Abstract
Context:
The Foot and Ankle Ability Measure (FAAM) is a valid, reliable, and self-reported outcome instrument for the foot and ankle region.
Objective:
To provide evidence for translation, cross-cultural adaptation, validity, and reliability of the Japanese version of the FAAM (FAAM-J).
Design:
Cross-sectional study.
Setting:
Collegiate athletic training/sports medicine clinical setting.
Patients or Other Participants:
Eighty-three collegiate athletes.
Main Outcome Measure(s):
All participants completed the Activities of Daily Living and Sports subscales of the FAAM-J and the Physical Functioning and Mental Health subscales of the Japanese version of the Short Form-36v2 (SF-36). Also, 19 participants (23%) whose conditions were expected to be stable completed another FAAM-J 2 to 6 days later for test-retest reliability. We analyzed the scores of those subscales for convergent and divergent validity, internal consistency, and test-retest reliability.
Results:
The Activities of Daily Living and Sports subscales of the FAAM-J had correlation coefficients of 0.86 and 0.75, respectively, with the Physical Functioning section of the SF-36 for convergent validity. For divergent validity, the correlation coefficients with Mental Health of the SF-36 were 0.29 and 0.27 for each subscale, respectively. Cronbach α for internal consistency was 0.99 for the Activities of Daily Living and 0.98 for the Sports subscale. A 95% confidence interval with a single measure was ±8.1 and ±14.0 points for each subscale. The test-retest reliability measures revealed intraclass correlation coefficient values of 0.87 for the Activities of Daily Living and 0.91 for the Sports subscales with minimal detectable changes of ±6.8 and ±13.7 for the respective subscales.
Conclusions:
The FAAM was successfully translated for a Japanese version, and the FAAM-J was adapted cross-culturally. Thus, the FAAM-J can be used as a self-reported outcome measure for Japanese-speaking individuals; however, the scores must be interpreted with caution, especially when applied to different populations and other types of injury than those included in this study.
Key Words: self-reported outcome measures, questionnaires, outcome assessments
Key Points
The Japanese version of the Foot and Ankle Ability Measure (FAAM-J) was successfully translated and cross-culturally adapted.
Evidence of convergent validity, divergent validity, internal consistency, and test-retest reliability for both subscales of the FAAM-J was obtained.
The FAAM-J can be used as a self-reported outcome measure for Japanese speakers.
Foot and ankle injuries are common in sport activities. Ankle sprains are the most frequent of all athletic injuries.1,2 The greatest risk factor for an ankle sprain is a previous ankle sprain, and chronic ankle instability is a concerning and common result of an initial ankle sprain.3 With recurrent injuries, such as ankle sprains, athletes frequently suffer from residual symptoms.4,5
Outcome measures are essential to evidence-based practice because they offer a basis for clinical decisions.6–8 There are 2 types of outcome measures: clinician rated and patient rated.8,9 Clinician-rated measures are acquired by clinicians and primarily collect information about the disease or injury. Clinician-rated measures address impairments. In contrast, patient-rated measures focus on the data provided by patients, including information about how patients perceive the effect of the disease or injury on their function and participation in Activities of Daily Living (ADL) and sports. Incorporating patient-based outcome measures into health care is imperative to fully appreciate the effect of pathologic conditions on the patient's overall health.8,10 A self-reported outcome instrument allows clinicians to incorporate a patient's values into the medical treatment and to evaluate the effectiveness of interventions from the patient's perspective.
Self-reported outcome instruments can be generic or specific.10 Specific self-reported outcome instruments address disease, body region, dimension, summary items, and individual measures.10 Clinicians need to choose a self-reported outcome instrument based on its intended use. However, before a self-reported outcome instrument is used for that purpose, evidence must be provided that includes, among other items, face validity, content validity, construct validity, internal consistency, and reliability.10–13 Furthermore, a self-reported outcome instrument needs to be translated and cross-culturally adapted if it is to be used in another culture or by speakers of another language.14
More than a dozen self-reported outcome instruments have been developed for the foot and ankle region.15–17 The original version of the Foot and Ankle Ability Measure (FAAM) is 1 of the 4 instruments that provide evidence of content validity, construct validity, reliability, and responsiveness.15,16 To our knowledge, the FAAM has been translated into German, Persian, and French.18–20 Before this writing, it had not been translated into Japanese. Thus, the primary objective of our study was to provide evidence of the validity and reliability of the Japanese version of the FAAM (FAAM-J).
