Abstract
Iranian Mental Health Survey (IranMHS) was conducted to assess the twelve-month prevalence and severity of psychiatric disorders in the Iranian adult population and to determine the pattern of health care utilization and cost of services. IranMHS is a cross-sectional national household survey with face-to-face interviews as the main data collection method. The study was carried out between January and June 2011. A three-stage probability sampling was applied for the selection of a representative sample from the non-institutionalized population aged 15 to 64. The primary instrument utilized for assessing the prevalence of mental disorders was the Persian version of Composite International Diagnosis Interview, version 2.1. The instruments for assessing the service and cost of mental illness were developed by the research team. The response rate was 86.2%, and a total of 7886 individuals participated in the study. Sampling weights were the joint product of inverse probability of unit selection, non-response weights and post-stratification weights. This paper presents an overview of the study design, fieldwork organization and procedures, weightings and analysis. The strengths and limitations of the study are also discussed.
Keywords: Epidemiology, mental disorders, health service utilization, research design, costs, Iran
Iran is a large country located in the Middle East with a population of more than 75 million (1). Iranians are from Indo-European race and their official language is Persian. More than 71% of the population is living in urban areas and around 99 percent are Muslim (1). Adult literacy rate is 85% (2). Iran is classified as an upper middle income country with GNI per capita of 4520 US$ in 2009 (3) and ranks as 88th in terms of human development index (4).
Iran’s 2003 national study on burden of diseases reported that neuropsychiatric diseases had the highest burden only after injuries and disasters and were contributing to 16.04 % of the burden of diseases (5). Since then, the health sector is giving a high priority to mental health planning, service development and research.
To date, two large national household surveys have been carried out on the prevalence of psychiatric disorders. The first which was conducted in 1999 on 35,014 individuals aged 15 and over using General Health Questionnaire (GHQ-28) showed 21.5% point prevalence for psychiatric disorders (6). The second was carried out in 2001 on 25,180 individuals aged 18 and over, by means of the Schedule for Affective Disorders and Schizophrenia (SADS) and reported 10.8% lifetime prevalence for psychiatric disorders (7). In addition, a systematic review on the prevalence of psychiatric disorders in Iran included 35 studies and showed that the prevalence estimates varied in the range of 1.9-58.8%. The median point prevalence was 28.7% in screening studies and 18.6% in studies using diagnostic interviews. Pooled estimates were obtained through meta-analysis for screening, and diagnostic studies were 29.1% and 21.9%, respectively (8).
Iranian Mental Health Survey (IranMHS) was conducted in 2011 to evaluate the twelve-month prevalence and severity of psychiatric disorders in the Iranian adult population and to determine the pattern of health care utilization and cost of services.
Study Rationale
There were many reasons for carrying out a comprehensive household survey on psychiatric disorders in Iran. First of all, mental health authorities needed reliable and up-to-date information on the epidemiology of psychiatric disorders for the effective development of mental health plans and strategies to allocate resources. A nationwide representative epidemiologic study is an opportunity to produce useful information for planning mental health services. In the meantime, a scientometric study on Iranian mental health scientific products showed a decline in mental health service research over time (9). Second, the information on psychiatric disorders and the associated factors can generate a valuable context for creating many theories that can be tested in the future. Third, it could be a first step to develop a repeated national survey to monitor the mental health of the general population and trends of the protective and risk factors. Finally, the previous national surveys conducted in 1999 (6) and 2001 (7) showed conflicting results and lacked data on service utilization. The study on the burden of diseases and injury in Iran conducted in 2003 (5) documented a large information gap between various psychiatric disorders in terms of prevalence, course, severity, associated disability and treatment adequacy.
In 2006, Mental Health Office of Ministry of Health and Medical Education in collaboration with Tehran University of Medical Sciences started planning IranMHS. Several meetings were held with the key persons of mental health sector of Ministry of Health and Medical Universities. The core research team conducted an extensive review of the literature and made contacts with national and international experts in epidemiological assessment of mental illness to provide a clear background for designing and developing the national mental health survey in Iran.
Aims
The aims of the survey were
To estimate the 12 month prevalence of major psychiatric disorders and problems among the Iranian population aged 15 to 64 living in Iran;
To investigate the associations between psychiatric disorders and socio-demographic variables;
To measure the severity and social disability associated with psychiatric disorders;
To estimate unmet need, the barriers to service utilization and the level of receiving minimally adequate treatment for people with psychiatric disorders and the socio-demographic factors associated with inadequate service use. The patterns of service utilization for psychiatric disorders and other mental health problems and issues were also studied.
To assess the costs of psychiatric disorders, including health and non-health direct costs and indirect cost due to work loss.
Study Design
The study consisted of two phases: 1) a preparatory phase, in which the instruments were prepared and a pilot study in a sample of the general population was carried out; 2) the main study. Below, the two phases are described in their time order.
Preparatory Phases
Development of Instruments
The following studies were conducted to prepare the study instruments:
Clients (n = 72) were recruited from two psychiatric outpatient services in Tehran. The concurrent validity of telephone vs face-to-face interview of the Structured Clinical Interview for Diagnostic (SCID) and Statistical Manual of Mental Disorders, Fourth Edition, for diagnosis of “any psychotic disorder” was assessed.
Inpatient and outpatient cases (n = 104) from two psychiatric hospitals in Tehran were assessed for the following objectives: inter-rater reliability of the drug and alcohol module of the CIDI 2.1, internal consistency and convergent validity of the Persian version of the Sheehan Disability Scale (SDS), the inter-rater reliability of the questionnaire for suicidal thoughts and behaviors and the validity of a researchers-made short form for the assessment of drug and alcohol use in the last 12 months.
Outpatient clients of a primary health care clinic in Tehran (n=60) were asked to participate in a study for the assessment of inter-rater reliability of the drug and alcohol module of the CIDI 2.1 and the inter-rater reliability of service use and cost for outpatient services.
Inpatient cases from two psychiatric hospitals in Tehran (n=60) were assessed for the reliability of service use and cost for inpatient services.
During the pilot phase of the study on the general population in an area of Tehran, and an urban and rural area of Khoozestan province in South-west of Iran, 73 individuals were asked to participate, and the inter-rater reliability, as well as internal consistency and known group validity of the Persian version of the Sheehan Disability Scale (SDS) were assessed. In addition, the inter-rater reliability of the following questionnaires were also investigated: CIDI 2.1, questionnaire for assessment of aggression, screening questionnaire on service use for mental disorders and problems, the instrument for assessing the socio-economic status (SES), short form for the assessment of drug and alcohol use, the primary screening tool for somatoform disorders, Mood Disorder Questionnaire (MDQ) and the questionnaire for suicidal thoughts and behaviors.
