Abstract
Background
Insoles are frequently used in orthotic therapy as the standard conservative treatment for symptomatic flatfoot deformity to rebuild the arch and stabilize the foot. However, the effectiveness of therapeutic insoles remains unclear. In this study, we assessed the effectiveness of therapeutic insoles for flatfoot deformity using subject-based three-dimensional (3D) computed tomography (CT) models by evaluating the load responses of the bones in the medial longitudinal arch in vivo in 3D.
Methods
We studied eight individuals (16 feet) with mild flatfoot deformity. CT scans were performed on both feet under non-loaded and full-body-loaded conditions, first with accessory insoles and then with therapeutic insoles under the same conditions. Three-dimensional CT models were constructed for the tibia and the tarsal and metatarsal bones of the medial longitudinal arch (i.e., first metatarsal bone, cuneiforms, navicular, talus, and calcaneus). The rotational angles between the tarsal bones were calculated under loading with accessory insoles or therapeutic insoles and compared.
Findings
Compared with the accessory insoles, the therapeutic insoles significantly suppressed the eversion of the talocalcaneal joint.
Interpretation
This is the first study to precisely verify the usefulness of therapeutic insoles (arch support and inner wedges) in vivo.
Keywords: Insoles, Three-dimensional Image, Flatfoot, Medial Longitudinal Arch, Loading, CT
1. INTRODUCTION
Flatfoot deformity is characterized by a drop in the medial longitudinal arch, eversion of the hindfoot, and abduction of the forefoot under load (Myerson, 1997; Van Boerum and Sangeorzan, 2003). The standard conservative treatment for symptomatic flatfoot deformity is orthotic therapy with the aid of insoles or ankle foot orthoses (AFOs) or exercise therapy (Wapner and Chao, 1999; Coughlin et al., 2007a). Therapeutic insoles, which are designed to rebuild the arch and stabilize the foot, are commonly used in conservative treatment. However, their reported effectiveness varies (Coughlin et al., 2007b; Alvarez et al., 2006; Lin et al., 2008; Kulcu et al., 2007; Chen et al., 2010) and remains debatable.
A few cadaver studies have used a flatfoot deformity model to evaluate the effectiveness of orthoses based on the load response of the tarsal bones (Imhauser et al., 2002; Kitaoka et al., 2002; Havenhill et al., 2005; Hirano et al., 2009). All of those studies reported improved hindfoot alignment as a result of the orthoses. Recently, in vivo studies have been conducted using video images or markers for motion analysis, but these studies have failed to demonstrate any beneficial effects of orthoses (Kulcu et al., 2007; Chen et al., 2010).
Computed tomography (CT) is currently the most useful method for performing a detailed anatomic analysis of the complex tarsal bones. The kinematics of the hindfoot (Imai et al., 2009) during plantarflexion and dorsiflexion have been analyzed in vivo using subject-based three-dimensional (3D) CT models. The load responses of the hindfoot (Kido et al., 2011) and the medial longitudinal arch (Kido et al., 2013) in patients with flatfoot deformity were also analyzed using subject-based CT models in vivo, and the results indicated that the flat feet dorsiflexed more at the first tarsometatarsal joint and everted more at the talonavicular and talocalcaneal joints under full-body loading in comparison with healthy feet. This method could be powerful for clarifying the effectiveness of therapeutic insoles for flatfoot deformity, based on our hypothesis that therapeutic insoles provide support for the medial longitudinal arch, especially in the first tarsometatarsal, talonavicular, and talocalcaneal joints. The objective of the present study was to quantitatively evaluate the effects of therapeutic insoles for flat feet by analyzing the rotation of the tarsal bones in the medial longitudinal arch in response to load-bearing with and without therapeutic insoles.