METHODS
The Instrument
The FAAM, originally developed by Martin et al,21 has 29 items in its questionnaire, with 21 items (72%) in the ADL subscale and 8 items (28%) in the Sports subscale. Each item is scored on a 5-point Likert scale, with 4 representing no difficulty at all; 3, slight difficulty; 2, moderate difficulty; 1, extreme difficulty; and 0, unable to do. Therefore, the highest possible scores are 84 for the ADL subscale and 32 for the Sports subscale. Unanswered items or N/A responses are not counted in the total score, and for every item without a response or with an N/A, 4 points are subtracted from the highest potential score. To calculate percentage values, each total subscale score is divided by the highest potential score. A higher score represents a higher level of physical function. At the end of each subscale, global ratings of functions for ADL (GRF-ADL) and sport-related activities (GRF-SP) are also calculated, with 0% indicating the inability to perform any of the usual daily activities and 100% indicating the level of function before injury. Additionally, at the end of the form, patients are asked to rate the current level of function with a 4-point Likert scale (normal, nearly normal, abnormal, or severely abnormal). Patients rate each item according to the difficulty they encounter with each task because of their foot and ankle condition. We obtained permission from the developers to translate and adapt the FAAM (R.L. Martin, oral communication, 2012).
Short-Form 36, Version 2, Health Survey
The Short-Form 36, Version 2 (SF-36v2, commonly known as the SF-36), Health Survey is a generic, self-reported outcome instrument for measuring a range of the effects of a condition or disease on patients.22,23 It consists of 8 subscales: (1) Physical Functioning (PF), (2) Role-Physical, (3) Bodily Pain, (4) General Health Perception, (5) Vitality, (6) Social Functioning, (7) Role-Emotional, and (8) Mental Health (MH). Each subscale has a 0 to 100 score range, and a higher score represents a better health status. The Japanese version of the SF-36 was validated by Fukuhara et al.24,25
Translation and Cross-Cultural–Adaptation Process
We conducted the translation and cross-cultural–adaptation process in accordance with the guidelines set by the International Society for Quality of Life Assessment.14 The forward translation of the original version of the FAAM was performed by 2 independent, native Japanese translators (T1 and T2) with extensive English expertise, who had no medical background. In a consensus meeting, T1 and T2 discussed the discrepancies and agreed on the preliminary version of the FAAM-J. Translator 3, a native Japanese speaker with medical expertise and broad experience in translating medical literature, rated the preliminary version of the FAAM-J in terms of clarity, common language use, and conceptual equivalence, creating the forward-translation version of the FAAM-J. Translators 4 and 5, native Japanese speakers with extensive translation experience, then translated the forward-translation version of the FAAM-J back into English (back-translation version of the FAAM-J). Translator 6, a native American-English speaker with no medical background, compared the back-translation version of the FAAM-J with the original FAAM for conceptual equivalence to make further adjustments as needed. A committee reviewed and discussed the disagreements and possible modifications and agreed on the prefinal version of the FAAM-J. We pilot tested the prefinal version of the FAAM-J on 20 collegiate students for accuracy of wording and ease of understanding; no difficulties were noted during that process.