Pilot Phase
A pilot study, which was a miniature of the national study, was carried out in the summer of 2010. The aim of the pilot study was to investigate the feasibility and limitations in the study design. The pilot study was conducted in an area of Tehran, the capital city of Iran, as well as an urban and rural area of Khoozestan province in South-west of Iran, where the mother language of a part of population was Arabic. A total of 192 households were selected.
In the pilot phase, it was presumed that the national study will be carried out in two stages: The first stage for the assessment of psychiatric disorders and the second stage for evaluating the cost of the used service and those whose data analysis showed to be positive for any psychiatric disorder in the past twelve months. However, the pilot phase showed a low feasibility of carrying out the study in two stages, and we decided to implement both in one stage. In order to design it as a one-stage survey, we added screening questions for service use. All who had used any services for any mental health problem in the past twelve months were requested to answer the details about their service use and cost. The only problem for implementing the national study in one stage was the length of the interview. Therefore, we removed Global Assessment of Functioning (GAF), Major Life Events Checklist and some parts of CIDI with less importance and lower level of reliability, such as somatoform disorders, specific phobia and cognitive disorders. In order to further shorten the duration of the interview, we also decided to administer GHQ-28 for half of the sample and the short form of the questionnaire on drug use and sexual dysfunction in another half.
Several procedures were used in order to assess the feasibility of the data collection methods. We assessed the opinions of all participants of the pilot study on different aspects of the interview. All of the questionnaires were evaluated for possible filling errors. Moreover, a focus group discussion with all managers and interviewers involved in the pilot phase was carried out, and various aspects of the field work and the instruments were discussed. We modified the data collection and quality control procedures for the national study according to the experiences and feedback from the implementation of the pilot phase.
The main study
IranMHS was a cross-sectional national household survey, and performing face-to-face interviews with the individuals was the main data collection method. The study was carried out between January and June 2011.
Sampling
A three-stage probability sampling was applied for the selection of a representative sample from the non-institutionalized population aged 15 to 64. In the first stage, the first stratum was the province level and a probability sample of 1525 blocks was selected from all provinces in the country. The number of blocks in each province was determined proportional to size of the province population. The blocks were the smallest geographic units of buildings or rural land segments confined by the public paths or natural structures within the districts. The blocks were selected from the national list of blocks developed from 2006 national census. The number of households in each selected block ranged from three to 1326 with a mean of 62.6. If the number of households in the block was less than 6, the interviewers were allowed to add the adjacent block located in the east side of the first block to find more households. The second stage was to select 6 households within each block by a systematic random sampling scheme. For this selection, interviewers visited and mapped each block, counted the number of households and divided it to six to determine the “sampling interval” (K). With adding K repeatedly to a “random number” between one and K, selected from a table of random numbers, the six households were determined. In the third stage, all the residents were listed in the selected household by interviewing a household informant. A checklist of inclusion and exclusion criteria was filled out for all listed residents. The Kish grid method was used for selecting one person from the eligible members (10). The Kish grid tables were previously assigned for each household, and applying the appropriate Kish grid table was one of the items, which field managers and supervisors were checking as a quality control measure.
The sample size was calculated as the minimum number of the participants at the national level, which was enough to estimate the proportion of patients with severe mental disorder who received adequate treatment. This was the lowest prevalence from the list of objectives of the study and the sample necessary for estimating this proportion would have been greater than the sample needed for other estimations. The prevalence of severe mental disorder among the general population was estimated as 1%, and previous studies suggested that about 20% of these patients receive adequate treatment in Iran. If the acceptable error for this estimate was 10%, then the sample size would have been 6147 for the general population. The design effect for cluster sampling with 6 subjects in each cluster was estimated to be 1.2. Because we decided to have no substitutions for the participants who were not accessible or refused to participate in this study, we corrected the “non-response rate” in the sample size calculation. The non-response rate in similar studies ranged from 10% to 38% (average 24%). Therefore, the final sample size was calculated to be 9150 and included 1525 blocks.
Inclusion and Exclusion Criteria
The inclusion criteria consisted of Iranian residents aged 15 to 64. Those with any of the following criteria were excluded:
People who were not able to respond to questions due to any acute or severe illness
People who could not understand Persian language. It should be noted that although there are lots of various ethnicities with different languages in the country, the majority of people understand Persian, the official language of the country.
Those who could not be accessed in the total three months duration of the field work in each province such as those with long-term institutionalization, those who were traveling and students living in campus group housings.
Fieldwork Organization
Organization
In Iran, the health services all over the country are under the supervision of 45 universities of medical sciences. The executives of the mental health offices in the universities acted as the field managers of the survey. Two hundred and thirty two interviewers carried out the interviews under the supervision of the field managers. Ten experienced supervisors in the survey secretariat supervised the work of the field managers, provided continuous training and counseling and controlled the quality of the fieldwork.
Interviewers
The field managers selected the interviewers according to the criteria provided by the research team. The interviewers were all psychologists with a minimum of BA degree and some clinical experience and were familiar with the culture and language of the geographical area. Most of them were the mental health staff of the district they carried out the fieldwork in, and almost all were between 30 and 50 years of age. Each interviewer had an assistant from the opposite gender, who provided assistance in the logistics of the fieldwork and accompanied the interviewer to the homes of the respondents.
Training of the Interviewers
The 232 interviewers and 54 field managers underwent an intensive training in December of 2010. The training was provided by IranMHS study team and those researchers who translated and validated the Persian version of CIDI v.2. The training included 38 hours of interactive class, covering the following subjects: the study objectives, general interview techniques, ethical considerations, proper administration of CIDI and other questionnaires, sampling and the field work. In addition, each person participated in 10-hour mock interview sessions, interviewing and observing other interviews and 8-hour interview in a psychiatric hospital with cooperative patients. At the end, each interviewer and field manager passed an examination to be certified for the assignment.
Fieldwork Procedures
Several strategies were used to inform the households and encourage their cooperation. Before and during the Iran MHS fieldwork, numerous mass media messages and advertisements were broadcasted or published in national and local radio and television and newspapers in order to increase public awareness of the survey. In addition, when a selected block was first visited by an interviewer, posters introducing the Iran MHS study were installed in the crowded areas of the block, informing the residents that their home might have been selected randomly and the interviewers would make contact with them.
