (CFI= 0.94, TLI=0.93, RMSEA=0.010). We used the four-factor CFA model to build higher-order hierarchical models. Data on the distribution of individual liabilities based on the four-factor model are available on request.
Coordinates and Distance between Disorders
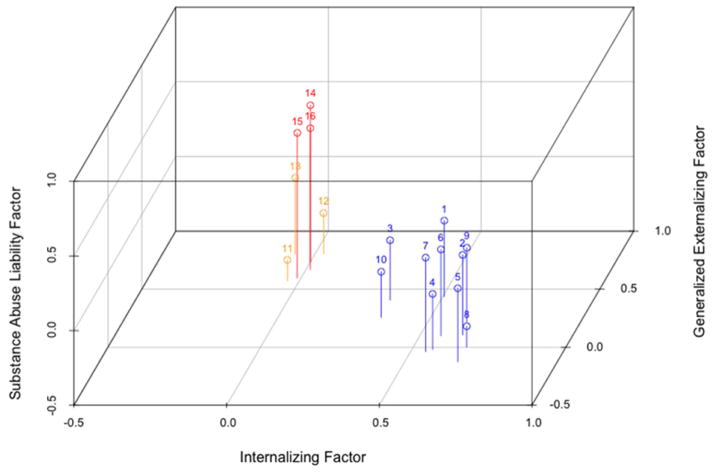
The coordinates for each disorder can be derived from Table 1. In the three-factor model, graphically represented in Figure 1, the coordinates for GAD are 0.638, 0.107, and 0.0035, whereas for nicotine dependence, they are respectively 0.014, 0.671 and 0.445. There was broad variation in the pattern of coordinates. Some disorders, such as GAD and CD, had coordinates with large values in one dimension but low in the others. Other disorders, such as drug use disorders, had coordinates with moderate to large values in more than one dimension.
Figure 1.
Three-dimensional representation of the space of common psychiatric disorders in the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) using the 3-factor exploratory factor analysis (EFA) model. Note: 1. Major depressive episode/dysthymia; 2. generalized anxiety disorder; 3. mania/hypomania; 4. specific phobia; 5. agoraphobia (with/without panic disorder); 6. social anxiety disorder; 7. panic disorder; 8. separation disorder; 9. posttraumatic stress disorder; 10. eating disorder; 11. Attention-deficit/hyperactivity disorder; 12. oppositional defiant disorder; 13. conduct disorder; 14. drug use disorder; 15. alcohol use disorder; 16. nicotine dependence.
Table 2 presents the Euclidian distance between all pairs of disorders in the three-factor model. Because Euclidian distances are symmetric, only the cells below the matrix diagonal are presented. Although there was a wide range of distances between pairs of disorders, from social anxiety disorder and GAD (0.079) to specific phobia and CD (1.173), the overall pattern indicated that disorders traditionally considered within the same group and included in the same DSM-IV chapter (e.g., drug use disorders and alcohol use disorders) tended to have smaller distances separating them than did disorders considered less similar such as GAD and nicotine dependence. The correlation between distances calculated using the 3-factor model and 4-factor model (available on request) was 0.89, indicating that the location of disorders in the space did not substantially depend on dimensionality.
Table 2.
