Abstract
Objective
Longitudinal studies of the role of community context in childhood obesity are lacking. The objective of this study was to examine associations of community socioeconomic deprivation (CSD) on trajectories of change in body mass index (BMI) in childhood and adolescence.
Methods
Data come from electronic health records on 163,473 children aged 3-18 residing in 1288 communities in Pennsylvania whose weight and height were measured longitudinally. CSD at the year of birth was measured using 6 census variables and modeled in quartiles. Trajectories of BMI within CSD quartiles were estimated using random effects growth-curve models accounting for differences by age, sex, race/ethnicity as well ascorrecting for non-constant residual variance across age groups.
Results
CSD was associated with higher BMI at average age (10.7 years) and with more rapid growth of BMI over time. Children born in communities with greater CSD had steeper increases of BMI at younger ages. Those born into the poorest communities displayed sustained accelerated BMI growth. CSD remained associated with BMI trajectories after adjustment for a measure of household socioeconomic deprivation.
Conclusions
Higher CSD may be associated with more obesogenic growth trajectories in early life. Findings suggest that individual-level interventions that ignore the effect of community context on obesity related behaviors may be less efficient.
INTRODUCTION
Despite vigorous efforts by researchers and policy makers, the childhood obesity epidemic persists with one in five children being overweight or obese (1). The cumulative effect of obesity on children’s and adolescents’ physical and mental health, social integration and academic achievement can be substantial and resonate into adulthood (2). Further, sustained weight loss is difficult to achieve; obese children and adolescents are more likely to become obese adults (3) who are at increased risk of early death from heart disease and obesity-related cancers (4). The obesity epidemic also carries a heavy economic burden due to escalating health care costs and loss of productivity (5).
Interventions targeting individual diet and physical activity have proven to be largely ineffective for promoting long-term change (6). One consistent theme in the literature is that changing energy balance-related behavior without regard to the larger social context is difficult and unlikely to be sustained (7).
This has led to an interest in finding modifiable social contextual determinants that may be the “causes of the causes” of obesity (8). A recent review has called for longitudinal studies of community factors across the life-course (9). The purpose of this study was to understand the obesogenic effects of the larger-scale community context within which individual behaviors and decisions unfold. More specifically, we examined associations of a summary scale of community socio-economic deprivation (CSD) on longitudinal BMI trajectories in a large population of Pennsylvania children. This measure does not permit the investigation of the role of separate dimensions of CSD, however, it does permit the investigation of CSD as a whole affects weight change throughout childhood and adolescence. Individual diet and physical activity are enabled or constrained by features of the environment which act as “risk regulators” (8) that alter the odds of healthy energy-balance behaviors. Therefore, understanding the role of community context is important for identifying policy levers that may point toward more effective population-level interventions. Further, community characteristics that enable healthy behaviors are promising intervention targets since structural changes to the environment are potentially more sustainable, cost effective, and may yield larger scale impacts (10).
Communities that are socioeconomically deprived exhibit a host of structural features linked to higher rates of obesity, such as inadequate access to healthy foods (11, 12), increased exposure to fast food restaurants (13), absence of recreational facilities and parks (14), as well as psychosocial hazards including physical dilapidation of buildings and sidewalks, and heightened social disorder and crime (15). We hypothesize that CSD is a risk regulator that increases exposure to a cluster of environmental features that promote positive energy balance (8). These factors may impact children and adolescents directly through physical activity and diet, as well as younger children, indirectly through parental behavior (16). We also hypothesize that the environment is likely to impact children differently by age; because younger children are less independent and therefore may be more exposed to the effects of their community context.
Most studies have either examined associations of CSD with obesity cross-sectionally (17, 18), assessed body mass index (BMI) change using only two time points, or had small numbers of children and or communities. To our knowledge, no study has investigated the longitudinal association of CSD with BMI growth trajectories throughout childhood and adolescence in a large number of diverse communities. Studying longitudinal BMI trajectories allows the identification of critical periods of increased vulnerability that may prove to be important for intervention (19). In this paper, we examined associations of CSD measured at year of birth on longitudinal growth trajectories of BMI in children residing in a 37-county area of Pennsylvania using electronic health records from the Geisinger Health System. We further investigated whether there are critical periods of heightened vulnerability and whether earlier excess weight gain is sustained during adolescence.
METHODS AND PROCEDURES
Study population
The Geisinger Health System consists of a network of providers in a 37-county area covering central and northeastern Pennsylvania. We obtained information from electronic health records on all children that visited their primary care provider during 2001 and 2012. These patients represent the general population in the region (20). Data collection is described in detail elsewhere (21). The study population consists of 163,473 children aged 3-18 years (523,674 visits) whose addresses could be geo- coded using ArcGIS software and who could be assigned a value of CSD for their year of birth. Each home address was assigned to one of 1288 communities, defined as townships or boroughs, in rural areas and census tracts in cities (20). Height and weight were measured longitudinally in the clinical setting. Using BMI for analysis while controlling for sex and age instead of age and sex standardized z- scores from CDC growth-norms has been recommended for longitudinal modeling because it is more sensitive to within-person change, produces more valid effect estimates and yields more interpretable results (22). Implausible BMI values, defined as 5 standard deviations above and below the median (23), were assumed to be mis-measurement or data entry errors and were deleted using the standard CDC SAS Program. Data were also obtained on sex, age, and race/ethnicity (non-Hispanic white, African American, Hispanic or other) and the source of payment.. To better understand the association between CSD and BMI, we also adjusted for household socioeconomic deprivation in an attempt to disentangle the endogenous relationship of community and household SES. A participant was considered as residing in a socioeconomic deprived household if he or she used one of 14 medical assistance programs to pay for three or more healthcare visits (21).
