Abstract
New developments in PET/CT technology have enabled the commercial availability of continuous bed motion (CBM) acquisition methods. This technology has some potential performance benefits compared to standard step and shoot (SS) imaging, however, this technology has not been assessed with regard to quantitative and image quality parameters compared to traditional SS techniques. This study seeks to compare clinically relevant quantitative and image quality parameters using CBM and SS data collection methods with the intent of providing assistance in making educated decisions regarding imaging protocol development when using CBM technology versus SS imaging.
Keywords: PET, CT, continuous bed motion, CBM
Introduction
Preclinical positron emission tomography (PET) and computed tomography (CT) systems have had implementations of continuous bed motion (CBM) since before 2009 where it has been shown to effectively increase a scanner’s possible axial extent, enable whole-body kinetics, and potentially improve image quality because of axial oversampling [1-3]. Other techniques to improve PET image quality were assessed, including “wobbling” the bed or detector arrays to increase image resolution, however, the hardware for these systems did not lend itself to further commercialization and realized only limited use in research studies [4-6].
For over a decade, CBM-based PET/CT systems have been in development, with initial data from these studies indicating that a CBM acquisition technique may result in improved axial sampling and image uniformity [7]. Strides were made in 2000 by Dahlbom, et al. to develop the fundamental framework for the development of CBM acquisition and processing methods for clinical platform, including rigorous assessments of new sampling schemes for PET imaging [8,9]. This work was followed by additional work by Townsend, et al. but no viable commercial systems developed at that time from those efforts [10,11]. The methods behind this prototype and related processing systems were patented in 2005 with further work performed by Burbar et. Al. to develop the workflow into a clinically relevant routine [12,13]. Recently, this prior work in CBM technology has coalesced into a commercially available platform.
The clinical benefits of CBM PET/CT are potentially manifold. One such benefit is the potential for improved axial sensitivity. Step and shoot (SS) acquisition methods require that multiple overlapping beds be used to cover the entire axial extent of the patient. These individual beds have sensitivity profiles that degrade as you extend axially from the center of the field of view [14]. With CBM techniques, there is no overlap of bed positions that may cause artifacts and the axial sensitivity profile is uniform throughout the defined axial extent as compared in Figure 1. Uniformity and sensitivity is also potentially improved as each part of the patient will pass through the center of the PET imaging system [15]. Improvements in axial sensitivity may result in improved image contrast because of slight reductions in overall image noise [16]. This work investigates key performance parameters when using CBM acquisitions techniques and provides insight into the effect this type of acquisition may have on PET/CT data.
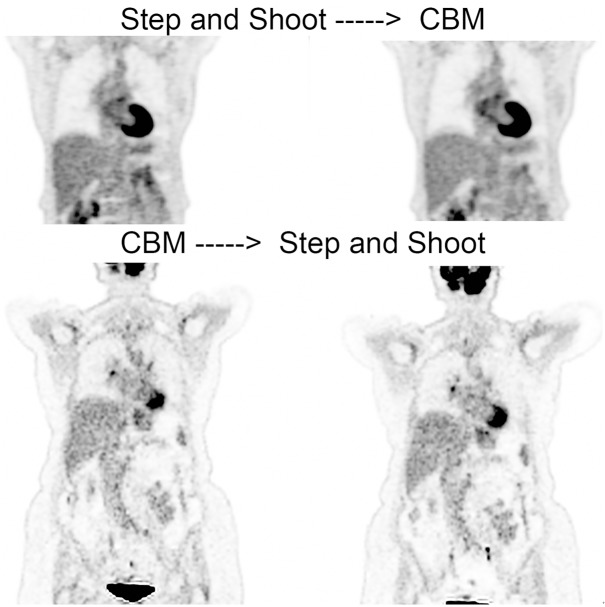
Figure 1.
Shows the comparison of the axial range selection between step & shoot and continuous bed motion methods. A topogram is shown for each image with the intermediate lines illustrating overlapping beds for step & shoot and the colored bars representing three different scan speeds selected over the course of a single continuous bed motion scan.
