Abstract
We report a 31-year-old woman with end-stage cervical carcinoma who suffers both lower intestinal and vaginal bleeding. A selective internal iliac arteriogram demonstrated pseudoaneurysm formation in the vaginal branch of the left internal iliac artery. There was also a fistula between the pseudoaneurysm and the lower intestinal segments. Selective transcatheter coil embolization was performed, and the bleeding was treated successfully. We conclude that the internal iliac artery should be evaluated first in patients with advanced pelvic malignancy when searching for the source of lower gastrointestinal (GI) bleeding. Additionally, transcatheter arterial embolization is a safe and effective treatment technique.
Keywords: Angiography, Coil embolization, Hemorrhage, Lower gastrointestinal bleeding, Transcatheter
Özet
Eş zamanlı vajinal ve alt intestinal kanamalı son dönem servikal kanseri bulunan 31 yaşındaki kadın hastanın transkateter koil embolizasyonunu sunuyoruz. Hastanın selektif iliak arteriogramında sol internal iliak arterinin vajinal dalında yalancı bir anevrizma formasyonu ve yalancı anevrizma ile alt intestinal segmentlerde fistül traktı gözlenmesi üzerine anjiografik girişim planlandı. Selektif koil embolizasyonu ile kanama başarılı olarak tedavi edildi.Olgudan çıkardığımız sonuç ileri evre pelvik malignitesi olan hastalardaki alt intestinal kanamalarda öncelikle internal iliak arter çalışılmalıdır. Embolizasyon tedavileri de gelişen teknoloji ile birlikte oldukça başarılı hale gelmiştir.
Introduction
Although both rectal and vaginal bleeding can be caused by arterial hemorrhage, their etiologies are different. Colonic diverticulosis, angiodysplasia, neoplasms, infections, and inflammatory bowel disease are the most common disorders associated with rectal bleeding. Malignant tumor extension, infection, surgery and pelvic radiation are the most frequent etiologies of vaginal bleeding. In patients with advanced pelvic malignancy, vaginal and lower intestinal bleeding can be observed simultaneously. Because the pelvic vascular anatomy of these patients can change due to the many dysplastic arterial structures, arterioarterial or arteriovenous fistulas and pseudoaneurysm formations can result from surgical treatments, tumor extension, infections and pelvic radiation [1, 2]. The angiographic approach is a noninvasive and safe treatment method for these clinic conditions [3–7].
Case Report
A 31-year-old woman with inoperable stage IIIB cervical carcinoma was admitted to our emergency department with an altered mental status and a history of rectal and vaginal bleeding. She had a blood pressure of 90/60 mmHg, a heart rate of 86 beats/min and a respiratory rate of 22 breaths/min. Her first diagnosis had been established two years prior to this hospital admission, and she had undergone total abdominal hysterectomy, bilateral oophorectomy, pelvic radiation and systemic chemotherapy. Six months later, a diverting colostomy was performed for the treatment of proctitis. She developed recurrent disease and received a second course of systemic chemotherapy three months prior to the current admission. After the first clinical evaluation, she was referred to our interventional radiology unit for possible arterial embolization. An abdominal aortogram and selective angiographies of the superior mesenteric artery (SMA) and the inferior mesenteric artery (IMA) were performed, all of which were negative for the source of bleeding. Then, we performed a pelvic arteriogram, and a pseudoaneurysm of the vaginal branch of the left internal iliac artery was observed. Additionally, a fistulous communication between lower intestinal structures and the pseudoaneurysm was observed during the angiography (Figure 1). Coil embolization to stop the bleeding was planned, and two pushable coils (5×20–30) (Cook’s) were used to occlude the feeding vessel of the pseudoaneurysm. There was no contrast filling in the pseudoaneurysm on the control angiograms (Figure 2). In the following two weeks, there was no complaint of vaginal or rectal bleeding by the patient, and her vital signs were stable in this period. We discharged her two weeks after the inpatient admission.
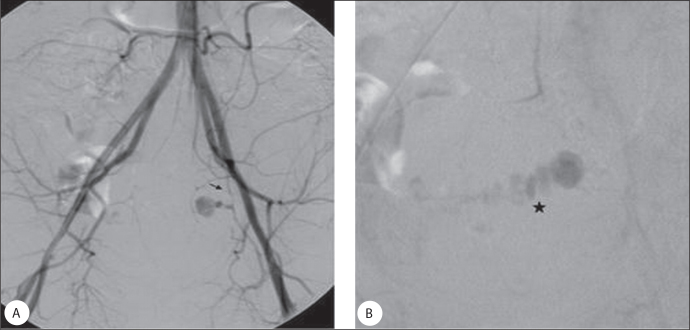
Figure 1.
