Abstract
Context
Violence, experienced in either childhood or adulthood, has been associated with physical health outcomes including cardiovascular disease. However, the consistency of the existing literature has not been evaluated.
Evidence acquisition
In 2013, the authors conducted a PubMed and Web of Science review of peer reviewed articles published prior to August 2013 on the relation between violence exposure, experienced in either childhood or adulthood, and cardiovascular outcomes. To meet inclusion criteria, articles had to present estimates for the relation between violence exposure and cardiovascular outcomes (hypertension, blood pressure, stroke, coronary disease, or myocardial infarction) adjusted for demographic factors. Articles focusing on violence from TV, video games, natural disasters, terrorism, or war were excluded.
Evidence synthesis
The initial search yielded 2,273 articles; after removing duplicates and applying inclusion and exclusion criteria, 30 articles were selected for review. A consistent positive relation was noted on the association between violence experienced during childhood and cardiovascular outcomes in adulthood (i.e., hypertension, coronary heart disease, and myocardial infarction). Associations across genders with varying types of violence exposure were also noted. By contrast, findings were mixed on the relation between adult violence exposure and cardiovascular outcome.
Conclusions
Despite varying definitions of violence exposure and cardiovascular endpoints, a consistent relation exists between childhood violence exposure, largely assessed retrospectively, and cardiovascular endpoints. Findings are mixed for the adult violence–cardiovascular health relation. The cross-sectional nature of most adult studies and the reliance of self-reported outcomes can potentially be attributed to the lack of findings among adult violence exposure studies.
Introduction
Heart disease remains the leading cause of death in the U.S., and prevention of cardiac disease is a major public health goal.1 A growing body of research suggests that experiencing violence in either childhood or adulthood is associated with cardiovascular disease (CVD). National estimates show that the prevalence of experiencing violence during childhood is high, with 42% experiencing a physical assault in the U.S.2 Furthermore, estimates of family violence against women and children indicate widespread exposure to violence in the home.3 The U.S. state and local child protective services estimate that 681,000 children were victims of some form of maltreatment (i.e., physical abuse, sexual abuse, or neglect) in 2011.4 In addition to being highly prevalent, exposure to violence has been recognized as a significant public health problem.5–7 Children exposed to violence either at home or in the community have been found to express higher levels of negative emotions (anxiety, depressive mood, anger, and hostility) and adverse stress reactivity.8,9
The effects of violence may differ by life course stage. Healthy development of the brain and other organ systems can be derailed under chronic exposure to stress, making children particularly vulnerable to the effects of violence exposure.10 These developmental effects can have long-term consequences on the development of chronic disease including CVD. Violence exposure in childhood has been associated with the development of cardiovascular risk factors in childhood,11 which persist into adulthood.12 Coping by modifying lifestyle factors and engaging in substance use behaviors, during childhood or adulthood, may increase an individual’s CVD risk. However, in adulthood, the cumulative effects of lifestyle and substance use behaviors are relatively less compared to childhood, as the number of years in which risky behaviors are engaged is fewer. Furthermore, given the long developmental process of CVD, adult exposures to violence may operate under different biological mechanisms compared to violence experienced decades earlier. Therefore, the existing literature of violence exposure and CVD is evaluated separately by timing of violence exposure occurring either in childhood or adulthood while recognizing that individuals often experience violence during both periods.
WHO has developed a typology of violence where it is characterized as three different types: self-directed (e.g., suicidal behavior), interpersonal (e.g., family and community), and collective (e.g., political). Rather than including all three typologies, the authors chose to conduct a systematic review of interpersonal violence exposure over the life course and CVD to synthesize extant research. Interpersonal violence, defined as “the intentional use of physical force or power against another person that can result in injury, death, psychological harm, maldevelopment, or deprivation,”13 is considered a proximal and often chronic form of violence that threatens the security and stability of both children and adults and is recognized as a public health problem. This systematic review aims to provide an integrated and unbiased summary of extant research, evaluate the consistency of findings around this topic, and outline next steps for future research. Among relevant studies, vast heterogeneity exists regarding exposure and outcome measures, sample populations, and study designs; thus, a meta-analysis was not conducted at this point.
Methods
Inclusion Criteria
The inclusion criteria for this systematic review required that studies examine the association between violence (experienced at any point in the life course) and one of the outcomes of interest (described below). The manuscript had to be an original report of the association between violence and cardiovascular mortality, morbidity, or cardiovascular indices. Further criteria required that the analyses of violence and the outcome of interest be central to the aims of the study and analyses. The following outcomes were included: coronary heart disease (CHD), myocardial infarction (MI), stroke, hypertension, and blood pressure (BP). Several types of violence exposure were included: intimate partner violence (IPV), child abuse, sexual assault, and physical assault where the perpetrator was a stranger or non-stranger.
Exclusion Criteria
Because the focus was on experiences of interpersonal violence, exposures to natural or man-made disasters, such as earthquakes, terrorist attacks, or combat/war were excluded. Papers that focused on violence in video games, TV, or print media were also excluded. Studies that did not explicitly test the relationship between violence and cardiovascular outcomes, adjusting for sociodemographic factors (at least one of the following: age, gender, or SES), were excluded. Studies that considered aggregate measures of the home environment, but did not examine the association between violence and the outcome of interest separately, were excluded. Studies that did not evaluate CVD as a separate outcome or only assessed inflammatory markers were also excluded.
Search Strategy and Data Extraction
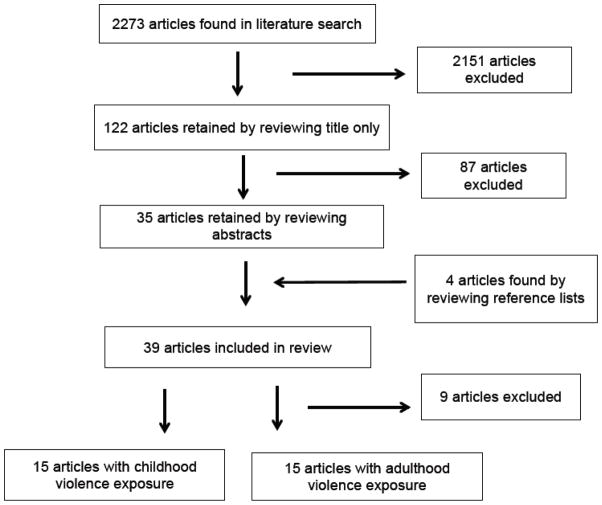
In 2013, using the established exposure and outcome definitions, a literature search was conducted using two electronic databases: Web of Science and PubMed (National Library of Medicine, Bethesda MD). PubMed and Web of Science were searched for the following parameters: Medical Subject Heading (MeSH) terms of either violence, trauma, or abuse, and a second MeSH term including cardiovascular disease, stroke, hypertension, ischemic heart disease, myocardial infarction, blood pressure, or cardiovascular in PubMed and using the Topics option in Web of Science with the same parameters. The search was limited to English studies of humans. The search, through August 2013, yielded 2,273 articles, including duplicates. The titles of these articles were screened and the exclusion criteria were applied. Published systematic reviews and meta-analyses were utilized solely for investigation of references and not otherwise included in the analysis. This stage yielded 122 articles (Figure 1). Abstracts of these articles were screened to discard duplicates of articles, commentaries, and letters or editorials. After review of the abstracts, 35 articles were retained. An additional manual search consisted of screening reference lists of selected relevant articles in order to identify other articles not captured by Web of Science or PubMed searches. This secondary screening yielded an additional four articles of interest, for a total of 39 articles. These articles were read in their entirety to ensure that exposures and outcomes met the inclusion and exclusion criteria. In total, 30 articles merited inclusion in the final review, 15 examining childhood violence exposure and 15 with adulthood violence exposure. Nine articles were excluded at this stage because they did not meet the inclusion/exclusion criteria. Information on developmental period of exposure, sample size and demographics, exposure and outcome assessment, variables used for stratification and adjustment, and findings both of the main association of interest as well as gender-stratified results were extracted when available.
