Abstract
The purpose of this study was to examine a model of the relationships between parenting deficits and skills, along with child outcomes, in a sample of mothers living with HIV (MLH) and their 6 to 14 year old children. Sixty-two MLH (61% Latina, 26% black, 3% white, & 10% multiracial) and their well children (age 6 – 14) were recruited from the greater Los Angeles, California, region to participate in an intervention (IMAGE: Improving Mothers’ parenting Abilities, Growth, and Effectiveness) designed to assist MLH with parenting and self-care skills. Constructs examined included parenting deficits, parenting skills, and child outcomes. Covariance structural modeling was used for the analyses. Covariance structural modeling confirmed the hypothesized set of construct associations. As predicted, fewer parenting deficits were associated with better parenting skills, which, in turn, were associated with better child outcomes. This study delineated further the parenting issues with which MLH struggle, providing information on the interventions needed for this population. MLH who have little confidence they can enact parenting skills and limited knowledge of basic parenting practices appear to be less likely to provide family routines consistently, monitor their children, or to engender family cohesion or a close parent-child relationship. Such parenting skills were found to be associated with child functioning.
Introduction
Maternal Illness & Parenting Deficits
Ill parents express anxiety about being less able to meet their children’s needs (Altschuler & Dale, 1999), and feel unprepared to struggle with parenting issues. For example, mothers with chronic pain have been found to engage in lax parenting and report reduced relationship quality with children compared to control mothers (Evans, Shipton, & Keenan, 2006). Mothers living with HIV (MLH) report their greatest source of stress is combining the maternal with the psychological and medical demands of coping with a chronic life-threatening condition. In fact, MLH report compromised parenting skills across a variety of parenting domains.
Many MLH express concerns about parenting deficits (i.e., poor parenting practices, lack of parental involvement, poor parenting style) through reports of lower levels of parenting self-efficacy relative to uninfected women (Dorsey, Klein, Forehand, & Family Health Project Research Group, 1999). MLH also have difficulty implementing parenting skills, including poorer and/or less frequent family routines, insufficient parental monitoring, and poorer mother-child relationships (e.g., Murphy, Marelich & Amaro, 2009; Murphy, Marelich, Herbeck, & Payne, 2009). In a number of these studies, the mothers’ level of illness is associated with parenting (cf., Murphy, Marelich, Hoffman, & Schuster 2006). Dorsey and colleagues (Dorsey et al., 1999) found a linear increase in children’s report of externalizing (i.e., acting out behaviors) and internalizing (i.e., emotional distress) difficulties as their mothers progressed through stages of HIV infection and then AIDS. Thus, evidence suggests that maternal HIV infection may disrupt effective parenting.
Effect of Maternal Illness on Child Outcomes
The body of research at the intersection of parental illness and child outcomes is relatively young (Russell & Rauch, 2012). Prior to studies focused on parental HIV, most research focused on children affected by parental cancer. In a review of 15 years of literature on children of ill parents by Romer and colleagues (Romer, Barkmann, Schulte-Markwort, Thomalla, & Riedesser, 2002), it was reported that overall children of seriously ill parents had higher scores than controls on symptom scales, with a tendency towards internalizing symptomatology. Several studies (e.g., Bauman, Silver, Draimin, & Hudis, 2007; Hough, Brumitt, Templin, Saltz, & Mood, 2003; Murphy & Marelich, 2008; Murphy, Marelich, & Herbeck, 2012; Reyland, McMahon, Higgins-Delessandro, & Luthar, 2002) have demonstrated that parental HIV is associated with negative outcomes for children. Moreover, these negative outcomes did not result from direct knowledge about maternal infections (Forehand et al., 2002).