Materials and methods
Hardware and software
All data were collected using a Biograph mCT Flow with FlowMotion CBM acquisition capabilities (Siemens Medical Solutions USA, Inc.). Syngo software (Siemens Medical Solutions USA, Inc.), version VG50, was used for data acquisition, histogramming, and reconstruction. Data analysis was performed using the Inveon Research Workplace version 4.1 (Siemens Medical Solutions USA, Inc.) and standard spreadsheet software. Statistical analysis was performed using SPSS (IBM).
Patient population
Patients in this study were recruited under University of Tennessee Graduate School of Medicine Institutional Review Board approved protocol (#3539). Patients selected for this work were sampled from our routine outpatient PET/CT population with no preference given for any particular type of disease or scan type.
Phantom data comparison
Three separate studies were performed comparing phantom data between SS and CBM acquisition methods.
Body phantom comparison
The first set of measurements were acquired using a “body phantom” comprised of a uniform cylinder joined to the Society of Nuclear Medicine & Molecular Imaging Lung phantom. Whole-body PET/CT data using SS as well as CBM methods were acquired over an axial range covering the entire cylinder and torso phantom. Time per bed position for our single speed scans were set to our typical whole-body settings of 1.5 minutes per bed while our varying speed scans set the head region to be acquired at 1.5 minutes per bed and the torso region acquired at 2 minutes per bed. CBM acquisition protocols for our single bed speed scans were set to acquire data at a speed of 1.5 mm/s per manufacturer recommended equivalence settings on our imaging system (1.5 minutes per bed=1.5 mm/s). Protocols involving selection of multiple bed speeds over the axial range used four speeds: 2.5 mm/s and 1 mm/s in the head and neck regions and 1.5 mm/s and 2 mm/s in the torso regions. A total of twelve ROIs were drawn in the uniform cylinder as well as in sites of “lesions” found in the torso phantom for use in this comparison. ROI statistics were compared between acquisition modes and statistical analysis performed to determine differences between acquired data values.
Uniform cylinder comparison
The second group of tests focused on numerical analysis and comparison of regions of interest drawn in a uniform Ge-68 phantom for a more controlled test of image quality characteristics. Bed speed and time per bed selections for this series of scans were based on having equal scan times for both acquisition methods to cover a typical 90 cm patient scan. This required 7 overlapping beds for SS imaging using our PET/CT system.
Two comparisons were made with each scan repeated five times:
1. CBM scans at 1.5 mm/s and SS scans at 1.4 minutes per bed
a. Equivalent to a 10 minute scan @ 90 cm
2. CBM scans at 2.4 mm/s and SS scans at 0.8 minutes per bed
a. Equivalent to a 6.25 minute scan @ 90 cm
For each scan, the image was segmented using a defined cylindrical VOI placed centrally in the uniform cylinder. Descriptive statistics and coefficients of variation (CV) were calculated and statistically compared between acquisition methods and scan speeds with P<0.05 considered significant. Additionally, ratios between noise increases with changes in scan time were assessed to determine if either acquisition mode was less sensitive to changes in acquisition time.
End plane comparison
A third set of tests performed examined image quality at the end planes of typical single bed scan lengths to further test these initial results. For these tests, a uniform Ge-68 cylinder was placed centrally in the field of view with data acquired over only the range of a single bed position (~22 cm). This was to create a sub-optimal situation where end planes would be clearly visible with uniform activity and so that out of FOV activity effects would be present. The same single bed step shoot range was selected for CBM acquisition modes using only a single selected bed speed of 1.5 mm/s. SUVs were calculated at the center of the phantom and at the edges of the fields of view by drawing regions of interest in those regions as shown in Figure 2. Line profiles were drawn through the length of the phantom to visually compare edges with and without CBM acquisition methods. This series of tests was repeated five times to obtain an average value for measurements at the end planes and within the central portion of the phantom.