Figure 1.
Itemization of articles included in systematic review
Evidence Grade Criteria
A method for evaluating the quality of the reviewed studies was developed to establish an evidence grade for each study. One point each was assigned for the following four criteria: sample size >500 subjects, prospective follow-up for cardiovascular outcomes, a validated exposure measure (e.g., Revised Conflicts Tactics Scale), and a validated outcome measure (e.g., medical chart review) or an objectively measured outcome (e.g., BP taken by study staff). A higher score indicated higher quality study.
Results
Tables 1 and 2 summarize the 30 publications, organized by whether the violence exposure under evaluation occurred in childhood or adulthood.
Appendix Table 1.
Childhood violence exposure and cardiovascular outcomes, by study design and sample size
| Ref No. |
First Author (Year) |
Sample Size/ Gender/Age |
Study Design/ Setting |
Retrospective/ Prospective Exposure Assessment |
Exposure Measurement |
Self-report/ Objective Outcome Assessment |
Outcome Measure | Results | Evidence Grade |
|---|---|---|---|---|---|---|---|---|---|
| Prospective Studies | |||||||||
| 24 | Rich-Edwards JW (2012) | 66,798 F Mean age: 35 |
Prospective cohort of female nurses in the US | Retrospective assessment of physical and sexual abuse | R-CTS assessment of physical abuse prior to age 18 categorized into none/mild/moderate/severe; sexual abuse prior to age 18 categorized as none, unwanted sexual touching, forced sexual activity | Self-reported CV events with attempted confirmation by medical record review or additional information | CV events defined as MI and stroke (3 levels of case ascertainment: self-reported only, probable/definite by additional information, and definite confirmed by medical record review) with 14 years of retrospective outcome assessment and 4 years of prospective assessment | Severe physical abuse was associated with all CV events (AHR: 1.5, 95% CI: 1.1, 1.9). Forced sex was associated with CV events (AHR: 1.6, 95% CI: 1.2, 2.0), prospective cases (AHR: 1.7, 95% CI: 1.1, 2.6), and definite cases (AHR: 1.4, 95% CI: 1.1, 2.0). | ++++ |
| 25 | Riley EH (2010) | 64,733 F Mean age: 35 |
Prospective cohort of female nurses in the US | Retrospective assessment of physical/sexual abuse in childhood and adolescence | Childhood (up to age 11) and adolescence (ages 11–17): PA assessed with R-CTS (no abuse, mild to moderate, severe as child or teen, severe as both), SA with Gallup survey (no abuse, touched, forced sex as child or teen, forced sex as both) | Self-reported HTN | Physician-diagnosed HTN with 12 years of retrospective assessment and 2 years of prospective assessment | Forced sex as both child and teen was associated with HTN (AOR: 1.2, 95% CI: 1.1, 1.3). Severe physical abuse as both child and teen (AOR: 1.1, 95% CI: 1.1, 1.2) and child or teen (AOR: 1.2, 95% CI: 1.1, 1.3) was associated with increased risk for HTN. | +++ |
| 16 | Roy A (2010) | 444 M/F 60% F Mean age: 29 |
Prospective study of Type 1 diabetics in NJ, USA | Retrospective assessment of childhood emotional, physical, sexual abuse and physical and emotional neglect | CTQ scales assessing childhood emotional, physical, sexual abuse, and physical and emotional neglect; positive responses summed | Medical record review for CVD | Discharge diagnosis of angina pectoris, MI, or stroke within 6 years of follow-up | Number of childhood traumas was significantly associated with the 6-year incidence of any CVD (AOR: 1.2, 95% CI: 1.0, 1.5). | +++ |
| Cross-sectional Studies | |||||||||
| 26 | Afifi TO (2013) | 34,226 M/F Age >20 years |
Cross-sectional representative survey of adults in the US | Retrospective assessment of physical, sexual, and emotional abuse and neglect | Frequency of experiences used to define experiences of physical abuse, emotional abuse and harsh physical punishment. Sexual abuse and neglect defined as any positive response. | Self-reported HTN or CVD | Physician-diagnosed HTN or CVD (angina pectoris, MI, tachycardia) | Childhood maltreatment was associated with HTN (AOR: 1.2, 95% CI: 1.1, 1.3) and CVD (AOR: 1.6, 95% CI: 1.1, 1.8). Harsh physical punishment was associated with CVD (AOR: 1.4, 95% CI: 1.1, 1.8). | + |
| 28 | Stein DJ (2010) | 18,600 M/F 53% F 53% 21–44 yo |
Cross-sectional, representative survey of adults in 10 countries | Retrospective assessment of childhood physical and sexual abuse, neglect, and family violence | Assessment of any physical and at least 3 instance of sexual abuse, neglect, and family violence | Self-reported HTN | Adult onset (age >20), physician-diagnosed HTN | Physical abuse (HR: 1.2, 95% CI: 1.0, 1.5) and family violence (HR: 1.2, 95% CI: 1.0, 1.3) were associated with HTN. No significant association of HTN with sexual abuse or neglect. | + |
| 15 | Dong M (2004) | 17,337 M/F 54% F Mean age: 56 |
Cohort of adults in a health care plan in San Diego, CA, USA | Retrospective childhood abuse and neglect assessment | Childhood emotional and physical abuse (CTS), emotional and physical neglect (CTQ), and sexual abuse prior to age 18 | Self-reported IHD | MI, pain or heavy pressure in chest with exertion, or use of nitroglycerine | Childhood emotional (AOR: 1.7, 95% CI: 1.5–1.9), physical (AOR: 1.5, 95% CI: 1.4–1.9) and sexual (AOR: 1.4, 95% CI: 1.3–1.6) abuse and emotional (AOR: 1.3, 95% CI: 1.1–1.6) and physical (AOR: 1.4, 95% CI: 1.2–1.8) neglect were all associated with IHD. | ++ |
| 27 | Fuller-Thomson E (2010) | 13,093 M/F 52% female 60% <50 yo |
Cross-sectional, representative survey of individuals ≥12 yo in Manitoba & Saskatchewan, Canada | Retrospective childhood physical abuse assessment | Positive response to query on physical abuse prior to age 18 | Self-reported heart disease | Physician-diagnosed heart disease | Childhood physical abuse was associated with self-reported heart disease (AOR: 1.5, 95% CI: 1.0–2.1). | + |