Participants
Competitive athletes with foot and ankle injuries, from 7 competitive, collegiate varsity teams (men's basketball [n = 1; 14%], women's basketball [n = 3; 43%], men's rugby [n = 1; 14%], men's soccer [n = 1; 14%], and men's gymnastics [n = 1; 14%]) from 3 institutions participated in the study. Athletes' foot and ankle injuries included in the study were musculoskeletal and originated during sports participation. Participants were excluded if they had injuries to the lower back, hip, knee, lower leg, ankle, or foot regions within the previous 6 months before the study. Other exclusion criteria were a history of surgery to the above-mentioned areas, coexisting musculoskeletal injuries in other body parts, or chronic conditions, such as systematic inflammatory rheumatic disease, neurologic or vascular conditions, cancer, diabetes mellitus, alcohol abuse, or psychiatric disorders.21
Injury Classification
The locations and injury types were categorized in a system modified from previous literature.26 The locations of injury were the Achilles tendon, ankle, foot, and toes. The types of injuries included fractures (traumatic); stress fractures (overuse); other bone injuries, dislocations or subluxations; tendon ruptures; sprains (injury of joint or ligaments or both); lesions of meniscus or cartilage; strains or muscle ruptures or tears; contusions, hematomas, or bruises; tendinosis or tendinopathy; bursitis; lacerations, abrasions, or skin lesions; and muscle cramps or spasms.26
Data Collection
Before the study, each participant signed an informed consent release and was asked to complete the FAAM-J and SF-36. The forms were given to the participant once he or she had a condition with an acute or chronic onset and sought medical attention from team medical personnel while the nature of the condition and the inclusion-exclusion criteria were confirmed. For reliability testing, 19 of the 83 participants (23%), whose conditions were expected to remain stable (ie, chronic state, no treatments), were asked to fill out the forms again 2 to 6 days after the initial recording. This study was approved by the institutional review board of Waseda University.
Statistical Analysis
To examine the convergent validity, we analyzed correlations between the ADL and Sports subscales of the FAAM-J and the PF subscale of the SF-36 with the Pearson product moment correlation coefficient. Similarly, we analyzed the correlations between the ADL and Sports subscales of the FAAM-J and the MH subscale of the SF-36 to assess the divergent validity. The a priori α level for this analysis was set at .05. Also, the Pearson product moment correlation coefficients between the ADL subscale of the FAAM-J and the GRF-ADL and the Sports subscale of the FAAM-J and the GRF-SP were calculated.
A Cronbach α coefficient was determined to assess the internal consistency. The standard error of measurement (SEM) for each subscale score was calculated as 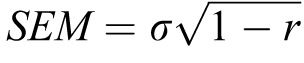 , where σ was the standard deviation of the score, and r was the coefficient α. The error associated with a score at a single time point was acquired by calculating a 95% confidence interval (95% CI).
, where σ was the standard deviation of the score, and r was the coefficient α. The error associated with a score at a single time point was acquired by calculating a 95% confidence interval (95% CI).
Test-retest reliability was examined with the intraclass correlation coefficient (ICC [2,1]). To confirm there was no systemic bias between the test and retest sessions, a paired t test was performed. We determined the SEM using the ICC test-retest reliability coefficient. The SEM was multiplied by  , and a 95% CI was calculated to determine the minimal detectable change (MDC). All statistical analyses were performed using SPSS (version 20.0; IBM Corp, Armonk, NY).
, and a 95% CI was calculated to determine the minimal detectable change (MDC). All statistical analyses were performed using SPSS (version 20.0; IBM Corp, Armonk, NY).
RESULTS
Participants
Eighty-three participants (59 men [71%] and 24 women [29%]) with foot and ankle injuries volunteered for the study. The demographic information, injury types, and injury location are presented in the Table. The predominant body part involved was the ankle, and the most-frequent injury type was a sprain.
Table.
