Abstract
The impact of the bifurcation angle (BA) between the left main (LM) and the main branch on clinical outcomes after single stenting has never been documented. Therefore, the aim of this study was to investigate the impact of the BA on clinical outcomes after single cross-over LM to left anterior descending artery (LAD) stenting. A total of 170 patients who underwent percutaneous coronary intervention (PCI) in unprotected LM bifurcation with successful single cross-over stenting from the LM into the LAD were enrolled. The main vessel angle between the LM and the LAD was computed in end-diastole before PCI with three-dimensional (3D) quantitative coronary angiography (QCA) software. The patients were classified into three groups according to tertiles of the main vessel angle. The cumulative incidence of major adverse cardiac event (MACE: cardiac death, myocardial infarction, any revascularization including target lesion revascularization) rates throughout a 12-month period were compared between the three groups. Baseline patient characteristics were not a significant difference between the three groups. Compared to the high angle group, the low angle group had a significantly higher incidence of MACE (p = 0.041). In conclusion, this study revealed that low BA between the LM and the LAD had an adverse clinical impact after single cross-over LM to LAD stenting.
Keywords: Coronary artery disease, left main bifurcation lesion, bifurcation angle, percutaneous coronary intervention, three-dimensional quantitative coronary angiography
Introduction
Percutaneous coronary intervention (PCI) for unprotected left main coronary artery (ULMCA) disease is a technically challenging procedure. However, reduction in clinical restenosis with drug-eluting stents (DES), PCI with DES implantation has been shown to be a feasible and safe approach at clinical follow-up [1-4].
In the last few years, the largest trial, the SYNTAX (Synergy Between PCI With TAXUS and Cardiac Surgery) trial, which compared PCI and coronary artery bypass graft surgery (CABG) for treating patients with previously untreated three-vessel or ULMCA, reported that major adverse cardiac or cerebrovascular events (MACE) at 1 year were higher in the PCI group because of an increased rate of repeat revascularization [5].
Previous studies have reported that PCI for distal bifurcation lesions in ULMCA was associated with inferior clinical outcomes than was ostial, mid-shaft lesions in ULMCA, largely because there is a higher need for repeat revascularization in distal lesions [6]. Klaus et al. reported that a true bifurcation lesion was an independent predictor for in-stent restenosis on the outcome of the LMCA itself after DES implantation [7].
Recently, a number of studies have reported on the importance of bifurcation angles (BA) in predicting the immediate procedural success or the long-term outcome [8]. There was also a study that predicted that distal BA are affected by cardiac motion in left main bifurcation lesions with a three-dimensional (3D) QCA algorithm [9,10]. The latest 3DQCA software has been reported to have higher reproducibility in calculating the real BA than 2D QCA which has several limitations due to foreshortening and vessel overlap [11-13]. However, the studies reporting on BA in LM lesions were largely on the distal BA. The relationship of the main vessel angle between the LM and the left anterior descending artery (LAD) and clinical outcomes has never been documented. The purpose of this study was to investigate the impact of this angle with a 3D QCA algorithm on clinical outcomes after cross-over single stent strategy.
Materials and methods
Study population
A total of 170 patients with stable coronary artery disease were enrolled in this study from January 2006 to May 2011. PCI for de novo ULM bifurcation lesions was performed in the case of recurrent angina with the development of significant coronary stenosis in Kokura Memorial Hospital. This study was conducted to investigate the impact of the BA on clinical outcomes after cross-over single stent strategy from LM to LAD in LM bifurcation lesions. Treatment strategy of the side branch (SB) was dependent on the operator’s discretion. Procedural success was defined as a composite of the following: residual diameter stenosis < 30% of the main vessel, thrombolysis in myocardial infarction (TIMI) flow grade 3 in all branches. We excluded patients in whom a bail-out second stent in SB. Stent type and devices were used at the operator’s discretion. For the purpose of this study, we analyzed the cine-angiograms of 170 patients who underwent PCI of the LM bifurcation. The study was approved by the hospital’s ethics committee and conducted in accordance with the Declaration of Helsinki.
BA analysis method
BA parameters were computed in end-diastole before PCI with a validated program of 3D angiographic analysis [11-13]. We defined the angle between the LM and the LAD as the Main vessel angle [14]. Other types of BA are presented in accordance with the European Bifurcation Club consensus document [15]; the distal BA was delineated between the LAD and the left circumflex artery (LCX), whereas the proximal BA was defined as the angle between the LM and the LCX (Figure 1). 3D images required two different cine-angiograms, which were separated by more than 30 degrees. 3D reconstruction was performed offline by two experienced operators with the Cardiovascular Angiography Analysis System (CASS) 5, 3-D QCA software (CAAS 5 version 5.9.2, Pie Medical BV, Maastricht, The Netherlands) [16].
Figure 1.