| 23 | Fuller-Thomson E (2012) | 12,863 M/F 60% F 56% <50 yo |
Cross-sectional representative survey of adults in 5 US states | Retrospective assessment of childhood forced sex | Positive response to query on penetrative forced sex prior to age 18 | Self-reported MI | Physician-diagnosed MI | Forced sex was associated with MI in males (AOR: 3.0, 95% CI: 1.1, 7.9) but not females (AOR: 0.9, 95% CI: 0.3, 2.8). | + |
| 22 | Goodwin RD (2004) | 5,877 M/F 50% F Mean age: 33 |
Cross-sectional, representative survey of individuals 15–54 yo in the US | Retrospective assessment of childhood sexual and physical abuse and serious neglect | Positive response to query on sexual abuse (rape or molestation), physical abuse or serious neglect prior to age 18 | Self-reported HTN or cardiac disease | HTN or cardiac disease (heart attack or other serious heart trouble) experienced in the past 12 months | Physical abuse associated with HTN among males (AOR: 1.6, 95% CI: 1.2–2.3). Neglect associated with cardiac disease among females (AOR: 5.7, 95% CI: 2.2, 14.5). Sexual abuse associated with cardiac disease (AOR: 8.5, 95% CI: 2.3, 31.7) and HTN (AOR: 1.6, 95% CI: 1.0, 2.6) among females. | + |
| 19 | Batten SV (2004) | 5,395 M/F 50% F Mean age: 33 |
Cross-sectional, representative survey of adults 15–54 in the US | Retrospective child sexual/physical abuse and neglect assessment | Questions on rape, molestation, physical abuse, and serious neglect | Self-reported CVD | HTN, MI, or stroke | Childhood maltreatment was associated with increased CVD among women (AOR: 8.8, p<.001) but not men (AOR: 0.9, NS). | + |
| 29 | van Reedt Dortland AK (2011) | 2,755 M/F 66% F Mean age: 42 |
Cross-sectional baseline data from a prospective cohort of adults using health care in the Netherlands | Retrospective assessment of emotional neglect, physical, psychological and sexual abuse | Frequency of emotional neglect, psychological, physical, and sexual abuse prior to age 16 assessed by Childhood Trauma Interview | Measured BP and metabolic risk factors | DBP, SBP, HDL, triglycerides, waist circumference, and glucose. Metabolic risk factors were summed to create a metabolic risk score | Emotional neglect was inversely associated with SBP (beta= −0.05, p=.03). History of sexual abuse (beta=0.5, p=.004), physical abuse (beta=0.05, p=.001), and psychological abuse (beta=0.05, p=.001) were associated with metabolic risk score. | +++ |
| 17 | Springer KW (2007) | 2,051 M/F 52% F Mean age: 55 |
Cross-sectional data from a prospective, population-based cohort in WI, USA | Retrospective assessment of child physical abuse | CTS with childhood physical abuse defined as “some” or “a lot” of abuse | Self-reported CV problems | CV problems defined as physician-diagnosed circulation problems, heart trouble, high BP, and high cholesterol | Childhood physical abuse was significantly associated with circulation problems (AOR: 1.5 95% CI: 1.0, 2.2), heart troubles (AOR: 1.5 95% CI: 1.0, 2.2) and high BP (AOR: 1.4, 95% CI: 1.1, 1.9). | ++ |
| 18 | Clark R (2006) | 172 M/F 50% F Mean age: 12 |
Cross-sectional study of healthy African-American teenagers in a Midwestern city in the US | Retrospective assessment of violence in the home and neighborhood | Violence that was heard, seen or experienced in the home or neighborhood was assessed by Screen for Adolescent Violence Exposure scale | Measured BP and heart rate | BP and heart rate before and after a stressor (reactivity) | Violence exposure was inversely related to SBP reactivity (Beta −0.05 SE 0.02) and DBP reactivity (Beta −0.04 SE 0.01). | + |
| 20 | Murali R (2005) | 115 M/F 62% F Mean age: 17 |
Cross-sectional study of adolescents in St. Louis, MO, USA | Retrospective assessment of observed, experienced, and subjective perceptions of violence | Lifetime experiences, observations, and subjective perceptions of violence were summed. Frequency, proximity and severity to violence were evaluated using the Exposure to Violence scale | Measured CV vital signs | HRt, HRV, SBP, DBP measured at baseline and in response to stressor (reactivity) | Total experiences of violence was correlated (r=.22, p<.05) with higher baseline DBP. Higher frequency of experienced violence was correlated with elevated baseline DBP (r=.31, p<.05) and HRt (r=.30, p<.05). Subjective violence score was correlated with baseline SBP (r= −.24, p<.01). Total experiences of violence was associated with decreased SBP (beta= −.14, p<.05) and HR (beta= −.21, p<.001) reactivity. Total observed violence was associated with decreased SBP reactivity (beta=−.14, p<.05). | ++ |
| 21 | Wilson DK (2002) | 56 M/F 52% F Mean age: 13 |
Cross-sectional study of healthy African-American adolescents in Richmond, VA | Retrospective assessment of experiencing, seeing, or hearing about violence in the community | Frequency of experiencing, seeing, or hearing about violence in the community in the past year using RSSECV | Measured BP dipping status | BP readings every 15 min over a 24-hour period; nondipping status based on <10% or difference in mean BP between waking and sleeping | Mean BP nondipping status was positively associated with victimization (beta 0.32, SE 0.15). Hearing about violence was associated with mean BP nondipping status among men (beta 2.29 SE 1.03). | + |
Abbreviations: AHR: Adjusted hazard ratio, AOR: Adjusted odds ratio, ARR: Adjusted risk ratio, BP: Blood pressure, CTI: Childhood Trauma Interview, CTS: Conflict Tactics Scales, CTQ: Childhood Trauma Questionnaire, CV: Cardiovascular, CVD: Cardiovascular disease, DBP: Diastolic bood pressure, HbA1C: Hemoglobin A1c, HDL: High density lipoprotein, HR: Hazard ratio, HRt: Heart rate, HRV: Heart rate variability, HTN: Hypertension, IHD: Ischemic heart disease, MI: Myocardial infarction (heart attack), OR: Odds ratio, R-CTS: Revised Conflict Tactics Scale, RSSECV: Richters and Saltazman’s Survey of Exposure to Community Violence, SBP: Systolic blood pressure
Appendix Table 2.