2. METHODS
The protocols for this study were all approved by the Institutional Review Board (IRB) (ERB-C-127). Eight subjects were recruited. All of the participants provided written informed consent. Sixteen feet with symptomatic mild flatfoot deformity (four men, age range 29-38 years; four women, age range 26-38 years; mean age 32.1 years (SD 4.8 years)) were studied. Flatfoot deformity was diagnosed by two board certified orthopedic surgeons (specializing in foot and ankle surgery) on the basis of clinical examinations and X-ray images taken under load-bearing conditions. The talo-first metatarsal angle was measured on the lateral projection of the X-ray images. Mild flatfoot was defined as a foot with a talo-first metatarsal angle greater than 4° and less than 15° (mean 8.0° (SD 2.2°), range 5.6-14.0°) (Karasick et al., 1993; Supple et al., 1992).
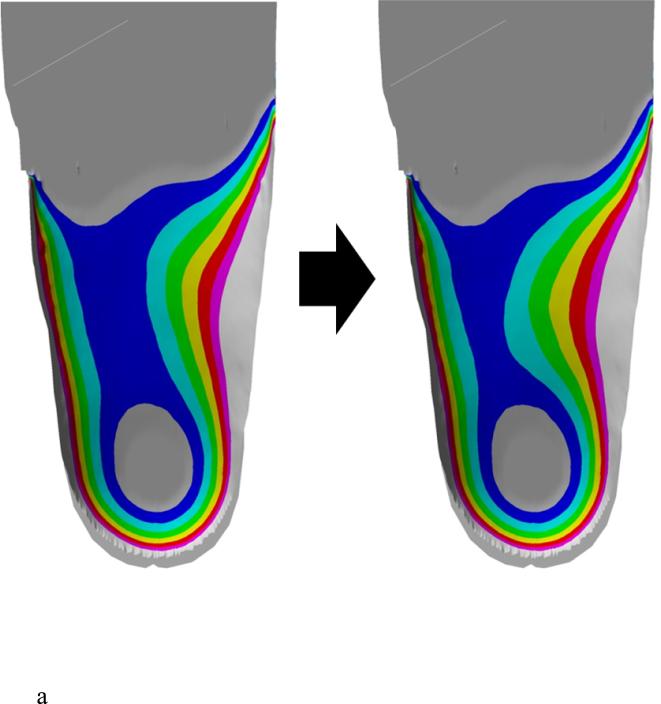
The shoes used in the study were commercially available standard sneakers. The therapeutic insoles were made using a CAD system (Pedcad Insole Designer; Pedcad, Oberkochen, Germany) to make the product quality as uniform as possible (Fig. 1a, 1b). A licensed orthotist supervised the production of the insoles, which were designed to raise the medial longitudinal arch by 10 mm with a 5-mm inner wedge, particularly reducing the burden of the posterior tibial tendon (Fig. 1a).
Figure 1.
Production of therapeutic insoles. a) Therapeutic insoles were mechanically produced using CAD software. The plantar geometry was raised in the medial longitudinal arch by 10 mm with a 5-mm inner wedge by a licensed orthotist (left; before processing, right; after processing). b) Appearance of a therapeutic insole.