A) A pseudoaneurysm that measured 13.5×15.5 mm can easily be seen on non-selective pelvic DSA after distal abdominal injection. The feeding artery of this pseudoaneurysm is the vaginal branch of left internal iliac artery (arrow). B) The fistulous formation between the pseudoaneurysm and the lower intestines views on the following angiogram (star).
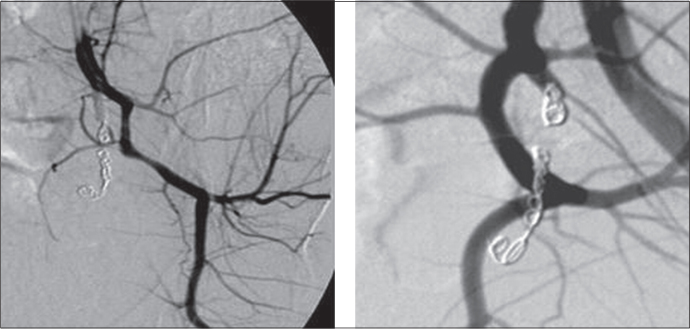
Figure 2.
After the coil embolization, pseudoaneurysm and the fistulous formation is not seen on the following angiograms.
Discussion
SMA and IMA are the most common sources of rectal bleeding, including some cases of severe rectal bleeding. The celiac artery (CA) can also be a source of hemorrhage [8]. Lower intestinal bleeding that arises from the branches of the internal iliac artery (IIA) is very rare, and we typically see this kind of hemorrhage in patients who have advanced pelvic malignancies. Finding the source of the bleeding is very difficult in these patients because we have to study the abdominal aorta, CA, SMA, IMA, common iliac artery and IIA. We must keep in mind that the IIA can be the source of the lower GI bleeding, and angiographic studies should begin with injections into the IIA in patients with advanced pelvic malignancy.
The surgical treatment of pelvic hemorrhage secondary to pelvic malignancy is a great challenge. The effects of pelvic irradiation, large tumor size, and the insufficient ligation of hypogastric arteries are the most common difficulties [9, 10]. Pelvic irradiation makes the vascular structures very fragile, and the fibrosis of surrounding tissues after pelvic irradiation is one of the dissection problems for the surgical approach. A hematoma may play a life-saving role due to its local tamponading effect; the surgical aspiration of such a hematoma is frequently contraindicated due to its protective role. The recurrence of bleeding is also a common problem due to the advanced pelvic collaterals and dysplastic arteries. Arterial access for approaching the distal arteries should always be maintained, but after an insufficient surgical ligation of the hypogastric arteries, no arterial access points for transarterial embolization could be identified, making an angiographic process impossible [11].
The transcatheter arterial embolization of the internal iliac arteries was first described by Margolies and Ring in 1972 and 1973, respectively [12, 13]. The indications of this treatment method have recently increased, and now it is commonly applied to the management of intractable hemorrhage due to traumatic, congenital, neoplastic and iatrogenic conditions [14–20].
Karanicolas et al. reported that almost half of angiograms reveal the source of lower gastrointestinal bleeding, and that half of the patients continue to bleed during their inpatient period [21]. We think that the management of lower gastrointestinal bleeding should also include selective angiography of the IIA, especially for patients with pelvic neoplasms or for patients who have had pelvic irradiation so that the diagnostic ratio of angiography can be increased.
The transarterial embolization of pelvic and mesenteric vessels is not a perfect treatment method. It has some advantages and some disadvantages. It is a safe, minimally invasive technique that can be completed repeatedly. The disadvantages of this technique are with the use of ionizing radiation and the inability to identify extravasations under the rate of 1 ml/s. however, this technique can be life saving in patients who have massive bleeding due to advanced pelvic malignancy. We think that transarterial embolization is the treatment of choice for patients with pelvic neoplasms who have vaginal or intestinal bleeding.