Adult violence exposure and cardiovascular outcomes, by study design and sample size
| Ref No. |
First Author (Year) |
Sample Size/ Gender/Age |
Study Design/ Setting |
Retrospective/ Prospective Exposure Assessment |
Exposure Measurement |
Self-report/ Measured Outcome Assessment |
Outcome Measure |
Results | Evidence Grade |
|---|---|---|---|---|---|---|---|---|---|
| Prospective Studies | |||||||||
| 33 | Mason SM (2012) | 51,434 F Mean age: 46 |
Prospective cohort of registered nurses in the US | Retrospective assessment of physical and sexual IPV and current assessment of emotional abuse | Any experience of physical or sexual IPV or emotional abuse in ongoing relationships (3 levels of severity) | Self-reported HTN | Physician-diagnosed HTN reported in 6 years of follow-up after exposure ascertainment | No significant association was noted between incident HTN and physical (AHR: 1.1, 95% CI: 1.0–1.1) or sexual IPV (AHR: 1.0, 95% CI: 0.9–1.1). Women with most severe emotional abuse had increased incidence of HTN (AHR: 1.2, 95% CI: 1.0–1.5) compared to women without emotional abuse. | ++ |
| 34 | Stene (2013) | 5,593 F 31% 30 yo 45% 40,45 yo 24% 59,60 yo |
Prospective population-based cohort of women aged 30–60 in Oslo, Norway | Retrospective assessment of IPV | Any experience of psychological IPV or physical and/or sexual IPV | CV drug use ascertained from national prescription database | Incident CV drug use ascertained from Norwegian Prescription Database including all CV drugs, anti-HTN drugs, and lipid-modifying drugs | Psychological IPV was not associated with any CV drug use. Physical/sexual IPV was associated with anti-HTN drug use (AIRR: 1.4, 95% CI: 1.1–1.7). | ++ |
| Cross-sectional Studies | |||||||||
| 35 | Breiding MJ (2008) | 70,156 M/F 61% F Age >18 |
Cross-sectional, representative survey of adults in 16 states in the US | Retrospective assessment of IPV | Any experience of threatened, attempted or completed physical or sexual violence by current or former intimate partner | Self-reported CV events or signs | History of physician-diagnosed high BP, high cholesterol, MI, stroke, CHD | Among women, IPV was associated with high cholesterol (AOR: 1.3, 95% CI: 1.1–1.4), stroke (AOR: 1.8, 95% CI: 1.4–2.2), high BP (AOR: 1.1, 95% CI: 1.0–1.2), MI (AOR: 1.4, 95% CI: 1.1–1.8) and CHD (AOR: 1.8, 95% CI: 1.5–2.1). Among men, IPV was associated with stroke (AOR: 1.4, 95% CI: 1.0–2.1). |
+ |
| 44 | Vives-Cases C (2011) | 13,094 F 40% >50 yo |
Cross-sectional nationally representative survey in Spain | Retrospective assessment of IPV and VAW | IPV defined as violence in the past 12 months where the perpetrator was the woman’s intimate partner; VAW defined as violence perpetrated by a unknown man or woman or known man who was not their partner | Self-reported HTN or CHD | Physician-diagnosed HTN or CHD | No association between HTN and IPV (AOR: 0.8, 95% CI: 0.5–1.5) or VAW (AOR: 1.0, 95% CI: 0.5–1.8) in past 12 months. Significant association noted between IPV and CHD (AOR 5.3 95% CI: 1.5, 19.3). Unable to estimate association between VAW and CHD due to small numbers. | + |
| 38 | Frayne SM (1999) | 3,632 F Mean age: 47 |
Cross-sectional survey of women using VA health care | Retrospective assessment of sexual assault in the military | Any experience of sexual assault while in the military | Self-reported CVD events and symptoms | Reports of being bothered by angina or other heart problem; treatment for HTN, MI, TIA, or stroke in past 12 months | History of sexual assault in military was associated with angina (AOR: 1.6, 95% CI: 1.3–2.0), other heart problems (AOR: 1.6, 95% CI: 1.3–2.1), HTN (AOR: 1.3, 95% CI: 1.1–1.6), and MI (AOR: 2.3, 95% CI: 1.4–4.0) but not TIA (AOR: 1.2, 95% CI: 0.7–2.1) or stroke (AOR: 1.5, 95% CI: 0.8–2.9). | + |
| 37 | Frayne SM (2003) | 3,632 F Mean age: 47 |
Cross-sectional survey of women using VA health care | Retrospective assessment of sexual assault in the military | Any experience of sexual assault while in the military | Self-reported HTN | Self-reported HTN | History of sexual assault in military was associated with HTN (AOR: 1.2, 95% CI: 1.0–1.5). | + |
| 32 | Bonomi AE (2009) | 1,928 F 55% 45–64 yo |
Cross-sectional study of healthcare plan members in Washington and Idaho, USA | Retrospective assessment of IPV | Any experience of physical, sexual or non-physical abuse by intimate partner in the past year compared with women with no history of IPV in adulthood | ICD-9 codes from health care visits | ICD-9 codes for CV signs and symptoms, disorders of lipid metabolism and HTN in the past year | No significant associations were noted between IPV in past year and CV s/s (AOR: 1.1, 95% CI: 0.7–1.7), disorders of lipid metabolism (AOR: 0.9, 95% CI: 0.5–1.6), or HTN (AOR: 1.3, 95% CI: 1.0–1.8). | ++ |
| 41 | Golding JM (1994) | 1,610 F Mean age: 40 |
Cross-sectional representative survey of adults in Los Angeles, CA, US | Retrospective assessment of sexual assault | Lifetime experience of sexual assault including forced touching or intercourse | Self-reported heart disease or HTN | Lifetime history of heart disease and HTN | No significant associations between sexual assault and heart disease (AOR: 1.6, p–value=0.06) or HTN (AOR: 1.2, p–value=0.28). | + |
| 39 | Sparrenberger F (2008) | 1,474 M/F 59% F Mean age: 49 |
Cross-sectional representative survey of adults in Porto Alegre, Brazil | Retrospective assessment of physical violence | Any type of physical violence experienced in the past year perpetrated by any person | Measured blood pressure | HTN was defined as blood pressure above 140/90 mmHg or use of blood pressure lowering medication | Adjusted analyses showed no significant associations between physical violence and HTN in either men (AOR: 0.3, 95% CI: 0.1–1.1) or women (AOR: 0.7, 95% CI: 0.2–3.0). | ++ |
| 43 | Ruiz-Perez, I (2007) | 1,402 F Mean age: 39 |
Cross-sectional study of women attending family practices in Spain | Retrospective assessment of IPV | Current (past year) and past IPV (physical, psychological or sexual abuse by a partner) in 4 combinations of (psychological only, psychological and physical, psychological and sexual, all 3 types); duration of abuse recorded as no abuse, 1 month–1 year, >1 year | Self-reported HTN | Self-reported HTN | No association between any lifetime IPV and HTN (AOR: 1.0, 95% CI: 0.6–1.7) or between specific combinations of IPV and HTN. | + |
| 40 | Gass JD (2010) | 1,229 F Age >18 |
Cross-sectional nationally-representative sample of adults in South Africa | Retrospective assessment of physical IPV | Physical IPV by current or most recent intimate partner | Self-reported stroke, MI, heart disease, and high BP | Stroke or MI in past 12 months; heart disease or high BP ever | IPV was not significantly associated with MI (AOR: 1.8, 95% CI: 1.0–3.3), stroke (AOR: 1.3, 95% CI: 0.6–2.8), high BP (AOR: 1.5, 95%CI: 1.0–2.2), or heart disease (AOR: 1.2, 95% CI: 0.7–2.2). | + |
| 42 | Lown EA (2001) | 1,155 F Mean age: 32 |
Cross-sectional representative survey of Mexican Americans living in Fresno County, CA, USA | Retrospective assessment of IPV | Physical or sexual IPV by a current partner in past 12 months | Self-reported high BP, MI and other serious heart trouble | MI or serious heart trouble, or high BP in the past 12 months | Physical/sexual IPV was associated with MI (AOR: 17.0, 95% CI: 4.3–66.7) but not high BP (AOR: 0.9, 95% CI: 0.3–2.8). | + |
| 30 | Coker AL (2000) | 1,152 F 44% 40 yo |
Cross-sectional study of women attending family practice clinics in SC, USA | Retrospective assessment of IPV | Any experience of physical or sexual violence with or without psychological abuse by intimate partner; psychological abuse without any physical/sexual violence by intimate partner | Self-reported CV events or problems | Physician-diagnosed MI, stroke, HTN, angina, other heart or circulatory problems | Physical/sexual violence associated with angina (AOR: 2.0, 95% CI: 1.2–3.5) and other heart or circulatory problems (AOR: 1.5, 95% CI: 1.0–2.2) but not with HTN (AOR: 1.0, 95% CI: 0.8–1.3). Psychological abuse was not significantly associated with any CV outcome. | + |
| 36 | Keyes KM (2013) | 1,054 M/F 53% F Mean age: 44 |
Population-based cohort of adults in Detroit, MI, USA | Retrospective assessment of assaultive violence | Assaultive violence included any experience of rape, other sexual assault, being shot, stabbed, held captive, tortured, kidnapped, mugged, held up, threatened with a weapon, or badly beaten up | Self-reported CVD | CVD included physician-diagnosed HTN, MI, stroke, chest pain, congestive heart failure | Assaultive violence was not associated with CVD (OR: 1.0, 95% CI: 0.7–1.3). | + |
| 31 | Newton TL (2005) | 39 F Mean age: 51 |
Cross-sectional study | Retrospective assessment of lifetime victimization | Lifetime victimization severity score includes robbery, child physical abuse, stalking or threatening behavior, adult sexual or physical assault as well as other crime victimization | Measured BP and heart rate | Ambulatory BP and heart rate over an average 18 hours | Lifetime victimization severity was associated with heart rate variability. | + |
Abbreviations: AIRR: Adjusted incident rate ratio, AHR: Adjusted hazard ratio, AOR: Adjusted odds ratio, BP: Blood pressure, CAD: Coronary artery disease, CHD: Coronary heart disease, CTS: Conflict Tactics Scales, CV: Cardiovascular, CVD: Cardiovascular disease, DBP: Diastolic blood pressure, HbA1C: Hemoglobin A1c, HDL: High density lipoprotein, HR: Hazard ratio, HRT: Heart rate, HRV: Heart rate variability, HTN: Hypertension, IHD: Ischemic heart disease, IPV: Intimate partner violence, MI: Myocardial infarction (heart attack), OR: Odds ratio, R-CTS: Revised Conflict Tactics Scale, SBP: Systolic blood pressure, TIA: Transient ischemic attack, VA: Veteran’s Administration, VAW: Violence against woman
Childhood Exposures
Fifteen manuscripts, from 13 studies, examined the relation between childhood violence exposure and cardiovascular health outcomes (Appendix Table 1). Twelve studies employed a cross-sectional study design and three used a prospective study design. The majority of the studies’ sample populations were based in the U.S. (12 of 15 studies).15–26 Of the 15 studies exploring childhood exposures selected for review, 12 explored the effects of childhood abuse on cardiovascular outcomes in adulthood15–17,19,22–29 and only three examined the effects of experiencing violence in the community during childhood/adolescence.18,20,21 The 12 studies that focused on child abuse all assessed child abuse exposure retrospectively during adulthood (Table 1). Among these 12 studies, six assessed childhood abuse with validated scales, mainly the Childhood Trauma Questionnaire or Conflict Tactic Scales.15–17,24,25,29 Positive associations were noted among studies using validated scales as well as those using non-validated questions.