Participants' Demographic and Injury Information
| Participants |
Value, No. (% or Range, SD) |
| Age, y | 20.3 (18–24, ±3.7) |
| Sex, n = 83 | |
| Male | 59 (71) |
| Female | 24 (29) |
| Foot and Ankle Ability Measure score, % | |
| Activities of Daily Living subscale | 74.2 (0–100, ±29.4) |
| Sports subscale | 52.1 (0–100, ±35.7 ) |
| Injury location (n = 83) | |
| Ankle | 63 (76) |
| Foot | 19 (23) |
| Toe | 1 (1) |
| Injury classification (n = 83) | |
| Sprain (injury of joint and/or ligaments) | 71 (86) |
| Fracture (traumatic) | 2 (2) |
| Lesion of meniscus or cartilage | 2 (2) |
| Other bone injuries | 2 (2) |
| Stress fracture (overuse) | 2 (2) |
| Tendinosis/tendinopathy | 2 (2) |
| Contusion/hematoma/bruise | 1 (1) |
| Other | 1 (1) |
Translation and Cross-Cultural Adaptation
No major difficulties were encountered during the translation and cross-cultural adaptation process. As expected, we found a few minor discrepancies during the forward-translation process; however, the translators reached agreement. In item 5 of the Sports subscale, cutting was translated as kattinngu in katakana (a Japanese alphabet for foreign words) by 1 translator and as houkoutenkan (literally “change of direction” in Japanese) by the other translator. We decided to use houkoutenkan rather than kattinngu because we thought kattinngu described a sport-specific maneuver and was appropriate if the FAAM was intended only for athletes and physically active individuals. Furthermore, kattinngu seemed too technical a term in Japanese for the general population, which, therefore, might be misinterpreted by many individuals who did not understand the meaning of the word. In addition, we thought that because houkoutenkan was listed in the Sports subscale, people would understand the word houkoutenkan within a sports activity context. Therefore, houkoutenkan would be correctly interpreted by respondents. In contrast, in item 7 of the Sports subscale, the word technique was translated as gihou by 1 translator, but we agreed to use tekunikku, literally written as technique in katakana, because it is more often used in the Japanese language than gihou is. After initial corrections of the minor discrepancies, no further difficulties were noted during the translation, evaluation, or pilot-testing processes.
Convergent and Divergent Validity
Statistical analyses revealed correlation coefficients of 0.86 between the ADL subscale and the PF section of the SF-36 (P < .001) and 0.75 between the Sports subscale and the PF section of the SF-36 (P < .001). Also, the ADL subscale had a correlation coefficient of 0.29 with the MH section of the SF-36 (P = .007), and the Sports subscale had a correlation coefficient of 0.27 with the MH section of the SF-36 (P = .013). In addition, the ADL subscale showed correlation coefficients of 0.89 (P < .001) and 0.80 (P < .001) with the GRF-ADL and GRF-SP, respectively, whereas the Sports subscale correlation coefficients were 0.80 (P < .001) and 0.87 (P < .001), respectively.
Internal Consistency
The Cronbach α for internal consistency was 0.99 for the ADL subscale (P < .001) and 0.98 for the Sports subscale (P < .001). The SEM for the ADL subscale was 2.9 and the MDC at 95% CI was ±8.1, whereas the SEM for the Sports subscale was 5.0 and the MDC at 95% CI was ±14.0.
Test-Retest Reliability
A paired t test revealed no systemic bias between the test and retest scores for both ADL (P = .096) and Sports (P = .848) subscales. Both subscales were shown to have excellent reliability. The MDC at 95% confidence was ±6.8 for the ADL subscale and ±13.7 for the Sports subscale.
DISCUSSION
Clinician-rated measures relate to impairment-oriented data, such as strength, pain, swelling, and range of motion, and provide information of an uncertain clinical utility.6,27 Although valuable in many ways, those measures should not be used alone.9 Patient-rated measures reflect patients' values and their perceptions of the condition they suffer from,8,10 and they provide the patient-oriented evidence that is directly related to the interests of the patients. Moreover, a recent study28 indicated that clinician-rated and patient-rated outcome measures assess different aspects of health status. Thus, it is important to incorporate both types of outcome measures into the clinical decision-making process.
Our study provided evidence for translation, cross-cultural adaptation, convergent validity, divergent validity, internal consistency, and test-retest reliability for both subscales of the FAAM-J. Therefore, the use of the FAAM-J as a self-reported outcome measure for the foot and ankle region was validated with some limitations.