Pseudoaneursyms are caused by the inadequate healing of damaged vessels related to surgery or trauma. Blood flow continues to dissect the tissues around the damaged artery and forms a saccular dilatation that communicates with the damaged artery [22–24]. Although an untreated pseudoaneurysm can expand or rupture, pseudoaneurysms can be easily treated with transarterial embolization. [22–27]. Gelfoam, polyvinyl alcohol particles (PVA), detachable balloons, coils and covered stents can all be used for embolization. Due to the risk of shunting of the polyvinyl alcohol particles (PVA) into the systemic circulation, coils have some advantages for the occlusion of the proximal large feeding arteries [28]. We occluded the feeding artery of the pseudoaneurysm using coils, and we observed no complications.
In conclusion the management of lower intestinal bleeding in patients with advanced pelvic malignancy is a challenge. The decision should be made immediately because this is a time-sensitive and life-threatening condition. For these reasons, before mesenteric angiography, an internal iliac artery angiogram should be studied in patients with advanced pelvic malignancy. Transcatheter arterial embolization is a safe and effective treatment technique that can be applied during the same session.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Spinosa DJ, Angle JF, McGraw JK, Maurer EJ, Hagspiel KD, Matsumoto AH. Transcatheter Treatment of Life-Threatening Lower Gastrointestinal Bleeding Due to Advanced Pelvic Malignancy. CardioVasc and Int Radiol. 1998;21:503–5. doi: 10.1007/s002709900312. [DOI] [PubMed] [Google Scholar]
- 2.Reuter SR, Redmond C, Cho KJ. Gastrointestinal Angiography. WB Saunders; Philadelphia: 1986. pp. 282–338. [Google Scholar]
- 3.Inaba Y, Arai Y, Ino S, Matsueda K, Aramaki T, Takaki H. Transcatheter Arterial Embolization for External Iliac Artery Hemorrhage Associated with Infection in Postoperative Pelvic Malignancy. J Vasc Interv Radiol. 2004;15:283–7. doi: 10.1097/01.rvi.0000116192.44877.46. [DOI] [PubMed] [Google Scholar]
- 4.Matsunaga N, Hayashi K, Aikawa H, et al. Transcatheter arterial embolization for perforation of the external iliac artery. Nippon Igaku Hoshasen Gakkai Zasshi. 1987;47:1287–92. [PubMed] [Google Scholar]
- 5.De Baere T, Ousehal A, Kuoch V, Sapoval M, Lagrange C, Roche A. Endovascular management of bleeding iliac artery pseudoaneurysms complicating radiation therapy for pelvic malignancies. AJR Am J Roentgenol. 1998;170:349–53. doi: 10.2214/ajr.170.2.9456944. [DOI] [PubMed] [Google Scholar]
- 6.Husted J, Dempsey D. Angiographic management of arteriocolic fistulae. Cardiovasc Intervent Radiol. 1986;9:158–60. doi: 10.1007/BF02577928. [DOI] [PubMed] [Google Scholar]
- 7.Lukens ML, Cardella JF, Fox PS. Progressive arteriocolonic fistulization following pelvic irradiation. J Vasc Interv Radiol. 1995;6:615–8. doi: 10.1016/s1051-0443(95)71146-0. [DOI] [PubMed] [Google Scholar]
- 8.Browder WB, Cerise FJ. Litwin MS. Impact of emergency angiography in massive lower gastrointestinal bleeding. Ann Surg. 1986;204:530–6. doi: 10.1097/00000658-198611000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith DC, Wyatt JF. Embolization of the hypogastric arteries in the control of massive vaginal hemorrhage. Obstet Gyneco. 1977;49:317–22. [PubMed] [Google Scholar]
- 10.Siegel P, Mangert WF. Internal iliac artery ligation in obstetrics and gynecology. JAMA. 1961;178:1059–62. doi: 10.1001/jama.1961.03040500001001. [DOI] [PubMed] [Google Scholar]
- 11.Heaston DK, Mineau DE, Brown B J, Miller FJ. Transcatheter arterial embolization for control of persistent massive puerperal hemorrhage after a bilateral surgical hypogastric artery ligation. A JR. 1979;133:152–4. doi: 10.2214/ajr.133.1.152. [DOI] [PubMed] [Google Scholar]
