Abstract
Tracheobronchial injury is one of cases which are relatively uncommon, but must be suspected to make the diagnosis and managed immediately. In such a case, primary initial goals are to stabilize the airway and localize the injury and then determine its extend. These can be possible mostly with flexible bronchoscopy conducted by a surgeon who can repair the injury. Most of the penetrating injuries occur in the cervical region. On the other hand, most of the blunt injuries occur in the distal trachea and right main bronchus and they can be best approached by right posterolateral thoracotomy. The selection of the manner and time of approaching depends on the existence and severity of additional injuries. Most of the injuries can be restored by deploying simple techniques such as individual sutures, while some of them requires complex reconstruction techniques. Apart from paying attention to the pulmonary toilet, follow-up is crucial for determination of anastomotic technique or stenosis. Conservative treatment may be considered an option with a high probability of success in patients meeting the criteria, especially in patients with iatrogenic tracheobronchial injury.
Keywords: Trachea, bronchus, injury
Özet
Trakeobronşiyal yaralanmalar göreceli olarak daha nadir görülen, ancak tanı konulabilmesi için şüphelenilmesi gereken ve sıklıkla anında müdahale gerektiren durumlardır. Bu durumda ilk yapılması gereken iki önemli amaç vardır; havayolunun stabilizasyonu ve yaralanmanın lokalizasyonu ve genişliğinin belirlenmesidir. Bunlar da sıklıkla yaralanmayı tedavi edebilecek bir cerrah tarafından yapılan fiberoptik bronkoskopi ile mümkün olur. Penetran yaralanmaların çoğu servikal bölgede olur. Künt yaralanmaların çoğu ise distal trakea ve sağ ana bronşda olur ve en iyi sağ posterolateral torakotomi ile yaklaşılır. Yaklaşım şeklinin seçimi ve zamanı ek yaralanmaların varlığı ve trakeobronşiyal yaralanmanın şiddetine bağlıdır. Yaralanmaların çoğu tek tek suturler kullanılarak yapılan basit tekniklerle onarılabilirken bazıları kompleks rekonstruksiyon teknikleri gerektirir. Pulmoner temizliğe dikkat edilmesi yanında anastomotik teknik veya stenozun tesbit edilmesi için takip önemlidir. Özellikle iatrojenik yaralanmalı hastalarda konservatif tedavi yaklaşımları da kabul edilebilir bir yaklaşım seçeneği olmaktadır.
Introduction
Tracheobronchial injuries (TBI) are rare but potentially life-threatening injuries. They rather comprise injuries that occur between the cricoid cartilage and right and left main-stem tracheal bifurcation. The position of trachea, mandible relative, sternum and vertebral column protect itself from injuries. While there might be death caused by asphyxia at the moment of injury, sequel respiratory tract tightness may develop later as a result of lack of recognition or incorrect management. Penetrating injuries may occur due to blunt/ penetrating traumas or projectile injuries to the neck or chest. On the other hand, blunt injuries can occur from a variety of direct or indirect traumas. Although TBIs were previously accepted as absolutely fatal injuries, as a result of the development of prehospital ambulatory care and regional trauma units, there has been an apparent increase in the incidence of patients with airway injuries reaching ER alive which was the cause of high diagnosis rate. The main condition of a successful treatment of TBI is prompt recognition and appropriate surgical approach.
Only 0.5% of patients with multiple injuries, who are managed in modern trauma centers, are diagnosed with tracheobronchial injuries [1]. While 3–6% of penetrating neck injuries consist of injuries of cervical trachea, such rate is less than 1% in penetrating chest trauma [2, 3]. In general, 1–2% of patients with thoracic trauma have penetrating trachea-bronchial trauma [2, 4]. On the other hand, the TBI incidence in blunt traumas was reported as 2.8% out of 1178 patients dying due to blunt trauma in the autopsy series [3]. Most of the injuries due to blunt trauma involve the intrathoracic trachea and mainstem bronchi. The frequency of injury rates are as follows: cervical trachea 4%, distal thoracic trachea 22%, right mainstem bronchus 27%, left proximal mainstem bronchus 17%, complex injury within trachea and mainstem bronchi 8% and lobar orifices 16% [4].