When a household was selected, and a resident was first contacted, the interviewer introduced the study and presented a brochure about the objectives of Iran MHS and the method of study. If nobody answered, the interviewer left the brochure with a message regarding the study and informed them that they would be contacted again. The brochure consisted of information about the importance of the study, its objectives and sample size, timeframe of the fieldwork, the responsible organizations and contact numbers for receiving additional information. The interviewer had to explore the time of availability of the selected household from the neighbors and approach the household or the selected individual for at least three times at different days and times from which one had to be a holiday.
After the selection of an individual for the main interview, if the person was available, the interviewer would explain the study and ask for his/her consent using a text for guidance. When the selected person announced the consent and was ready, the interview was started; otherwise an appointment was set for another appropriate time. If the individual was reluctant to participate in the study, the supervisor would contact the individual to provide more information and assurance on confidentiality. No other households were replaced in the case of non-response due to rejection or unavailability.
A short screening section was located at the beginning of the questionnaire and was administered to all respondents. Those household informants who were reluctant to be interviewed were asked to provide the list of the household members and were only asked the short screening section about the selected individual.
Typically, the interview took place in the respondent’s home. Interview in the closest public primary health care center was also offered for those individuals who were not willing to be interviewed at their home. The median length of the interview was 80 minutes, and the mean (±SD) was 87.8 (± 39.8) minutes. A gift was handed over to the interviewee at the end of the interview.
Quality Control of the Fieldwork
Controlling the quality of the fieldwork was done by the field managers and the supervisors in two levels. When the fieldwork was started, the whole process of the field work, including the sampling procedure in a block and the process of making the contact, obtaining the consent and interviewing the first two cases were observed by the field manager. The supervisor also witnessed a sampling process in a block and observed an interview during his/her visit to the field and provided additional on-site trainings and feedbacks. If necessary, more cases were observed.
The process of the second and third stage of the sampling, which had to be done by the interviewer, as well as the number of contacts with the households and the selected individuals and the outcomes of the contacts were recorded in the pre-designed forms. The forms were reviewed by the field managers and supervisors. Special attention was paid to the refusals and cases of non-contact.
The field manager reviewed all completed questionnaires and listed any errors and returned it to the interviewer within 72 hours to re-contact the respondent and obtain the correct data. The first five completed questionnaires of each interviewer and another 20% of the completed questionnaires were rechecked by the supervisor as well. In addition, there were several parts of the questionnaire where high rates of errors were detected in the first days of the fieldwork. The supervisors rechecked these parts in all completed questionnaires.
The field manager re-contacted ten percent of the respondents to each interviewer via telephone. The sampling within household, the overall behavior of the interviewer, the length of the interview and the answers to at least two screening questions were rechecked and recorded in the quality control sheets. The same method of re-contact was applied by the supervisor for two respondents per interviewer as well. If significant errors were found, the number of re-contacts was increased. The interviewer was contacted and provided by appropriate advice on the detected and reported errors. The interviewers who were found to have a low performance or showed intentional errors were dismissed from the study and all of their completed questionnaires were discarded. Overall, three interviewers were dismissed, and 251 questionnaires were removed and replaced.
To ensure continuous communication, each supervisor contacted the field manager every other night to follow-up with the progress and inquired about any possible problems in the ground. In addition, the survey’s website provided continuous training and feedback on important problems and errors. Tens of follow-up emails and letters were issued to inform the field managers and the interviewers on the frequently found errors.
The interviewers were paid on the basis of their functioning in the training course, the number of interviews, the length of the interviews, carrying out fieldwork in the remote areas, completing the assigned fieldwork on time and the quality of the filled questionnaires.
IranMHS Instruments
IranMHS instruments mainly composed of the following instruments: 1) for assessing psychiatric disorders and other mental health problems; 2) other instruments for determining the severity of mental illness and the functional impairments, for defining the pattern of service use and the barriers of using mental health care and for calculating the cost of mental illness. There were also other questionnaires to describe socio-demographic and socio-economic status of the study sample. The instruments are introduced below, and the detailed descriptions on the items are presented in Table 1.
Table 1.
List of sections of the Iranian Mental Health Survey (IranMHS) instruments and items of each section
| Section | Number of items | Rule for Filling out | Subjects of each section |
|---|---|---|---|
| Basic information | |||
| Household information | 10 | All household informants or respondents |
|
| Short Screening section for mental illness and service use | 3 | All household informants or respondents |
|
| Socio-demographic information | 17 | All respondents |
|
| Service use and cost of illness | |||
| Screening questionnaire for service use | 42 | All respondents |
|
| Inpatient psychiatric service use and costs | 35 | Respondents with history of psychiatric inpatient admission in L12M |
|
| Outpatient mental health services and costs | 38 | Respondents reported any need for professional intervention for mental health problems in LT |
|
| Other service use for mental illness and costs | 103 | Respondents reported any need for professional intervention for mental health problems in LT |
|
| Health services for medical problems and costs | 8 | All respondents |
|
| Admission to a hospital for medical reason and costs | 13 | Those hospitalized for medical reason in L12M |
|
| Other costs | 7 | All respondents |
|
| Mental disorders and problems | |||
| Anxiety disorders (section D & K, CIDI 2.1) | 36 | All respondents |
|
| Depressive disorders (section E, CIDI 2.1) | 54 | All respondents |
|
| Mania (section F, CIDI 2.1) | 22 | All respondents |
|
| Drug use disorders (section L, CIDI 2.1) | 22 | All respondents |
|
| Alcohol use disorders (section J, CIDI 2.1) | 18 | All respondents |
|
| Psychotic symptoms (section G, CIDI 2.1) | 21 | All respondents |
|
| Psychotic disorders (SCID-1) (Phone interview) | 20 | Those with positive screening for psychotic symptoms by CIDI |
|
| Screening for somatoform disorders | 15 | All respondents |
|
| MDQ | 15 | All respondents |
|
| ASEX | 5 | Literate and married respondents with even-numbered identification code |
|
| Suicidal thoughts and attempts | 6 | All respondents |
|
| Aggressive behaviors | 6 | All respondents |
|
| Short-form for drug & alcohol use and other risk behaviors | 12 | All respondents with even-numbered identification code |
|
| GHQ-28 | 28 | All respondents with odd-numbered identification code |
|
| Other questionnaires | |||
| Sheehan Disability Scale | 5 | All respondents |
|
| Physical injury | 8 | All respondents |
|
| Socio-economic status | 16 | All respondents |
|
Composite International Diagnosis Interview version 2.1 (CIDI 2.1)
It was the primary instrument employed to identify the subjects with psychiatric disorders in the past 12 months. It is a fully structured diagnostic interview based on Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and International Classification of Diseases- 10th Revision (ICD-10). The Persian version of the paper and pencil interview form (PAPI) of CIDI 2.1 had been validated and utilized for the Iranian general population (11). The study could not afford to produce and use Computerized Assisted Personal Interviewing (CAPI). Applying whole package of CIDI 2.1 was a time-consuming process and imposed boredom and exhaustion on both interviewers and respondents. We decided to consider the most important psychiatric disorders based on the available evidence in the national burden of diseases study (5) and through extensive discussion with several mental health stakeholders. The selected psychiatric disorders eventually were Major Depressive Disorder (MDD), Bipolar I & II Disorders (BID & BIID), dysthymia, panic disorder with/without agoraphobia, agoraphobia without history of panic disorder, social phobia, Generalized Anxiety Disorder (GAD), Obsessive-Compulsive Disorder (OCD), Post-Traumatic Stress Disorder (PTSD), drug use disorders and alcohol use disorders.