CSD was derived from a factor analysis of six U.S. Census indicators (proportion of the population with less than high school, unemployed, not in labor force, in poverty, receiving public assistance and households without a car) for the years 1990, 2000 and the 5-year estimates of the American Community Survey (ACS) for 2005-2009. To assign a unique CSD score to the child’s year of birth, we used linear interpolation for intercensal years. The distribution of all CSD scores was used to calculate quartiles that allow modeling non-linear associations with BMI across levels of increasing CSD (17, 18). Each child was assigned the quartile ranking of the CSD score for the year of birth. Those born before 1990 (18%) were assigned the 1990 score because some indicators were not available for 1980. We conducted a sensitivity analysis to assess whether this assignment affected our analysis.
Statistical analysis
The purpose of this study was to estimate associations of CSD with longitudinal BMI trajectories in children ages 3-18, while taking account of the nested structure of the data, addressing non- stationarity of residual variances across ages, and adjusting for potential individual and household confounders. Analysis methods have been previously reported (21). In brief, we use hierarchical mixed- effects regression to model the growth trajectories of BMI. Each model included random effects to capture unmeasured variability between BMI measures within and between children. In primary analyses, we did not include a random effect for community due to the high computational burden. We undertook a planned sensitivity analysis in a subset of communities. A random intercept for community did not change estimated parameters or standard errors. We also estimated three-level unconditional means models with no-covariates using all communities and found small intraclass correlation coefficients, indicating that most of the variability is within rather than between communities. This suggests that estimates from a two-level mixed effects model are unlikely to have biased standard error estimates.
The base model included fixed effects for age (centered at the population mean of 10.7 years), its second and third order terms and child-level random effects for the growth curve intercept, age and age age-squared. To control for sex-differences in BMI trajectories, the base model also contained fixed effects for the cross-products of all age terms and sex. This model also included race/ethnicity (African- American, Hispanic and other vs. non-Hispanic white) and its interactions with age. Three models are presented: Model 1 included the base model and the fixed effect of CSD on BMI at average age; Model 2 added interaction terms of age (linear, squared, and cubed) and CSD to evaluate if growth trajectories varied by CSD; and Model 3 added a surrogate measure of household socioeconomic deprivation to control for compositional effects. Models were evaluated for goodness of fit, normality of residuals, and homoscedasticity. Fit was also evaluated by comparing model regression lines to Lowess lines that were estimated using multiple bandwidths on added variable plots. Influential observations were detected using Cook’s distance; their deletion from the dataset did not affect results. All models were estimated in SAS (version 9.3) using the Proc Mixed procedure.
RESULTS
We are provided with data on 163,473 children with, on average, 3.2 observations per child (range 1-13) (Table 1). On average, children were at the 66th percentile of the 2000 CDC growth curve charts. The sample was sex balanced but, in accordance with the demographic features of this area of Pennsylvania was predominantly non-Hispanic white (91.3%). Although the percentages of African American (4.7%) and Hispanic (1.1%) children were small, due to the large sample size, we had data on substantial numbers of children in both groups (7700 and 1864, respectively). The mean (SD) age across all observations was 10.7 (4.8) years.
Table 1.
Descriptive statistics of children and visits that are included in the analysis, information from electronic health record, all children ages 3-18, 2001 - 2012
| Variable | N | Mean/Perc | (SD) | Range |
|---|---|---|---|---|
| BMI(a) percentile (Visits) | 65.86 | (28.99) | 1 - 100 | |
| BMI z-score (Visits) | 0.59 | (1.12) | −6.3-3.9 | |
| Age (years) (Visits) | 10.68 | (4.75) | 3-18 | |
| Age at first BMI, years | 8.86 | (5.05) | 3-18 | |
| Age at last BMI, years | 11.83 | (5.09) | 3-18 | |
| Sex (Children) | ||||
| Male | 81,266 | 50.32% | ||
| Female | 81,207 | 49.68% | ||
| Duration between 1st and last BMI, years |
297(b) | (0.01) | 0-11.1 | |
| Number of annual BMI measures for analysis |
3.2 | (2.41) | 1 - 13 | |
| Race/ethnicity (Children) | ||||
| Non-Hispanic White | 149,191 | 91.26% | ||
| Black | 7,700 | 4.71% | ||
| Hispanic | 1,864 | 1.14% | ||
| Other or missing | 4,718 | 2.89% | ||
| On Medical Assistance | 55,171 | 33.75% |
BMI: body mass index (kg/m2) percentile, according to CDC growth curves, children > 85th percentile are considered overweight, children > 95th percentile are considered obese
32.2% of children only had one observation
Table 2 presents selected results of models 1-3. Full model results are available in an online supplement. All main effects of age showed statistically significant associations with BMI (Table 2). Birth year CSD was significantly associated with higher BMI at the average age adjusting for sex and race/ethnicity (Table 2, model 1). The associations of CSD with BMI at average age demonstrated an exposure-effect relation across CSD quartiles, ranging from an average difference (compared to the first quartile reference group) of 0.14 BMI units in the second quartile to 0.23 in the most deprived communities (all p-values < 0.001).