Mechanism of injury
Most TBIs occur as a result of blunt and penetrating traumas, other than the rare causes such as iatrogenic injuries, burn or caustic injuries (Figure 1). The causes of most penetrating injuries are the perforating tools or fire guns. Due to the deep localization of the intrathoracic trachea, almost all of trachea injuries caused by stab are located in the cervical site. Knife injuries cause tearing or cutting effect resulting in perforation, linear laceration or transsection [2] (Figure 2).
Figure 1. a–d.
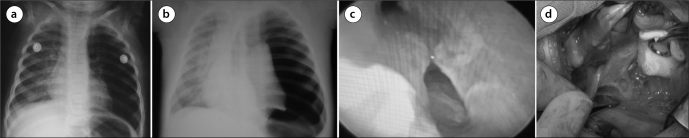
Six-month-old boy. Organic foreign body aspiration. Hyperinflation in the left lung (a). Organic foreign body was extracted by rigid bronchoscopy from the left bronchial system. Post-bronchoscopy X-ray revealed pneumothorax on the left side (b). Bronchial perforation (15 mm) was seen by re-bronchoscopy (c). Perforated part of left main bronchus was repaired by interrupted 4/0 monofilament absorbable sutures through a right mini thoracotomy (d).
Figure 2. a–c.
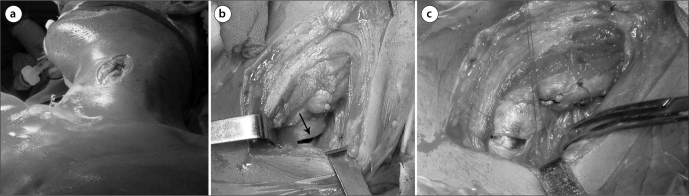
Twenty-two y/m. Air leakage from the penetrating wound was seen in the left side of the neck. 4 cm long laceration of the cervical trachea on the left side was repaired by monofilament absorbable sutures.
Gunshot wounds are the most frequent causes of penetrating TBIs and they might occur in any region of respiratory tract. Because of the fatal injuries of heart or great vessels associated with the penetrating injuries of distal trachea making impossible for such patients to reach to the trauma center, 75–80% of penetrating tracheal traumas still consist of cervical injuries [2]. Gunshot wounds produce a crush injury. The wound cavity changes depending on the speed, caliber and bullet type of the gun. Serious damages are caused by high-velocity rifles which cause much larger cavitation and much more damage in the soft tissues compared to those caused by the low-velocity guns.
Blunt traumas of cervical trachea are mostly caused by a direct trauma or sudden hyperextension. Direct cervical traumas cause bruise type injuries in the trachea as a result of the impact from hard and stable vertebral bodies. This typically occurs in the hyperextension of the automobile driver’s neck in sudden head crashes. The neck smashes into the steering wheel or the front dash-board are called as “dash-board” injuries [5]. Elevated safety belt causes compressive and rotational impact to the neck from the front in automobile accidents similar to clothesline-type injuries. The other injuries causing traction and distraction with the result of laryngotracheal separation may occur mostly due to sudden hyperextension.
Three theories have been proposed regarding the exact mechanism for blunt intrathoracic TBIs [6]. One is the sudden and forceful anteroposterior compression of the chest and it is the most frequent injury type that causes tracheobronchial disruption. This leads to an increase in the transverse diameter which pulls the lungs apart at the carina. Second one involves compression of the chest and trachea while the glottis is closed. This produces a rapid increase in airway pressure, especially in the trachea and larger bronchi. When the pressure exceeds the elasticity of the tracheobronchial tree, the airway ruptures usually at the membranous portion. The third theory relates to rapid deceleration injuries where shearing forces occur at the relative fixation points such as cricoid cartilage and carina. This mechanism of injury seems the most logical in the current population of blunt trauma victims, the majority of whom are involved in motor vehicle accidents. Since the left mainstem bronchus is fixed with major vessels, it can be partially protected. However, as the supporting structures are less in the right mainstem bronchus and heavier right lung on the shorter right main bronchus, mostly right mainstem bronchus ruptures are encountered in such mechanism. Some investigators have found equal frequency of right-sided and left-sided injuries [7]. The acuity of the presentation of a patient with a right-sided injury may be related to a higher incidence of associated injuries. Right-sided injuries may also be detected earlier because injuries to the left bronchus are more protected by adjacent structures in the mediastinum.