Although the concepts are related, face validity addresses whether an instrument is measuring what it is designed to measure, whereas content validity is concerned with adequacy, or the extent to which the items in an instrument measure the domain of interest.13,29 Not only experts but also patients need to participate in developing an instrument.10,11 The original version of the FAAM went through a rigorous item-selection process in which both expert clinicians and patients participated, using item-reduction theory.21 The evaluation of face and content validity is qualitative and subjective, but the meticulous process in the development of the original version of the FAAM, which incorporated both the expert clinicians' and the patients' values and opinions, provided evidence for its face and content validity.
The construct validity of an instrument is determined by evaluating the correlation between the tested instrument and other measures that are logically hypothesized from a relationship between the patient's health status and the construct. Also, there are 2 types of construct validity: convergent and discriminant (divergent).13 Evidence for convergent validity is provided when the instrument is shown to have a strong correlation with other measures of the same construct. Divergent validity occurs when the relationship is weak or nonexistent between the score on the tested instrument and measures of a different construct. The constructs that the FAAM is intended to measure are functional limitations to the foot and ankle regions and activity restrictions. In this study, as expected, both subscales of the FAAM-J had high correlations with the PF and low correlations with the MH sections of the SF-36. The correlation coefficients with PF were 0.86 for the ADL subscale and 0.75 for the Sports subscale, whereas those with MH were 0.29 for the ADL subscale and 0.27 for the Sports subscale. Furthermore, our results were in accordance with the original and French versions of the FAAM.20,21 Thus, the subscales of the FAAM-J were correlated with the PF aspect of the patients' health status but not with the MH aspect, providing evidence for the convergent and divergent validity of the FAAM-J.
Internal consistency is the extent to which the items in an instrument are measuring different aspects of the construct and is associated with an error within a single measure. Internal consistency is commonly assessed with correlations between all items in the instrument. In this study, the Cronbach α for internal consistency was 0.99, with an SEM of 2.9 for the ADL subscale, and 0.98, with an SEM of 5.0 for the Sports subscale. The 95% CI with a single measure was ±8.1 and ±14.0 for respective subscales. The 95% CI value for the Sports subscale of the FAAM-J was different from the values found for the original and French versions of the FAAM.20,21 Although speculative, several sources of the discrepancy were possible. First, the patient population could be a source of the discrepancy; adults (age = 41.2 ± 16.3 years for the original version and 50.5 ± 14.6 years for the French version) were the participants in the other 2 studies, whereas young, competitive athletes (age = 20.3 ± 3.7 years) were the participants in this study. Second, the proportions of various injury locations and types varied among the studies. In our study, the locations and types of injuries were largely acute ankle sprains, which was expected because we studied competitive collegiate athletes.1
Reliability relates to the stability of the scores with repeated measures when no change to the health status is expected and is assessed by the test-retest measure. The evidence for the reliability of the FAAM-J was provided with the high ICCs for the ADL and Sports subscales. The MDC value for the Sports subscale was different from the values in the original and French versions. A possible explanation, along with the above-mentioned sources of discrepancies, may be the time between the test and retest; it was 4 weeks in the original version and 2 days in the French version, whereas it was 2–6 days in this study.
The FAAM has been widely used as a self-reported outcome measure to assess (1) the functional limitations and activity restrictions caused by various pathologic conditions of the foot and ankle region and (2) the effectiveness of interventions that clinicians provide. Such conditions include foot and ankle trauma,17 acute ankle sprain,30 plantar heel pain,31 plantar fasciitis,32 ankle arthrodesis,33 ankle arthritis,34 chronic ankle instability,35–37 recurrent peroneal subluxation,38 and diabetes.39,40 The original version of the FAAM, along with 3 other questionnaires, provided evidence for content validity, construct validity, reliability, and responsiveness to support their use.16 Also, the FAAM and the Foot and Ankle Disability Index, a prototype of the FAAM, were considered to be the most-suitable self-reported outcome instruments for chronic ankle instability during a systemic review.15 Therefore, we deemed it appropriate and valuable to translate and cross-culturally adapt the FAAM for its use in Japanese.