Table 2.
Principal associations of CSD with BMI trajectories from growth-curve models, boys and girls aged 3-18 years
| MODEL 1(a) | MODEL 2 | MODEL 3 | ||||
|---|---|---|---|---|---|---|
| Fixed effects: |
Beta
Coefficient |
(SE) |
Beta
Coefficient |
SE |
Beta
Coefficient |
SE |
| Fixed Intercept | 19.7656*** | 0.0198 | 19.4465*** (e) |
0.0270 | 19.3615*** | 0.0274 |
| Age in years(b) | 0.8901*** | 0.0029 | 0.8280*** | 0.0046 | 0.8104*** | 0.0046 |
| Age2 | 0.0199*** | 0.0003 | 0.0206*** | 0.0005 | 0.0203*** | 0.0005 |
| Age3 | −0.0052*** | 5exp-5 | −0.0048*** | 8exp-5 | −0.0046*** | 8exp-5 |
| Community socioeconomic deprivation (CSD)(c), | ||||||
| CSD 2nd Q.(d) | 0.1360*** | 0.0162 | 0.4842*** | 0.0345 | 0.4423*** | 0.0345 |
| CSD 3rd Q. | 0.1812*** | 0.0168 | 0.5951*** | 0.0340 | 0.5310*** | 0.0341 |
| CSD 4th Q. | 0.2325*** | 0.0176 | 0.7113*** | 0.0337 | 0.6024*** | 0.0342 |
|
Age × CSD 2nd
Q. |
0.0726*** | 0.0059 | 0.0628*** | 0.0059 | ||
| Age × CSD 3rd Q. | 0.0716*** | 0.0058 | 0.0567*** | 0.0058 | ||
| Age × CSD 4th Q. | 0.0987*** | 0.0057 | 0.0729*** | 0.0058 | ||
|
Age2 × CSD 2nd
Q. |
−0.0011 | 0.0007 | −0.0014** | 0.0007 | ||
|
Age2 × CSD 3rd
Q. |
−0.0022*** | 0.0007 | −0.0027*** | 0.0007 | ||
|
Age2 × CSD 4th
Q. |
−0.0008 | 0.0006 | −0.0017** | 0.0007 | ||
|
Age3 × CSD 2nd
Q. |
−0.0006*** | 0.0001 | −0.0004*** | 0.0001 | ||
|
Age3 × CSD 3rd
Q. |
−0.0004*** | 0.0001 | −0.0003** | 0.0001 | ||
|
Age3 × CSD 4th
Q. |
−0.0005*** | 0.0001 | −0.0003** | 0.0001 | ||
|
Medical
Assistance |
0.5165*** | 0.0261 | ||||
|
Age × Medical
Assistance |
0.1095*** | 0.0045 | ||||
|
Age2 × Medical
Assistance |
0.0028*** | 0.0005 | ||||
|
Age3 × Medical
Assistance |
−0.0009*** | 0.0001 | ||||
| Random effects | ||||||
|
Level 1 residual
2 variance δ2 Ages 3-5 |
0.5521 | 0.00386 | 0.5519 | 0.00386 | 0.5517 | 0.00385 |
| Ages 5-8 | 0.8217 | 0.00741 | 0.8219 | 0.00741 | 0.8219 | 0.00741 |
| Ages 8 + | 1.7004 | 0.00588 | 1.7006 | 0.00588 | 1.6999 | 0.00588 |
|
Variance in child-
specific intercept (πoo) |
17.5362 | 0.00108 | 17.5087 | 0.07567 | 17.4618 | 0.07549 |
|
Variance in
random slope of age (π10) |
0.1785 | 0.001098 | 0.1775 | 0.00109 | 0.1763 | 0.00109 |
|
Variance of
random slope of age2 (π20) |
0.002037 | 0.00002 | 0.00204 | 0.00002 | 0.002035 | 0.00002 |
|
Overall model fit
(−2 log likelihood) |
2241302 | 2240956 | 2240070 | |||
|
Change in −2 log
likelihood |
346 | 886 | ||||
Mixed effects (multilevel) models estimated using full maximum likelihood. Level 1 residuals estimated separately for three age groups. All models contained a random intercept for each child along with fixed main effects of sex and race/ethnicity (black, Hispanic, and other, non- Hispanic white is reference), random slopes of age and age2, and fixed effects cross-products of all age terms with sex and race/ethnicity.
Age was centered at the overall population grand mean of 10.7 years. Therefore, the overall intercept represents the fixed estimate of BMI at the population average age, conditional on the random effects in the model.
First quartile of the CSD distribution is the reference group
CSD 2nd Q. (low-moderate), CSD 3rd Q. (moderate-high), CSD 4 Q. (highest), are the second, third and fourth quartiles of CSD, with ranges of [−1.77–0.51; 0.51–3.73; and 3.73 31.38] respectively. The reference group, CSD 1st Quartile (lowest) had a range of [−7.82–1.77].