Penetrating airway traumas are frequently associated with significant injuries of adjacent cervical and intrathoracic structures. Penetrating cervical tracheal injuries are associated with esophageal injuries (28%), hemopneumothorax (24%), carotid artery and jugular venous injuries (13%), recurrent laryngeal nerve injuries (8%), cervical spine and spinal cord injuries (3%) and larynx injuries. On the other hand, intrathoracic penetrating trauma of trachea may be accompanied by hemopneumothorax 32%, esophageal injuries (11%), major vascular injuries (18%), cardiac injuries (5%), spinal cord injuries (7%), intra-abdominal injuries (18%), as well as left recurrent nerve, ascending and descending aorta and pulmonary arteries [8].
Blunt traumas are generally accompanied not only by chest, but also abdomen, head and orthopedic structures. Therefore, a more detailed examination must be done on the patient in terms of such structures. Head, facial or cervical spine injuries are frequent and they are important indicators of mortality and morbidity. 40–100% of patients with blunt airway traumas have additional major injuries and most of them consist of orthopedic injuries. Almost half of them have facial trauma, pulmonary contusions or intra-abdominal injuries. 10-20% of the patients have major closed-head injuries and approximately 10% of them have additional spinal cord injuries [9,10]. Furthermore, 50% vocal cord dysfunction affiliated with recurrent nerve injuries have been reported in patients with blunt airway injuries [11].
Diagnosis
TBIs have the first priority in trauma. The diagnosis of airway pathology must be immediately established and the first stage treatments must be immediately applied due to their critical importance and urgency in stabilizing the patient. Nevertheless, TBIs are not diagnosed immediately in 25% to 68% of the patients [7]. Dyspnea and respiratory distress are frequent symptoms occurring in 76–100% of the patients [8, 10]. The other frequently (46%) seen symptoms are hoarseness or dysphonia [11]. Stridor and dyspnea are the common signs of tracheal stenosis. Air leakage from a penetrating wound in the neck is pathognomonic finding for airway laceration and it is seen in approximately 60% of patients with penetrating injury of cervical trachea [12]. Ceasing cervical air leakage after intubation verifies the diagnosis.
Routine radiological studies such as chest and cervical spine X-ray are the most useful of early diagnostic methods in the initial trauma survey. 60% of the patients with TBI’s have deep cervical emphysema and pneumomediastinum, 70% of them have pneumothorax. A high quality cervical spine or chest X-ray may show the separation in the tracheal or bronchial air column. Over-inflation of endotracheal tube cuff or displacement of endotracheal tube is an additional radiological finding [13]. Complete separation of the mainstem bronchus may result in the classic findings of atelectasia; “absent hilum” or collapsing of the lung away from the hilum towards to diaphragm known as “falling lung sign of Kumpe” [14]. Pneumothorax, which persists along with the excessive air leakage, should increase the suspicion of intrathoracic tracheal or bronchial injury.
Computerized tomography (CT) of the neck and upper chest is of critical importance for the precise diagnosis of laryngeal injuries, but its role in tracheobronchial injuries have not been determined accurately [5]. However, thorax CT sustains its validity in approaching trauma and it is extremely valuable in investigating the existence of possible great vessel injuries or mediastinal hematoma. The CT scan may show mediastinal air, separation in the tracheobronchial air column, respiratory tract deviation or specific location of the separation. In the patient, who is hemodynamically unstable or whose respiratory tract is unstable, the CT scan is contra-indicated. Negative CT does not obviate the need for bronchoscopy or other diagnostic transactions. In some cases, CT bronchography or virtual bronchoscopy may be helpful [15]. Since the esophagus injuries frequently associated, especially after penetrating trauma, contrast esophagogram is mostly necessary [16]. Angiography of the aortic arch or cervical vessels can be used in stable patients with major suspicion for great vessel or aortic injury.
If the initial diagnosis of airway injury is missed, granulation tissue and stricture of the trachea or bronchus develop within the first 1 to 4 weeks and usually leads to symptoms, signs and radiologic findings of pneumonia, bronchiectasis, atelectasis and abscess. This development usually leads to nonfunctional lung tissue distal to the area of stenosis, even if the airway can be restored. However, when the airway is completely obstructed, the distal lung is often filled mucus and protected from infection. These patients do not have parenchymal destruction, but instead maintain functional pulmonary tissue beyond the point of obstruction (Figure 3).