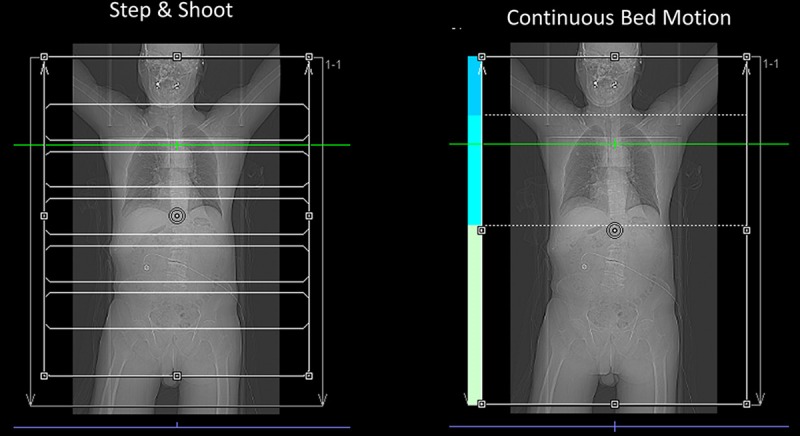
Figure 2.
Shows the analysis of end planes on a uniform 68-Germanium cylinder phantom. Analysis of regions of interest indicate that mean SUVs were nearly equivalent with up to an 80% change in SUVmax values and 30-50% reduction in standard deviation in end plane regions.
Clinical patient data comparison
The assessments described below were to determine the clinical relevance and effect of using CBM acquisition techniques in routine clinical use.
Quantitative comparison
Spherical regions of interest (ROIs) with a volume of ~870 mm3 were drawn in various areas throughout the patients for both acquisition methods. These regions included the liver, lungs, brain and background. Anatomical points of reference were used for consistent positioning of regions of interest in the analysis. Liver regions were defined approximately 5 cm from the spine and 3 cm caudally from the upper most portion of the liver. Lung regions were drawn approximately 2 cm from the lung wall and placed centrally in the lung. Spine region statistics were calculated from three regions drawn in three separate vertebra and the average values assessed. Background measurements were taken 2 cm from the furthest transaxial extent of uptake. For some patients this was 2 cm from the outside of the arm, while for others, this was 2 cm from the chest wall extending radially outward.
For each region of interest, descriptive statistics were calculated and compared between SS and CBM acquisition methods. Mean SUVs between groups were calculated as well as percent differences in standard deviation with the following formula used to calculate percent difference:
% Difference = (StdCBM-StdSS)/StdCBM
Qualitative comparison
All routine PET/CT protocols were updated to use CBM acquisition methods with CBM acquisition protocols matched to our standard SS protocols using manufacturer recommended settings for comparable imaging times as shown in Figure 3. Radiology reports were examined and any claims regarding altered image quality or anomalies were recorded along with any verbal complaints or concerns received during this time. This study was carried out over an approximate 14 week period with over 420 patient datasets acquired during that time period. Seventy-eight samples were examined from the 420 patient datasets to achieve a 10% confidence interval with a 95% confidence level.
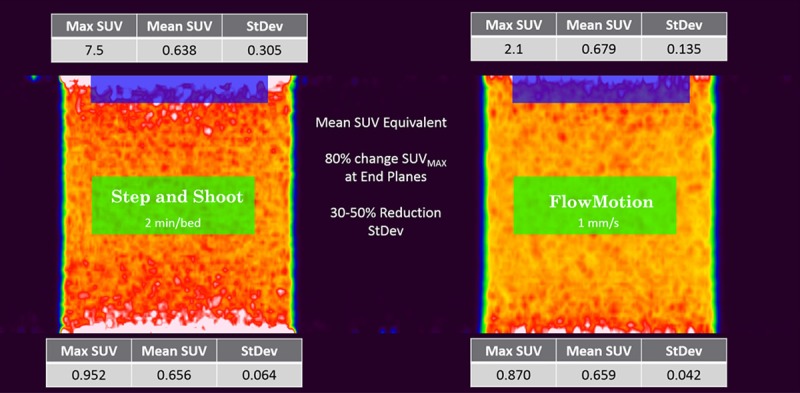
Figure 3.
Shows the manufacturer recommended conversion between traditional and continuous bed motion imaging. The numbers shown are based on a standard sized patient using a 10 mCi injection of FDG with axial coverage of 90 cm. The blue line indicates the conversion plot for a 3 ring system while the pink line indicates the conversion for a 4 ring system.
A visual comparison was performed by qualified imaging professionals comprised of three physicians (1-nuclear medicine and radiology board certified, 1-first year resident, and 1-fourth year radiology board-eligible resident). Visual comparisons were based on overall physician impression of images between the two modes of acquisition. A basic questionnaire was used to assess physician opinions of the image data compared between SS and CBM. This questionnaire assessed the physicians’ opinions regarding comparative image quality and preference between the two datasets presented. Table 1 provides the list of questions given in this survey along with answer expectations.