During the preparatory phase of the study, the inter-rater reliability of CIDI 2.1 was assessed in 73 individuals from the general population and showed kappa of 0.5 and more for different psychiatric disorders. In addition, inter-rater reliability of the drug and alcohol module of the CIDI 2.1 was assessed in two different groups: First, in 104 inpatient and outpatient individuals from two psychiatric hospitals, the kappa for inter-rater reliability was from 0.69 for cannabis dependence to 0.98 for opioid dependence and stimulant abuse. Second, in 60 outpatient clients of a primary health care clinic the kappa for inter-rater reliability was 0.9 and higher for use of more than four times of all drugs, which is the screening questions of the questionnaire.
Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I)
In the previous validation studies, the CIDI 2.1 did not show adequate psychometric properties for assessing psychotic disorders (12, 13). Therefore, a two-stage procedure was used for the detection of any psychotic disorders. In the first stage, the participants were screened to check any psychotic symptom in lifetime, such as delusion and hallucination using questions from the G section of the CIDI. In the second stage, all participants who had endorsed one or more items or had been hospitalized for a psychiatric illness in the past 12 months were contacted by telephone, and the Persian version of the SCID-I was applied to determine the presence of a psychotic disorder. The source of information was both the subject and the closest person in the household that usually included either a spouse or a first degree relative. The Persian translation of the SCID had showed acceptable to good reliability and validity indices (14). In addition, in the preparatory phase of our study, a comparison study between the face-to-face and telephone administration of the Persian version of the SCID in clients of outpatient psychiatric services showed adequate comparability to differentiate those with and without a psychotic disorder (15). The positive likelihood ratio of telephone-administered SCID for diagnosis of “any lifetime psychotic disorder” was 5.1 when compared with the face-to-face SCID. The results indicate that any lifetime delusion has the highest sensitivity: 88.2% of patients with any lifetime delusion in face-to-face interviews were also found to have lifetime delusion in telephone interviews.
Screening Tool for Somatoform Disorders
The section for somatoform disorders in CIDI 2.1 was too long and the pilot study showed that we had to shorten the length of the interview in order to combine all data collection procedures in a single phase. Therefore, we decided to use a screening instrument to study somatoform illnesses. We selected a screener that was developed by the World Health Organization (WHO) for use in the WHO International Study of Somatoform Disorders (16). It is a brief questionnaire consisting of 12 questions about common somatoform complaints such as pains and gastrointestinal problems, and the subjects were asked whether they have had three or more of these complaints together in the last 12 months for 3 or more months. Therefore, we added two questions to the screener: if positive to the abovementioned, whether they have consulted a physician or other health professionals for the complaints and if the physician/health professional believed that these symptoms are related to some psychiatric problem. The latter will provide us with a rough estimate of the prevalence of a somatoform illness in a general but not a specific DSM-IV disorder. The reliability study showed that the inter-rater administration yields fair to acceptable Kappa values.
Mood Disorder Questionnaire (MDQ)
The MDQ was applied to screen the history of bipolar disorder spectrum in lifetime. It is a short instrument, and the Persian version of the MDQ had been validated and provided good psychometric properties (17). During the preparatory phase of the study, we assessed the inter-rater reliability of MDQ in individuals from the general population. It showed a fair reliability.
The Arizona Sexual Experience Scale (ASEX): Sexual dysfunction was assessed by ASEX. It was attached to the short-form for drug and alcohol use and was completed by the same method. As the subject has a sensitive nature, it was just completed by married and literate respondents with even-numbered identification code. Psychometric properties of the ASEX have already been examined (18).
Questionnaire for Suicidal Thoughts and Behaviors
An instrument for assessment of suicide was developed by translating and modifying the instrument used in the World Mental Health (WMH) survey (19). In the preparatory phase of our study, the questionnaire was translated to Persian, and the inter-rater reliability was assessed in inpatient and outpatient psychiatric cases and showed an excellent reliability. In addition, its assessment in individuals from the general population showed a good reliability for suicidal thoughts, but the prevalence of suicidal behaviors was low and assessment of its reliability was not possible.
Questionnaire for Assessment of Aggression
The history of perpetrating violence in last 12 months was asked by a set of questions, which had been used in a general population sample before (20). During the preparatory phase of the study, the inter-rater reliability of the questionnaire was assessed in individuals from the general population and showed kappa of 0.6 for any aggression in last 12 months.
Short-Form for Drug and Alcohol Use and other High Risk Behaviors
IranMHS instruments included sections “L” and “J” of the 12-month version of the CIDI to assess drug and alcohol use disorders, which was completed almost at the end of the interview. However, some respondents might have been reluctant to respond to such questions during the face-to-face interview. Therefore, a self-administered and anonymous questionnaire was developed. It was about use of common abusive drugs in past 12 months and some other high risk behaviors and situations in life time.