Figure 3. a–d.
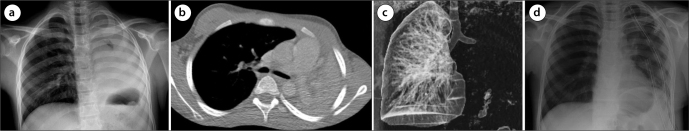
15 y/m. He had a history of traffic accident. Rigid bronchoscopy was performed due to left atelectasis (a, b). Total obstruction of the left main bronchus was seen via rigid bronchoscopy (c). The distal stenotic segment of the left main bronchus was resected and end-to-end anastomosis was performed by left thoracotomy. Postoperatively X-ray (d).
Bronchoscopy provides the single definitive diagnostic study in a patient with suspected airway injury. Laryngoscopy, which is applied by an otolaryngologist, is a crucial part of endoscopic study in cervical trauma or suspected laryngeal injury. Careful examination of the tracheobronchial tree with the fiberoptic bronchoscopy provides information about the location and extend of injury. The advantages of fiberoptic bronchoscopy are that it can be applied easily and quickly even in the accompanying neck-head or cervical spine injuries. If bronchoscopy is to be applied in an intubated patient, the endotracheal tube must be carefully withdrawn in order not to miss out proximal tracheal injury.
Initial airway management
The first and most important priority in acute TBIs is to ensure adequate airway. Patients with distress and clinical suspicion of airway injury must be immediately intubated preferably under the guidance of flexible bronchoscopy. Patients with air leakage from a penetrating cervical injury may be intubated through the neck directly to the tracheal lumen. It is reported that this method is applied in approximately 25% of penetrating cervical injuries [10]. Tracheostomy is mostly unnecessary. Airway control may be the best choice in patients with severe maxillofacial trauma, immediate tracheostomy. A transsected cervical trachea may retract into the mediastinum. In such cases, the best way is to place finger to the mediastinum in front of the esophagus and to locate the distal trachea by palpation, and then to grip it with clamp and ensure distal intubation by withdrawing it to the cervical wound [16].
Management of the injuries of distal trachea, carina and proximal mainstem bronchi can be extremely challenging. Close cooperation between the anesthesiologist and surgeon is critical to the successful treatment of TBIs. In most cases, single lumen tube is not sufficient but safe. Because of their rigidity and size, the use of double-lumen tubes should be avoided. They might increase the extension of wound. In such cases, a long endotracheal tube must be placed beyond the injury location or on a suitable main bronchus in order to ensure single lung ventilation. In some selected cases, endobronchial blocker or carefully passed double lumen tube may be required. In hemodynamically stable patients, high frequency jet ventilation ensures an efficient option for ventilation during the reconstruction of airway, because the air is distributed with a smaller and less rigid catheter and it ensures easier placement of sutures. Nevertheless, in many cases, sterile tubes placed from operative field or the standard oral intubation are sufficient.
Unless accompanied by heart or great vessels injuries, cardiopulmonary by-pass (CPB) is never necessary for the management of isolated airway injuries. After a major trauma, CPB may exacerbate intracerebral or intra-abdominal hemorrhage and may cause ARDS with systematic inflammatory response. In patients, who cannot be extubed due to additional injuries, the operation must be concluded with a large-bore, single lumen endotracheal tube to allow good pulmonary toilet and to use fiberoptic bronchoscopy if necessary. In major maxillofacial o laryngeal injuries, if long term ventilation is necessary, tracheostomy must be placed after tracheobronchial restoration is completed. Tracheostomy may contaminate the suture line and cause tearing apart and stenosis, and therefore it should not be close to the tracheal restoration [16].
Surgical treatment
It may not be possible to recognize minor injuries due to distal intubation, conducted quickly during the stabilization of the patient with multiple injuries or clinically unsuspected. Such minor injuries may heal without negative sequela and without requiring surgical repair, if they are in the form of linear laceration, and if they involve less than one third of the diameter of airway. The mucosal defects where the lung reexpansion is fully ensured and which does not have a continuing air leakage may also heal without requiring an early intervention. However, after such injuries, granulation and structure may develop in some cases that require late correction.