Table 1.
Survey questions given to 3 physician readers of varying experience. These questions were intended to assess basic opinions regarding comparative image quality between the two scan types
| Question | Answer Type | Additional Comments Allowed |
|---|---|---|
| Did findings differ between the two presented datasets? If yes, please provide more details | Yes/No | Yes |
| Please rate the similarity between the two cases presented | Leikert scale: 1-5 | No |
| • 1: Not at all Similar | ||
| • 2: Somewhat Similar | ||
| • 3: Moderately Similar | ||
| • 4: Very Similar | ||
| • 5: Extremely Similar | ||
| Which of the two images presented do you prefer? | Multiple choice: 1, 2, or 3 | No |
| • 1: Data acquired 1st | ||
| • 2: Data acquired 2nd | ||
| • 3: No preference because of similarity between images |
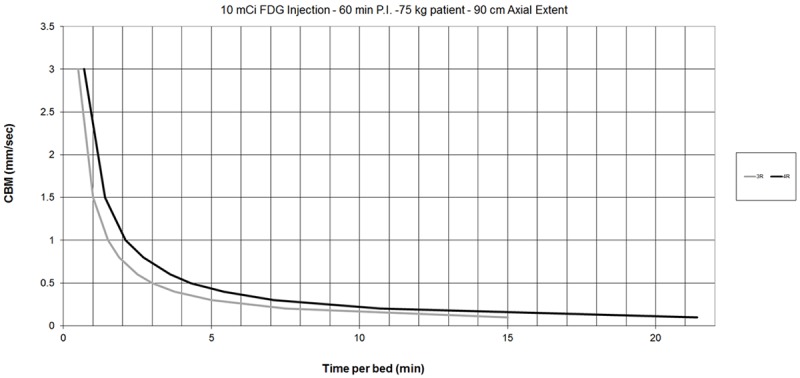
For the visual comparison, a total of 50 patients presenting with various forms of disease were imaged using both SS and CBM acquisition methods. Step & shoot per bed acquisition times ranged from 1-1.5 min/bed while clinically used CBM speeds ranged from 0.8-2 mm/s. Because differences in uptake times can result in changes to SUV measurements, the first 30 patients in this study first received a standard step & shoot scan followed immediately by a CBM acquisition. For the next set of 30 patients, the workflow was reversed with the step & shoot acquisition following the CBM acquisition. On average, each subsequent acquisition was performed within 12 minutes from the start of the initial step & shoot acquisition or CBM acquisition. Figure 4 shows example images from each series of data collection. Following collection of scan data, physicians were asked to randomly choose 20 patients from each group to make their assessment of image quality and preference.
Figure 4.
Shows examples of images taken from data acquired for the visual comparison portion of this study. The top images shows the comparison of images when step and shoot was acquired first followed by continuous bed motion. The bottom image shows the comparison when continuous bed motion acquisition occurred before step and shoot imaging.
Results
Phantom data comparison
Phantom data results indicated mean SUVs calculated for all regions to be 6.39 for SS and 6.47 for single bed speed CBM and 6.45 for variable speed CBM with an average of 6.44±0.04. The average standard deviation for all datasets was 2.96±0.01. There was no significant difference detected between mean SUV, t(12)=-1.08, p>0.05, for standard SS compared to single-speed CBM techniques, nor was any statistical difference seen comparing SS to variable-speed CBM imaging, t(12)=-0.89, p>0.05.
Standard deviation analysis in the uniform phantom scans equalized to equivalent scan time over a 90 cm axial range, showed statistically significant reductions in standard deviation for both comparisons with t(4)=-12.5, p<0.001 for the 6.25 minute acquisition and t(4)=-17.5, p<0.001 for the 10 minute acquisition. CBM acquisitions reduced standard deviation measurements by an average of 8% for fast protocols and nearly 4% for slower imaging studies. CBM acquisition modes were also observed to have a lower percentage increase in noise per change in acquisition time with CBM noise increasing by 7% with each 1 minute decrease in scan time while SS modes increased in noise by 8.6% per 1 minute decrease in scan time.