**p-value < 0.001;**0.001 > p-value ≤ 0.05.
We next evaluated how CSD altered the average BMI trajectories by adding the interaction terms of CSD and age and its higher-order terms, (Table 2, model 2). Overall, adding the age and CSD cross-products improved model fit (difference in -2 log likelihood of model 1 and 2: 346 [DF=9, p-value < 0.001]) suggesting that average BMI trajectories differed across levels of CSD.
The cross-products of CSD with age were significant and positive for all quartiles (all p-values < 0.001). The cross-product of age and the highest quartile had the strongest coefficient, suggesting that on average, living in more deprived communities was associated with more rapid BMI growth, particularly at earlier ages. Cross-products between CSD and age-squared (quartile 3 only, p-value < 0.001) and age cubed (all quartiles, p-values <0.001) were significant and negative, pointing to a slowing of BMI growth in later years that was stronger in communities with intermediate values of CSD.
After adjustment by a surrogate measure for household socioeconomic deprivation (Table 2, model 3), CSD remained significantly associated with average BMI and BMI trajectories, although most associations were attenuated. Main effects of CSD decreased by up to 15%; the interactions of CSD with age decreased by up to 26% (all p-values < 0.001). All three interactions of CSD with age-squared increased slightly in strength (becoming significant or more negative with p-values of 0.043; <0.001; and 0.008 for each of the CSD quartiles included in the analysis). The negative interaction effects of CSD with age-cubed decreased in size (p-values <0.001, 0.006 and 0.012 respectively).
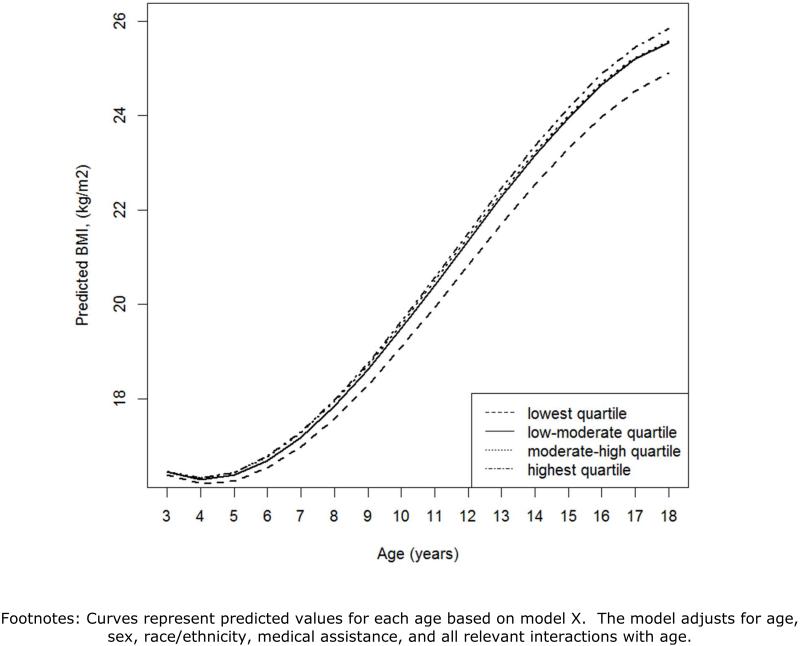
Figure 1 plots predicted BMI for children born into communities in the four categories of CSD. All children exhibited s-shaped growth curves of BMI from ages 3-18 years. In the least deprived places the average BMI growth trajectory began to accelerate between ages four and five, followed by a deceleration of BMI growth around age 15. The average BMI of children born into these communities was the lowest at all ages compared to children from communities with higher CSD. Children born into the middle two quartiles had trajectories that were similar to one another but were different from that of children in the lowest CSD quartile. Their BMI trajectory accelerated more rapidly after age four and increased more steeply leading to a difference of 0.66 BMI points at age 18 for children from the least deprived communities. At younger ages, children born into communities with the highest levels of CSD displayed a trend that was similar to those born into the second and third quartile. Their BMI trajectory however accelerated slightly more and decelerated later and less. At age 18 the highest CSD was 0.95 BMI points higher compared to children born into communities with the lowest CSD.
Figure 1.
Predicted BMI over age of Model 3, by quartile of community socioeconomic deprivation (CSD)
We conducted three sensitivity analyses. First, we evaluated whether assigning 1990 CSD scores to pre 1990-births affected the results by reproducing models only among children born after 1990. Overall, effects strengthened and inferences remained the same, suggesting that this was a conservative strategy for dealing with the unavailability of comparable census information. Second, we assumed that place-type (township, borough, census tracts), which was correlated with CSD was a proxy measure of CSD and not a common cause of CSD and faster BMI growth (a confounder). To assess the sensitivity of our results to this assumption we reran the analyses after including place-type; inferences did not change, and regression coefficients changed minimally. Finally, our approach for estimating birth year CSD depended on the stability of the measurement structure over time. Two of the six census variables displayed time trends that were at least partly due to policy changes resulting in fewer families on public assistance and higher rates of high school graduation, independent of whether community CSD had truly changed. We re-estimated models dropping these indicators from the CSD summary score. Without public assistance, inferences remained consistent in direction and magnitude. Results excluding percent adults with less than high school education resulted in an overall attenuation of associations, but the pattern of results remained consistent with the exception of one CSD by age interaction, which was no longer significant.