Furthermore, a standard method of assessment allows comparisons of different treatment methods.41 The prevalent use of the FAAM enables clinicians to make such comparisons for better clinical decisions. Thus, a cross-culturally adapted version of the FAAM is beneficial not only for the individuals who speak that language but also for those who speak the languages used in the other versions of the FAAM.
A recent study42 showed that people with functional ankle instability (FAI) had lower FAAM scores and SF-36 physical component summaries. In addition, both the ADL and Sports subscales of the FAAM for FAI were positively correlated with the SF-36 Physical Component Summary and related subscales but not with the Mental Component Summary. Furthermore, the scores of the FAAM were correlated with the PF subscale to a greater degree than with the Physical Component Summary or other subscales of the Physical Component Summary. Therefore, although the functional limitations caused by FAI contribute to the health-related quality-of-life score, the FAAM primarily captured, and was more specific to, a physical dimension, and other factors contributed to the overall health-related quality of life. Thus, clinicians need to be careful about the dimensions they intend to capture with the FAAM.
The current study had some limitations. First, although our translation process was in accordance with the guidelines in previous literature,14 there were limitations to our validation process with classic test theory; namely, classic test theory focuses only on the whole test score and disregards the interaction between a respondent's ability and the characteristics of the item, such as difficulty, and each item's sensitivity to the respondent's ability level, whereas item-reduction theory can account for those factors. A study using item-reduction theory indicated that some items in a self-reported outcome instrument are more culture specific than others are,43 whereas our study did not address that issue because the classic test theory was applied. Additionally, the FAAM-J was compared with the original version of the FAAM and the SF-36, and hence, the reliability and validity of the FAAM-J were confined to those instruments. Therefore, although our method was similar to that of the development of the French version of the FAAM, future researchers need to address those limitations within the FAAM-J.
Second, the characteristics of our participants were different than those tested for the original and French versions of the FAAM. Specifically, this study was conducted on young, competitive athletes, whereas the previous 2 studies were of adults in a general population. A previous investigation44 showed that the SF-36 scores of uninjured, elite athletes differed slightly from the age-matched norm values, and that trend was more substantial among women. Another study of physically active individuals showed that the uninjured control group, as well as the FAI group, had better PF subscale scores than the general population did, whereas only the uninjured controls had better PF scores than the age-matched population.42 However, both the control and FAI groups had Mental Component Summary scores similar to those of the general population, although they were below those of the age-matched population. Furthermore, the magnitudes of functional limitations, participation restrictions, and disabilities experienced by injured individuals might vary according to the expected normal levels for each person.45 Therefore, further evidence is needed on this aspect of the FAAM-J, and the scores of the FAAM-J must be interpreted with caution when applied to a general population.
CONCLUSIONS
This study provides evidence for translation, cross-cultural adaptation, convergent and divergent validity, internal consistency, and test-retest reliability for the FAAM-J. Thus, the FAAM-J can be used as a self-reported outcome measure of an athletic population of Japanese-speaking individuals with acute ankle injuries; however, the scores of the FAAM-J must be interpreted with caution, especially when applied to different populations and other types of injury.