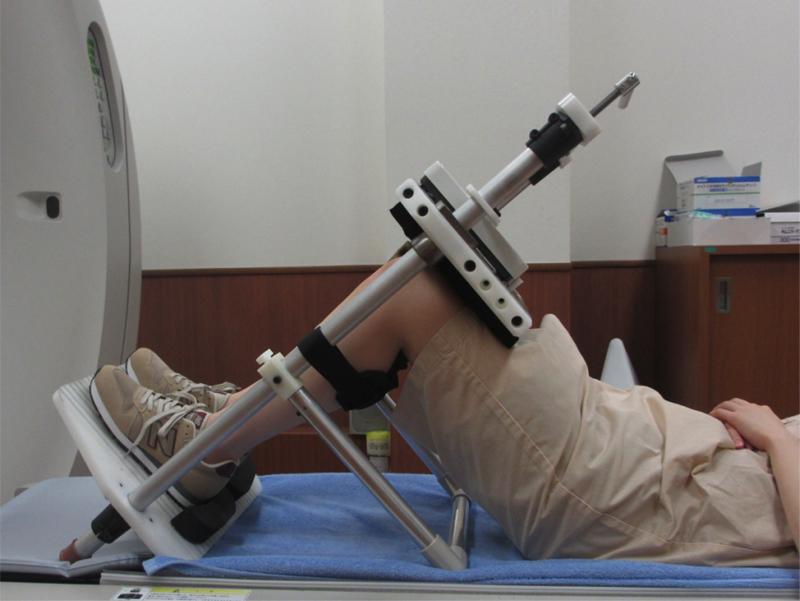
Each subject underwent axial foot CT scanning under non-loaded and full-body-loaded conditions using a custom loading device (Fig. 2) (Kido et al., 2011, 2013). CT images of 0.5-mm thickness were scanned from the sole of the foot to a position 5 cm proximal to the tibiotalar joint. The CT system used was an Aquilion CX64 (0.5 s × 0.5 mm × 64 rows, 120 kV × 45 mA, volume EC, 512 × 512 matrix; Toshiba, Tokyo, Japan). A total of four CT scanning sessions were performed, first with accessory insoles (Condition A) with and without loading and then with therapeutic insoles (Condition B) with and without loading.
Figure 2.
CT scans in the loading condition. Loading was performed with an original loading device as reported in the previous studies.
The resulting CT images were converted to Digital Imaging and Communication in Medicine (DICOM) format and reconstructed using 3D image reconstruction software (Mimics; Materialise, Inc., Leuven Belgium). The threshold level for cortical bone was selected for the tibia segments and each of the individual bones of the medial longitudinal arch (first metatarsal bone, cuneiforms, navicular, talus, and calcaneus).
The rotation of each medial longitudinal arch bone associated with loading was measured using a validated volume merge method (Imai et al., 2009; Kido et al., 2011, 2013; Ochia et al., 2006; Watanabe et al., 2012). A validated volume merge method was used for 3D-3D registration of the tarsal and metatarsal bones. In the volume merge method, a tarsal bone or a metatarsal bone in the unloaded position (the moving bone) was virtually rotated and translated toward the same bone in a loaded position (the stationary target). These rotations and translations of the bone were conducted with 0.1° and 0.1 mm increments, respectively, until the moving bone merged with the stationary target in the loaded position. The degree of volume merging was calculated at each transformation using an algorithm previously described, and the transformation was repeated until the maximum degree of volume merging was obtained. The accuracy of the volume merge method was reported to be 0.1 mm in translation and 0.2° in rotation (Ochia et al., 2006).
The rotation of the following bones was assessed: the first metatarsal bone relative to the cuneiforms at the first tarsometatarsal joint; the cuneiforms relative to the navicular at the cuneonavicular joint; the navicular relative to the talus at the talonavicular joint; the calcaneus relative to the talus at the talocalcaneal joint; the talus relative to the tibia at the tibiotalar joint; the first metatarsal bone relative to the talus; and the first metatarsal bone relative to the tibia. The amount of bone rotation between the tarsal bones while wearing accessory (Condition A) and therapeutic (Condition B) insoles was compared. A global X-Y-Z coordinate system corresponding to anatomical axes was used to describe the orientation of the tarsal bones in the unloaded condition (Fig. 3). The Z-axis ran along the tibial shaft through the center of the ankle, and the Y-axis ran parallel to the projection of a line connecting the center of the heel and the second metatarsal head on a plane perpendicular to the Z-axis. The X-axis was determined according to a right-hand rule from the Y-axis and Z-axis. The coronal (XZ) plane, sagittal (YZ) plane, and transverse (XY) plane were defined from these X-Y-Z axes. A local coordinate system was defined for each tarsal bone with its origin at the centroid of each bone and the same orientation as the X-Y-Z axes. The rotations of the tarsal bones and metatarsal bones under loading were expressed using Eulerian angles in a transverse plane-sagittal plane-frontal plane (Z-X-Y) sequence (Glasoe et al., 2014). Dorsiflexion, eversion, and abduction were designated by a plus sign, and plantar flexion, inversion, and adduction were designated by a minus sign (Imai et al., 2009; Kido et al., 2011, 2013). The results are expressed as the mean ± standard deviation (SD). Differences in the load response between flat feet with accessory insoles (Condition A) and those with therapeutic insoles (Condition B) were analyzed using an unpaired t-test with Bonferroni's adjustment with a p value of 0.017. A p value of less than 0.05 was considered to be statistically significant.