DISCUSSION
The goal of this study was to investigate how CSD influenced BMI trajectories during childhood and adolescence. Electronic health record data allowed us to cost-effectively assemble a large historical cohort of children residing in a large number of communities, using measured height and weight from clinical encounters over a decade. In addition, we linked data on children from a large geography that varied substantially across levels of CSD to assess the effect of the community environment. This is the largest, most comprehensive longitudinal investigation of the association between CSD and childhood and adolescent BMI trajectories to date.
Socioeconomic deprivation has been linked in cross-sectional studies to child BMI at multiple geographic scales, ranging from census tracts to states (24, 25). There are very few longitudinal studies of the effects of CSD on BMI and none that covers childhood and adolescence (26, 27). One longitudinal study by Oliver (26) using a sub-sample of children of the Canadian National Survey of Children and Youth evaluated associations of neighborhood income on children’s BMI during ages 2-10 years. The number of evaluated neighborhoods was not reported, children’s weight and height were self-reported by parents, and regression models did not allow for non-linear relations with age. The authors reported associations of neighborhood income with changes in BMI percentiles. Like our study, Greves Grow et al. (28) used electronic health records and US census data and found a cross-sectional association between risk of childhood obesity and median household income, rates of homeownership, and single parent households in census tracts in Kings County, WA. Further, an experimental study found that re-locating families into less deprived areas lead to lower BMIs (29). These studies were not able to evaluate longitudinal BMI trajectories during childhood and adolescence, a key feature of the present report. We observed that the association between CSD and BMI varied across the age span and by the degree of community deprivation. The initial acceleration in BMI growth was steeper in children living in higher CSD communities. After age 15, BMI trajectories of children born into communities in the middle quartiles of CSD were parallel to, but continued to be higher than, those of children born into the least deprived communities. On average, children born into communities with the highest CSD, evidenced continued divergence of the BMI trajectory throughout adolescence, compared to children in the lowest quartile of CSD. The data demonstrate that early life BMI increases associated with CSD can extend throughout adolescence. At age 18 the difference in average BMI of adolescents in the least and most deprived communities (0.95) is comparable in size to the most potent among 37 childhood obesity interventions reviewed in a recent meta-analysis (30).
This study is the first to show evidence for an age-graded effect of CSD on children’s BMI. We hypothesize that the impact of community context on BMI growth may be mediated through parental behaviors related to food purchasing and or physical activity. Prior literature suggests that CSD is associated with lower healthy food availability (31), and greater access to unhealthy food. The community food environment is hypothesized to influence food purchasing behavior and the availability of healthy foods in the home. In addition, high CSD communities have been found to provide fewer opportunities for outdoor play (14). Parents living in high CSD communities also have been found to restrict outdoor play due to safety concerns (17). Our results suggest that childhood and early adolescence may be periods of increased vulnerability to the impact of community socio-economic deprivation. Based on previous research, we believe that older adolescents may exercise more autonomy in their food and physical activity related behaviors, which is a candidate mechanism to explain our results. However, we are not able to assess the role of these mediating factors directly because we lack detailed longitudinal measures of diet or activity. One explanation for why the impact of high CSD communities persisted throughout adolescence is that these children may have fewer opportunities for travel and less exposure to different environments. Differences between BMI age- trajectories are biggest between the first and the second quartile suggesting that there might be a threshold effect with non-deprived communities being particularly protective.
CSD remained associated with BMI trajectories after adjustment for a surrogate for household socioeconomic deprivation. Several associations were partially attenuated suggesting that there may be a mix of contextual influences as well as compositional effects related to the selective migration of low- SES families to high-deprivation communities. Our findings mirror those of previous studies that found compositional as well as contextual effects of community deprivation on BMI (32). Because we used data from electronic health records, we lacked more detailed measures of family SES such as income or education. Medical Assistance is a means tested program; it should reasonably measure household deprivation, but may not be sensitive to the full range of SES. Residual confounding remains a possibility. Given the strength and consistency of the community-level associations after adjustment for medical assistance, compositional effects are unlikely to be driving these findings.
In the present study, we used the address that was given during a doctor’s visit and assumed that children were born at that address. It is possible that residential mobility resulted in misclassification of exposure. It is unlikely that residential mobility was differential by BMI status. Simulation studies have shown that unmeasured moving results in bias toward the null. These effects are likely to be minor; the population of central Pennsylvania has low rates of mobility and research suggests that families tend to move between communities that are comparable in terms of socioeconomic characteristics (33). It is possible that the stronger associations with CSD early in childhood reflect more precise measurement of CSD in early life. BMI in later life might be influenced by a cumulative effect of CSD over the life course or lagged effects of more recent CSD. Conceptualizing and modeling the effect of changing community context over time however is not straightforward since contextual effects are lagged in time, might be cumulative or follow other, more complicated functions. In the near future, we will explore the effect of current, lagged and cumulative measures of CSD to assess if and how changes in CSD over time affect BMI trajectories.