A positive relation between child abuse and hypertension in adulthood was found in all five studies evaluating hypertension as an endpoint, with all studies using self-reported hypertension.17,22,25,26,28 Gender differences in the association between abuse and hypertension were only examined in one study. Using data from the National Comorbidity Survey, experiencing physical abuse during childhood was associated with self-reported hypertension among adult men but not women; however, sexual abuse was associated with self-reported hypertension among women but not men.22
Eight studies examined CVD as an endpoint, all noting significant positive associations between child abuse and CVD.15–17,19,22,24,26,27 CVD was generally defined as experiencing any one of a series of potential endpoints, such as stroke, MI, or angina; however, definitions varied across studies. Using data from the Adverse Childhood Events study, Dong and colleagues15 noted a relationship between emotional, physical, and sexual abuse and ischemic heart disease, which was defined as ever experiencing a heart attack, pain, or heavy pressure in chest with exertion or use of nitroglycerine. Only two studies, both from the National Comorbidity Survey, examined gender differences in the childhood abuse and CVD association, noting positive associations among women but not men.19,22 Of the seven studies that examined CVD as an endpoint, all used self-reported CVD measures and noted positive associations. Two studies used medical record reviews to validate self-reported cardiovascular outcomes.16,24 A positive association between forced sex and definite CVD events, defined as MI or stroke confirmed by medical record review, was noted in the Nurses Health Study.24 Interestingly, patients with a history of abuse were less likely to allow access to medical records and were thus less likely to have self-reported CVD outcomes confirmed by medical records. The strength of the association between forced sex and cardiovascular events was also attenuated in the confirmed event cases compared to the self-reported cases. Roy and colleagues16 used discharge diagnosis of CVD (MI, stroke, or CHD) to confirm self-reported CVD and also noted positive associations with childhood abuse and neglect. Number of childhood traumas as measured by the Childhood Trauma Questionnaire was associated with 6-year incidence of CVD based on discharge diagnosis.
One study assessed the relation between childhood sexual abuse and self-reported physician-diagnosed MI, noting a significant association among men but not women.23 In the Nurses Health Study,36 forced sex in childhood was associated with a non-significant increase in confirmed or probable MI among women. Severe physical abuse and forced sex were significantly associated with increased risk of confirmed or probable stroke. No other study examined cardiovascular endpoints independently.
Only three studies examined the impact of experiencing violence in the community on cardiovascular risk among adolescents or children.18,20,21 Wilson and colleagues21 noted that adolescents who experienced violence victimization were more likely to be classified as non-dippers, where the typical nocturnal decrease in blood pressure is absent or blunted, which has been associated with stroke and left ventricular hypertrophy. Murali and Chen20 examined the effects of violence on laboratory assessments of cardiovascular and neuroendocrine measures, both at baseline and in response to an interpersonal laboratory stressor (a debate or puzzle task) in 115 urban high school students aged 16–19 years. Increased frequency of lifetime violence exposure was associated with higher basal diastolic BP and heart rate. Higher levels of violence exposure also predicted decreased cardiovascular reactivity to the acute laboratory stressor based on the physiologic indicators (i.e., BP, heart rate, and heart rate variability).
Adult Exposures
Fifteen manuscripts, from 12 studies, were selected for review of the relation between adult violence exposure and cardiovascular endpoints (Appendix Table 2).30–44 Only two studies employed a prospective design,33,34 and only three included both men and women in their sample.35,36,45
With the exception of four studies,37,39,41,44 all focused on the effects of IPV, assessed retrospectively, and did not consider other forms of violence in adulthood (i.e., community). Hypertension was examined in 13 of 15 studies, with mixed findings. Eight studies noted no association between adult violence exposure and hypertension.30,32,39–44 Using the Spanish National Health Survey, Vives-Casas and colleagues44 examined the relation between IPV and self-reported hypertension among women but noted no significant associations. In contrast, a significant association was noted between IPV and self-reported hypertension among women but not men in the Behavioral Risk Factor Surveillance System Study (BRFSS).35 Most studies relied on self-report of hypertension; only two used BP measurements or ICD-9 codes from medical records, noting no significant findings.32,39 Sparrenberg and colleagues39 observed no associations when examining the relation between physical violence in the past year and hypertension based on BP ≥140/90 mmHg or use of BP-lowering medications.
Ten studies examined violence exposure in adulthood and CVD as an endpoint. Nine studies used self-reported CVD measures defined as either heart/circulatory problems,30,38 CHD,35,40,44,46 cardiovascular signs or symptoms,32 or a combination of hypertension, MI, stroke, chest pain, or congestive heart failure,36,42 with mixed findings. Four of 9 studies noted positive associations between violence in adulthood and CVD.30,35,42,44 Of the ten studies that examined adult violence and CVD endpoints, one study defined CVD as use of CVD medications ascertained through a national prescription database, noting no significant associations.34
Three studies assessed the relation between violence exposure in adulthood and MI, and all used a self-reported measure of MI. One noted a significant association among a representative sample of U.S. adults.35 Another study using a sample of women utilizing the Veterans Affairs healthcare system, noted significant associations between histories of sexual assault in the military and MI in the past 12 months.38 A third study based on the South African Stress and Health Study noted nearly significant associations between IPV and self-reported heart attack in the past 12 months.40
Three studies assessed the relation between violence exposure and stroke.35,38,40 Using the BRFSS, Breiding and colleagues35 noted significant associations between IPV and stroke, among both women and men. Two other studies noted no significant associations, though the number of stroke cases was small.38,40
Discussion
A consistent positive relation between child abuse and CVD in adulthood is noted, despite varying child abuse definitions as well as varying definitions of CVD. Adult violence exposure was not consistently associated with cardiovascular outcomes. Discrepancies in study findings may be attributed to methodologic limitations discussed below.