In the preparatory phase of the study, we assessed the validity of the short form in comparison to the drug and alcohol modules of Composite International Diagnosis Interview, last 12 months, version 2.1 (CIDI 2.1). The study was carried out on inpatient and outpatient individuals from two psychiatric hospitals and showed that the questionnaire was understandable. It showed that the cut-off frequency of “daily or almost daily use” although is associated with the highest specificity (>95% for dependence and use disorder of all illicit drugs and alcohol), has a low sensitivity (from lower than 20% for alcohol use disorders to around 67% for opioid and cannabis dependence) and highly underestimate the diagnosis of substance use disorders. The best cut-off would be the frequency of “monthly use or more”, with a sensitivity of 71.4% for cannabis use disorders to 91.7% for opioid use disorders, and specificity of 94.1% for opioid use disorders to 98.7% for stimulant use disorders.
In addition, its inter-rater reliability was assessed in individuals from the general population. It showed a good reliability for smoking and alcohol use and poor reliability for abuse of prescription drugs. Assessment of reliability of illicit drug use was not possible due to the low prevalence. In the main national study, the questionnaire was placed in the middle of the interview package. It was separated from the package and was completed by the respondents, themselves. Then, they dropped the filled questionnaire in a ballot-type box. The box was opened by the field supervisors in the survey secretariat. The tool was completed by half of the respondents with even-numbered identification code.
28-items General Health Questionnaire (GHQ-28)
Psychological distress was assessed using GHQ-28. It provided an opportunity to compare the results with the previous national survey (6). GHQ-28 has been widely used in local and national level surveys, and the validation study of Persian version of the GHQ-28 has been already well documented (21). We applied this questionnaire for half of the interviewees who had odd-numbered identification code.
Service Use
In the preparatory phase of IranMHS, we developed a questionnaire to assess service use. For this purpose, two other instruments, “services” section of WMH survey and questionnaire used in “Health Services Utilization Study of Iran”, were used. Then, it was modified culturally and tailored according to the existing mental health care services in Iran. It consisted of inpatient and outpatient service use due to mental health problems and medical problems and barriers to mental health service use. Face and content validity of the questionnaire were evaluated through several focus group discussions, and its inter-rater reliability was studied in a group of clients of primary health care services and a group of inpatient cases of psychiatric hospitals. The inter-rater reliability for the items was from poor to excellent. As examples, the kappa for inter-rater reliability was 0.80 for “any lifetime referral for psychiatric problems” and 0.60 for any delay of 30 days or more to refer for psychiatric problems. The items with poor and fair reliability were reviewed and appropriate changes were made by considering the possible reasons for the low reliability.
Cost of Mental Illness
In the preparatory phase of IranMHS, we developed questionnaires for assessing the cost of mental illness or problem. It consisted of all direct health and non-health costs of mental and medical illnesses and indirect cost of loss of working days due to mental illness. Face and content validity and reliability of the developed questionnaires were studied in association with the questionnaire for service use.
Sheehan Disability Scale (SDS)
SDS is a short, self-reported scale, which was used to assess disability related to psychiatric problems in main functional domains. It was translated, and the Persian version of the SDS was validated in the preparatory phase for IranMHS (22). In the general population study, the SDS met a good internal consistency (α = 0.81). The inter-rater reliability was perfect for “school/work responsibility”. The analysis showed that the psychiatric cases (based on CIDI) had a significantly greater score of disability in all domains of the SDS and more days out of role than the non-cases.
Questionnaire on Socio-Demographic Characteristics
Socio-demographic characteristics assessed in the survey included age, sex, education, marital status, number of children, occupational status and insurance status.
Short Form Injury Questionnaire 7 (SFIQ-7)
This questionnaire includes main aspects of all injuries occurred for the individual in the last three months. It was developed and validated in the preparatory phase of IranMHS. The inter-rater reliability in a group of respondents from the general population showed fair to good reliability for different questions (23).
Socio-Economic Status (SES) Questionnaire
The SES questionnaire was applied in the “Health Services Utilization Study of Iran” (24). During the preparatory phase of the study, the inter-rater reliability of the SES questionnaire was assessed in the individuals from the general population and showed good reliability indices.
Ethical Considerations
The research protocol was approved by the Ethics Committee of Tehran University of Medical Sciences in Iran. The field workers were intensively trained about the ethical issues related to the study and signed a code of commitment. Participation in the study was on a voluntary basis, and informed consent was obtained for the interview. The participant could reject to respond to any part of the interview or any specific question as well. All efforts were made to guarantee privacy and confidentiality during the interviews. All questionnaires and databases of the study were kept confidential by the research team.
Response Rate
After obtaining a household listing, 21,687 out of 24,055 inhabitants aged 18-64 were found to be eligible. Table 2 shows the percentage of non-eligible inhabitants by each exclusion criteria. From 21687 eligible inhabitants, 9150 were selected randomly to be interviewed. A total of 7886 completed the interview. The total response rate was 86.2% which varied from 72.2% and 74% in Alborz and Tehran provinces to 100% in Chaharmahal-o-Bakhtiary and South Khorasan (Table 3).
Table 2.
Total eligible and excluded sample in selected households in Iranian Mental Health Survey (IranMHS)
| N | % | |
|---|---|---|
| Total inhabitants aged 15-64 in the households’ lists | 24055 | 100 |
| Non-eligible individuals (excluded inhabitants) | ||
| Not understood Persian language | 1163 | 4.8 |
| Not available until the end of survey | 879 | 3.7 |
| Severe mental/physical illness | 158 | 0.7 |
| Had more than one of above exclusion criteria | 168 | 0.7 |
| Eligible individuals for inclusion in the survey | 21687 | 90.2 |
Table 3.