REFERENCES
- 1.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 2.Junge A, Langevoort G, Pipe A, et al. Injuries in team sport tournaments during the 2004 Olympic Games. Am J Sports Med. 2006;34(4):565–576. doi: 10.1177/0363546505281807. [DOI] [PubMed] [Google Scholar]
- 3.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 4.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3) doi: 10.1136/bjsm.2004.011676. e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 6.Jette AM. Outcomes research: shifting the dominant research paradigm in physical therapy. Phys Ther. 1995;75(11):965–970. doi: 10.1093/ptj/75.11.965. [DOI] [PubMed] [Google Scholar]
- 7.Jette AM, Keysor JJ. Uses of evidence in disability outcomes and effectiveness research. Milbank Q. 2002;80(2):325–345. doi: 10.1111/1468-0009.t01-1-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valovich McLeod TC, Snyder AR, Parsons JT, Curtis Bay R, Michener LA, Sauers EL. Using disablement models and clinical outcomes assessment to enable evidence-based athletic training practice, part II: clinical outcomes assessment. J Athl Train. 2008;43(4):437–445. doi: 10.4085/1062-6050-43.4.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michener LA. Patient- and clinician-rated outcome measures for clinical decision making in rehabilitation. J Sport Rehabil. 2011;20(1):37–45. doi: 10.1123/jsr.20.1.37. [DOI] [PubMed] [Google Scholar]
- 10.Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2(14):i–iv. 1–74. [PubMed] [Google Scholar]
- 11.Lohr KN, Aaronson NK, Alonso J, et al. Evaluating quality-of-life and health status instruments: development of scientific review criteria. Clin Ther. 1996;18(5):979–992. doi: 10.1016/s0149-2918(96)80054-3. [DOI] [PubMed] [Google Scholar]
- 12.Ware JE, Jr, Brook RH, Davies AR, Lohr KN. Choosing measures of health status for individuals in general populations. Am J Public Health. 1981;71(6):620–625. doi: 10.2105/ajph.71.6.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Portney LG, Watkins MP. Validity of measurements. In: Portney LG, Watkins MP, editors. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, NJ: Prentice Hall;; 2000. pp. 79–110. [Google Scholar]
- 14.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25(24):3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 15.Eechaute C, Vaes P, Van Aerschot L, Asman S, Duquet W. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: a systematic review. BMC Musculoskelet Disord. 2007;8:6. doi: 10.1186/1471-2474-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin RL, Irrgang JJ. A survey of self-reported outcome instruments for the foot and ankle. J Orthop Sports Phys Ther. 2007;37(2):72–84. doi: 10.2519/jospt.2007.2403. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein CL, Schemitsch E, Bhandari M, Mathew G, Petrisor BA. Comparison of different outcome instruments following foot and ankle trauma. Foot Ankle Int. 2010;31(12):1075–1080. doi: 10.3113/FAI.2010.1075. [DOI] [PubMed] [Google Scholar]
- 18.Nauck T, Lohrer H. Translation, cross-cultural adaption and validation of the German version of the Foot and Ankle Ability Measure for patients with chronic ankle instability. Br J Sports Med. 2011;45(10):785–790. doi: 10.1136/bjsm.2009.067637. [DOI] [PubMed] [Google Scholar]
- 19.Mazaheri M, Salavati M, Negahban H, et al. Reliability and validity of the Persian version of Foot and Ankle Ability Measure (FAAM) to measure functional limitations in patients with foot and ankle disorders. Osteoarthritis Cartilage. 2010;18(6):755–759. doi: 10.1016/j.joca.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 20.Borloz S, Crevoisier X, Deriaz O, Ballabeni P, Martin RL, Luthi F. Evidence for validity and reliability of a French version of the FAAM. BMC Musculoskelet Disord. 2011;12:40. doi: 10.1186/1471-2474-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Jr, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):903–912. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 24.Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 health survey for use in Japan. J Clin Epidemiol. 1998;51(11):1037–1044. doi: 10.1016/s0895-4356(98)00095-x. [DOI] [PubMed] [Google Scholar]