A relation was noted among childhood experiences of physical or sexual violence and various cardiovascular endpoints in adulthood. Over half of the child violence articles selected for review also assessed neglect, noting associations with various cardiovascular endpoints. Violence exposure may affect cardiovascular health directly through disruption of various physiologic mechanisms or indirectly by affecting mental health or modifying health behaviors. Violence exposure during childhood has been shown to disrupt normal physiologic development, particularly emerging brain architecture as well as cognitive and behavioral functioning.10 Psychological stress has been associated with the activation of the sympathetic and adrenomedullary system and the hypothalamic-pituitary-adrenal axis.47 Stress can lead to impairment of endothelial function; increases in circulating levels of inflammatory cytokines such as interleukin-6, C-reactive protein, and tumor necrosis factor-α; platelet activation; and prothrombotic changes in molecules involved in coagulation; factors that are involved in the atherosclerotic process.48–50
Violence exposure in childhood and adulthood may also affect cardiovascular health through indirect pathways. Long-term effects of violence exposure have been noted in relation to depression, aggression, substance use, and risk-taking behaviors.35,51,52 Many, though not all, children and adults exposed to violence develop post-traumatic stress disorder (PTSD) and depression. Both PTSD and depression have been linked to obesity, hypertension, and adverse cardiac outcomes.53,54 Although many children and adults exposed to violence may exhibit emotional disturbances (e.g., depression, PTSD, anxiety) as a result of their experiences, others experience adverse physical effects in the absence of adverse mental health effects. Children and adults employ different coping mechanisms to manage the stress associated with violence exposure, which may include changes in lifestyle factors (i.e., worsening diet and decreased physical activity) and engaging in substance use behaviors (i.e., smoking and alcohol use), which are known to affect heart disease risk.55,56 Though not a focus of this review, various studies have documented associations among violence exposures and tobacco use, alcohol use, poor dietary habits, and sedentary lifestyle, potential mechanisms linking violence exposure and cardiovascular health. An extensive literature has shown that smoking, alcohol use, and decreased physical activity increase the risk of cardiovascular morbidity and mortality.57 Smoking has been shown to be associated with more stressful violent environments,52,58,59 and in conjunction with alcohol use, has also been proposed as a type of self-medication to cope with a stressful situation or environment.60
Limitations and Recommendations
First, there is a lack of uniformity on how violence is assessed and characterized. In general, existing studies have examined different types of violence exposure (i.e., physical, sexual, or emotional) separately in relation to CVD but have not accounted for the chronicity or severity of these exposures.22 Furthermore, often only one question was used to assess exposure to a specific form of violence. Most of the studies focused on adult IPV characterized IPV with a single yes/no and did not consider frequency of abuse, severity, or whether the abuse occurred with multiple partners. Although most studies relied on a yes/no categorization of violence exposure that did not account for the type or the severity of the abuse, using data from the Nurses Health Study, Mason and colleagues33 created IPV categories based on type and created three levels of severity when considering emotional abuse. The authors noted a significant association between emotional abuse and hypertension, particularly at the highest levels of abuse. It is plausible that differential characterization of exposure across studies is contributing to the mixed findings.
These issues are not exclusive to studies that explore IPV exposures in adulthood. Studies that examined child abuse also had limitations associated with the use of limited exposure assessments. Violence during childhood was often also limited to only one question. A simplified, yes/no classification of child abuse assumes that all forms of abuse have the same effect on health outcomes. Furthermore, it ignores when in the life course the exposure occurred. If, as recent research suggests, only the most severe experiences have an impact on CVD, using a maltreatment classification that ignores chronicity or severity of exposure will obscure true effect estimates. Despite this limitation, most studies that explored child abuse noted positive associations.
There is also a heavy reliance on self-reported outcomes. The vast majority of reviewed studies relied on self-reported measures of CVD, which could introduce misclassification of the outcome that may or may not be differential with respect to violence exposure.22,28 For example, National Health and Nutrition Examination Survey data have demonstrated that only 83% of hypertensive adults aged >18 years are aware of their hypertension,61 thus, use of self-reported hypertension would underestimate the true prevalence of hypertension and potentially bias results toward the null, assuming non-differential misclassification. Alternatively, differential misclassification may result; in the Nurses Health Study,24 a stronger association was noted between non-verified cardiovascular outcomes and violence exposure compared to associations that relied on verified cardiovascular outcomes. In addition, several studies combined cardiovascular outcomes such as hypertension, MI, and stroke into a single CVD category, making it difficult to distinguish effects that may be associated with only some cardiovascular outcomes.
Positive findings on the relation of child abuse and cardiovascular outcomes in spite of the potential for misclassification of both the exposure and outcome may be attributed to a large causal effect of child abuse on cardiovascular outcomes compared to the effect of adult violence exposure on cardiovascular outcomes. For both childhood and adulthood violence, it is possible that the observed effects are an underestimate of the true association, given the potential misclassification of exposure and outcome.
The studies had a wide range of sample sizes, ranging from studies with less than 100 participants to national studies with tens of thousands of participants. Sample size was not a factor among studies that examined childhood exposures, as all noted significant associations with CVD outcomes regardless of sample size. Among adult studies, where findings were mixed, no discernible trend appeared, in that both large and small studies failed to see an association. This suggests that the population under the study and the exposure and outcome assessments may be more important considerations with regard to the significance of the findings.
Sex differences in the relation between violence exposure and cardiovascular outcomes need to be explored further. Sex differences were examined in only a handful of studies, potentially obscuring associations that may exist in only one gender. Of the 15 reviewed papers that focused on violence exposure in adulthood, only two included both men and women in their samples.35,39 Although women are more likely to experience IPV compared to men, men are also at risk. In the National Violence Against Women Survey that included men and women aged 18–65 years, 29% of women and 23% of men reported experiencing IPV in their lifetime. The prevalence of cardiovascular outcomes also differs by gender, with men having increased prevalence of hypertension, stroke, and MI compared to women.
All but one of the reviewed studies considered the childhood period, often defined as age <18 years, as one developmental period without consideration for sensitive periods that may exist within childhood. Research suggests that exposure to child abuse in early childhood, which is a critical period of brain development, is more detrimental to behavioral and cognitive development than exposure to child abuse at later stages of child development.10 Whether childhood critical periods of exposure exist for the development of CVD remains unknown.
Few studies examined the relation between violence exposure and cardiovascular endpoints in childhood/adolescence. Those that did noted a positive association, suggesting a possible trajectory of health risk that starts in adolescence. Most studies focused on adult populations and only three examined adolescents prior to the onset of CVD.18,20,21 Identifying those most at risk for development of CVD earlier in life would have a greater impact in prevention efforts. Violence exposure in childhood may be particularly important, as biological mechanisms used to compensate for chronic stress exposure may be detrimental to health, setting the stage for the early development of CVD.62 Furthermore, unhealthy habits used to cope with stress exposure are formed during these early years and could contribute to greater cardiovascular risk.63
The cross-sectional nature of most adult violence exposure studies limits the ability of observing associations with adult violence exposures. Given the long developmental nature of CVD, the interval between adult exposure to violence and CVD assessment may not be sufficiently long. This may be particularly true for studies that examined past-year experiences of violence in adulthood.