Euclidian Distances Among Psychiatric Disorders in the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) in the 3-Factor Model
| Disorders | MDE/Dys | GAD | Mania/HypoM | SP | AG | SocAD | PD | SEP | PTSD | ED | ADHD | ODD | CD | DUD | AUD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MDE/Dys | |||||||||||||||
| GAD | 0.321 | ||||||||||||||
| Mania/HypoM | 0.222 | 0.401 | |||||||||||||
| SP | 0.459 | 0.234 | 0.424 | ||||||||||||
| AG | 0.539 | 0.228 | 0.562 | 0.186 | |||||||||||
| SocAD | 0.335 | 0.079 | 0.391 | 0.237 | 0.230 | ||||||||||
| PD | 0.481 | 0.207 | 0.507 | 0.257 | 0.177 | 0.151 | |||||||||
| SEP | 0.542 | 0.403 | 0.497 | 0.248 | 0.378 | 0.442 | 0.495 | ||||||||
| PTSD | 0.217 | 0.117 | 0.327 | 0.291 | 0.335 | 0.166 | 0.314 | 0.406 | |||||||
| ED | 0.354 | 0.398 | 0.175 | 0.321 | 0.491 | 0.387 | 0.470 | 0.379 | 0.359 | ||||||
| ADHD | 0.679 | 0.852 | 0.474 | 0.781 | 0.954 | 0.834 | 0.913 | 0.779 | 0.791 | 0.468 | |||||
| ODD | 0.591 | 0.855 | 0.458 | 0.863 | 1.017 | 0.845 | 0.955 | 0.875 | 0.768 | 0.550 | 0.293 | ||||
| CD | 0.586 | 0.845 | 0.479 | 0.885 | 1.013 | 0.817 | 0.912 | 0.961 | 0.771 | 0.598 | 0.428 | 0.241 | |||
| DUD | 0.693 | 0.868 | 0.721 | 1.002 | 1.038 | 0.821 | 0.879 | 1.173 | 0.832 | 0.857 | 0.929 | 0.776 | 0.555 | ||
| AUD | 0.632 | 0.774 | 0.628 | 0.883 | 0.925 | 0.719 | 0.763 | 1.066 | 0.750 | 0.743 | 0.836 | 0.730 | 0.513 | 0.162 | |
| ND | 0.605 | 0.781 | 0.613 | 0.900 | 0.948 | 0.733 | 0.793 | 1.069 | 0.744 | 0.744 | 0.820 | 0.684 | 0.467 | 0.119 | 0.089 |
Note: ADHD=attention-deficit/hyperactivity disorder; AG=agoraphobia (with/without panic disorder); AUD=alcohol use disorder; CD=conduct disorder; DUD=drug use disorder; ED=eating disorder; GAD=generalized anxiety disorder; Mania/HypoM=mania or hypomania; MDE/Dys=major depressive episode/dysthymia; ND=nicotine dependence; ODD=oppositional defiant disorder; PD=panic disorder; PTSD=posttraumatic stress disorder; SEP=separation disorder; SocAD=social anxiety disorder; SP=specific phobia.
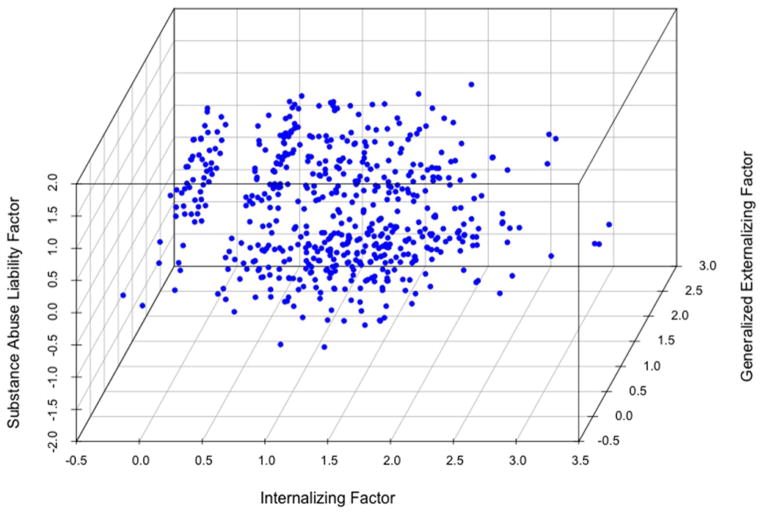
Distribution of individuals in the space of disorders
Of the 6,483 participants in the NCS-A, 2,454 had at least one psychiatric disorder, indicating that there could be at most 2,455 different liabilities (since individuals with no disorders would all have the same liability). Women had higher average scores on the internalizing factor (0.22 versus 0.04, p<.001), and on the substance abuse liability factor (0.06 versus 0.02, p<.005). There were no differences in the general externalizing factor (0.19 versus 0.20, p=.5). When examining the distribution of liabilities, we found 546 different liabilities, representing 22% (546/2455) of all potential liabilities among individuals in the sample (Figure 2), but only 0.83% (546/65520) of all theoretically possible liabilities.