Figure 3.
X-Y-Z axes. A global X-Y-Z coordinate system corresponding to anatomical axes was used to describe the orientation of the tarsal bones. The rotation of each medial longitudinal arch bone associated with loading was measured.
3. RESULTS
The subjects voiced no complaints of discomfort throughout the experiments.
The notable differences included less eversion of the calcaneus in the coronal plane relative to the talus at the talocalcaneal joint (Condition A: 3.6° (1.5°); Condition B: 2.4° (1.4°), p = 0.0003) in the therapeutic insoles group (Condition B) compared with the accessory insoles group (Condition A) under loading conditions (Table 1).
Table 1.
Comparison of the load response between flat feet with accessory insoles (Condition A) and those with therapeutic insoles (Condition B) at the first tarsometatarsal, cuneonavicular, talonavicular, talocalcaneal, and tibiotalar joints and the talo- and tibio-first metatarsal relationships.
| Condition A | Condition B | Difference | p value | ||
|---|---|---|---|---|---|
| First tarsometatarsal Joint | df+/pf− | 0.9 (1.0°) | 0.7 (0.9°) | −0.2° | 0.7704 |
| ev+/iv− | 0.0 (1.0°) | −0.3 (0.9°) | 0.3° | 0.999 | |
| abd+/add− | −0.1 (1.4°) | 0.0 (0.8°) | 0.1° | 0.999 | |
| Cuneonavicular joint | df+/pf− | 0.8 (1.0°) | 0.7 (0.8°) | −0.1° | 0.999 |
| ev+/iv− | −0.7 (0.9°) | −0.6 (0.9°) | 0.1° | 0.999 | |
| abd+/add− | 0.1 (1.3°) | 0.0 (1.1°) | −0.1° | 0.999 | |
| Talonavicular joint | df+/pf− | 2.1 (1.1°) | 2.0 (1.3°) | −0.1° | 0.999 |
| ev+/iv− | 5.0 (2.5°) | 4.0 (2.7°) | −1.0° | 0.0519 | |
| abd+/add− | 4.3 (3.5°) | 3.6 (2.4°) | −0.7° | 0.999 | |
| Talocalcaneal joint | df+/pf− | 2.1 (1.2°) | 1.8 (1.2°) | −0.3° | 0.6015 |
| ev+/iv− | 3.6 (1.5°) | 2.4 (1.4°) | −1.2°* | 0.0003 | |
| abd+/add− | 2.2 (1.7°) | 2.0 (1.5°) | −0.2° | 0.999 | |
| Tibiotalar joint | df+/pf− | −2.0 (1.2°) | −2.2 (1.4°) | −0.2° | 0.999 |
| ev+/iv− | −0.1 (0.7°) | 0.0 (0.6°) | 0.1° | 0.999 | |
| abd+/add− | −0.6 (2.2°) | −1.1 (1.4°) | −0.5° | 0.6558 | |
| Talo-first metatarsal Relationship | df+/pf− | 3.9 (2.1°) | 3.4 (2.0°) | −0.5° | 0.5367 |
| ev+/iv− | 4.3 (2.5°) | 3.1 (2.5°) | −1.2° | 0.0498 | |
| abd+/add− | 4.1 (3.2°) | 3.4 (2.5°) | −0.7° | 0.8064 | |
| Tibio-first metatarsal Relationship | df+/pf− | 1.8 (1.5°) | 1.2 (1.2°) | −0.6° | 0.2082 |
| ev+/iv− | 4.4 (2.8°) | 3.2 (2.5°) | −1.2° | 0.1221 | |
| abd+/add− | 3.5 (2.7°) | 2.3 (2.4°) | −1.2° | 0.2310 | |
df: dorsiflexion +/ pf: plantarflexion - ev: eversion +/ iv: inversion - abd: abduction +/ add: adduction -
The data are expressed as the mean (SD).