- 25.Fukuhara S, Ware JE, Jr, Kosinski M, Wada S, Gandek B. Psychometric and clinical tests of validity of the Japanese SF-36 health survey. J Clin Epidemiol. 1998;51(11):1045–1053. doi: 10.1016/s0895-4356(98)00096-1. [DOI] [PubMed] [Google Scholar]
- 26.Junge A, Engebretsen L, Alonso JM, et al. Injury surveillance in multi-sport events: the International Olympic Committee approach. Br J Sports Med. 2008;42(6):413–421. doi: 10.1136/bjsm.2008.046631. [DOI] [PubMed] [Google Scholar]
- 27.Hurwitz SR, Slawson D, Shaughnessy A. Orthopaedic information mastery: applying evidence-based information tools to improve patient outcomes while saving orthopaedists' time. J Bone Joint Surg Am. 2000;82(6):888–894. doi: 10.2106/00004623-200006000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Roddey TS, Cook KF, O'Malley KJ, Gartsman GM. The relationship among strength and mobility measures and self-report outcome scores in persons after rotator cuff repair surgery: impairment measures are not enough. J Shoulder Elbow Surg. 2005;14(suppl 1):95S–98S. doi: 10.1016/j.jse.2004.09.023. [DOI] [PubMed] [Google Scholar]
- 29.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 30.Cosby NL, Hertel J. Clinical assessment of ankle injury outcomes: case scenario using the foot and ankle ability measure. J Sport Rehabil. 2011;20(1):89–99. doi: 10.1123/jsr.20.1.89. [DOI] [PubMed] [Google Scholar]
- 31.Cleland JA, Abbott JH, Kidd MO, et al. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2009;39(8):573–585. doi: 10.2519/jospt.2009.3036. [DOI] [PubMed] [Google Scholar]
- 32.Drake M, Bittenbender C, Boyles RE. The short-term effects of treating plantar fasciitis with a temporary custom foot orthosis and stretching. J Orthop Sports Phys Ther. 2011;41(4):221–231. doi: 10.2519/jospt.2011.3348. [DOI] [PubMed] [Google Scholar]
- 33.Hendrickx RP, Stufkens SA, de Bruijn EE, Sierevelt IN, van Dijk CN, Kerkhoffs GM. Medium- to long-term outcome of ankle arthrodesis. Foot Ankle Int. 2011;32(10):940–947. doi: 10.3113/FAI.2011.0940. [DOI] [PubMed] [Google Scholar]
- 34.Criswell BJ, Douglas K, Naik R, Thomson AB. High revision and reoperation rates using the agility total ankle system. Clin Orthop Relat Res. 2012;470(7):1980–1986. doi: 10.1007/s11999-012-2242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012;30(11):1798–1804. doi: 10.1002/jor.22150. [DOI] [PubMed] [Google Scholar]
- 36.Woodman R, Berghorn K, Underhill T, Wolanin M. Utilization of mobilization with movement for an apparent sprain of the posterior talofibular ligament: a case report. Man Ther. 2013;18(1):e1–e7. doi: 10.1016/j.math.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 37.Carcia CR, Martin RL, Drouin JM. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boykin RE, Ogunseinde B, McFeely ED, Nasreddine A, Kocher MS. Preliminary results of calcaneofibular ligament transfer for recurrent peroneal subluxation in children and adolescents. J Pediatr Orthop. 2010;30(8):899–903. doi: 10.1097/BPO.0b013e3181fbfcea. [DOI] [PubMed] [Google Scholar]
- 39.Martin RL, Hutt DM, Wukich DK. Validity of the Foot and Ankle Ability Measure (FAAM) in diabetes mellitus. Foot Ankle Int. 2009;30(4):297–302. doi: 10.3113/FAI.2009.0297. [DOI] [PubMed] [Google Scholar]
- 40.Kivlan BR, Martin RL, Wukich DK. Responsiveness of the Foot and Ankle Ability Measure (FAAM) in individuals with diabetes. Foot (Edinb) 2011;21(2):84–87. doi: 10.1016/j.foot.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 41.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 42.Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. J Athl Train. 2011;46(6):634–641. doi: 10.4085/1062-6050-46.6.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Custers JW, Hoijtink H, van der Net J, Helders PJ. Cultural differences in functional status measurement: analyses of person fit according to the Rasch model. Qual Life Res. 2000;9(5):571–578. doi: 10.1023/a:1008949108089. [DOI] [PubMed] [Google Scholar]
- 44.McAllister DR, Motamedi AR, Hame SL, Shapiro MS, Dorey FJ. Quality of life assessment in elite collegiate athletes. Am J Sports Med. 2001;29(6):806–810. doi: 10.1177/03635465010290062201. [DOI] [PubMed] [Google Scholar]
- 45.Vela LI, Denegar C. Transient disablement in the physically active with musculoskeletal injuries, part I: a descriptive model. J Athl Train. 2010;45(6):615–629. doi: 10.4085/1062-6050-45.6.615. [DOI] [PMC free article] [PubMed] [Google Scholar]