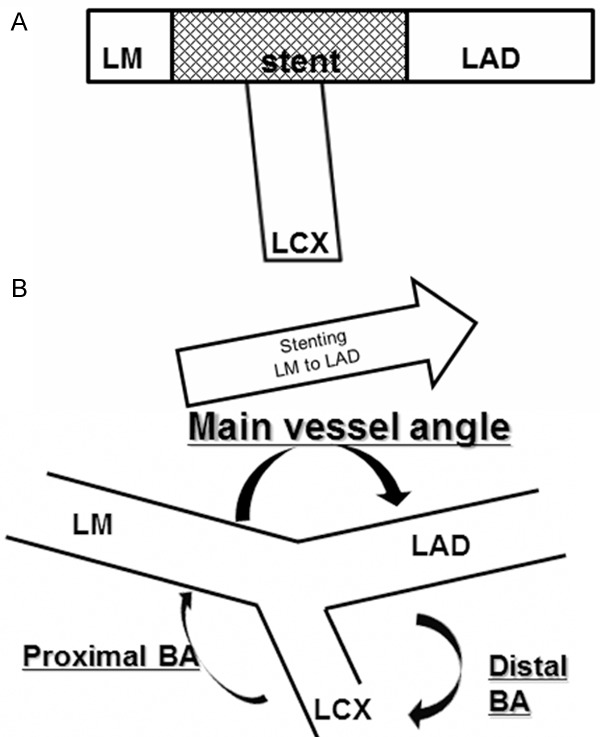
Bifurcation angle analysis. Percutaneous coronary intervention (PCI) was performed single cross-over stenting from the left main (LM) into the left anterior descending artery (LAD) (A). Bifurcation angle (BA) parameters were computed in end-diastole before PCI with 3D QCA software. Three BA ware defined as follows; the main vessel angle is defined as the angle between the LM and the LAD, the distal BA is delineated between the LAD and the left circumflex (LCX), whereas the proximal BA is defined as the angle between the LM and the LCX (B).
Study design
The patients were followed from January 2006 to May 2012. The average follow-up period was 894 ± 596 days (range, 14-365 days).
The primary endpoint was the cumulative incidence of MACE, that is, cardiac death, myocardial infarction (MI) including fatal/non-fatal MI, and any repeat revascularization including target lesion revascularization (TLR), onto the main vessel and, or side branch. MI was defined as elevated cardiac enzymes (CK-MB) above the upper limit of the normal range with ischemic symptoms or electrocardiography findings indicative of ischemia not related to the index procedure. The predictors of MACE were also analyzed using logistic models.
3D reconstruction was performed before PCI. To evaluate the effect of the main vessel angle on the LM bifurcation angulation and clinical outcome, patients were stratified into three groups according to tertiles of the main vessel angle in end-diastolic frames, and the incidence of MACE was analyzed.
Statistical analysis
Continuous data was expressed as the mean ± SD and compared between groups by unpaired Student t tests. Categorical variables were presented as counts and, or percentages; comparisons were performed with the chi-square test. The cumulative probability of MACE was estimated using the Kaplan-Meier method and compared among three groups divided with the tertile of pre-PCI main vessel angle with a log-rank test. The relationship between all parameters and the incidence of MACE was also investigated using Cox’s proportional hazards model. Independent predictors of 1-year MACE were sought among variables significant beyond the level of p = 0.05 in univariable analysis. Statistical analyses were performed using Stat View-J 5.0. All reported p-values were 2-sided, and p < 0.05 was regarded as statistically significant.
Results
Baseline characteristics
A total of 170 patients with LM bifurcation lesions were enrolled and were analyzed by 3D QCA. The baseline clinical characteristics were well matched between the 3 groups (Table 1). There were no significant differences in the angiographic and procedural characteristics between the 3 groups (Table 2). The median of the bifurcation angles were follows: main vessel angle; 141.4 degrees, distal BA; 86.3 degrees and proximal BA; 106.9 degrees. The patients were classified into three groups according to tertiles of the main vessel angle, which was defined as the low BA < 128.0 degree (n = 57), the middle BA = 128.0-151.6 degree (n = 57), and the high BA > 151.6 degree (n = 56) (Figure 2). Diastolic proximal BA was low in the high angle group. No difference was found between the 3 groups in the distribution of bifurcations based on the Medina classification. SYNTAX scores were well balanced between the 3 groups. The mean SYNTAX score in this study population was approximately 20 in all groups. The number of case with high SYNTAX scores was few in the 3 groups. There was no difference in the rate of the kissing balloon technique after stenting between the 3 groups.
Table 1.
Baseline clinical characteristics
| Low angle group (n = 57) | Middle angle group (n = 57) | High angle group (n = 56) | P value | |
|---|---|---|---|---|
| Mean age (years) | 70.9 ± 10.2 | 72.6± 9.6 | 72.1 ± 11.5 | 0.65 |
| Male (%) | 44 (77.2%) | 39 (68.4%) | 39 (69.4%) | 0.53 |
| Hypertention (%) | 37 (64.9%) | 37 (64.9%) | 40 (71.4%) | 0.70 |
| Diabetes Mellitus (%) | 21 (36.8%) | 20 (35.1%) | 19 (33.9%) | 0.69 |
| Dyslipidemia (%) | 28 (49.2%) | 23 (40.3%) | 28 (50%) | 0.52 |
| Current smoker (%) | 13 (22.8%) | 8 (14.0%) | 10 (17.9%) | 0.48 |
| Dialysis (%) | 6 (10.5%) | 5 (8.8%) | 5 (8.9%) | 0.94 |
| OMI (%) | 17 (29.8%) | 12 (21.1%) | 19 (33.9%) | 0.42 |
| Prior PCI (%) | 27 (47.4%) | 27 (47.4%) | 28 (50%) | 0.95 |
| Prior CAGB (%) | 3 (5.3%) | 1 (1.8%) | 0 | 0.17 |
| Emergency (%) | 5 (8.8%) | 6 (10.5%) | 5 (8.9%) | 0.94 |
| LVEF < 35% (%) | 3 (5.3%) | 4 (7.0%) | 4 (7.1%) | 0.87 |
| LM bifurcation + RCA | 15 (26.3%) | 16 (28.1%) | 11 (19.6%) | 0.61 |
| SYNTAX Score | 20.6 ± 4.8 | 21.2 ± 4.4 | 20.0 ± 3.8 | 0.36 |
| < 22 | 46 (80.7%) | 36 (63.2%) | 41 (73.2%) | 0.11 |
| 23-32 | 12 (21.1%) | 21 (36.8%) | 17 (30.4%) | 0.18 |
| > 33 | 3 (5.3%) | 2 (3.5%) | 0 | 0.24 |
Values are mean ± SD or n (%). OMI = old myocardial infarction; PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft; LVEF = left ventricular ejection fraction; LM = left main; RCA = right coronary artery; SYNTAX = Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery.