- 12.Margolies MN, Ring EJ, Waltman AC, Kerr WS, Baum S. Arteriography in the management of hemorrhage from pelvic neoplasms. N Engl J Med. 1972;287:317–21. doi: 10.1056/NEJM197208172870701. [DOI] [PubMed] [Google Scholar]
- 13.Ring ES, Athanasoulis C, Waltman AC, Margolies MN, Baum S. Arteniographic management of hemorrhage following pelvic fractune. Radiology. 1973;109:65–70. doi: 10.1148/109.1.65. [DOI] [PubMed] [Google Scholar]
- 14.Lang EK. Transcatheter embolization of pelvic vessels for control of intractable hemorrhage. Radiology. 1981;140:331–9. doi: 10.1148/radiology.140.2.7196055. [DOI] [PubMed] [Google Scholar]
- 15.Ayella RJ, Du Priest RW, Jr, Khaneja SC. Transcatheter embolization of autologous clotin the mangement of bleeding associated with fractures of the pelvis. Sung Gynecol Obstet. 1978;147:849–52. [PubMed] [Google Scholar]
- 16.Lang EK, Deutsch JS, Goodman JR, Barnett TF, Lanasa JA, Jr, Duplessis GH. Transcatheter embolization of hypogastnic branch antenies in the management of intractable bladder hemorrhage. J Urol. 1979;121:30–6. doi: 10.1016/s0022-5347(17)56648-3. [DOI] [PubMed] [Google Scholar]
- 17.Carmignani G, Belgrano E, Puppo P, Chichero A, Giuliani L. Treatment of bladder hemorrhage due to inoperable pelvic cancers by embolization of the hypogastnic arteries. Radiol. 1979;60:423–8. [PubMed] [Google Scholar]
- 18.Lang EK, Pisco JM. Transcatheter embolization of hypogastnic branch arteries in the management of intractable bladder hemorrhage. Interventional Radiology. 1980:102–4. doi: 10.1016/s0022-5347(17)56648-3. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein HM, Medellin H, Ben-Menachen Y, Wallace S. Transcatheter arterial embolization in the management of bleeding in the cancer patient. Radiology. 1975;115:603–8. doi: 10.1148/15.3.603. [DOI] [PubMed] [Google Scholar]
- 20.Faysal M. Angiognaphic management of post-prostatectomy bleeding. J Urol. 1979;122:129–31. doi: 10.1016/s0022-5347(17)56284-9. [DOI] [PubMed] [Google Scholar]
- 21.Karanicolas PJ, Colquhoun PH, Dahlke E, Guyatt GH. Mesenteric angiography for the localization and treatment of acute lower gastrointestinal bleeding. Can J Surg. 2008;51:437–41. [PMC free article] [PubMed] [Google Scholar]
- 22.Kwon JH, Kim GS. Obstetric Iatrogenic Arterial Injuries of the Uterus: Diagnosis with US and Treatment with Transcatheter Arterial Embolization. RadioGraphics. 2002;22:35–46. doi: 10.1148/radiographics.22.1.g02ja0735. [DOI] [PubMed] [Google Scholar]
- 23.Bromley PJ, Clark T, Weir IH, Zwirewich CV. Radiologic diagnosis and management of uterine artery pseudoaneurysm: Case report. Can Assoc Radiol J. 1997;48:119–22. [PubMed] [Google Scholar]
- 24.Zimon AE, Hwang JK, Principe DL, Bahado-Singh RO. Pseudoaneurysm of the uterine artery. Obstet Gynecol. 1999;94:827–30. doi: 10.1016/s0029-7844(99)00229-x. [DOI] [PubMed] [Google Scholar]
- 25.Pelage JP, Soyer P, Repiquet D, et al. Secondary postpartum hemorrhage: treatment with selective arterial embolization. Radiology. 1999;212:385–9. doi: 10.1148/radiology.212.2.r99jl05385. [DOI] [PubMed] [Google Scholar]
- 26.Langer JE, Cope C. Ultrasonographic diagnosis of uterine artery pseudoaneurysm after hysterectomy. J Ultrasound Med. 1999;18:711–4. doi: 10.7863/jum.1999.18.10.711. [DOI] [PubMed] [Google Scholar]
- 27.Ball RH, Picus D, Goyal RK, Wilson DB, Rader JS. Ovarian artery pseudoaneurysm: Diagnosis by Doppler sonography and treatment with Transcatheter embolization. J Ultrasound Med. 1995;14:250–2. doi: 10.7863/jum.1995.14.3.250. [DOI] [PubMed] [Google Scholar]
- 28.Novak D. Embolization materials. In: Dondelinger RF, Rossi P, Kurdziel JC, Wallace S, editors. Interventional radiology. New York, NY: Thieme; 1990. pp. 295–313. [Google Scholar]