Conclusions
In this systematic review, a consistent positive association across studies that examined the relation between child abuse and CVD endpoints is noted. In contrast, mixed findings are noted across studies examining the relation between adult violence exposure and cardiovascular outcomes. Inconsistencies in the manner in which violence exposure is characterized as well as the cross-sectional nature of most adult violence exposure studies make it difficult to draw definitive conclusions from these studies. Alternatively, sensitive or vulnerable time periods may exist in relation to violence exposure and cardiovascular health. Further research that captures the chronicity and severity of violence exposure across the life course is needed to further elucidate the relation between violence exposure and cardiovascular outcomes. Additionally, sufficient time should elapse between the exposure and query of the outcome, particularly for adulthood exposure to violence. Studies that examine the mechanisms through which violence is associated with cardiovascular endpoints as well as identify protective factors of the effects of violence would be fruitful areas of research that could effectively inform interventions. Given the high prevalence of experiencing and witnessing serious and lethal violence among youth,4 the number of children at risk for developing adverse emotional and behavioral outcomes as well as increased risk of obesity, diabetes, and CVD makes this a significant public health problem.5,6,64
Acknowledgments
Dr. Suglia was supported by grant No. K01HL103199.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC. A Public Health Action Plan to Prevent Heart Disease and Stroke. 2008. [Google Scholar]
- 2.Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: an update. JAMA Pediatr. 2013;167(7):614–21. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- 3.Wright RJ, Wright RO, Isaac NE. Response to battered mothers in the pediatric emergency department: a call for an interdisciplinary approach to family violence. Pediatrics. 1997;99(2):186–92. doi: 10.1542/peds.99.2.186. [DOI] [PubMed] [Google Scholar]
- 4.CDC. Child Maltreatment; Facts at a Glance 2013. 2013 www.cdc.gov/violenceprevention/pdf/cm-data-sheet--2013.pdf.
- 5.Koop CE, Lundberg GB. Violence in America: a public health emergency: time to bite the bullet back. JAMA. 1992;267(22):3075–6. [PubMed] [Google Scholar]
- 6.Glodich A. Traumatic exposure to violence: a comprehensive review of the child an adolescent literature. Smith Coll Stud Soc Work. 1998;68(3):321–45. [Google Scholar]
- 7.CDC. Adverse childhood experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(49):1609–13. [PubMed] [Google Scholar]
- 8.Roy A. Childhood trauma and neuroticism as an adult: possible implication for the development of the common psychiatric disorders and suicidal behaviour. Psychol Med. 2002;32(8):1471–4. doi: 10.1017/s0033291702006566. [DOI] [PubMed] [Google Scholar]
- 9.Bunce SC, Larsen RJ, Peterson C. Life after trauma: personality and daily life experiences of traumatized people. J Pers. 1995;63(2):165–88. doi: 10.1111/j.1467-6494.1995.tb00806.x. [DOI] [PubMed] [Google Scholar]
- 10.Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 11.Boynton-Jarrett R, Fargnoli J, Suglia SF, Zuckerman B, Wright RJ. Association between maternal intimate partner violence and incident obesity in preschool-aged children: results from the fragile families and child well-being study. Arch Pediatr Adolesc Med. 2010;164(6):540–6. doi: 10.1001/archpediatrics.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suglia SF, Clark CJ, Gary-Webb TL. Adolescent obesity, change in weight status, and hypertension: racial/ethnic variations. Hypertension. 2013;61(2):290–5. doi: 10.1161/HYPERTENSIONAHA.111.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–8. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 14.Mulrow CD. Rationale For Systematic Reviews. Brit Med J. 1994;309(6954):597–9. doi: 10.1136/bmj.309.6954.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110(13):1761–6. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 16.Roy A, Janal MN, Roy M. Childhood trauma and prevalence of cardiovascular disease in patients with type 1 diabetes. Psychosom Med. 2010;72(8):833–8. doi: 10.1097/PSY.0b013e3181eafc2d. [DOI] [PubMed] [Google Scholar]
- 17.Springer KW, Sheridan J, Kuo D, Carnes M. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl. 2007;31(5):517–30. doi: 10.1016/j.chiabu.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark R, Benkert RA, Flack JM. Violence exposure and optimism predict task-induced changes in blood pressure and pulse rate in a normotensive sample of inner-city black youth. Psychosom Med. 2006;68(1):73–9. doi: 10.1097/01.psy.0000195744.13608.11. [DOI] [PubMed] [Google Scholar]
- 19.Batten SV, Aslan M, Maciejewski PK, Mazure CM. Childhood maltreatment as a risk factor for adult cardiovascular disease and depression. J Clin Psychiat. 2004;65(2):249–54. doi: 10.4088/jcp.v65n0217. [DOI] [PubMed] [Google Scholar]
- 20.Murali R, Chen E. Exposure to violence and cardiovascular and neuroendocrine measures in adolescents. Ann Behav Med. 2005;30(2):155–63. doi: 10.1207/s15324796abm3002_8. [DOI] [PubMed] [Google Scholar]
- 21.Wilson DK, Kliewer W, Teasley N, Plybon L, Sica DA. Violence exposure, catecholamine excretion, and blood pressure nondipping status in African American male versus female adolescents. Psychosom Med. 2002;64(6):906–15. doi: 10.1097/01.psy.0000024234.11538.d3. [DOI] [PubMed] [Google Scholar]
- 22.Goodwin RD, Stein MB. Association between childhood trauma and physical disorders among adults in the United States. Psychol Med. 2004;34(3):509–20. doi: 10.1017/s003329170300134x. [DOI] [PubMed] [Google Scholar]
- 23.Fuller-Thomson E, Bejan R, Hunter JT, Grundland T, Brennenstuhl S. The link between childhood sexual abuse and myocardial infarction in a population-based study. Child Abuse Negl. 2012;36(9):656–65. doi: 10.1016/j.chiabu.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Rich-Edwards JW, Mason S, Rexrode K, et al. Physical and sexual abuse in childhood as predictors of early-onset cardiovascular events in women. Circulation. 2012;126(8):920–7. doi: 10.1161/CIRCULATIONAHA.111.076877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riley EH, Wright RJ, Jun HJ, Hibert EN, Rich-Edwards JW. Hypertension in adult survivors of child abuse: observations from the Nurses’ Health Study II. J Epidemiol Community Health. 2010;64(5):413–8. doi: 10.1136/jech.2009.095109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Afifi TO, Mota N, MacMillan HL, Sareen J. Harsh physical punishment in childhood and adult physical health. Pediatrics. 2013;132(2):e333–40. doi: 10.1542/peds.2012-4021. [DOI] [PubMed] [Google Scholar]
- 27.Fuller-Thomson E, Brennenstuhl S, Frank J. The association between childhood physical abuse and heart disease in adulthood: findings from a representative community sample. Child Abuse Negl. 2010;34(9):689–98. doi: 10.1016/j.chiabu.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Stein DJ, Scott K, Haro Abad JM, et al. Early childhood adversity and later hypertension: Data from the World Mental Health Survey. Ann Clin Psychiatry. 2009;22(1):19–28. [PMC free article] [PubMed] [Google Scholar]
- 29.van Reedt Dortland AK, Giltay EJ, van Veen T, Zitman FG, Penninx BW. Personality traits and childhood trauma as correlates of metabolic risk factors: the Netherlands Study of Depression and Anxiety (NESDA) Prog Neuropsychopharmacol Biol Psychiatry. 2012;36(1):85–91. doi: 10.1016/j.pnpbp.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Coker AL, Smith PH, Bethea L, King MR, McKeown RE. Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med. 2000;9(5):451–7. doi: 10.1001/archfami.9.5.451. [DOI] [PubMed] [Google Scholar]