Table 2.
Angiographic and procedural characteristics
| Low angle group (n = 57) | Middle angle group (n = 57) | High angle group (n = 56) | P value | |
|---|---|---|---|---|
| Medina classification | 10 (17.5%) | 9 (15.8%) | 6 (10.7%) | 0.55 |
| 1, 1, 1 | 12 (21.1%) | 8 (14.0%) | 16 (28.6%) | 0.17 |
| 1, 1, 0 | 22 (38.6%) | 21 (36.8%) | 16 (28.6%) | 0.49 |
| 0, 1, 1 | 0 | 1 (1.8%) | 3 (5.4%) | 0.16 |
| 1, 0, 0 | 3 (5.3%) | 5 (8.9%) | 8 (14.3%) | 0.25 |
| 0, 1, 0 | 19 (33.3%) | 20 (35.1%) | 13 (23.2%) | 0.34 |
| 1, 0, 1 | 1 (1.8%) | 2 (3.5%) | 0 | 0.37 |
| Dimension of proximal LCX (mm) | 2.1 ± 0.4 | 2.2 ± 0.5 | 2.2 ± 0.7 | 0.75 |
| Reference diameter LAD/LCX ratio | 1.0 ± 0.3 | 0.9 ± 0.2 | 0.9 ± 0.6 | 0.92 |
| Bifurcation angles | ||||
| Diastolic distal BA | 84.4 ± 27.4 | 84.4 ± 23.6 | 88.1 ± 28.2 | 0.68 |
| Diastolic proximal BA | 110.8 ± 24.9 | 115.0 ± 26.3 | 95.7 ± 32.1 | 0.0008 |
| IVUS Guided | 40 (70.2%) | 39 (68.4%) | 38 (67.9%) | > 0.99 |
| Rotablation | 6 (10.5%) | 2 (3.5%) | 6 (10.7%) | 0.29 |
| Post- stenting KBT | 30 (52.6%) | 28 (49.1%) | 30 (53.6%) | 0.84 |
| Main vessel stent type | 0.06 | |||
| BMS | 22 (38.6%) | 10 ( 17.5%) | 13 (23.2%) | |
| SES | 16 (28.1%) | 10 (17.5%) | 12 (21.4%) | |
| PES | 7 (12.3%) | 8 (14.0%) | 11 (19.6%) | |
| ZES | 1 (1.8%) | 1 (1.8%) | 1 (1.8%) | |
| EES | 11 (19.3%) | 28 (49.1%) | 19 (33.9%) | |
| Total Stent Length (mm) | 20.2 ± 4.8 | 19.1 ± 4.7 | 21.6 ± 6.0 | 0.10 |
| Stent Diameter (mm) | 3.3 ± 0.3 | 3.3 ± 0.4 | 3.3 ± 0.3 | 0.37 |
Values are mean ± SD or n (%). LCX = left circumflex artery; LAD = left anterior descending artery; BA = bifurcation angle; IVUS = intravascular ultrasound; KBT = kissing balloon technique; BMS = bare-metal stent; SES = sirolimus-eluting stent; PES = paclitaxel-eluting stent; ZES = zotarolimus-eluting stent; EES = everolimus-eluting stent.
Figure 2.
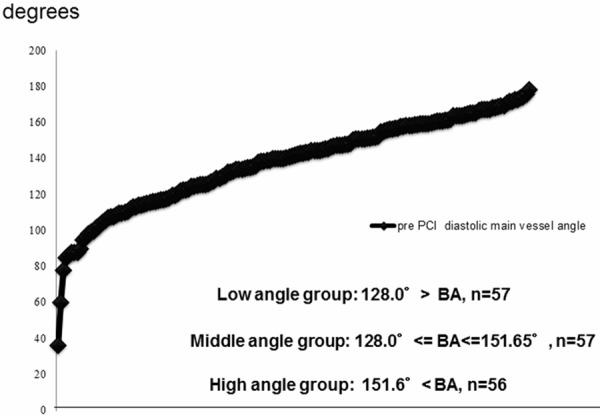
Main vessel angle values distribution. Median of the main vessel angle was 141.4 degree. The patients were classified into three groups according to tertiles of the main vessel angle. PCI = Percutaneous coronary intervention; LM = left main; LAD = left anterior descending artery; LCX = left circumflex; BA = bifurcation angle.