Distribution of sample and the response rate in the different geographical regions of Iran
| Geographical region | Provinces | Universities of Medical Sciences | No. of blocks | No. of interviewers | Sample size | No. of completed interviews | Response rate |
|---|---|---|---|---|---|---|---|
| North west | Guilan | Guilan | 52 | 8 | 312 | 276 | 88.5 |
| Ardabil | Ardabil | 27 | 4 | 162 | 132 | 81.5 | |
| Azarbaijan-e-Sharqi | Tabriz | 77 | 11 | 462 | 419 | 90.7 | |
| Zanjan | Zanjan | 21 | 3 | 126 | 123 | 97.6 | |
| Azarbaijan-e-Gharbi | Urmia | 61 | 9 | 366 | 349 | 95.4 | |
| West | Kurdistan | Kurdistan | 31 | 5 | 186 | 172 | 92.5 |
| Lorestan | Lorestan | 38 | 6 | 228 | 219 | 96.1 | |
| Ilam | Ilam | 11 | 2 | 66 | 60 | 90.9 | |
| Kermanshah | Kermanshah | 41 | 6 | 246 | 228 | 92.7 | |
| Hamadan | Hamadan | 36 | 5 | 216 | 161 | 74.5 | |
| Central | Tehran | Tehran | 71 | 10 | 426 | 1088 | 74.0 |
| Iran | 80 | 12 | 480 | ||||
| Shahid Beheshti | 94 | 14 | 564 | ||||
| Qom | Qom | 23 | 4 | 138 | 135 | 97.8 | |
| Alborz | Alborz | 45 | 6 | 270 | 195 | 72.2 | |
| Qazvin | Qazvin | 25 | 4 | 150 | 138 | 92.0 | |
| South-East | Sistan-o-Baluchestan | Zahedan | 45 | 7 | 270 | 310 | 95.7 |
| Zabol | 9 | 2 | 54 | ||||
| Hormozgan | Hormozgan | 31 | 5 | 186 | 174 | 93.5 | |
| Kerman | Kerman | 40 | 6 | 240 | 323 | 96.1 | |
| Jiroft | 10 | 2 | 60 | ||||
| Rafsanjan | 6 | 1 | 60 | ||||
| South-West | Isfahan | Isfahan | 90 | 13 | 540 | 582 | 98.0 |
| Kashan | 9 | 1 | 54 | ||||
| Markazi | Arak | 22 | 3 | 132 | 121 | 92.0 | |
| Chaharmahal-va-Bakhtiari | Shahrekord | 19 | 3 | 114 | 114 | 100 | |
| Khuzestan | Ahvaz Jundishapur | 82 | 12 | 492 | 494 | 89.5 | |
| Dezful | 10 | 1 | 60 | ||||
| North | Semnan | Semnan | 8 | 1 | 48 | 69 | 88.5 |
| Shahroud | 5 | 1 | 30 | ||||
| Mazandaran | Mazandaran | 53 | 8 | 318 | 337 | 89.2 | |
| Babol | 10 | 2 | 60 | ||||
| Golestan | Golestan | 35 | 5 | 210 | 178 | 84.8 | |
| North-east | Khorasan-e-Razavi | Mashad | 93 | 13 | 558 | 623 | 85.8 |
| Torbat Heydariyeh | 6 | 1 | 36 | ||||
| Gonabad | 2 | 1 | 12 | ||||
| Sabzevar | 10 | 1 | 60 | ||||
| Nishapur | 10 | 2 | 60 | ||||
| Khorasan-e-Jonubi | Birjand | 13 | 2 | 78 | 78 | 100 | |
| Khorasan-e-Shomali | North Khorasan | 17 | 3 | 102 | 91 | 89.2 | |
| South | Fars | Shiraz | 85 | 12 | 510 | 534 | 95.7 |
| Fasa | 4 | 1 | 24 | ||||
| Jahrom | 4 | 1 | 24 | ||||
| Bushehr | Bushehr | 20 | 3 | 120 | 113 | 94.2 | |
| Kohgiluyeh-va-Boyer-Ahmad | Yasuj | 14 | 2 | 84 | 80 | 95.2 | |
| Yazd | Shahid Sadoughi | 22 | 3 | 132 | 121 | 91.7 |
The mean (± SD) number of in-person call attempts was 1.8 (± 1.0) and the median was 2. The minimum and maximum number of such attempts was 1 and 8, respectively. The diagram of the selected sample and the outcome of contact and response are shown in Figure 1. Overall, some families or the individuals refused to participate in the study in 835 (9.1%) cases. In another 328 cases (3.6%), it was not possible to contact the family or the selected individual.
Fig 1.
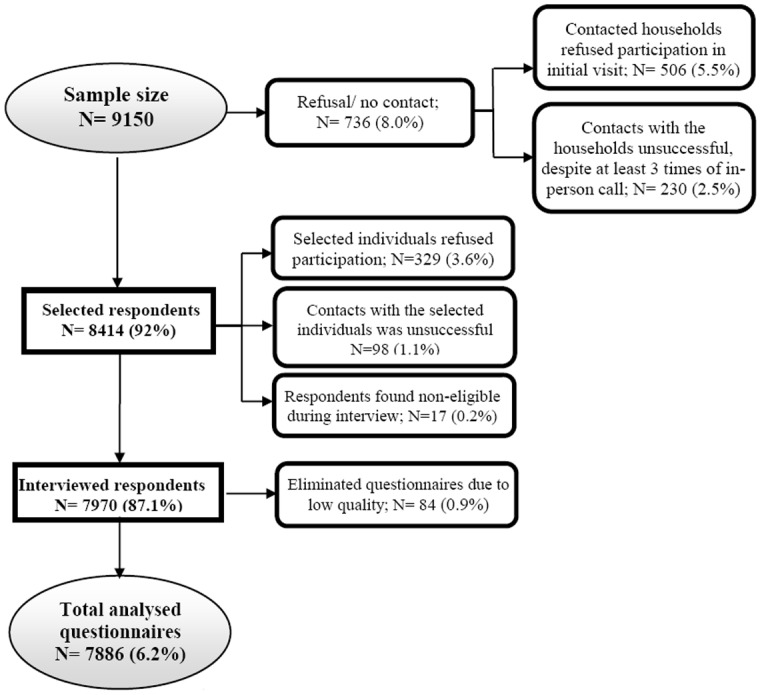
Flowchart of sample disposition in Mental Health Survey (IranMHS)
A short screening section was located at the beginning of the questionnaire and was administered to all respondents. Those household informants who were reluctant to be interviewed were asked to provide the list of household members and only responded to the short screening section about the selected individual. A total of 440 families (47.2% of 933) who were contacted, but did not respond to other parts of the questionnaire responded to these questions. The non-responder group included a higher percentage of men (56.3% vs 43.0%, p<0.001) and a higher average age (34.7 vs 33.0, p=0.004). This non-response group reported a lower prevalence of mental problems in the past 12 months than those who responded to other questionnaires (13.0% vs 27.2%, p<0.001). They also reported a lower rate of referral for treatment services for their mental problems in the past 12 months (4.5% vs 10.1%, p<0.001).