The traditional treatment for TBIs has been surgery. However, it was estimated that the maximum tracheal injury length that can be treated conservatively was 4 cm or less. But should not in itself be the main factor that influences the choice of one treatment over another. The strict adherence to certain selection criteria (vital sign stability, no evidence of esophageal injury, no open tracheal injury, no evidence of difficulty with mechanical ventilation if intubation is needed, no development of subcutaneous or mediastinal emphysema, and no signs of sepsis related to iatrogenic TBI) should be the only factor [17–19]. In patients, who cannot be approached conservatively, the most appropriate treatment is the surgical treatment as early as possible. The essences of surgical treatment is debridement of devitalized tissue including cartilage, end to end anastomosis with absorbable sutures, flexion of the neck to avoid anastomosis line tension and supporting the suture line with the adjacent structures. The proximal half of trachea can be reached by low collar incision which ensures excellent exposure to vascular or esophageal injuries in the neck. “T” incision over the manubrium and the separation of manubrium through the second intercostal space leads to reach middle third of the trachea and to provide proximal control of innominate artery and vein. The distal third of the trachea, carina and right mainstem bronchus, azygous vein, superior vena cava, right atrium and most of intrathoracic esophagus can be easily approached by a right thoracotomy. Left thoracotomy provides a good exposure to the left main-stem bronchus, distal part of aortic arch, descending thoracic aorta and proximal left subclavian artery. Nevertheless, it is hard to reach to the proximal left mainstem bronchus, carina, distal trachea or right mainstem bronchus through a left thoracotomy because of the overlying aortic arch.
Since heart and great vessels are located anterior to the distal trachea, carina and proximal mainstem bronchi, the penetrating injuries in the chest are most probably accompanied by life-threatening cardiovascular injuries. While median sternotomy ensures optimal access to the hearth and major veins, it is less beneficial for trachea, carina and bronchi. Also, it does not provide appropriate exposure for the restoration of additional esophageal injuries. Bilateral thoracosternotomy or “Clamshell” incision conducted from the fourth intercostal space ensures good exposure to mediastinum and both hemithorax. However, this approach makes much less contribution to the airway exposure compared to the incisions previously described.
Simple clean lacerations without airway devascularization can be repaired with simple interrupted absorbable sutures. Generally 4-0 multifilament or monofilament absorbable sutures are preferred. In cases with serious tracheobronchial damage, all devitalized tissue should be debrided with the care of preserving as much viable airway as possible. In such cases, circumferential resection and end-to-end anastomosis is almost always preferable to partial wedge resection and primary restoration of traumatized airway [20]. The dissection is limited with the region to be resected in order to preserve the tracheobronchial blood supply to the area of anastomosis. Correct placement of absorbable interrupted sutures ensures airtight anastomosis and eliminates the discrepancy between the distal and proximal airway. It also ensures minimal anastomotic granulations.
In many serious tracheal injuries, primary resection and reconstruction can be made without encountering any difficulty. The wide injuries of carina are more problematic and should be repaired rather than resected, if possible. Only 3–4 cm part of airway including carina can be resected and allowed for reconstruction. For a tension-free anastomosis, various tracheobronchial releasing maneuvers have been used. For limited tracheal resections, blunt dissection of anterior avascular pretacheal area is sufficient along with the neck flexion. For wider proximal tracheal resections, suprahyoid laryngeal releasing can be ensured in 1–2 cm as supplement to the proximal releasing. For main bronchus or carina resections, opening the pericardium around the inferior part of hilum ensures 1–2 cm mobilization of distal airway [21].
The accompanying esophagus injuries should be restored in two layers. Vascularized muscle or tissue flap must be placed between the trachea and esophagus. Intrathoracic tracheobronchial suture line is wrapped preferably with a pedicled pericardial fat, intercostal muscle or pleura, with the aim to separate the airway anastomosis from the closest blood vessels. Respiratory track’s mobility is ensured using a neck flexion which is maintained by “guardian suture” placed between the chin and sternum in the postoperative period. The patients with isolated airway injuries are extubated in the operating room even after complex reconstructions.