Figure 2.
Factor scores of 6,483 participants in the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), derived from the 3-factor exploratory factor analysis (EFA) model.
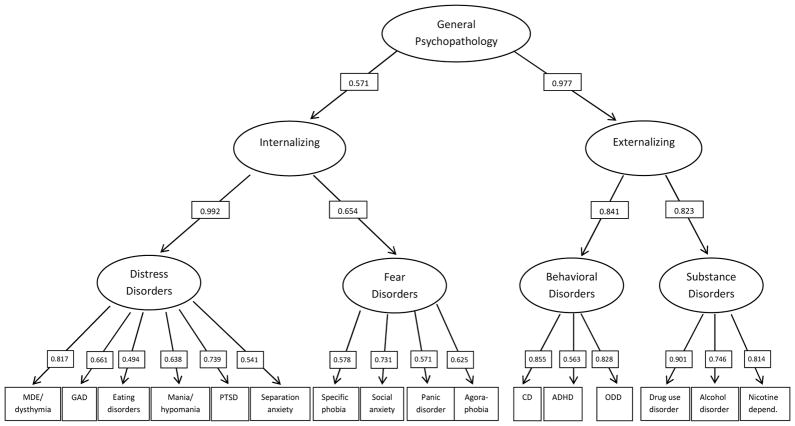
Hierarchical model
A CFA subsuming the four factors identified in the EFA into two higher-order factors, one representing the internalizing dimension and the other representing the externalizing dimension, provided a good fit (CFI=0.96, TLI=0.95, RMSEA=0.008). These two correlated factors could equivalently be used to identify a third-order model with one general psychopathology factor (Figure 3).
Figure 3.
The hierarchical structure of common psychiatric disorders in adolescence. Note: ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; GAD = generalized anxiety disorder; MDE = major depressive episode; ODD = oppositional defiant disorder; PTSD = posttraumatic stress disorder.
Discussion
This is the first study to use a formal measure of similarity of proximity between disorders in a nationally representative sample of adolescents, and to examine the distribution of liability to psychiatric disorders in that sample. We found that interrelationships among 12-month psychiatric disorders were well described by three or four correlated dimensions representing different facets of underlying internalizing and externalizing dimensions. When the factors were used to span a space and their loadings used as the coordinates in that space, disorders included in the same DSM-IV diagnostic classes tended to have smaller distances among themselves than from disorders in other chapters. The factors could be organized hierarchically, yielding progressively more general dimensions of psychopathology. Furthermore, representation of individuals of the sample in the space revealed a broad diversity of individual liabilities.
The dimensions identified were similar to those found in previous studies in adults18 and adolescents,9, 32 including an analysis of the lifetime comorbidity in this sample,9 although in contrast to most prior analyses, we identified two externalizing factors, one more substance use-related and the other more closely related to disruptive behaviors.33 Using a recently developed approach, we used the loadings to obtain estimates of the relative importance of each dimension for each disorder and to create a space in which psychiatric disorders could be placed.18 In accordance with previous results in adults,34 no disorder was perfectly aligned in one dimension. Instead, each disorder was better understood from the perspective of a multidimensional space similar to that of the mood circumplex concept that provides a multidimensional structure of emotion.35 As a result, although disorders were generally located near those in the same DSM-IV chapter, some relationships, such as the proximity between mania/hypomania and eating disorders, crossed chapters. This association is consistent with the suggestion that bipolar and eating disorders are pathophysiologically related conditions.36, 37
A novel finding of our study was that the four latent dimensions could be subsumed into progressively higher-order factors, suggesting that psychopathology may be viewed as including at least four different levels of organization, from disorder to the more general psychopathology factor. These complementary levels of organization capture different levels of abstraction and may be appropriate for different clinical and research purposes.17 For example, specific diagnostic categories may be useful for clinicians confronting therapeutic choices for individual patients, whereas higher order dimensions may be preferable for etiological or treatment research.