Significant difference: p value < 0.017
4. DISCUSSION
The present study investigated the effect of therapeutic insoles on the changes in the medial longitudinal arch bone associated with loading in vivo. We found that therapeutic insoles significantly suppressed the eversion of the talocalcaneal joint compared with accessory insoles. Kulcu et al. (2007) and Chen et al. (2010) performed gait analyses on flatfoot patients using optical surface marker systems on the feet to investigate the effect of insoles on flatfoot deformity during gait; however, neither study demonstrated the effectiveness of insoles. Several cadaveric studies have been conducted to verify the effectiveness of orthoses in a severe flatfoot deformity model produced by resecting almost all of the soft tissue around the talus (Imhauser et al., 2002; Kitaoka et al., 2002; Havenhill et al., 2005; Hirano et al., 2009). These studies confirmed that some parameters, such as arch and hindfoot alignment, were improved by orthoses in the severe flatfoot deformity model.
Our study investigated custom therapeutic insoles with an additional 5-mm inner wedge for treating patients with mild flatfoot deformity. This is the first study to verify the usefulness of insoles (arch support and inner wedge) in vivo. The results of the present study indicated that the insoles suppressed the eversion of the talocalcaneal joint, which may be the most important problem for flexible flat feet. In this study, the patients experienced an improvement in the deformity, represented by reductions in the rotational angles in 1.2° eversion. The change in the rotational angles attributable to the therapeutic insoles was less than the results reported by Hirano et al. (2009) and Imhauser et al. (2002) using the cadaveric severe flatfoot deformity model. The inclusion of patients with mild flatfoot deformity in the present study and the inherent differences between cadaveric studies and in vivo studies, such as the lack of muscle forces in the cadaveric studies, may have caused the differences in the effectiveness of the orthoses.
Regarding the clinical significance, the reduction in the rotational angles was only slight by 1.2°. Considering the extremely large number of steps or motions other than axial loading that a human takes in daily life, a small amount of bone rotation at each single transition from non-loaded to full-body loaded condition may develop gradually and finally result in a significant change over time. Therefore, the improvements of the deformity observed in this in vivo study, although small, may still have value in the clinical treatment for symptomatic flatfoot deformity.
The measurements in this study were performed on subject-based 3D CT models created by CT images taken under unloaded and loaded conditions. The 3D measurement technique was able to demonstrate the subtle movements of the tarsal bones caused by weight bearing. The present study used the coordinates with orientations corresponding to the conventional anatomical planes. Several studies on the 3D alignment of tarsal bones and metatarsal bones used the local coordinate systems based on the 3D orientation of the individual tarsal bone or metatarsal bone determined by inertial axes of each bone (Ledoux et al., 2006; Glasoe et al., 2013; Glasoe et al., 2014). While these coordinate systems provide refined relative motions at each joint in the foot, the 3D orientation of an individual tarsal bone or metatarsal bone may not always correlate with the anatomical planes, which makes interpreting the results difficult in such cases. Another study defined a local coordinate system using anatomical landmarks set at each tarsal bone or metatarsal bone (Gutekunst et al., 2013). Although this coordinate system provides segmental motion at each joint in the foot in a more clinically relevant manner, determination of the anatomical landmarks appears to require manual selection. A future study will utilize a local coordinate system set at individual joint surfaces of the foot in a standardized manner for better understanding of the segmental motions in the foot.