Impact of BA on MACE
The outcome data at 12 months is reported in Table 3. The TLR rate was higher in the lower BA group. Free survival rate from MACE using the Kaplan-Meier method and compared across the tertile values of the main vessel angle parameter with the log-rank test showed significant statistical difference between the three groups (p = 0.041). At 12 months, free survival rates from MACE was 66.7% in the low BA group, 85.7% in the middle BA group and 91.1% in the high BA group (Figure 3).
Table 3.
Major Adverse Cardiac Events at 12 month
| Low angle group (n = 57) | Middle angle group (n = 5) | High angle group (n = 56) | P value | |
|---|---|---|---|---|
| MACE | 19 (33.3%) | 8 (14.0%) | 5 (8.9%) | 0.0041 |
| cardiac death | 3 (5.3%) | 0 | 1 (1.8%) | > 0.99 |
| MI | 1 (1.8%) | 1 (1.8%) | 2 (3.6%) | > 0.99 |
| TLR | 15 (26.3%) | 8 (14.0%) | 3 (5.4%) | 0.016 |
Values are mean n (%). MACE = major adverse cardiac events; MI = myocardial infarction; TLR = target lesion revascularization.
Figure 3.
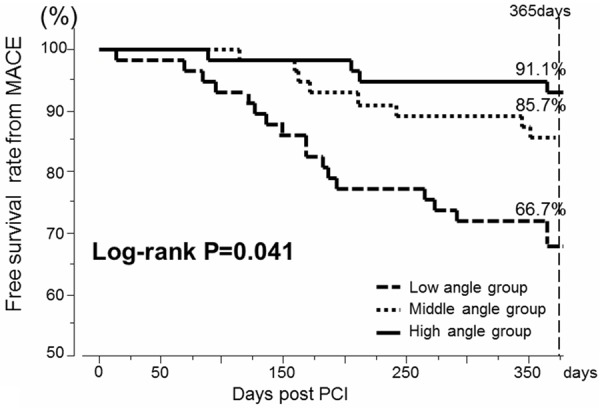
Cumulative free survival curves of MACE in three main vessel angle groups. The cumulative probability of MACE was estimated using the Kaplan–Meier method and compared among three groups divided with the tertile values of the main vessel angle parameter with the log-rank test. MACE = major adverse cardiac event; PCI = percutaneous coronary intervention.
Multivariate analysis in MACE
Based on the strong correlation between the main vessel angle parameters, a multivariate analysis of MACE prevalence was performed. At 12 months after PCI, multivariable analysis is reported in Table 4. Bare-Metal Stent (BMS) use (hazard ratio [HR], 3.9; 95% confidence interval [CI], 1.75-8.68, p = 0.0008) was an independent predictor of MACE. And a higher diastolic main vessel angle (HR, 0.99; 95% CI, 0.98-1.00, p = 0.048) and a bigger stent diameter (HR, 0.20; 95% CI, 0.07-0.55, p = 0.002) were found to be significantly associated with a lower incidence of 1-year MACE.
Table 4.
Predictive risk factors of MACE: multivariate analysis
| Multivariate | |||
|---|---|---|---|
|
|
|||
| HR | 95% CI | P value | |
| BMS use | 3.90 | 1.75-8.68 | 0.0008 |
| Diastolic main vessel angle | 0.99 | 0.98-1.00 | 0.048 |
| Diastolic distal BA | 0.99 | 0.97-1.00 | 0.10 |
| Diastolic proximal BA | 1.01 | 0.99-1.02 | 0.35 |
| Rotablation | 2.70 | 0.95-7.68 | 0.063 |
| Stent Diameter (mm) | 0.20 | 0.07-0.55 | 0.002 |
Values are mean ± SD or n (%). MACE = major adverse cardiac events; BA = bifurcation angle; BMS= bare-metal stent.
Discussion
This study is the first report on clinical outcome in patients undergoing coronary LM bifurcation PCI with single stent strategy from LM to LAD analyzed main vessel angle using 3D QCA. The use of BMS was the most significant predictive risk factor of MACE, however, several key results regarding BA were revealed.
The main findings of this study are as follows:
1) There is a large variation in the main vessel angle in LM bifurcation lesion;
2) MACE rates throughout 12 months after PCI are significantly affected by the pre-PCI main vessel angle values (p = 0.041);
3) The TLR rate is significantly higher in the lower BA group (p = 0.016), which suggests high dependence of MACE rate on the TLR rate.
Advantage of 3D QCA analysis
Recently, to provide solutions to the limitations associated with 2D QCA because of the vessel tortuosity, vessel overlap and foreshortening, 3D reconstruction software algorithms have been developed [17,18]. In terms of LM bifurcation, a 3D QCA algorithm was employed in a recent sub-study of the SYNTAX trial and its impact on mid and long term clinical outcome was described [9,10].
Impact of BA on outcome
The impact of distal BA on immediate procedural success or long-term outcome has been discussed in many studies. The outcome of the subgroups of the SYNTAX subgroup trial analysis, treated with single stent in LM bifurcation, did not differ across distal BA values [9]. However, there were no reports on main vessel angle after single stent strategy of bifurcation lesions.