Analysis
Data Entry and Data Cleaning
Data were entered to PASW 18 (SPSS Inc., Chicago, IL, 2010) and were checked for inconsistencies and errors. Skipping errors were identified and corrected. The out-of-range data were compared with the original questionnaires and if necessary phone calls were made to subjects to correct the data. We used official WHO scoring programs to extract 12-months DSM-IV diagnoses from the questionnaire data.
Sampling Weights and Statistical Analysis
Sampling weights were calculated so that each respondent can be inflated to represent other individuals in Iran. The consolidated weights (w) were the joint product of inverse probability of unit selection into the sample (w1), non-response weights (w2) and post-stratification weights (w3). w=w1*w2*w3
To calculate the post-stratification weights (w3), the proportion of subjects in each stratum in National Census 2006 was divided by the proportion of the same group in the sample. Based on 5-year age groups, sex and urbanicity status in each of 31 country provinces, 1240 post-stratification weights were generated.
We used STATA version 10.0 to perform complex sample analysis. Table 4 demonstrates how sampling weights and complex sample analysis helped to achieve better national estimates.
Table 4.
Weighted and un-weighted sample by demographic characteristics
| Characteristic* | Number in the sample | Proportion in the sample | Estimated proportion (complex sample analysis) | Proportion in the population (Census 2006) | |
|---|---|---|---|---|---|
| Age groups | 15-19 | 998 | 12.7 | 18.1 | 17.8 |
| 20-24 | 1222 | 15.5 | 18.7 | 18.3 | |
| 25-29 | 1327 | 16.8 | 15.0 | 14.7 | |
| 30-34 | 1239 | 15.7 | 11.6 | 11.3 | |
| 35-39 | 961 | 12.2 | 10.2 | 10.0 | |
| 40-44 | 696 | 8.8 | 8.4 | 8.3 | |
| 45-49 | 492 | 6.2 | 6.9 | 7.2 | |
| 50-54 | 398 | 5.1 | 5.3 | 5.6 | |
| 55-59 | 306 | 3.9 | 3.4 | 3.8 | |
| 60-64 | 247 | 3.1 | 2.5 | 3.0 | |
| Sex | Male | 3387 | 43.0 | 50.5 | 50.6 |
| Female | 4499 | 57.0 | 49.5 | 49.4 | |
| Urbanicity | Urban | 4380 | 55.5 | 70.9 | 70.3 |
| Rural | 3506 | 44.5 | 29.1 | 29.7 | |
| Employment | Employed | 2803 | 35.6 | 38.4 | 40.0 |
| Student | 937 | 11.9 | 17.0 | 14.5 | |
| Retired | 166 | 2.1 | 2.4 | 2.2 | |
| Home maker | 3241 | 41.1 | 32.7 | 30.7 | |
| Unemployed | 737 | 9.4 | 9.5 | 5.9 | |
| Marital status | Never married | 2025 | 25.7 | 33.0 | 34.5 |
| Married | 5527 | 70.1 | 63.5 | 62.3 | |
| Ex-married | 332 | 4.2 | 3.6 | 3.2 | |
The weightings were done only for the first three variables
Strengths and Limitations of the Study Design
The study design had several strengths. It was the first national study that provided detailed information on prevalence, severity and cost of several most important mental disorders, as well as service use for mental disorders and problems. We used CIDI, which has been widely used in other national (25-27) and multi-national studies (28, 29); therefore, it creates an excellent opportunity to compare the results with studies in other countries. We used one-step field work, and the respondents responded to all relevant questions during the interview. We applied high standards in the data collection procedures, which was essential for such a comprehensive national mental health survey. The response rate was 86.2%, which shows a very good rate compared to many other national studies. The response rate in the World Mental Health Study in 15 countries was between 45.9% in France and 87.7% in Columbia (28). In addition, although generally it is expected that those who refuse to be interviewed have higher rates of mental disorders than those who participate in the study (30), our non-response group showed a lower prevalence of mental disorders than those who responded. The Netherlands Mental Health Survey has also reported a similar finding (25).
The study has some limitations as well. It was not possible to include the assessment of all mental disorders. We selected the most important disorders based on the available evidence produced by the national burden of diseases study and through extensive discussions with mental health stakeholders. This was a household study, and certain disorders, but the overall number is low and it does not seem to considerably affect the results, at least for more common disorders. In addition, it was not possible for us to prepare several versions of CIDI in local languages. Therefore, we also excluded those who could not understand Persian, the official language of Iran. This group consisted of 4.8% of individuals in the approached households and it is not known whether psychiatric morbidity is different in this minor group. In addition, we excluded those who were not able to respond to questions due to any acute or severe physical or mental illness. This group consisted of only 0.7% and it does not seem that excluding this group has significantly affected the results. We used the paper-and-pencil procedure. Although computer-assisted interview has several advantages over the paper-and-pencil administration (31), utilizing the technology was not feasible in the whole country.
Conclusion
This was the first comprehensive national mental health study that covers both prevalence and service utilization aspects of psychiatric problems. It applied high standards of methodological procedures and quality of data collection and a very high response rate. The study has provided a great deal of information, and it will take many years to analyze and publish the whole produced data. The findings of this study will lead to a better understanding of mental health problems and needs of our population and will also help the public health planners to improve preventive, treatment and care services.
Acknowledgments
The study was financially supported by the Ministry of Health through the contract number 132-1491 of Tehran University of Sciences and the contract number 89-D-432-143 of Mental Health Research Network.
The authors acknowledge supports received from Dr Ali Reza Mesdaghinia, Dr Hassan Emami Razavi, Dr Abbas Ali Nasehi, Dr Mohammad Bagher Saberi Zafarghandi, Dr Mohammad Reza Mohammadi and Dr Minoo Mohraz and contribution of Dr Shahrokh Sardarpour Goodarzi, Dr Firouzeh Raisi, Dr Samaneh Kariman, Maryam Gholamrezaei, Leila Moazami Goodarzi, Farideh Kolahi Heshmat, Dr Reza Mahdavi, and Fahima Farrahi in conducting the study. We also wish to thank provincial field managers and interviewers, as well as all the participants in the study.
References
- 1.Statistical Center of Iran. Selected findings of the 2011 national population and housing census. Tehran, Iran: 2012. [19 Dec 2012] Available from: http://www.amar.org.ir/portals/1/iran/census-2.pdf. [Google Scholar]
- 2.UNESCO Institute for Statistics. Key statistics and indicators on literacy. The United Nations Educational Scientific and Cultural Organization Institute for Statistics; 2012. [9 April 2012]Available from: http://stats.uis.unesco.org/unesco/tableviewer/document.aspx?ReportId=143&IF_Language=en. [Google Scholar]
- 3.The World Bank. Data on Economies by country. 2012 Available from: http://data.worldbank.org/country.