- 31.Newton TL, Parker BC, Ho IK. Ambulatory cardiovascular functioning in healthy postmenopausal women with victimization histories. Biol Psychol. 2005;70(2):121–30. doi: 10.1016/j.biopsycho.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 32.Bonomi AE, Anderson ML, Reid RJ, Rivara FP, Carrell D, Thompson RS. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med. 2009;169(18):1692–7. doi: 10.1001/archinternmed.2009.292. [DOI] [PubMed] [Google Scholar]
- 33.Mason SM, Wright RJ, Hibert EN, Spiegelman D, Forman JP, Rich-Edwards JW. Intimate partner violence and incidence of hypertension in women. Ann Epidemiol. 2012;22(8):562–7. doi: 10.1016/j.annepidem.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stene LE, Jacobsen GW, Dyb G, Tverdal A, Schei B. Intimate partner violence and cardiovascular risk in women: a population-based cohort study. J Womens Health (Larchmt) 2013;22(3):250–8. doi: 10.1089/jwh.2012.3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breiding MJ, Black MC, Ryan GW. Chronic disease and health risk behaviors associated with intimate partner violence-18 U.S. states/territories, 2005. Ann Epidemiol. 2008;18(7):538–44. doi: 10.1016/j.annepidem.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 36.Keyes KM, McLaughlin KA, Demmer RT, Cerda M, Koenen KC, Uddin M, et al. Potentially traumatic events and the risk of six physical health conditions in a population-based sample. Depress Anxiety. 2013;30(5):451–60. doi: 10.1002/da.22090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frayne SM, Skinner KM, Sullivan LM, Freund KM. Sexual assault while in the military: violence as a predictor of cardiac risk? Violence Vict. 2003;18(2):219–25. doi: 10.1891/vivi.2003.18.2.219. [DOI] [PubMed] [Google Scholar]
- 38.Frayne SM, Skinner KM, Sullivan LM, Tripp TJ, Hankin CS, Kressin NR, et al. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Womens Health Gend Based Med. 1999;8(6):835–45. doi: 10.1089/152460999319156. [DOI] [PubMed] [Google Scholar]
- 39.Sparrenberger F, Fuchs SC, Moreira LB, Fuchs FD. Stressful life events and current psychological distress are associated with self-reported hypertension but not with true hypertension: results from a cross-sectional population-based study. BMC Public Health. 2008;8:357. doi: 10.1186/1471-2458-8-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gass JD, Stein DJ, Williams DR, Seedat S. Intimate partner violence, health behaviours, and chronic physical illness among South African women. S Afr Med J. 2010;100(9):582–5. doi: 10.7196/samj.4274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Golding J. Intimate Partner Violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence. 1999;14(2):99–132. [Google Scholar]
- 42.Lown EA, Vega WA. Intimate partner violence and health: self-assessed health, chronic health, and somatic symptoms among Mexican American women. Psychosom Med. 2001;63(3):352–60. doi: 10.1097/00006842-200105000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Ruiz-Perez I, Plazaola-Castano J, Del Rio-Lozano M. Eur J Public Health. 2007;17(5):437–43. doi: 10.1093/eurpub/ckl280. [DOI] [PubMed] [Google Scholar]
- 44.Vives-Cases C, Ruiz-Cantero MT, Escriba-Aguir V, Miralles JJ. The effect of intimate partner violence and other forms of violence against women on health. J Public Health (Oxf) 2011;33(1):15–21. doi: 10.1093/pubmed/fdq101. [DOI] [PubMed] [Google Scholar]
- 45.Sparrenberger F, Cichelero FT, Ascoli AM, Fonseca FP, Weiss G, Berwanger O, et al. Does psychosocial stress cause hypertension? a systematic review of observational studies. J Hum Hypertens. 2009;23(1):12–9. doi: 10.1038/jhh.2008.74. [DOI] [PubMed] [Google Scholar]
- 46.Golding JM. Sexual assault history and physical health in randomly selected Los Angeles women. Health Psychol. 1994;13(2):130–8. doi: 10.1037//0278-6133.13.2.130. [DOI] [PubMed] [Google Scholar]
- 47.Cacioppo JT, Berntson GG, Malarkey WB, et al. Autonomic, neuroendocrine, and immune responses to psychological stress: the reactivity hypothesis. Ann N Y Acad Sci. 1998;840:664–73. doi: 10.1111/j.1749-6632.1998.tb09605.x. [DOI] [PubMed] [Google Scholar]
- 48.Steptoe A, Kivimaki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013;34:337–54. doi: 10.1146/annurev-publhealth-031912-114452. [DOI] [PubMed] [Google Scholar]
- 49.Ranjit N, Diez-Roux AV, Shea S, et al. Psychosocial factors and inflammation in the multi-ethnic study of atherosclerosis. Arch Intern Med. 2007;167(2):174–81. doi: 10.1001/archinte.167.2.174. [DOI] [PubMed] [Google Scholar]
- 50.McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci. 2004;1032:1–7. doi: 10.1196/annals.1314.001. [DOI] [PubMed] [Google Scholar]
- 51.Campbell C, Schwarz DF. Prevalence and impact of exposure to interpersonal violence among suburban and urban middle school students. Pediatrics. 1996;98(3 Pt 1):396–402. [PubMed] [Google Scholar]
- 52.Jun HJ, Rich-Edwards JW, Boynton-Jarrett R, Wright RJ. Intimate partner violence and cigarette smoking: association between smoking risk and psychological abuse with and without co-occurrence of physical and sexual abuse. Am J Public Health. 2008;98(3):527–35. doi: 10.2105/AJPH.2003.037663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Edmondson D, Kronish IM, Shaffer JA, Falzon L, Burg MM. Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. Am Heart J. 2013;166(5):806–14. doi: 10.1016/j.ahj.2013.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davidson KW. Depression and coronary heart disease. ISRN Cardiol. 2012;2012:743–813. doi: 10.5402/2012/743813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Durant RH, Altman D, Wolfson M, Barkin S, Kreiter S, Krowchuk D. Exposure to violence and victimization, depression, substance use, and the use of violence by young adolescents. J Pediatr. 2000;137(5):707–13. doi: 10.1067/mpd.2000.109146. [DOI] [PubMed] [Google Scholar]
- 56.Greenfield EA, Marks NF. Violence from parents in childhood and obesity in adulthood: using food in response to stress as a mediator of risk. Soc Sci Med. 2009;68(5):791–8. doi: 10.1016/j.socscimed.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119(3):e21–181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 58.Anderson C, Roux G, Pruitt A. Prenatal depression, violence, substance use, and perception of support in pregnant middle-class women. J Perniat Educ. 2002;11(1):14–21. doi: 10.1624/105812402X88560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ganz ML. The relationship between external threats and smoking in central Harlem. Am J Public Health. 2000;90(3):367–71. doi: 10.2105/ajph.90.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rod N, Grønbæk M, Schnohr P, Prescott E, Kristensen T. Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J Intern Med. 2009;266(5):467–75. doi: 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- 61.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief. 2013;(133):1–8. [PubMed] [Google Scholar]
- 62.Taylor SE, Lerner JS, Sage RM, Lehman BJ, Seeman TE. Early environment, emotions, responses to stress, and health. J Pers. 2004;72(6):1365–93. doi: 10.1111/j.1467-6494.2004.00300.x. [DOI] [PubMed] [Google Scholar]
- 63.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 64.Lancaster J. Violence as a public health problem. Fam Community Health. 2010;33(2):79. doi: 10.1097/FCH.0b013e3181dbdf4b. [DOI] [PubMed] [Google Scholar]