In previous studies, the single stent technique with provisional side branch intervention was simple and is currently regarded as the standard technique for most bifurcation lesions [19,20]. Moreover, more alterations in the BA were observed after double stenting of bifurcation lesions than after single stenting [21]. In this study, we selected patients treated with the single-stent technique. To our knowledge, this is the first study of 3D QCA-derived angulation data analyzing MACE treated with cross-over single stent strategy from LM to LAD.
The bifurcation angulation pattern changes after stent implantation in the main vessel. Dobrin et al. reported that stent implantation caused straightening of the main vessel and significantly increased the angle between the main vessel and the main branch [22]. This has led us to believe that pre-procedural main vessel angle would have an impact on the clinical outcome after cross-over single stent strategy from LM to LAD in LM bifurcation lesions.
In this study, the TLR rate was significantly higher in the low pre-procedural main vessel angle group. We have estimated several mechanisms of a highly incidence of in-stent restenosis (ISR) in low BA including mechanical stress, flow biomechanics and pathological findings.
BA and mechanical stress
Several mechanisms are believed to the main factors of the results. One of them is stent fracture. Coronary stent fracture has been identified as one of the reasons for ISR, causes of which are proposed to be excessive mechanical stress due to extrinsic compression or extreme flexion of the vessel [23]. The BA is assumed to be one of the contributing factors of stent fracture vulnerability [24]. Ino et al. reported that the maximal angulation at the hinge points in the target lesion might play a role in stent fracture [25]. Even when not visible by angiography, the mechanical constraints might result in micro-fracture of the stent strut. Besides those mechanisms, it was reported that the angulation of the bifurcation plays an important role due to the degree of stent bending [26]. Several studies have suggested that stent fracture after sirolimus-eluting stent implantation cause a decrease in local drug delivery at the fracture site, resulting in binary restenosis [27-31]. In previous study assessed by optical coherence tomography, it was reported that in coronary bifurcation lesions, strut malapposition were frequent and severe at the level of the side branch origin and its hinge points at the bifurcation lesion that might play a role in the high incidence of TLR [32]. Another mechanism of TLR possibly associated with BA is stent recoil. Excessive mechanical stress on hinge point of the stent leads to stent recoil. We speculate that the degree of stent bending depends on the main vessel angle, treated with cross-over single stenting, and hence plays an important role in the mechanical stent recoil.
Flow biomechanics and pathological findings
Recent data generated from computational fluid dynamics (CFD) models suggest that the vascular geometry created by implanted stents cause local alterations in wall shear stress (WSS) or endothelial shear stress (ESS) related neointimal hyperplasia [33]. It had been proposed that low WSS or low ESS and elevated WSS gradients are associated with neointimal hyperplasia. Thus, theoretically deleterious variations in WSS distribution may occur in stent deformation, leading to substantial degrees of foreshortening. A previous study suggested that stent strut angle influences cellular adhesion in vitro. La Disa et al. reported that the change in incident stent strut angle caused progressive degrees of stent foreshortening that increased the intrastrut area of the luminal surface exposed to low WSS and elevated WSS gradients [34]. Hence, progressive degrees of stent foreshortening were also associated with strut misalignment relative to the direction of blood flow as indicated by analysis of near–wall velocity vectors. A recent study found that stenting of the main branch lowered WSS on the vessel wall, especially downstream of the bifurcation [35]. Chen et al. discussed that local thrombosis may occur when the flow is reduced [36].
Pathology studies have shown that arterial branch points are foci of low shear and low flow velocity, and are sites predisposed to the development of atherosclerosis plaque and thrombus [37]. Yiannis S. et al. reported in vivo that low ESS induced endothelial discontinuity and accumulation of activated inflammatory cells, thereby augmenting the expression and elastolytic activity of extracellular matrix degrading proteases in the intima and shifting the balance with their inhibitors toward matrix breakdown [38]. Moreover, previous in vitro experimental bifurcation models demonstrated that deployment of stents can alter boundary layer separation of the lateral wall, producing disturbances at the carina, especially at larger angles of bifurcation, causing greater turbulence [39].
Our data demonstrated the impact of 3D pre-procedural main vessel angle on 1-year outcomes of post PCI stenting LM to LAD patients for LM bifurcation lesions. In this study, 3D QCA analysis may provide new insight into LM bifurcation lesions and may serve as an important tool for planning interventional procedures. The lower main vessel angle is, the steeper it is, consequently the greater the stent deformation to be implanted from the LM into LAD, and the lower the WSS on inner curve. Hence, all mechanical and bioengineering effects would be pronounced. In high and low shear stress areas that are supposed in low BA, platelet activation and stasis might be promoted, and these phenomena would possibly lead to increase rates of thrombosis and restenosis.
Study limitations
First, the angulation parameters calculated by 3D QCA software have some limitations. To use this software in this study, it was important during each procedure to take two separate images with the least overlap. This might have possibly induced a bias for BA parameters.
Second, the side branch, LCX, stenosis at follow-up was estimated visually, and operator bias must be taken into consideration. Planned revascularizations of the side branch could likely be underestimated.
Third, the number of patients in the present single-center study was too small to determine the cut-off value for the ratio and to adequately examine its relationship with other low incidental cardiac events. A large-scale study should therefore be performed to adequately evaluate the relationship between BA parameters and other low incidental cardiac events including cardiac death, MI etc.
Conclusion
The low pre-procedural main vessel angle had an adverse impact on clinical outcomes after single cross-over LM to LAD stenting.
Disclosure of conflict of interest
None to disclose.