Armistead, Klein, and Forehand (1995) noted that HIV-infected parents’ physical illness appears to be associated with some difficulties in child functioning, however, particular areas affected varied substantially across and within studies. A number of factors may be related to outcomes among children affected by parental HIV (e.g., Murphy, Armistead, Marelich, Payne, & Herbeck, 2011; Murphy, Marelich, Graham, & Payne, in press; Murphy, Marelich, Hoffman, & Schuster, 2006). Some studies have reported that parental HIV is associated with child depressive symptoms (Esposito et al., 1999; Murphy Greenwell, Mouttapa, Brecht, & Schuster, 2006; Murphy, Marelich, & Hoffman, 2002), and with acting out behavior (Forehand et al., 1998). Reyland, McMahon, Higgins-Delessandro, & Luthar (2002) compared the psychosocial adjustment of children 11 to 16 years of age living with a seropositive mother to children attending public school. After statistical models adjusted for child age and gender, the HIV-affected group showed poorer psychological functioning. The authors suggested that risk for psychosocial maladjustment in children living with an HIV-seropositive parent extends through late childhood into early to middle adolescence. In our 12-year longitudinal study of children affected by maternal HIV (conducted with a different sample than that of the current study), results show a negative effect of maternal health status on child/adolescent outcomes, including child/adolescent depression, anxiety/worry, aggression, and self-concept (Murphy, Marelich, & Herbeck, 2012). Interaction effects within the growth models suggest younger children are more impacted by poor maternal health than are older children/adolescents.
Theoretical Model
This study can be conceptualized according to a model proposed by Darling & Steinberg (1993) in which parenting style, and parenting practices and behaviors, influence child outcomes. Parenting style and parenting practices influence the child’s development through different processes; parenting practices have a direct effect on the development of specific child behaviors, while the primary processes through which parenting style influences child development are indirect, altering the parents’ capacity by changing the effectiveness of specific practices. Parenting style can be viewed as a contextual variable that moderates the relationship between specific parenting practices and child developmental outcomes. Parenting style communicates the emotional attitude but is not goal-directed or goal-defined, and is expressed partly through parenting practices, whereas parenting practices are behaviors defined by specific content and socialization goals.
Darling and Steinberg recognize that these parenting processes may (and probably do) vary as a function of other influences outside the immediate setting (e.g., socioeconomic class). Accordingly, in families affected by parental illness, such a stressor would be expected to influence parenting behaviors, and thus child outcomes.
Purpose of the Current Study
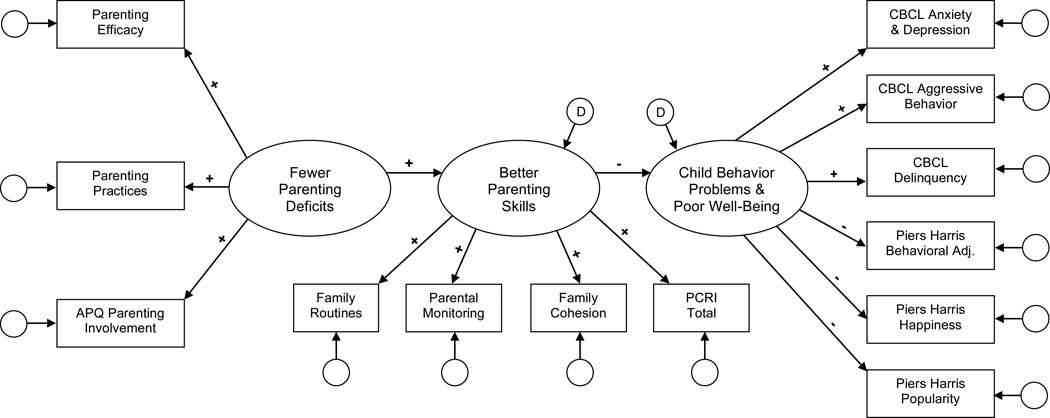
In this study, we examined a model (see Figure 1) of the relationships between parenting and child outcomes in a sample of MLH and their children. Specifically, we investigated whether MLH show significant parenting deficits, and if so whether the parenting deficits are related to poorer parenting skills. Finally, we considered child outcomes, to confirm our previous work that poorer parenting skills are associated with poorer child outcomes.