The present study investigated changes in the medial longitudinal arch under loading. However, this loading condition with a neutral ankle position only mimics a standing condition. Although the evaluation of the effects of the insoles using the subject-based 3D CT model may be limited to semi-static conditions, future studies of different loading conditions, such as the simulated toe-off position in the gait cycle, may be helpful to understand the effectiveness of the insole during gait in patients with flatfoot deformity.
Highlights.
▶ We investigated the effect of therapeutic insoles in patients with mild flatfoot.
▶ We examined tarsal bone rotational angles with accessory and therapeutic insoles.
▶ CT scans were performed on both feet under unloaded and full-body-loaded conditions.
▶ The CT scans were performed with accessory insoles and with therapeutic insoles.
▶ The therapeutic insoles suppressed the eversion of the talocalcaneal joint.
ACKNOWLEDGMENTS
This study was supported in part by MEXT KAKENHI 21500411 and NIH/NCCAM 1R01AT006692-01A1. The authors have no conflicts of interest to declare. We thank T. Kaji for providing helpful comments on the statistical analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27:2–8. doi: 10.1177/107110070602700102. [DOI] [PubMed] [Google Scholar]
- Chen YC, Lou SZ, Huang CY, Su FC. Effects of foot orthoses on gait patterns of flat feet patients. Clin. Biomech. (Bristol, Avon) 2010;25:265–270. doi: 10.1016/j.clinbiomech.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Coughlin MJ, Mann RA, Saltzman CL. Surgery of the foot and ankle. 8th ed. Mosby; St. Louis: 2007a. pp. 1027–1030. [Google Scholar]
- Coughlin MJ, Mann RA, Saltzman CL. Surgery of the foot and ankle. 8th ed. Mosby; St. Louis: 2007b. pp. 140–146. [Google Scholar]
- Glasoe WM, Phadke V, Pena FA, Nuckley DJ, Ludewig PM. An image-based gait simulation study of tarsal kinematics in women with hallux valgus. Phys Ther. 2013;93:1551–1562. doi: 10.2522/ptj.20130025. [DOI] [PubMed] [Google Scholar]
- Glasoe WM, Pena FA, Phadke V. Cardan angle rotation sequence effects on first-metatarsophalangeal joint kinematics: implications for measuring hallux valgus deformity. J Foot Ankle Res. 2014;7:29. doi: 10.1186/1757-1146-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutekunst DJ, Liu L, Ju T, Prior FW, Sinacore DR. Reliability of clinically relevant 3D foot bone angles from quantitative computed tomography. J Foot Ankle Res. 2013;6:38. doi: 10.1186/1757-1146-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havenhill TG, Toolan BC, Draganich LF. Effects of a UCBL orthosis and a calcaneal osteotomy on tibiotalar contact characteristics in a cadaver flatfoot model. Foot Ankle Int. 2005;26:607–613. doi: 10.1177/107110070502600806. [DOI] [PubMed] [Google Scholar]
- Hirano T, McCullough MB, Kitaoka HB, Ikoma K, Kaufman KR. Effects of foot orthoses on the work of friction of the posterior tibial tendon. Clin. Biomech. (Bristol, Avon) 2009;24:776–780. doi: 10.1016/j.clinbiomech.2009.07.009. [DOI] [PubMed] [Google Scholar]
- Imai K, Tokunaga D, Takatori R, Ikoma K, Maki M, Ohkawa H, Ogura A, Tsuji Y, Inoue N, Kubo T. In vivo three-dimensional analysis of hindfoot kinematics. Foot Ankle Int. 2009;30:1094–1100. doi: 10.3113/FAI.2009.1094. [DOI] [PubMed] [Google Scholar]