In early postoperative period, because of the difficulty of clearing secretions past the anastomotic line, aggressive pulmonary toilet is necessary. For the patients with vocal cord paralysis, mini tracheostomy allowing to make direct tracheal aspiration is helpful. There could be a difficulty in elevating the larynx during deglutition in patients with tracheal resection, including associated recurrent nerve injuries or suprahyoid laryngeal release. In the remaining cases, postoperative care is like the one in thoracotomy for pulmonary resection. In ventilated patients, endotracheal balloon must take place in the distal or proximal edge of tracheal suture. Such patients should be treated with the lowest possible airway pressures allowing sufficient oxygenation and ventilation, and should be extubated as soon as possible. Bronchoscopy should usually be performed 7 to 10 days after tracheobronchial repair or prior to discharge to assure satisfactory healing without granulation tissue.
Complications
The complications of tracheobronchial repair consists mostly of anastomotic problems. After tracheal reconstruction, 5–6% of the patients have anastomotic dehiscence, or restenosis occurs [22]. The initial treatment involves securing the airway endotracheal T-tube until healing is completed. Most of these patients may undergo subsequent airway resection and reconstruction 3 to 6 months after the first restoration [23]. Trachea-innominate artery fistula is rare, but frequently fatal and requires immediate operation. Tracheoesophageal fistula can usually be managed firstly by gastric drainage, enteral nutrition and treatment of pneumonia. When the patient is stabile and no longer requires ventilatory support, tracheal and esophageal defect is resected or restored, and vascularized tissue is placed to the suture line. If the vocal cord paralysis is permanent, lateralization and medicalization procedures can be used.
Late diagnosis
There are three reasons for delaying of treatment in patients after TBIs. First, the initial injury might be very small and it may have been missed during urgent and intermediate trauma approaches. Second, serious additional injuries may have prevented the full and early treatment of recognized airway injury. Third, the first attempts may be unsuccessful resulting in dehiscence or late stenosis. In all of these, the sequel is similar. Even if the respiratory tract separates partially or wholly, they may be held together to sustain airway and ventilation through its strong peritracheal connective tissue. Although the primary injury or secondary dehiscence heals, the granulation tissue and scar contracture result with subsequent stricture formation usually develops 1 to 4 weeks after injury [24].
These patients may initially have dyspnea on exertion, wheezing, stridor, cough, difficulty in secretion cleaning or recurrent respiratory infections. The history of trauma or prolonged intubation with any one of these symptoms should increase the suspicion of a late airway stenosis that should be diagnosed by bronchoscopy. 50% decrease in the diameter of trachea results in dyspnea only with significant exertion. The diameter of tracheal lumen decreases to less than 25%, dyspnea and stridor occur also at rest. Patients can be compensated despite serious stenosis reasonably, but small amount of airway edema or secretions may deteriorate the contraction as much as threatening the life. Bronchoscopy should be conducted immediately both for evaluation and for dilatation once recognized the critical airway stenosis [25]. The appropriate and definitive treatment for most of these patients is tracheal and bronchial resection with reconstruction. Except the patients with distal lung destruction by chronic infection, reestablishment of ventilation to lung parenchyma can be expected even years after the injury. Preoperative perfusion scanning could show little or no apparent function, but this is attributable to the reflex pulmonary vasoconstriction and is corrected through the ventilation. In such cases, first of all, the respiratory tract reconstruction must be considered. Pulmonary resection must be reserved for the patients with unreconstructable lesions or those with destroyed parenchyma from chronic infection or bronchiectasis.
Iatrogenic tracheobronchial injuries
They are rare, but serious injuries. The most common cause of iatrogenic TBIs is injury after intubation or tracheotomy procedures. The incidence of iatrogenic injuries is 1 in 20000 intubations and higher in the case of double-lumen intubation with an incidence of around 0.5% to 1% [26]. Intubation of patients by inexperienced persons, changing the position of intubation tube without deflation of the tube cuff or over inflation of tube cuff are the causes of injury. Most of them are recognized with dyspnea, subcutaneous emphysema and hemoptysis in the postoperative early period. They are almost always in the membranose part of the trachea. Diagnosis is established with bronchoscopy. The decision of management strategy (conservative/surgical treatment) is similar to the strategy in the other tracheobronchial traumatic injuries [17, 18]. As a different method, it is also possible to repair the membranose rupture of the cervical trachea with transcervical-transtracheal approach. After the membranose part is repaired, anterior trachea incision is closed [27].