Figure 1.
Proposed covariance structural model of the effects of parental deficits and parenting skills on child outcomes.
Methods
The IMAGE project (Improving Mothers’ parenting Abilities, Growth, & Effectiveness) is an intervention designed to assist MLH with parenting and self-care skills in order to improve child and maternal outcomes. MLH (N = 62) with children aged 6 – 14 (M = 10.7, SD = 2.3) were recruited for study participation through HIV/AIDS service organizations in Los Angeles County. Families were assessed at baseline and at 3, 6, and 12-month follow-up interviews, and mothers were randomly assigned to the 4 session individualized IMAGE intervention or standard care. The baseline data were used for this analysis.
Participants
The average age of MLH was 38.5 years (SD = 8.2); 61% (n = 38) were Latina, 26% black (n = 16), 3% white (n = 2), and 10% multiracial/multi-ethnic (n = 6). About half (52%, n = 32) spoke Spanish exclusively or primarily, and 66% were born outside of the United States (61% [n = 38] were born in Mexico, Central America or South America). About one-third (32%, n = 20) were married, 36% were separated/divorced (n = 22), 5% widowed (n = 3) and 27% never married (n = 17). Over half (53%) had less than a high school education (n = 33), 13% had a high school diploma (n = 8), and 34% had attended college or vocational school (n = 21); 32% were currently employed. On average, MLH’s total monthly income was $1,677 (SD = $1,286). Almost half (45%, n = 28) of the study children were female.
Procedures
Recruitment sites displayed English and Spanish language flyers in waiting rooms, and staff distributed flyers to potentially eligible mothers at agencies serving HIV-positive patients. In addition, 18% of eligible MLH were recruited via an acquaintance-based sampling approach in which eligible study participants provided their potentially eligible acquaintances with a brief study description and staff contact information. Mothers who referred an eligible acquaintance were offered payment of $10. Inclusion criteria were that the mother was diagnosed HIV+, spoke English or Spanish, had a well child (i.e., not HIV positive) age 6 – 14 living with her, and provided informed consent/assent. A total of 132 women contacted study staff and expressed an interest in participating in the study; 71 met eligibility criteria (54%); 9 eligible families did not enroll in the study. Thus, 62 of 71 eligible families (87%) participated in this study.
Trained, bilingual interviewers obtained signed informed consent from the MLH and assent from the child prior to the interview, which was conducted in the mother’s home or other private location according to MLH preference. Mothers were paid $60 for completing the baseline interview which lasted approximately 90 minutes. Procedures were approved by UCLA’s Institutional Review Board. Study documents (including assessment instruments that were not available in Spanish) were professionally translated and back translated by a team of three translators at the Worldwide Translation Center (WTC) in San Diego, CA.
Measures
A deficit is defined as a lack or impairment in a functional capacity. Here the operational definition is basic parenting practices and perceived ability to conduct basic practices. Parenting deficits were assessed using the Parental Involvement subscale of the Alabama Parenting Questionnaire, the Parenting Practices Scale, & Parenting Efficacy. The first two scales assess whether the parent understands basic parenting skills (e.g., importance of play time and time together, appropriate tone of voice with child, involvement in child’s life, spending time with child other than watching television). Skills are defined as competency in performance of a task, such as setting up and implementing family routines or parental monitoring, and bonding with the child; these were assessed through the Family Routines Questionnaire, Parental Monitoring Scale, Cohesion subscale from the Family Functioning Scale, & the Parent-Child Relationship Inventory.