By using longitudinal data to model BMI trajectories throughout childhood and adolescence, this study was able to provide strong support for prior reported associations of community deprivation with obesity (28, 34, 35). Since Hill and Peters first described key features of the obesogenic environment (36) the study of the role of communities has remained inconclusive (9, 37, 38). CSD may hold promise as a target for obesity prevention. CSD is partly the consequence of policies that control zoning, economic development, housing, taxation and transportation. These policies, while not directly related to health, lead to structural conditions that regulate risk and facilitate healthy energy-balance related behaviors. They are also subject to change. The American Dietic Association (39) has called for multicomponent interventions that include community features to facilitate behavioral change. Our results suggest that addressing the community context within which individual behavior unfolds may yield more efficient and sustainable results. Individually-focused obesity prevention and treatment programs have had limited success. Following, Geoffrey Rose (40), small changes in large-scale factors such as CSD may have potential to shift the population distribution of body weight in a more favorable direction. Further research and intervention efforts to prevent childhood obesity should consider accounting for the constraints and risks stemming from the socio-economic community context and weigh its potential for intervention.
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Cross-sectional studies have shown a relationship between community socioeconomic deprivation and overweight in children.
Very few studies have longitudinal data over large and varied areas to examine the impact of community factors on trajectories of bodyweight change.
WHAT THIS STUDY ADDS
Electronic health records provide a new and powerful way of studying determinants of obesity in populations.
Community socio-economic deprivation at time of birth is associated with faster weight gain in children, particularly during childhood and early adolescence. Children born into the poorest neighborhoods are continuously negatively impacted by their environment.
Individual-level dietary and physical activity interventions that ignore the role of context in energy balance behavior may be limited in effectiveness.
ACKNOWLEDGEMENTS
Nau, Glass, Schwartz and Bandeen-Roche were involved in the design of the analysis.
Nau and Glass conducted the analysis.
Nau, Glass, Schwartz, and Bandeen-Roche were involved in the writing of the manuscript.
Pollak, Liu, Bailey-Davis, Hirsch, Glass and Schwartz were involved in the data-collection or preparation of data.
The project described was supported by Grant Number U54HD070725 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The project is co-funded by the NICHD and the Office of Behavioral and Social Sciences Research (OBSSR). Nau was supported by the training core of the Johns Hopkins Global Center on Childhood Obesity. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or OBSSR.
Appendix
Table A.
Estimates of fixed and random effects of growth-curve Models 1-3, boys and girls aged 3-18 years (a)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| std | std | |||||
| Estimate | errors | Estimate | errors | Estimate | std errors | |
| Fixed Intercept | 19.76560*** | 0.01978 | 19.4465*** | 0.02703 | 19.3615*** | 0.02744 |
| Age in years(b) | 0.89010*** | 0.00290 | 0.828*** | 0.004549 | 0.8104*** | 0.00461 |
| Age2 | 0.01994*** | 0.00033 | 0.02061*** | 0.000536 | 0.02028*** | 0.000541 |
| Age3 | −0.00520*** | 0.00005 | −0.00484*** | 0.000075 | −0.00464*** | 0.000076 |
| CSD 2nd Q. (c,d) | 0.13600*** | 0.01616 | 0.4842*** | 0.03447 | 0.4423*** | 0.03452 |
| CSD 3rd Q. | 0.18120*** | 0.01683 | 0.5951*** | 0.03395 | 0.531*** | 0.03411 |
| CSD 4th Q. | 0.23250*** | 0.01760 | 0.7113*** | 0.03368 | 0.6024*** | 0.03416 |
| Female | 0.26510*** | 0.02384 | 0.2585*** | 0.02383 | 0.2453*** | 0.0238 |
| Female × Age | 0.03607*** | 0.00408 | 0.03471*** | 0.004073 | 0.03229*** | 0.004067 |
| Female × Age2 | −0.00754*** | 0.00045 | −0.00756*** | 0.000446 | −0.00775*** | 0.000446 |
| Female × Age3 | −0.00047*** | 0.00007 | −0.00046*** | 0.000068 | −0.00048*** | 0.000068 |