- 4.The United Nations Development Programme. Country Profiles and International Human Development Indicators. UNDP; 2011. Available from: http://hdr.undp.org/en/countries. [Google Scholar]
- 5.Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003. Popul Health Metr. 2009;7:9. doi: 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noorbala AA, Yazdi SAB, Yasamy MT, Mohammad K. Mental health survey of the adult population in Iran. British Journal of Psychiatry. 2004;184:70–73. doi: 10.1192/bjp.184.1.70. [DOI] [PubMed] [Google Scholar]
- 7.Mohammadi MR, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, et al. An epidemiological survey of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farhoudian A, Sharifi V, Amini H, Basirnia A, Mesgarpour B, Mansouri N, et al. Prevalence of psychiatric disorders in Iran: A systematic review. Iran J Psychiatry. 2007;2:137–150. [Google Scholar]
- 9.Sharifi V, Rahimi-Movaghar A, Mohammadi MR, Goodarzi RR, Izadian ES, Farhoudian A, et al. Analysis of mental health research in the Islamic Republic of Iran over 3 decades: a scientometric study. East Mediterr Health J. 2008;14:1060–1069. [PubMed] [Google Scholar]
- 10.Kish L. A Procedure for Objective Respondent Selection within the Household. J Am Stat Assoc. 1949;44:380–387. [Google Scholar]
- 11.Alaghband Rad J. Study of the reliability, validity, and feasibility of Farsi translation of the Composite International Diagnostic Interview (CIDI) In: Ahmadi Abhari SA, Malakooti K, Nasr Esfahani M, Razzaghi EM, Sadeghi M, Yasamy MT, editors. Mental health effects of Iraqi invasion of Kuwait in a war – torn population of Iran: an epidemiological and financial study of the consequences of the Kuwaiti oil well fire disaster in the aftermath of Iraqi invasion of Kuwait in 1991, United Nations Compensation Commission (UNCC) Monitoring and Assessment Project. Tehran - Iran: Islamic Republic of Iran Ministry of Health, Committee for assessment and follow up for damages resulting from the Iraq–Kuwait War; 2003. [Google Scholar]
- 12.Cooper L, Peters L, Andrews G. Validity of the Composite International Diagnostic Interview (CIDI) psychosis module in a psychiatric setting. J Psychiatr Res. 1998;32(6):361–8. doi: 10.1016/s0022-3956(98)00021-1. [DOI] [PubMed] [Google Scholar]
- 13.Wittchen HU. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 14.Sharifi V, Assadi SM, Mohammadi MR, Amini H, Kaviani H, Semnani Y, et al. A Persian translation of the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders Fourth Edition: psychometric properties. Vol. 50. Compr Psychiatry: 2009. pp. 86–91. [DOI] [PubMed] [Google Scholar]
- 15.Hajebi A, Motevalian A, Amin-Esmaeili M, Hefazi M, Radgoodarzi R, Rahimi-Movaghar A, et al. Telephone versus face-to-face administration of the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, for diagnosis of psychotic disorders. Vol. 53. Compr Psychiatry; 2012. pp. 579–583. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. WHO international study of somatoform disorders: Study Protocol and instruments. Jeneva: WHO. 1994 [Google Scholar]
- 17.Shabani A, Koohi-Habibi L, Nojomi M, Chimeh N, Ghaemi SN, Soleimani N. The Persian Bipolar Spectrum Diagnostic Scale and mood disorder questionnaire in screening the patients with bipolar disorder. Arch Iran Med. 2009;12:41–47. [PubMed] [Google Scholar]
- 18.Raisi F, Asadi M, Nejatisafa AA, Mehdizadeh Z. Arizona Sexual Experience Scale (ASEX): Persian Translation and cultural Adaptation. 20th World Congress for Sexual Health; Glasgow; United Kingdom: 2011. [Google Scholar]
- 19.Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71:1617–1628. doi: 10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mojtabai R. Psychotic-like experiences and interpersonal violence in the general population. Soc Psychiatry Psychiatr Epidemiol. 2006;41:183–190. doi: 10.1007/s00127-005-0020-4. [DOI] [PubMed] [Google Scholar]
- 21.Noorbala AA, Bagher Yazdi SA, Mohammad K. Validation of GHQ28 as a psychiatric screening tool [Abstract in English, Full text in Persian] Hakiim Research Journal. 1999;11:47–53. [Google Scholar]
- 22.Amin-Esmaeili M, Motevalian A, Rahimi-Movaghar A, Hajebi A, Hefazi M, Rad Goodarzi R, et al. Sheehan disability scale: translation and psychometric validation of the Persian version. Iran J psych. 2014;9 In print. [PMC free article] [PubMed] [Google Scholar]
- 23.Sharif-Alhoseini M, Saadat S, Rahimi-Movaghar A, Motevalian A, Amin-Esmaeili M, Hefazi M, et al. Reliability of a patient survey assessing “Short Form Injury Questionnaire 7” in Iran. Chin J Traumatol. 2012;15:145–147. [PubMed] [Google Scholar]
- 24.Naghavi M, Jamshidi HR. Utilization of Health Services. Tehran, Iran: Ministry of Health, Applied Researches Secretaria; 2005. [Google Scholar]
- 25.Bijl RV, van Zessen G, Ravelli A, de Rijk C, Langendoen Y. The Netherlands Mental Health Survey and Incidence Study (NEMESIS): objectives and design. Soc Psychiatry Psychiatr Epidemiol. 1998;33:581–586. doi: 10.1007/s001270050097. [DOI] [PubMed] [Google Scholar]
- 26.Henderson S, Andrews G, Hall W. Australia’s mental health: an overview of the general population survey. Aust N Z J Psychiatry. 2000;34:197–205. doi: 10.1080/j.1440-1614.2000.00686.x. [DOI] [PubMed] [Google Scholar]
- 27.Jacobi F, Wittchen HU, Holting C, Hofler M, Pfister H, Muller N, et al. Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German Health Interview and Examination Survey (GHS) Psychol Med. 2004;34:597–611. doi: 10.1017/S0033291703001399. [DOI] [PubMed] [Google Scholar]
- 28.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Jama. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 29.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]