Results from regions of interest drawn in the end planes of the cylindrical phantom placed on the edges of a single bed position field of view indicated nearly equivalent mean values of 0.638 and 0.679 (~6% difference) for SS and CBM techniques respectively. The standard deviation within this end plane region was reduced by 55.7% from 0.305 to 0.135 when using CBM while max SUV measurements were reduced by 72% from 7.5 to 2.1. Mean SUV from a region drawn centrally in the same phantom yielded nearly equivalent values of 0.656 and 0.659 (0.45% difference) for SS and CBM respectively with a 34% reduction in standard deviation when using CBM methods. Max SUV measurements in this region were nearly the same showing a difference of only 8%.
Clinical patient data assessment
Quantitative assessment
Results from region of interest analysis in clinical patient data comparing the two acquisition methods are shown in Table 2. Data acquired using SS followed by CBM had an average SUV of 1.88 for all regions acquired using step and shoot with a 95% confidence interval of 1.62-2.15. CBM acquired data showed an average SUV of 1.94 with a 95% confidence interval of 1.63-2.24. Data acquired with CBM prior to SS had an average SUV of 1.93 for CBM acquisitions with a 95% confidence interval of 1.78-2.07 while the step and shoot technique resulted in an average SUV of 1.89 for all regions with a 95% confidence interval of 1.76-2.03. For all regions measured, mean values were similar with overlapping confidence intervals. Mean values were shown to not differ statistically (t(11)=1.41, p>0.05) for SS compared to single-speed CBM or for SS compared to variable-speed CBM (t(11)=0.022, p>0.05).
Table 2.
indicates SUV measurements from WB, Liver, Spine, and All regions within the patient for all acquisition orders. Average values as well as 95% confidence intervals are shown for CBM and SS protocols in each group
| SS-CBM | ||||||||
|
| ||||||||
| CBM | SS | |||||||
|
|
||||||||
| WB | Liver | Spine | All | WB | Liver | Spine | All | |
|
| ||||||||
| Average | 1.13 | 2.21 | 2.47 | 1.94 | 1.15 | 2.25 | 2.25 | 1.88 |
| Upper 95% CI | 1.21 | 2.42 | 3.27 | 2.24 | 1.23 | 2.46 | 2.92 | 2.15 |
| Lower 95% CI | 1.06 | 1.99 | 1.67 | 1.63 | 1.08 | 2.04 | 1.57 | 1.62 |
|
| ||||||||
| CBM-SS | ||||||||
|
| ||||||||
| CBM | SS | |||||||
|
|
||||||||
| WB | Liver | Spine | All | WB | Liver | Spine | All | |
|
| ||||||||
| Average | 1.18 | 2.33 | 2.26 | 1.92 | 1.16 | 2.21 | 2.33 | 1.90 |
| Upper 95% CI | 1.24 | 2.47 | 2.47 | 2.06 | 1.23 | 2.36 | 2.57 | 2.05 |
| Lower 95% CI | 1.13 | 2.18 | 2.05 | 1.78 | 1.09 | 2.06 | 2.09 | 1.76 |
|
| ||||||||
| Group Averages | ||||||||
|
| ||||||||
| CBM | SS | |||||||
|
|
||||||||
| WB | Liver | Spine | All | WB | Liver | Spine | All | |
|
| ||||||||
| Average | 1.16 | 2.28 | 2.34 | 1.93 | 1.16 | 2.23 | 2.30 | 1.89 |
| Upper 95% CI | 1.21 | 2.40 | 2.67 | 2.07 | 1.21 | 2.35 | 2.60 | 2.03 |
| Lower 95% CI | 1.12 | 2.16 | 2.01 | 1.78 | 1.11 | 2.10 | 2.00 | 1.76 |
Standard deviation comparisons between lesion data showed a slight decrease overall when using CBM imaging compared to SS when CBM acquisition modes were used as the baseline. When the first scan in the series was SS, the difference was significant, with the greatest reduction observed being 97%, however, the average reduction in all regions as well as a single ROI placed over the whole body was approximately 8%.
Qualitative assessment
Radiology reports examined showed no signs of concerns regarding data quality. For the 75 reports sampled from 420 datasets, no comments indicated any peculiarities in findings. During the testing period, no communications were received regarding concerns about altered PET/CT image quality. Final post hoc 95% confidence intervals were calculated to be ±2%.