References
- 1.Park SJ, Kim YH, Lee BK, Lee SW, Lee CW, Hong MK, Kim JJ, Mintz GS, Park SW. Sirolimus-eluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J Am Coll Cardiol. 2005;45:351–6. doi: 10.1016/j.jacc.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 2.Meliga E, Garcia-Garcia HM, Valgimigli M, Chieffo A, Biondi-Zoccai G, Maree AO, Cook S, Reardon L, Moretti C, De Servi S, Palacios IF, Windecker S, Colombo A, van Domburg R, Sheiban I, Serruys PW. Longest available clinical outcomes after drug-eluting stent implantation for unprotected left main coronary artery disease: the DELFT (Drug Eluting Stent for Left Main) registry. J Am Coll Cardiol. 2008;51:2212–9. doi: 10.1016/j.jacc.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Chieffo A, Magni V, Latib A, Maisano F, Ielasi A, Montorfano M, Carlino M, Godino C, Ferraro M, Calori G, Alfieri O, Colombo A. 5-year outcomes following percutaneous coronary intervention with drug-eluting stent implantation versus coronary artery bypass graft for unprotected left main coronary artery lesions: the Milan experience. JACC Cardiovasc Interv. 2010;3:595–601. doi: 10.1016/j.jcin.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Park DW, Kim YH, Yun SC, Lee JY, Kim WJ, Kang SJ, Lee SW, Lee CW, Kim JJ, Choo SJ, Chung CH, Lee JW, Park SW, Park SJ. Long-term outcomes after stenting versus coronary artery bypass grafting for unprotected left main coronary artery disease: 10-year results of bare-metal stents and 5-year results of drug-eluting stents from the ASAN-MAIN (ASAN Medical Center–Left Main Revascularization) registry. J Am Coll Cardiol. 2010;56:1366–75. doi: 10.1016/j.jacc.2010.03.097. [DOI] [PubMed] [Google Scholar]
- 5.Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW SYNTAX Investigators. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Engl J Med. 2009;360:961–72. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 6.Naganuma T, Chieffo A, Meliga E, Capodanno D, Park SJ, Onuma Y, Valgimigli M, Jegere S, Makkar RR, Palacios IF, Costopoulos C, Kim YH, Buszman PP, Chakravarty T, Sheiban I, Mehran R, Naber C, Margey R, Agnihotri A, Marra S, Capranzano P, Leon MB, Moses JW, Fajadet J, Lefevre T, Morice MC, Erglis A, Tamburino C, Alfieri O, Serruys PW, Colombo A. Long-term clinical outcomes after percutaneous coronary intervention for ostial/mid-shaft lesions versus distal bifurcation lesions in unprotected left main coronary artery: the DELTA Registry (drug-eluting stent for left main coronary artery disease): a multicenter registry evaluating percutaneous coronary intervention versus coronary artery bypass grafting for left main treatment. JACC Cardiovasc Interv. 2013;6:1242–9. doi: 10.1016/j.jcin.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Tiroch K, Mehilli J, Byrne RA, Schulz S, Massberg S, Laugwitz KL, Vorpahl M, Seyfarth M, Kastrati A ISAR-LEFT MAIN Study Investigators. Impact of coronary anatomy and stenting technique on long-term outcome after drug-eluting stent implantation for unprotected left main coronary artery disease. JACC Cardiovasc Interv. 2014;7:29–36. doi: 10.1016/j.jcin.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 8.Dzavik V, Kharbanda R, Ivanov J, Ing DJ, Bui S, Mackie K, Ramsamujh R, Barolet A, Schwartz L, Seidelin PH. Predictors of long-term outcome after crush stenting of coronary bifurcation lesions: importance of the bifurcation angle. Am Heart J. 2006;152:762–9. doi: 10.1016/j.ahj.2006.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Girasis C, Serruys PW, Onuma Y, Colombo A, Holmes DR Jr, Feldman TE, Bass EJ, Leadley K, Dawkins KD, Morice MC. 3-Dimensional bifurcation angle analysis in patients with left main disease: a substudy of the SYNTAX trial (SYNergy Between Percutaneous Coronary Intervention with TAXus and Cardiac Surgery) JACC Cardiovasc Interv. 2010;3:41–8. doi: 10.1016/j.jcin.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Girasis C, Farooq V, Diletti R, Muramatsu T, Bourantas CV, Onuma Y, Holmes DR, Feldman TE, Morel MA, van Es GA, Dawkins KD, Morice MC, Serruys PW. Impact of 3-dimensional bifurcation angle on 5-year outcome of patients after percutaneous coronary intervention for left main coronary artery disease: a substudy of the SYNTAX trial (synergy between percutaneous coronary intervention with taxus and cardiac surgery) JACC Cardiovasc Interv. 2013;6:1250–60. doi: 10.1016/j.jcin.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Green NE, Chen SY, Messenger JC, Groves BM, Carroll JD. Three-dimensional vascular angiography. Curr Probl Cardiol. 2004;29:104–42. doi: 10.1016/j.cpcardiol.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Wellnhofer E, Wahle A, Mugaragu I, Gross J, Oswald H, Fleck E. Validation of an accurate method for three-dimensional reconstruction and quantitative assessment of volumes, lengths and diameters of coronary vascular branches and segments from biplane angiographic projections. Int J Card Imaging. 1999;15:339–56. doi: 10.1023/a:1006322609072. [DOI] [PubMed] [Google Scholar]