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - T.A.; Design - T.A.; Supervision - T.A., A.C.; Funding - Materials - T.A., A.C.; Data Collection and/or Processing - T.A., A.C.; Analysis and/or Interpretation - T.A.; Literature Review - T.A., A.C.; Writing - T.A., A.C.; Critical Review - T.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Gussack GS, Jurkovich GJ, Luterman A. Laryngotracheal trauma: a protocol approach to a rare injury. Laryngoscope. 1986;96:660–5. doi: 10.1288/00005537-198606000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Lee RB. Traumatic injury of the cervicothoracic trachea and major bronchi. Chest Surg Clin N Am. 1997;7:285–304. [PubMed] [Google Scholar]
- 3.Karmy-Jones R, Wood ED. Traumatic Injury to the Trachea and Bronchus. Thorac Surg Clin. 2007;17:35–46. doi: 10.1016/j.thorsurg.2007.03.005. http://dx.doi.org/10.1016/j.thorsurg.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Symbas PN, Justicz AG, Ricketts RR. Rupture of the airways from blunt trauma: treatment of complex injuries. Ann Thorac Surg. 1992;54:177–83. doi: 10.1016/0003-4975(92)91177-b. http://dx.doi.org/10.1016/0003-4975(92)91177-B. [DOI] [PubMed] [Google Scholar]
- 5.Lupetin AR. Computed tomographic evaluation of laryngotracheal trauma. Curr Probl Diagn Radiol. 1997;26:185–206. doi: 10.1016/s0363-0188(97)90011-6. http://dx.doi.org/10.1016/S0363-0188(97)90011-6. [DOI] [PubMed] [Google Scholar]
- 6.Kirsh MM, Orringer MB, Behrendt DM, et al. Management of tracheobronchial disruption secondary to nonpenetrating trauma. Ann Thorac Surg. 1976;22:93–101. doi: 10.1016/s0003-4975(10)63961-6. http://dx.doi.org/10.1016/S0003-4975(10)63961-6. [DOI] [PubMed] [Google Scholar]
- 7.Kiser AC, O’Brein SM, Dettrbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg. 2001;71:2059–65. doi: 10.1016/s0003-4975(00)02453-x. http://dx.doi.org/10.1016/S0003-4975(00)02453-X. [DOI] [PubMed] [Google Scholar]
- 8.Kelly JP, Webb WR, Moulder PV, et al. Management of airway trauma. I: tracheobronchial injuries. Ann Thorac Surg. 1985;40:551–5. doi: 10.1016/s0003-4975(10)60347-5. http://dx.doi.org/10.1016/S0003-4975(10)60347-5. [DOI] [PubMed] [Google Scholar]
- 9.Ramzy AI, Rodriguez A, Turney SZ. Management of major tracheobronchial ruptures in patients with multiple system trauma. J Trauma. 1988;28:1353–7. doi: 10.1097/00005373-198809000-00008. http://dx.doi.org/10.1097/00005373-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Rossbach MM, Johnson SB, Gomez MA, et al. Management of major tracheobronchial injuries: a 28-year experience. Ann Thorac Surg. 1998;65:182–6. doi: 10.1016/s0003-4975(97)01001-1. http://dx.doi.org/10.1016/S0003-4975(97)01001-1. [DOI] [PubMed] [Google Scholar]
- 11.Reece GP, Shatney CH. Blunt injuries of the cervical trachea: review of 51 patients. South Med J. 1988;81:1542–8. doi: 10.1097/00007611-198812000-00019. http://dx.doi.org/10.1097/00007611-198812000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Symbas PN, Hatcher CR, Jr, et al. Bullet wounds of the trachea. J Thorac Cardiovasc Surg. 1982;83:235–8. [PubMed] [Google Scholar]