| African American | 0.50420*** | 0.05668 | 0.4644*** | 0.05674 | 0.3435*** | 0.05704 |
| Other | −0.28000*** | 0.07478 | −0.2695*** | 0.07474 | −0.2992*** | 0.07467 |
| Hispanic | 0.78470*** | 0.12300 | 0.7375*** | 0.123 | 0.633*** | 0.123 |
| African American × Age | 0.06963*** | 0.00771 | 0.0621*** | 0.007703 | 0.04236*** | 0.007729 |
| Other × Age | −0.02680** | 0.01075 | −0.02595** | 0.01074 | −0.02957** | 0.01071 |
| Hispanic × Age | 0.04435** | 0.01734 | 0.03562** | 0.01732 | 0.02092 | 0.01728 |
| African American × Age2 |
−0.00110 | 0.00113 | −0.00097 | 0.001134 | −0.00214* | 0.001139 |
| Hispanic × Age2 | −0.00271 | 0.00291 | −0.00253 | 0.00291 | −0.00322 | 0.002908 |
| Other × Age2 | −0.00129 | 0.00166 | −0.00129 | 0.001664 | −0.00124 | 0.001662 |
| Age × CSD 2nd Q. | 0.07263*** | 0.005899 | 0.06277*** | 0.005906 | ||
| Age × CSD 3rd Q. | 0.07158*** | 0.005776 | 0.05668*** | 0.005805 | ||
| Age × CSD 4th Q. | 0.09866*** | 0.005722 | 0.07289*** | 0.005818 | ||
| Age2 × CSD 2nd Q. | −0.0011 | 0.000679 | −0.00138** | 0.00068 | ||
| Age2 × CSD 3rd Q. | −0.00218*** | 0.000656 | −0.0027*** | 0.000659 | ||
| Age2 × CSD 4th Q. | −0.00083 | 0.000644 | −0.00173** | 0.000655 | ||
| Age3 × CSD 2nd Q. | −0.00055*** | 0.000097 | −0.00043*** | 0.000097 | ||
| Age3 × CSD 3rd Q. | −0.00043*** | 0.000096 | −0.00027** | 0.000097 | ||
| Age3 × CSD 4th Q. | −0.00049*** | 0.000096 | −0.00025** | 0.000098 | ||
| Medical Assistance | 0.5165*** | 0.02605 | ||||
| Age × Medical Assistance |
0.1095*** | 0.00449 | ||||
| Age2 × Medical Assistance |
0.002765*** | 0.000501 | ||||
| Age3 × Medical Assistance |
−0.00088*** | 0.000074 | ||||
| Random effects | ||||||
| Level 1 residual | ||||||
| Variance (δ2) | 0.5521 | 0.00386 | 0.5519 | 0.00386 | 0.5517 | 0.00385 |
| Ages 3-5 | ||||||
| Ages 5-8 | 0.8217 | 0.00741 | 0.8219 | 0.00741 | 0.8219 | 0.00 741 |
| Ages 8 + | 1.7004 | 0.00588 | 1.7006 | 0.00588 | 1.6999 | 0.00588 |
| Variance in child- specific |
||||||
| intercept (π00) | 17.5362 | 0.00108 | 17.5087 | 0.07567 | 17.4618 | 0.07549 |
| Variance in random | ||||||
| slope of age (π10) | 0.1785 | 0.001098 | 0.1775 | 0.00109 | 0.1763 | 0.00109 |
| Variance of random | ||||||
| slope of age2 (π20) | 0.002037 | 0.00002 | 0.00204 | 0.00002 | 0.002035 | 0.00002 |
| Overall model fit | ||||||
| (-2 log likelihood) | 2241302 | 2240956 | 2240070 | |||
| Change in -2 log likelihood | 346 | 886 |
Mixed effects (multilevel) models estimated using full maximum likelihood. Level 1 residuals estimated separately for three age groups.
Age was centered at the overall population grand mean of 10.7 years. Therefore, the overall intercept represents the fixed estimate of BMI at the population average age, conditional on the random effects in the model.
First quartile of the CSD distribution is the reference group
CSD 2nd Q. (low-moderate), CSD 3rd Q. (moderate-high), CSD 4 Q. (highest), are the second, third and fourth quartiles of CSD, with ranges of [−1.77–0.51; 0.51–3.73; and 3.73–31.38] respectively. The reference group, CSD 1st Quartile (lowest) had a range of [−7.82–−1.77].
*** p-value < 0.001; ** 0.001 > p-value ≤ 0.05.
Footnotes
CONFLICTS OF INTEREST:
Dr. Nau reports grants from National Institute of Child Health and Development Development (U54 HD-070725), during the conduct of the study;
Dr. Schwartz reports grants from National Institute of Child Health and Development (U54 HD-070725), during the conduct of the study;
Dr. Bandeen-Roche reports other from Geisinger Center for Health Research, during the conduct of the study;
Dr. Liu reports grants from National Institute of Child Health and Development (U54 HD-070725), grants from NIH T32 Fellowship, during the conduct of the study;
Mr. Pollak reports grants from National Institute of Child Health and Development (U54 HD-070725), during the conduct of the study;
Dr. Hirsch reports grants from National Institute of Child Health and Development (U54 HD-070725), during the conduct of the study;
Dr. Bailey-Davis reports grants from National Institute of Child Health and Development (U54 HD-070725), during the conduct of the study;
Dr. Glass reports grants from National Institute of Child Health and Development (U54 HD-070725) during the conduct of the study.