Formal comparison of clinical images acquired using SS and CBM technology yielded no substantial changes to findings related to disease between presented images. Differences in bowel uptake, excretion patterns and background were noted in approximately 50% of the patient population. This difference was most likely because of the average 12 minute delay between scans resulting in minor physiological changes. Nearly 75% of responses from readers indicated improvements to the quality of images in the end planes. For the most experienced reader, 45% of CBM studies were flagged as having improved tumor to background ratios in ROIs as well as overall improved visual contrast when using CBM vs. SS.
Assessment of physician ratings of similarity indicated an average score of 4.73±0.6 for the SS→CBM group and 5.0±0 for the CBM→SS group. These results reflect the opinion that the images were extremely similar when compared side-by-side. The lowest similarity rating given for any of the 120 case combinations presented was a 3 indicating that the images were moderately similar. Ninety percent of all responses for all groups (108/120) were rated a five on the Leikert scale, indicating extreme similarity between presented cases. Responses for preference between case studies presented corroborated results from similarity results.
In the SS→CBM comparison, 70% (42/60) of responses indicated no preference in images because of similarity while 25% (15/60) preferred CBM and only 5% (3/60) preferred SS. Results from the CBM→SS comparison indicated 83% (50/60) of responses preferred the CBM acquisition with 13% indicating no preference and 3% preferring SS. Only 4% (5/120) of all responses indicated a preference for SS images compared side-by-side to CBM. Differences between mean preference ratings for SS→CBM were 2.65 indicating a strong preference for CBM or no preference. Mean preference ratings for CBM→SS were 1.3 indicating a strong preference for CBM over other options. Differences between groups were found to be statistically significant (t(114)=11.6, p<0.001). Odds ratio analysis indicated that when the order of acquisition was CBM followed by SS, physicians were 92% less likely to choose SS over CBM (OR=0.008, 95% CI=0.001-0.052) and were 89% less likely to choose No Preference over CBM (OR=0.011, 95% CI=0.003-0.046).
Discussion
All assessments indicated that image quality, quantitative measures, and physician preference using CBM imaging was as good as or better than SS imaging with significant improvements especially observe with regard to noise characteristics, uniformity, and end plane imaging. Quantitative assessments comparing CBM and SS indicated no difference between mean SUVs calculated for phantom or clinical patient studies. This shows quantitative consistency, regardless of the acquisition method chosen. This result is extremely important for validating SUV reliability as this new technology proliferates and imaging centers begin using this new functionality.
Noise assessments showed statistically significant improvements when using CBM techniques. Not only were the improvements statistically measureable, but were visually perceived by physicians performing qualitative assessments of patient data. This was found to be true in body phantoms, uniform phantoms, and clinical patient data illustrating that the uniform axial sensitivity of CBM acquisition modes translates to realizable benefits with regard to noise. Interestingly we were also able to show that the rates of change in noise with increasing bed speed or decreased acquisition times results in slower rates of change when using CBM techniques further demonstrating improvements over standard SS imaging.
Physician assessments of image quality yielded consistent results indicating a significant preference for CBM imaging over SS acquired data regardless of which scan was performed first. Physician comments regarding their preference were taken after the survey and indicated that their preference was often based on opinions that the images appeared to be more uniform when comparing CBM versus SS images. An example of this is that two of the physicians noted that the body outline of the patients in the CBM studies was more uniform throughout the image. Based on our observations, we believe that CBM acquisition types may provide a more uniform patient outline as seen during routine axial slice examinations of the data. This provides a consistent reference point for visual assessment through the axial extent of the patient but requires further study to assess this hypothesis.
Conclusions
CBM technology requires a change in the way we think about PET imaging. In the past, we have had to think in terms of time per bed and number of beds to determine image quality and scan time. SS imaging also makes it challenging to compare imaging protocols between manufacturers as each vendor has a different axial FOV as well as varying overlap between beds. As this technology is adopted, the use of single bed speed indications is potentially more powerful and robust in terms of assessing trade-offs between scan time and image quality as well as potentially improving the ease with which PET imaging protocols can be compared between manufacturers. Routine clinical imaging using CBM shows promise as a new technology that may improve on a number of basic performance aspects of traditional step and shoot PET/CT imaging.