- 13.Stark P. Imaging of tracheobronchial injuries. J Thorac Imaging. 1995;10:206–19. doi: 10.1097/00005382-199522000-00006. http://dx.doi.org/10.1097/00005382-199522000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Wintermark M, Schnyder P, Wicky S. Blunt traumatic rupture of a mainstem bronchus: spiral CT demonstration of the ‘’fallen lung’’ sign. Eur Radiol. 2001;11:409–11. doi: 10.1007/s003300000581. http://dx.doi.org/10.1007/s003300000581. [DOI] [PubMed] [Google Scholar]
- 15.Jones CM, Athanasiou T. Is virtual bronchoscopy an efficient diagnostic tool for the thoracic surgeon? Ann Thorac Surg. 2005;79:365–74. doi: 10.1016/j.athoracsur.2004.03.013. http://dx.doi.org/10.1016/j.athoracsur.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Mathisen DJ, Grillo H. Laryngotracheal trauma. Ann Thorac Surg. 1987;43:254–62. doi: 10.1016/s0003-4975(10)60608-x. http://dx.doi.org/10.1016/S0003-4975(10)60608-X. [DOI] [PubMed] [Google Scholar]
- 17.Jougon J, Ballester M, Choukroun E, Dubrez J, Reboul G, Velly JF. Conservative treatment for postintubation tracheobronchial rupture. Ann Thorac Surg. 2000;69:216–20. doi: 10.1016/s0003-4975(99)01129-7. http://dx.doi.org/10.1016/S0003-4975(99)01129-7. [DOI] [PubMed] [Google Scholar]
- 18.Gomez-Caro A, Moradiellos FJ, Diaz-Hellin V, et al. Role of Conservative Medical Management of Tracheobronchial Injuries. J Trauma. 2006;61:1426–35. doi: 10.1097/01.ta.0000196801.52594.b5. http://dx.doi.org/10.1097/01.ta.0000196801.52594.b5. [DOI] [PubMed] [Google Scholar]
- 19.Carbognani P, Bobbio A, Cattelani L, et al. Management of postintubation membranous tracheal rupture. Ann Thorac Surg. 2004;77:406–9. doi: 10.1016/S0003-4975(03)01344-4. http://dx.doi.org/10.1016/S0003-4975(03)01344-4. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell JD, Mathisen DJ, Wright CD, et al. Clinical experience with carinal resection. J Thorac Cardiovasc Surg. 1999;117:39–52. doi: 10.1016/s0022-5223(99)70468-x. [discussion: 52-3]. http://dx.doi.org/10.1016/S0022-5223(99)70468-X. [DOI] [PubMed] [Google Scholar]
- 21.Heitmiller RF. Tracheal release maneuvers. Chest Surg Clin N Am. 2003;13:201–10. doi: 10.1016/s1052-3359(03)00031-0. http://dx.doi.org/10.1016/S1052-3359(03)00031-0. [DOI] [PubMed] [Google Scholar]
- 22.Grillo HC, Zannini P, Michelassi F. Complications of tracheal reconstruction: incidence, treatment and prevention. J Thorac Cardiovasc Surg. 1986;91:322–8. [PubMed] [Google Scholar]
- 23.Wright CD, Grillo HC, Wain JC, et al. Anastomotic complications after tracheal resection: prognostic factors and management. J Thorac Cardiovasc Surg. 2004;128:731–9. doi: 10.1016/j.jtcvs.2004.07.005. http://dx.doi.org/10.1016/j.jtcvs.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Taskinen SO, Salo JA, Halttunen PE, et al. Tracheobronchial rupture due to blunt chest trauma: a follow-up study. Ann Thorac Surg. 1989;48:846–9. doi: 10.1016/0003-4975(89)90683-8. http://dx.doi.org/10.1016/0003-4975(89)90683-8. [DOI] [PubMed] [Google Scholar]
- 25.Stephens KEJ, Wood DE. Bronchoscopic management of central airway obstruction. J Thorac Cardiovasc Surg. 2000;119:473–7. doi: 10.1016/S0022-5223(00)70184-X. [DOI] [PubMed] [Google Scholar]
- 26.Borasio P, Ardissone F, Chiampo G. Post-intubation tracheal rupture. A report on ten cases. Eur J Cardiothorac Surg. 1997;12:98–100. doi: 10.1016/s1010-7940(97)00111-5. http://dx.doi.org/10.1016/S1010-7940(97)00111-5. [DOI] [PubMed] [Google Scholar]
- 27.Balcı AE. Trakeobronşiyal yaralanmalar. Türkiye Klinikleri J Surg Med Sci. 2007;3:52–62. [Google Scholar]