A second novel finding was that when considering the number of individuals with at least one disorder, there was a broad distribution of liability scores, reflecting diversity in the individual-level combination of observed disorders. Furthermore, most adolescents had liabilities across all factors, although individuals greatly varied with respect to the dimension with the highest liability. However, when considering all the theoretically possible liabilities, less than 1% were actually realized. Taken together, our findings may help reconcile the tension between dimensional and categorical (i.e., diagnosis-based) approaches to psychopathology and between the relatively restricted number of diagnostic entities and the broad variety and complexity of clinical presentations. At the same time, even the diversity of observed presentations represents only a fraction of all theoretical presentations, suggesting that clinical presentations tend to follow certain predetermined patterns of aggregation.
The results have nosological, etiological, and clinical implications for adolescent psychiatric disorders. From the nosological point of view, the latent structure of psychiatric disorders from adolescence onward appears to be well described by a limited number of underlying correlated dimensions corresponding to internalizing and externalizing predispositions that have a long history in child and adolescent psychiatric nosology.38 The results are also in line with findings in adults indicating that no disorder is perfectly aligned along one dimension, but rather that each disorder represents a defined level of a broader space.18, 34 Longitudinal studies should examine whether the correlation between the internalizing and externalizing dimensions are a result of an initial shared liability that progressively differentiates over time or a consequence of disorders in one dimension causing disorders in other dimensions.
From an etiological perspective, the resemblance of latent dimensions in adolescence and adulthood suggests temporal continuity in the structure of disorders. The brain circuits, psychological structures, and vulnerabilities underlying the common disorders appear to be relatively well defined by adolescence,19, 20 although their strength and interrelationships can vary over developmental stages.39–41 An important direction for future research will be to identify brain circuits that are central to the broad latent structures and the genetic and environmental factors that lead to abnormalities in the structure or function of these circuits using a developmental perspective. The hierarchical organization of psychopathology also suggests that there will be disruptions in some brain circuits or environmental conditions that serve as risk factors at the level of broad structures, whereas others will be specific to discrete disorders.42 The application of the methods described in this study to a range of biological measures at multiple levels may also help advance new initiatives for improved classification and treatment of psychiatric disorders.2, 43–45
From a clinical perspective, knowledge of the proximity among adolescent psychiatric disorders may help narrow differential diagnoses or prompt consideration of potential comorbidities, especially disorders that are closely located and therefore likely to co-occur. An understanding of proximity among disorders can also help inform treatment development and prevention strategies. Disorders that are more closely related are more likely to share risk factors or psychopathological mechanisms. Furthermore, because different risk factors are likely to act at different levels of psychopathology,17 interventions that address risk factors that act at the broader, more general level may have the greatest impact at ameliorating comorbid disorders or decreasing liability to future closely related psychiatric disorders. Finally, because there appears to be continuity in the latent structure of disorders between adolescence and adulthood,6, 11, 18 interventions that prevent or treat psychopathology in adolescents may decrease the risk of psychiatric disorders in adults.
Our study should be understood in the context of several limitations. First, the school-level response was relatively low, and the sample excluded adolescents not enrolled in school, which may reduce the external validity of the findings. Second, diagnoses were based on structured interviews, rather than on clinical assessments, although prior methodological work has shown good concordance of the interviews with clinical diagnoses.28 Third, the assessment of psychiatric disorders, while broad, was not exhaustive. Some disorders with childhood or adolescent onset, such as obsessive-compulsive disorder and autism, were not included in this study. Fourth, the assessments were cross-sectional. Replication of the analyses in prospective samples would be informative. Fifth, some categories (e.g., eating disorders, drug use disorders) had to be presented in aggregate to allow for stable estimates. Larger sample sizes may allow for the location of finer-grained categories. Sixth, although this analysis helps reconcile the existence of a limited number of underlying liabilities and diagnostic categories with the diversity of clinical presentations, it does not address the existence of heterogeneity within each diagnostic category.