- 13.Messenger JC, Chen SY, Carroll JD, Burchenal JE, Kioussopoulos K, Groves BM. 3D coronary reconstruction from routine single-plane coronary angiograms: clinical validation and quantitative analysis of the right coronary artery in 100 patients. Int J Card Imaging. 2000;16:413–27. doi: 10.1023/a:1010643426720. [DOI] [PubMed] [Google Scholar]
- 14.Elbasan Z, Akıllı RE, Kalkan GY, Şahin DY, Gür M, Caylı M. Predictors of failure of final kissing-balloon inflation after mini-crush stenting in non-left main bifurcation lesions: importance of the main-vessel angle. J Invasive Cardiol. 2013;25:118–22. [PubMed] [Google Scholar]
- 15.Louvard Y, Thomas M, Dzavik V, Hildick-Smith D, Galassi AR, Pan M, Burzotta F, Zelizko M, Dudek D, Ludman P, Sheiban I, Lassen JF, Darremont O, Kastrati A, Ludwig J, Iakovou I, Brunel P, Lansky A, Meerkin D, Legrand V, Medina A, Lefèvre T. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008;71:175–83. doi: 10.1002/ccd.21314. [DOI] [PubMed] [Google Scholar]
- 16.Onuma Y, Girasis C, Aben JP, Sarno G, Piazza N, Lokkerbol C, Morel MA, Serruys PW. A novel dedicated 3-dimensional quantitative coronary analysis methodology for bifurcation lesions. EuroIntervention. 2011;7:629–35. doi: 10.4244/EIJV7I5A100. [DOI] [PubMed] [Google Scholar]
- 17.Goktekin O, Kaplan S, Dimopoulos K, Barlis P, Tanigawa J, Vatankulu MA, Koning G, Tuinenburg JC, Mario CD. A new quantitative analysis system for the evaluation of coronary bifurcation lesions: Comparison with current conventional methods. Catheter Cardiovasc Interv. 2007;69:172–180. doi: 10.1002/ccd.20946. [DOI] [PubMed] [Google Scholar]
- 18.Ramcharitar S, Daeman J, Patterson M, van Guens RJ, Boersma E, Serruys PW, van der Giessen WJ. First direct in vivo comparison of two commercially available three-dimensional quantitative coronary angiography systems. Catheter Cardiovasc Interv. 2008;71:44–50. doi: 10.1002/ccd.21418. [DOI] [PubMed] [Google Scholar]
- 19.Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S, Niemelä M, Kervinen K, Jensen JS, Galløe A, Nikus K, Vikman S, Ravkilde J, James S, Aarøe J, Ylitalo A, Helqvist S, Sjögren I, Thayssen P, Virtanen K, Puhakka M, Airaksinen J, Lassen JF, Thuesen L Nordic PCI Study Group. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006;114:1955–61. doi: 10.1161/CIRCULATIONAHA.106.664920. [DOI] [PubMed] [Google Scholar]
- 20.Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, Bennett L, Holmberg S, Cotton JM, Glennon PE, Thomas MR, Maccarthy PA, Baumbach A, Mulvihill NT, Henderson RA, Redwood SR, Starkey IR, Stables RH. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010;121:1235–43. doi: 10.1161/CIRCULATIONAHA.109.888297. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan S, Barlis P, Dimopoulos K, La Manna A, Goktekin O, Galassi A, Tanigawa J, Di Mario C. Culotte versus T-stenting in bifurcation lesions: immediate clinical and angiographic results and midterm clinical follow-up. Am Heart J. 2007;154:336–343. doi: 10.1016/j.ahj.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 22.Vassilev D, Gil RJ. Relative dependence of diameters of branches in coronary bifurcations after stent implantation in main vessel--importance of carina position. Kardiol Pol. 2008;66:371–378. [PubMed] [Google Scholar]
- 23.Surmely JF, Kinoshita Y, Dash D, Matsubara T, Terashima M, Ehara M, Ito T, Nasu K, Takeda Y, Tanaka N, Suzuki T, Katoh O. Stent strut fracture- induced restenosis in a bifurcation lesion treated with the crush stenting technique. Circ J. 2006;70:936–938. doi: 10.1253/circj.70.936. [DOI] [PubMed] [Google Scholar]
- 24.Rathore S, Ball T, Nakano M, Kaplan A, Virmani R, Foerst J. Circumferential strut fracture as a mechanism of “crush” bifurcation restenosis. Am J Cardiol. 2013;111:770–773. doi: 10.1016/j.amjcard.2012.11.030. [DOI] [PubMed] [Google Scholar]
- 25.Ino Y, Kubo T, Kitabata H, Shimamura K, Shiono Y, Orii M, Okochi K, Sougawa H, Tanimoto T, Komukai K, Ishibashi K, Takarada S, Nakanishi H, Tanaka A, Kimura K, Hirata K, Mizukoshi M, Imanishi T, Akasaka T. Impact of hinge motion on in-stent restenosis after sirolimus-eluting stent implantation. Circ J. 2011;75:1878–1884. doi: 10.1253/circj.cj-10-1182. [DOI] [PubMed] [Google Scholar]