- Imhauser CW, Abidi NA, Frankel DZ, Gavin K, Siegler S. Biomechanical evaluation of the efficacy of external stabilizers in the conservative treatment of acquired flatfoot deformity. Foot Ankle Int. 2002;23:727–737. doi: 10.1177/107110070202300809. [DOI] [PubMed] [Google Scholar]
- Karasick D, Schweitzer ME. Tear of the posterior tibial tendon causing asymmetric flatfoot: radiologic findings. AJR Am J Roentgenol. 1993;161:1237–1240. doi: 10.2214/ajr.161.6.8249732. [DOI] [PubMed] [Google Scholar]
- Kido M, Ikoma K, Imai K, Maki M, Takatori R, Tokunaga D, Inoue N, Kubo T. Load response of the tarsal bones in patients with flatfoot deformity: in vivo 3D study. Foot Ankle Int. 2011;32:1017–1022. doi: 10.3113/FAI.2011.1017. [DOI] [PubMed] [Google Scholar]
- Kido M, Ikoma K, Imai K, Tokunaga D, Inoue N, Kubo T. Load response of the medial longitudinal arch in patients with flatfoot deformity: in vivo 3D study. Clin. Biomech. (Bristol, Avon) 2013;28:568–573. doi: 10.1016/j.clinbiomech.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitaoka HB, Luo ZP, Kura H, An KN. Effect of foot orthoses on 3-dimensional kinematics of flatfoot: a cadaveric study. Arch. Phys. Med. Rehabil. 2002;83:876–879. doi: 10.1053/apmr.2002.32681. [DOI] [PubMed] [Google Scholar]
- Kulcu DG, Yavuzer G, Sarmer S, Ergin S. Immediate effects of silicone insoles on gait pattern in patients with flexible flatfoot. Foot Ankle Int. 2007;28:1053–1056. doi: 10.3113/FAI.2007.1053. [DOI] [PubMed] [Google Scholar]
- Lin JL, Balbas J, Richardson EG. Results of non-surgical treatment of stage II posterior tibial tendon dysfunction: a 7- to 10-year followup. Foot Ankle Int. 2008;29:781–786. doi: 10.3113/FAI.2008.0781. [DOI] [PubMed] [Google Scholar]
- Ledoux WR, Rohr ES, Ching RP, Sangeorzan BJ. Effect of foot shape on the three-dimensional position of foot bones. J Orthop Res. 2006;24:2176–2186. doi: 10.1002/jor.20262. [DOI] [PubMed] [Google Scholar]
- Myerson MS. Adult acquired flatfoot deformity: treatment of dysfunction of the posterior tibial tendon. Instr. Course. Lect. 1997;46:393–405. [PubMed] [Google Scholar]
- Ochia RS, Inoue N, Renner SM, Lorenz EP, Lim TH, Andersson GB, An HS. Three-dimensional in vivo measurement of lumbar spine segmental motion. Spine. 2006;31:2073–2078. doi: 10.1097/01.brs.0000231435.55842.9e. [DOI] [PubMed] [Google Scholar]
- Supple KM, Hanft JR, Murphy BJ, Janecki CJ, Kogler GF. Posterior tibial tendon dysfunction. Semin Arthritis Rheum. 1992;22:106–113. doi: 10.1016/0049-0172(92)90004-w. [DOI] [PubMed] [Google Scholar]
- Van Boerum DH, Sangeorzan BJ. Biomechanics and pathophysiology of flat foot. Foot. Ankle Clin. 2003;8:419–430. doi: 10.1016/s1083-7515(03)00084-6. [DOI] [PubMed] [Google Scholar]
- Wapner KL, Chao W. Nonoperative treatment of posterior tibial tendon dysfunction. Clin. Orthop. Relat. Res. 1999;365:39–45. doi: 10.1097/00003086-199908000-00005. [DOI] [PubMed] [Google Scholar]
- Watanabe S, Inoue N, Yamaguchi T, Hirano Y, Espinoza Orías AA, Nishida S, Hirose Y, Mizuno J. Three-dimensional kinematic analysis of the cervical spine after anterior cervical decompression and fusion at an adjacent level: a preliminary report. Eur. Spine J. 2012;21:946–955. doi: 10.1007/s00586-011-2090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]