Disclosure of conflict of interest
No external financial disclosures.
References
- 1.Ceccarini G, Flavell RR, Butelman ER, Synan M, Willnow TE, Bar-Dagan M, Goldsmith SJ, Kreek MJ, Kothari P, Vallabhajosula S, Muir TW, Friedman JM. PET Imaging of Leptin Biodistribution and Metabolism in Rodents and Primates. Cell Metabolism. 2009;10:148–159. doi: 10.1016/j.cmet.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marik J, Tartis MS, Zhang H, Fung JY, Kheirolomoom A, Sutcliffe JL, Ferrara KW. Long-circulating liposomes radiolabeled with [18F] fluorodipalmitin ([18F] FDP) Nucl Med Biol. 2007;34:165–171. doi: 10.1016/j.nucmedbio.2006.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Del Guerra A, Belcari N. Molecular Imaging of Small Animals: Instrumentation and Applications. In: Zaidi H, editor. Molecular Imaging of Small Animals: Instrumentation and Applications. New York: Springer; 2014. pp. 337–365. [Google Scholar]
- 4.Chatziioannou A, Silverman RW, Meadors K, Farquhar TH, Cherry SR. Techniques to improve the spatial sampling of MicroPET-a high resolution animal PET tomograph. Nuc Sci IEEE Tran on. 2000;47:422–427. [Google Scholar]
- 5.Thompson CJ, Labuda A, Joonyoung S. Improving the spatial resolution of the microPET scanner by wobbling the bed. IEEE Nuc Sci Conf Rec. 2005:1636–1640. [Google Scholar]
- 6.Joon Young S, Thompson CJ, Labua A, Goertzen AL. Evaluation of the Spatial Resolution Improvement of the MicroPET R4 Scanner with a Wobbling Bed. Nuc Sci Conf Rec. 2006:2480–2483. [Google Scholar]
- 7.Dahlbom M, Yu D, Cherry S, Chatziioannou A, Hoffman E. Methods for improving image quality in whole body PET scanning. IEEE Trans on Nuc Sci. 1992;39:1079–1083. [Google Scholar]
- 8.Dahlbom M, Cutler PD, Digby WM, Luk WK, Reed J. Characterization of sampling schemes for whole body PET imaging. Phys Med Biol. 2013;58:7391–418. [Google Scholar]
- 9.Dahlbom M, Reed J, Young J. Implementation of true continuous 2D/3D whole body PET scanning. IEEE Nuc Sci Conf Rec. 2001 [Google Scholar]
- 10.Brasse D, Newport D, Carney JP, Yap JT, Reynolds C, Reed J, Bao J, Luk P, Michel C, Townsend DW. Continuous bed motion acquisition on a whole body combined PET/CT system. Nuc Sci Conf Rec. 2002:951–955. [Google Scholar]
- 11.Townsend DW, Reed J, Newport DF, Carney JPJ, Tolbert S, Newby D, Yap JT, Long MJ. Continuous bed motion acquisition for an LSO PET/CT Scanner. IEEE Nuc Sci Conf Rec. 2004 [Google Scholar]
- 12.Burbar Z, Michel C, Towsend D, Jakoby B, Sibomana M, Kehren F, Tolbert S, Reed J, Hubner K, Abidi M. Continuous bed motion data processing for a resolution LSO PET/CT scanner. Nuc Sci Conf Rec. 2005:2046–2048. [Google Scholar]
- 13.Newport DF, Casey ME, Luk WK, Reed JH, inventors. Continuous tomography bed motion data processing apparatus and method. United States Patent. 2005
- 14.Saha GB. Basics of PET imaging: physics, chemistry, and regulations. New York: Springer; 2010. [Google Scholar]
- 15.Zhang J, Hall N, Zhang B, Liu X, Knopp M, Tung C, Knopp M. Optimizing PET volume overlap in time-of-flight PET/CT acquisition. Soc Nuc Med. 2013 [Google Scholar]
- 16.Phelps M, Cherry S, Dahlbom M. PET: Physics, Instrumentation, and Scanners. New York: Springer; 2006. [Google Scholar]