- 26.Ino Y, Toyoda Y, Tanaka A, Ishii S, Kusuyama Y, Kubo T, Takarada S, Kitabata H, Tanimoto T, Mizukoshi M, Imanishi T, Akasaka T. Predictors and prognosis of stent fracture after sirolimus-eluting stent implantation. Circ J. 2009;73:2036–2041. doi: 10.1253/circj.cj-09-0343. [DOI] [PubMed] [Google Scholar]
- 27.Aoki J, Nakazawa G, Tanabe K, Hoye A, Yamamoto H, Nakayama T, Onuma Y, Higashikuni Y, Otsuki S, Yagishita A, Yachi S, Nakajima H, Hara K. Incidence and clinical impact of coronary stent fracture after sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2007;69:380–386. doi: 10.1002/ccd.20950. [DOI] [PubMed] [Google Scholar]
- 28.Lee MS, Jurewitz D, Aragon J, Forrester J, Makkar RR, Kar S. Stent fracture associated with drug-eluting stents: Clinical characteristics and implications. Catheter Cardiovasc Interv. 2007;69:387–394. doi: 10.1002/ccd.20942. [DOI] [PubMed] [Google Scholar]
- 29.Okumura M, Ozaki Y, Ishii J, Kan S, Naruse H, Matsui S, Ishikawa M, Hattori K, Gochi T, Nakano T, Yamada A, Kato S, Motoyama S, Sarai M, Takagi Y, Ismail TF, Nomura M, Hishida H. Restenosis and stent fracture following sirolimus-eluting stent (SES) implantation. Circ J. 2007;71:1669–1677. doi: 10.1253/circj.71.1669. [DOI] [PubMed] [Google Scholar]
- 30.Yang TH, Kim DI, Park SG, Seo JS, Cho HJ, Seol SH, Kim SM, Kim DK, Kim DS. Clinical characteristics of stent fracture after sirolimus-eluting stent implantation. Int J Cardiol. 2009;131:212–216. doi: 10.1016/j.ijcard.2007.10.059. [DOI] [PubMed] [Google Scholar]
- 31.Umeda H, Gochi T, Iwase M, Izawa H, Shimizu T, Ishiki R, Inagaki H, Toyama J, Yokota M, Murohara T. Frequency, predictors and outcome of stent fracture after sirolimuseluting stent implantation. Int J Cardiol. 2009;133:321–326. doi: 10.1016/j.ijcard.2007.12.067. [DOI] [PubMed] [Google Scholar]
- 32.Tyczynski P, Ferrante G, Moreno-Ambroj C, Kukreja N, Barlis P, Pieri E, De Silva R, Beatt K, Di Mario C. Simple versus complex approaches to treating coronary bifurcation lesions: direct assessment of stent strut apposition by optical coherence tomography. Rev Esp Cardiol. 2010;63:904–14. doi: 10.1016/s1885-5857(10)70184-5. [DOI] [PubMed] [Google Scholar]
- 33.LaDisa JF Jr, Olson LE, Hettrick DA, Warltier DC, Kersten JR, Pagel PS. Axial stent strut angle influences wall shear stress after stent implantation: analysis using 3D computational fluid dynamics models of stent foreshortening. Biomed Eng Online. 2005;4:59. doi: 10.1186/1475-925X-4-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LaDisa JF Jr, Olson LE, Molthen RC, Hettrick DA, Pratt PF, Hardel MD, Kersten JR, Warltier DC, Pagel PS. Alterations in wall shear stress predict sites of neointimal hyperplasia after stent implantation in rabbit iliac arteries. Am J Physiol Heart Circ Physiol. 2005;288:2465–75. doi: 10.1152/ajpheart.01107.2004. [DOI] [PubMed] [Google Scholar]
- 35.Williams AR, Koo BK, Gundert TJ, Fitzgerald PJ, LaDisa JF Jr. Local hemodynamic changes caused by main branch stent implantation and subsequent virtual side branch balloon angioplasty in a representative coronary bifurcation. J Appl Physiol. 2010;109:532–540. doi: 10.1152/japplphysiol.00086.2010. [DOI] [PubMed] [Google Scholar]
- 36.Chen HY, Moussa ID, Davidson C, Kassab GS. Impact of main branch stenting on endothelial shear stress: role of side branch diameter, angle and lesion. J R Soc Interface. 2012;9:1187–93. doi: 10.1098/rsif.2011.0675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glagov S, Zarins C, Giddens DP, Ku DN. Hemodynamics and atherosclerosis. Insights and perspectives gained from studies of human arteries. Arch Pathol Lab Med. 1988;112:1018–31. [PubMed] [Google Scholar]
- 38.Chatzizisis YS, Baker AB, Sukhova GK, Koskinas KC, Papafaklis MI, Beigel R, Jonas M, Coskun AU, Stone BV, Maynard C, Shi GP, Libby P, Feldman CL, Edelman ER, Stone PH. Augmented expression and activity of extracellular matrix-degrading enzymes in regions of low endothelial shear stress colocalize with coronary atheromata with thin fibrous caps in pigs. Circulation. 2011;123:621–630. doi: 10.1161/CIRCULATIONAHA.110.970038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakazawa G, Yazdani SK, Finn AV, Vorpahl M, Kolodgie FD, Virmani R. Pathological Findings at Bifurcation Lesions. J Am Coll Cardiol. 2010;55:1679–87. doi: 10.1016/j.jacc.2010.01.021. [DOI] [PubMed] [Google Scholar]