As noted by Darling and Steinberg (1993), poor parenting style (labeled “parenting deficits” in this paper) and parenting practices (labeled “parenting skills” in this paper) are closely related, however, there is an important distinction between these two constructs. Parenting style/deficits communicate a more general emotional attitude but are not goal-directed, whereas parenting practices/skills are defined by specific content and socialization goals. Parenting deficits primarily convey an overall unsupportive tone to how the parent interacts with her child, (for example, an item from the Parent Practices Scale includes, “how often do you tell your child about our own experience by saying something like, ‘I saw a pretty bird outside’” (see additional examples of specific items below). Conversely, parenting skills primarily elicit whether specific behaviors are performed, e.g., whether parents engage in specific family routines. While a few of the items could fall under either construct, most of the skill items elicit specific socialization goals, whereas most of the deficit items elicit more general parent-child styles of interaction.
Parenting deficit
Parenting practices
The Alabama Parenting Questionnaire (APQ) has been used to tap various aspects of parenting practices in families with school-aged children, and has been shown to distinguish between families with children who had disruptive behavior problems, and those without disruptive behavior problems (Frick, 1991; Shelton, Frick, & Wootton, 1996). MLH completed the 10 item APQ Involvement scale (e.g., “You play games or do other fun things with your child”); for this analysis (Cronbach’s alpha = .80). Higher scores indicate more maternal involvement.
In addition, selected items from the school-aged version of the Parent Practices Scale (Strayhorn & Weidman, 1988) were administered to MLH to assess favorable and unfavorable aspects of parental practices (e.g., “How often do you read to your child, or take turns with your child reading something aloud,” and “How often do you tell your child to do something, with an irritated or angry tone of voice”). The scale has been used in studies with children age 6 – 14, has shown good internal consistency and validity, and is significantly associated with measures of parental psychological and social health (McLaughlin & Harrison, 2006; Onyskiw & Hayduk, 2001). Higher scores indicate more positive parenting practices. Cronbach’s alpha for the sample was .73.
Parenting efficacy
A four item Parenting Efficacy scale, modeled after the HIV Self-Efficacy Questionnaire (Shively, Smith, Bormann, & Gifford, 2002) was used to assess MLH self-efficacy related to parenting abilities in establishing positive family routines and effectively monitoring their children’s behavior (“I can stay on top of where my child is when s/he is not home,” and “I can start new family routines as my children get older, or change old routines to fit new situations”). Response options ranged from 0 (I can’t do it) to 100 (completely confident I can do it). Cronbach’s alpha was .91 in this sample.
Parenting skill
Family routines
The Family Routines Questionnaire was administered to the mothers (e.g., “In our family, children go to bed at the same time each night;” “In our family, the whole family eats dinner together”). Higher scores equal more frequent involvement in each family routine. Cronbach’s alpha for the sample of MLH was .79.
Parental monitoring
Eleven items from the Parental Monitoring scale (Steinberg, Fletcher, & Darling, 1994; Steinberg, Lamborn, Dornbusch, & Darling, 1992) were administered to the MLH (e.g., “You know what your child does with his/her free time”). Higher scores indicate more parental monitoring. Cronbach’s alpha in this sample was .66.
Family cohesion
The Cohesion subscale from the Family Functioning Scale (Bloom & Naar, 1994) consists of five items. MLH rate the degree to which specific family characteristics were like her family on a four-point scale, with higher scores indicating a more cohesive family style (e.g., “people in my family really help and support one another”). In this sample, Cronbach’s alpha was .71.
Parent-child relationship
The Parent-Child Relationship Inventory assesses parental attitudes toward parenting and toward the child. The scale was standardized on an urban sample of more than 1,100 parents in the U.S; internal consistency of subscales shows no values below .70, and a median value of .82 (Gerard, 1994). For this analysis, subscales of quality of communication (e.g., “My child would say I am a good listener”) and parental support (“I sometimes feel overburdened by my responsibilities as a parent”) were summed for a total parental communication and support score, with a Cronbach’s alpha of .72. Higher scores indicate a more positive parent-child relationship.