REFERENCES
- 1.Baskin M, Ard J, Franklin F, Allison D. Prevalence of obesity in the United States. Obesity reviews. 2005;6:5–7. doi: 10.1111/j.1467-789X.2005.00165.x. [DOI] [PubMed] [Google Scholar]
- 2.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. New England journal of medicine. 1993;329:1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 3.Singh AS, Mulder C, Twisk JW, Van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity reviews. 2008;9:474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 4.Reilly J, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. International journal of obesity. 2010;35:891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 5.Thompson D, Wolf AM. The medical-care cost burden of obesity. Obesity reviews. 2001;2:189–197. doi: 10.1046/j.1467-789x.2001.00037.x. [DOI] [PubMed] [Google Scholar]
- 6.Connelly J, Duaso M, Butler G. A systematic review of controlled trials of interventions to prevent childhood obesity and overweight: a realistic synthesis of the evidence. Public health. 2007;121:510–517. doi: 10.1016/j.puhe.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Caballero B. Obesity prevention in children: opportunities and challenges. International journal of obesity. 2004;28:S90–S95. doi: 10.1038/sj.ijo.0802797. [DOI] [PubMed] [Google Scholar]
- 8.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Social science & medicine. 2006;62:1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 9.Boone-Heinonen J, Gordon-Larsen P. Obesogenic environments in youth: concepts and methods from a longitudinal national sample. Am J Prev Med. 2012;42:e37–46. doi: 10.1016/j.amepre.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doak C, Visscher T, Renders C, Seidell J. The prevention of overweight and obesity in children and adolescents: a review of interventions and programmes. Obesity reviews. 2006;7:111–136. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- 11.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. American journal of preventive medicine. 2009;36:74–81. e10. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 12.Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. American journal of preventive medicine. 2008;35:561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. American journal of preventive medicine. 2004;27:211–217. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 15.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–276. [PubMed] [Google Scholar]
- 16.Sealy YM. Parents’ perceptions of food availability: implications for childhood obesity. Social Work in Health Care. 2010;49:565–580. doi: 10.1080/00981381003635353. [DOI] [PubMed] [Google Scholar]
- 17.Burdette HL, Whitaker RC. A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics. 2005;116:657–662. doi: 10.1542/peds.2004-2443. [DOI] [PubMed] [Google Scholar]
- 18.Franzini L, Elliott MN, Cuccaro P, Schuster M, Gilliland MJ, Grunbaum JA, et al. Influences of physical and social neighborhood environments on children’s physical activity and obesity. Journal Information. 2009;99 doi: 10.2105/AJPH.2007.128702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dietz WH. Critical periods in childhood for the development of obesity. The American journal of clinical nutrition. 1994;59:955–959. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- 20.Liu AY, Curriero FC, Glass TA, Stewart WF, Schwartz BS. The contextual influence of coal abandoned mine lands in communities and type 2 diabetes in Pennsylvania. Health & Place. 2013:115–122. doi: 10.1016/j.healthplace.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Schwartz BS, Bailey-Davis L, Bandeen-Roche K, Pollak J, Hirsch AG, Nau C, et al. Attention Deficit Disorder, Stimulant Use, and Childhood Body Mass Index Trajectory. Pediatrics. 2014;133:668–676. doi: 10.1542/peds.2013-3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berkey CS, Colditz GA. Adiposity in Adolescents: Change in Actual BMI Works Better Than Change in BMI< i> z</i> Score for Longitudinal Studies. Annals of epidemiology. 2007;17:44–50. doi: 10.1016/j.annepidem.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 23.CDC Cut-offs to define outliers in the 2000 CDC Growth Charts 2014. [cited 2014 April 4 2014] Available from: http://www.cdc.gov/nccdphp/dnpa/growthcharts/resources/BIV-cutoffs.pdf.
- 24.Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. Journal of community health. 2008;33:90–102. doi: 10.1007/s10900-007-9071-7. [DOI] [PubMed] [Google Scholar]
- 25.Drewnowski A, D Rehm C, Solet D. Disparities in obesity rates: analysis by ZIP code area. Social science & medicine. 2007;65:2458–2463. doi: 10.1016/j.socscimed.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oliver LN, Hayes MV. Effects of neighbourhood income on reported body mass index: an eight year longitudinal study of Canadian children. BMC Public Health. 2008;8:16. doi: 10.1186/1471-2458-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stafford M, Brunner EJ, Head J, Ross NA. Deprivation and the development of obesity: a multilevel, longitudinal study in England. American journal of preventive medicine. 2010;39:130–139. doi: 10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 28.Greves Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P. Child obesity associated with social disadvantage of children’s neighborhoods. Soc Sci Med. 2010;71:584–591. doi: 10.1016/j.socscimed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhoods, obesity, and diabetes—a randomized social experiment. New England journal of medicine. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waters E, de Silva Sanigorski A, Hall B, Brown T, Campbell K, Gao Y, et al. Interventions for preventing obesity in children (Review) Cochrane collaboration. 2011:1–212. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 31.Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. Am J Prev Med. 2008;35:561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Lenthe F, Mackenbach J. Neighbourhood deprivation and overweight: the GLOBE study. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 2002;26:234–240. doi: 10.1038/sj.ijo.0801841. [DOI] [PubMed] [Google Scholar]
- 33.Massey DS, Gross AB, Shibuya K. Migration, segregation, and the geographic concentration of poverty. Am Sociol Rev. 1994;59:425–445. [Google Scholar]
- 34.Saelens BE, Sallis JF, Frank LD, Couch SC, Zhou C, Colburn T, et al. Obesogenic neighborhood environments, child and parent obesity: the Neighborhood Impact on Kids study. Am J Prev Med. 2012;42:e57–64. doi: 10.1016/j.amepre.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff (Millwood) 2010;29:503–512. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- 36.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–1374. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 37.Boehmer TK, Lovegreen SL, Haire-Joshu D, Brownson RC. What constitutes an obesogenic environment in rural communities? Am J Health Promot. 2006;20:411–421. doi: 10.4278/0890-1171-20.6.411. [DOI] [PubMed] [Google Scholar]
- 38.Schwartz BS, Stewart WF, Godby S, Pollak J, DeWalle J, Larson S, et al. Body mass index and the built and social environments in children and adolescents using electronic health records. American journal of preventive medicine. 2011;41:e17–e28. doi: 10.1016/j.amepre.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 39.Association AD. Position of the American Dietetic Association: individual-, family-, school-, and community-based interventions for pediatric overweight. Journal of the American Dietetic Association. 2006;106:925. doi: 10.1016/j.jada.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 40.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30:427–432. doi: 10.1093/ije/30.3.427. discussion 433-424. [DOI] [PubMed] [Google Scholar]