Despite these limitations, this study advances our understanding of the structure of psychiatric disorders. Our study suggests that a novel way of understanding psychiatric disorders in adolescents is as existing in a space with a limited number of dimensions with no disorder aligning along one single dimension. These dimensions are hierarchically organized, allowing for analyses at different levels of organization. Furthermore, young people with psychiatric disorders present with a broad of range of liabilities, reflecting the diversity of their clinical presentations. This information may be useful in reconciling categorical and dimensional approaches to psychiatric diagnoses of adolescents and suggesting new avenues for etiological and treatment research.
Acknowledgments
The National Comorbidity Survey (NCS) Adolescent Supplement and the larger program of related NCS surveys are supported by grant U01-MH60220 from NIMH. Work on this manuscript was supported by National Institutes of Health (NIH) grants DA019606, DA023200, MH0760551 and MH082773 (C.B.), and the New York State Psychiatric Institute (C.B., M.O.). The sponsors had no additional role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Dr. Wall, Ms. He, and Ms. Jin served as the statistical experts for this research.
Disclosure: Drs. Blanco, Wall, Krueger, Olfson, Burstein, Merikangas, and Ms. He and Ms. Jin report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Carlos Blanco, New York State Psychiatric Institute/Columbia University, New York City.
Dr. Melanie M. Wall, New York State Psychiatric Institute/Columbia University, New York City.
Ms. Jian-Ping He, Division of Intramural Research Programs, National Institute of Mental Health (NIMH), Bethesda, MD.
Dr. Robert F. Krueger, University of Minnesota, Minneapolis.
Dr. Mark Olfson, New York State Psychiatric Institute/Columbia University, New York City.
Ms. Chelsea J. Jin, New York State Psychiatric Institute/Columbia University, New York City.
Dr. Marcy Burstein, Division of Intramural Research Programs, National Institute of Mental Health (NIMH), Bethesda, MD.
Dr. Kathleen R. Merikangas, Division of Intramural Research Programs, National Institute of Mental Health (NIMH), Bethesda, MD.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Insel TR, Cuthbert BN, Garvey MA, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 3.Cross-Disorder Group of the Psychiatric Genomics Consortium. Smoller JW, Craddock N, et al. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–1379. doi: 10.1016/S0140-6736(12)62129-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blanco C, Rubio J, Wall MM, Wang S, Jiu CJ, Kendler KS. Risk factors for anxiety disorders: Common and specific effects in a national sample. Depress Anxiety. 2014;31:756–64. doi: 10.1002/da.22247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: generating new hypotheses. J Abnorm Psychol. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- 6.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 7.Lahey BB, Rathouz PJ, Van Hulle C, et al. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. J Abnorm Child Psychol. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- 8.Wittchen HU, Beesdo-Baum K, Gloster AT, et al. The structure of mental disorders re-examined: Is it developmentally stable and robust against additions? Int J Methods Psychiatr Res. 2009;18:189–203. doi: 10.1002/mpr.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kessler RC, Avenevoli S, McLaughlin KA, et al. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Psychol Med. 2012;42:1997–2010. doi: 10.1017/S0033291712000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 11.Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 12.Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112:437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- 13.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Ormel J, Petukhova M, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- 16.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farmer RF, Seeley JR, Kosty DB, Olino TM, Lewinsohn PM. Hierarchical organization of axis I psychiatric disorder comorbidity through age 30. Compr Psychiatry. 2013;54:523–532. doi: 10.1016/j.comppsych.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blanco C, Krueger RF, Hasin DS, et al. Mapping common psychiatric disorders: structure and predictive validity in the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 20.Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9:947–957. doi: 10.1038/nrn2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Avenevoli S, Costello EJ, et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009;18:69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Avenevoli S, Costello EJ, et al. National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design. J Am Acad Child Psy. 2009;48:380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalaydjian A, Swendsen J, Chiu WT, et al. Sociodemographic predictors of transitions across stages of alcohol use, disorders, and remission in the National Comorbidity Survey Replication. Compr Psychiatry. 2009;50:299–306. doi: 10.1016/j.comppsych.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Merikangas KR, Avenevoli S, Costello EJ, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. J Am Acad Child Psy. 2009;48:367–379. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnston C, Murray C. Incremental validity in the psychological assessment of children and adolescents. Psychol Assess. 2003;15:496–507. doi: 10.1037/1040-3590.15.4.496. [DOI] [PubMed] [Google Scholar]
- 27.Braaten EB, Biederman J, Dimauro A, et al. Methodological complexities in the diagnosis of major depression in youth: an analysis of mother and youth self-reports. J Child Adolesc Psychopharmacol. 2001;11:395–407. doi: 10.1089/104454601317261573. [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Avenevoli S, Green JG, et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Psy. 2009;48:386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leon S. Linear algebra with applications. Upper Saddle River, NJ: Prentice Hall; 2004. [Google Scholar]
- 30.Muthen LK, Muthen BO. Mplus User’s Guide. 7. Los Angeles: Muthen and Muthen; 1998–2012. [Google Scholar]
- 31.Kessler RC, Avenevoli S, Costello EJ, et al. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry. 2012;69:372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Behrendt S, Wittchen HU, Hofler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: Is early onset associated with a rapid escalation? Drug Alcohol Depend. 2009;99:68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 33.Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: an integrative quantitative model of the adult externalizing spectrum. J Abnorm Psychol. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roysamb E, Tambs K, Orstavik RE, et al. The joint structure of DSM-IV Axis I and Axis II disorders. J Abnorm Psychol. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russell JA, Barrett LF. Core affect, prototypical emotional episodes, and other things called emotion: dissecting the elephant. J Pers Soc Psychol. 1999;76:805–819. doi: 10.1037//0022-3514.76.5.805. [DOI] [PubMed] [Google Scholar]
- 36.McElroy SL, Frye M, Hellemann G, et al. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. J Affect Disord. 2011;128:191–198. doi: 10.1016/j.jad.2010.06.037. [DOI] [PubMed] [Google Scholar]
- 37.McElroy SL, Kotwal R, Keck PE, Jr, Akiskal HS. Comorbidity of bipolar and eating disorders: distinct or related disorders with shared dysregulations? J Affect Disord. 2005;86:107–127. doi: 10.1016/j.jad.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Achenbach TM. The classification of children’s psychiatric symptoms: A factor-analytic study. Psychol Monogr. 1966;80:1–37. doi: 10.1037/h0093906. [DOI] [PubMed] [Google Scholar]
- 39.Wegbreit E, Cushman GK, Puzia ME, et al. Developmental Meta-Analyses of the Functional Neural Correlates of Bipolar Disorder. JAMA Psychiatry. 2014;71:926–935. doi: 10.1001/jamapsychiatry.2014.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menon V. Developmental pathways to functional brain networks: emerging principles. Trends Cogn Sci. 2013;17:627–640. doi: 10.1016/j.tics.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 41.Gee DG, Humphreys KL, Flannery J, et al. A Developmental Shift from Positive to Negative Connectivity in Human Amygdala-Prefrontal Circuitry. J Neurosci. 2013;33:4584–4593. doi: 10.1523/JNEUROSCI.3446-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ridenour TA, Meyer-Chilenski S, Reid EE. Developmental momentum toward substance dependence: Natural histories and pliability of risk factors in youth experiencing chronic stress. Drug Alcohol Depend. 2012;123:S87–98. doi: 10.1016/j.drugalcdep.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Academy of Sciences. Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 44.Mirnezami R, Nicholson J, Darzi A. Preparing for precision medicine. N Engl J Med. 2012;366:489–491. doi: 10.1056/NEJMp1114866. [DOI] [PubMed] [Google Scholar]
- 45.National Institute of Mental Health. [Accessed 08/30/2013];The National Institute of Mental Health Strategic Plan. http://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml. Published August 2008.