Child outcomes
Behavior problems
The Child Behavior Checklist (CBCL) was administered to the MLH. The CBCL has standardized competence items that discriminate significantly between children who are adapting successfully versus children needing help for behavioral or emotional problems (Achenbach, 1991; Achenbach & Edelbrock, 1979). Subscales used in this analysis were Anxious/Depressed, Aggressive Behavior, and Delinquent Behavior. Cronbach’s alphas for this sample were .83, .90 and .71, respectively.
Self concept
The Piers-Harris Children’s Self-Concept Scale was administered to the children. It is a widely employed measure designed for use with children and adolescents, and has been found to be a psychometrically sound instrument (Hughes, 1984; Piers, 1993). The three subscales used in this analysis were the popularity scale, which assessed social functioning and perceived popularity (e.g., “I feel left out of things;” alpha = .66); the happiness and satisfaction scale, which assessed general feelings of happiness and satisfaction with life (e.g., “I am a happy person;” alpha = .70); and the behavioral adjustment scale, which assesses problematic behaviors in home and school settings (e.g., “I get into a lot of fights;” alpha = .68).
Analysis
Prior to evaluating the proposed model, descriptive statistics are presented, outlining the percent of MLH in the sample who had elevated parenting deficits. Covariance structural modeling is next performed using EQS (Bentler, 2006) with a maximum likelihood approach, with indirect effects suggestive of mediation also evaluated using a Sobel test extension. Although our sample size is small, we chose covariance structural modeling as the main analysis approach as it addresses our latent variables and their relationships from sets of observed variables, allowing for a broad assessment of model components and subsequent fit (issues of power for our model are noted in the Discussion). Using the variable groupings noted above, three constructs were formed consisting of parenting deficits, parenting skills, and child behavior and well-being outcomes (see Figure 1).
Results
Means, standard deviations, variances, covariances, and correlations of the measured variables are noted in Table 1. Although the general distributions of our analysis variables were normal, a majority of our sample mothers evidenced some type of parenting deficiencies (i.e., parenting deficits or parenting skills) across at least one of the analysis variables. For example, over 70% of the mothers scored below the sample mean on any of the deficit measures, and over 46% scored at or below the 25th percentile on any of the deficit measures. For parenting skills, 80.6% of the mothers scored below the sample mean on any of the parenting skills measures (with 58.1% scoring at or below the 25th percentile).
Table 1.
Covariance Matrix, Means and Standard Deviations for Measured Variables
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (12) | (13) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parenting Deficits | |||||||||||||
| (1) APQ Involvement | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (2) Parenting Practices | 46.99 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (3) Parenting Efficacy | 175.83 | 161.07 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Parenting Skills | |||||||||||||
| (4) Routines | 30.08 | 70.01 | 91.72 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (5) Monitoring | 9.58 | 16.25 | 29.47 | 15.24 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| (6) Family Cohesion | 8.46 | 9.43 | 76.98 | 10.15 | 2.39 | -- | -- | -- | -- | -- | -- | -- | -- |
| (7) PCRI Total | 16.21 | 35.71 | 179.97 | 24.39 | 6.95 | 8.1 | -- | -- | -- | -- | -- | -- | -- |
| Child Behavior Outcomes | |||||||||||||
| (8) CBCL Anxiety/Depression | −6.04 | −0.47 | −80.42 | −8.17 | −2.02 | −2.41 | −3.66 | -- | -- | -- | -- | -- | -- |
| (9) CBCL Aggressive Behavior | −8.00 | −0.81 | −86.35 | −15.62 | −2.80 | −2.67 | −4.34 | 22.66 | -- | -- | -- | -- | -- |
| (10) CBCL Delinquency | −5.22 | −1.68 | −26.08 | −6.53 | −3.57 | −1.38 | −1.81 | 4.09 | 9.15 | -- | -- | -- | -- |
| (11) Piers Harris Behavioral Adjustment | 0.06 | −5.37 | 5.18 | −1.79 | −0.48 | 0.48 | −0.09 | −2.71 | −3.52 | −1.71 | -- | -- | -- |
| (12) Piers Harris Popularity | 0.99 | −3.16 | −12.79 | −0.74 | −1.56 | 0.72 | 2.18 | −4.06 | −5.43 | −0.17 | 1.63 | -- | -- |
| (13) Piers Harris Happiness | −1.09 | −2.33 | −12.95 | −1.43 | −0.38 | 0.31 | 0.67 | −2.47 | −3.68 | −0.26 | 1.71 | 2.49 | -- |
| M | 40.05 | 51.89 | 349.45 | 59.35 | 52.34 | 17 | 52.06 | 5.05 | 8.66 | 2.1 | 14.05 | 8.19 | 8.82 |
| SD | 6.56 | 12.22 | 68.9 | 8.97 | 3.18 | 2.56 | 6.16 | 4.36 | 6.9 | 2.43 | 2.01 | 2.27 | 1.66 |
Looking more closely at the APQ for evidence of parenting deficits, 39% of mothers reported they “never” engaged in one or more of the positive parenting practices (such as having a friendly talk with their child), and 21% reported “always” engaging in at least one negative parenting practice (such as losing track of their child). On the PPQ (associated with parenting deficits), 52% “never” engaged in one or more positive parenting practice (such as playing together with their child). On the six items on the PCRI indicative of lack of support (such as feeling alone or stressed), 77% reported they “strongly agree” with at least one item, and 32% reported they “strongly agree” with at least half the items.
Regarding parenting skills, many of the MLH in this study seem to be lacking even the most basic set of abilities. For example, in investigating specific items on the Parent Practices Scale, “active listening” was used frequently by only 15%, and less than once a week by 19%; only approximately one-third of the MLH were enthusiastic about answering child questions (and of those, they were only enthusiastic less than half the time). This may be because they don’t interact enough directly the child, as 50% of the MLH reported spending half or more of the total time they spend with the child in a room with the television on—and 23% said they spend all of their time with their child in a room with the TV on.
Covariance Structural Model
To formally test our hypothesized model (see Figure 1), covariance structural modeling was utilized. One measured variable from each construct was set at 1.0 for identification purposes. All other measured variable paths were allowed to be estimated. The variance term for the exogenous construct was estimated as were the disturbance terms for the two endogenous constructs. Model fit was evaluated using multiple fit indices, including the comparative fit index (CFI), the incremental fit index (IFI), and the root mean square error of approximation (RMSEA). Values closer to 1.0 for the CFI and IFI indicate better fit, with desired values above .90 or .95. For RMSEA, smaller values indicate better fit, with good fit ranging from 0 to .10 (typical cutoffs are .05, .08, and .10 - values greater that .10 indicate poor fit; see Loehlin, 2004).
The initial model resulted in a χ2 value of 154.94 (df = 63), with a CFI of .70, an IFI of .71, and RMSEA of 0.155, all indicative of poor model fit. To improve fit, a number of model modifications were made. First, two within construct covariances were added (see Byrne & Baron, 1993; see also Tanaka & Huba, 1984), focusing on the Piers Harris subscales. Second, four specific variance paths were added to account for variance unaccounted for in a measured variable by its assigned construct (Bentler, 1990; Hoyle & Smith, 1994). Though not part of the shared variation within the assigned construct, the remaining nonrandom variance from these measured variables can directly affect other variables/outcomes. The specific paths added include a path from parenting practices to family routines (where remaining nonrandom variation from parenting practices is affiliated with the routines families adopt), a path from parenting efficacy to the parent-child relationship measure (where nonrandom variation regarding parenting efficacy affects how well the mother/child get along), and a path from parental monitoring to both the CBCL delinquency measure and the Piers Harris popularity subscale (where the remaining variation from parental monitoring may be seen as directly affecting delinquent acts, and popularity with friends and inclusion in activities).
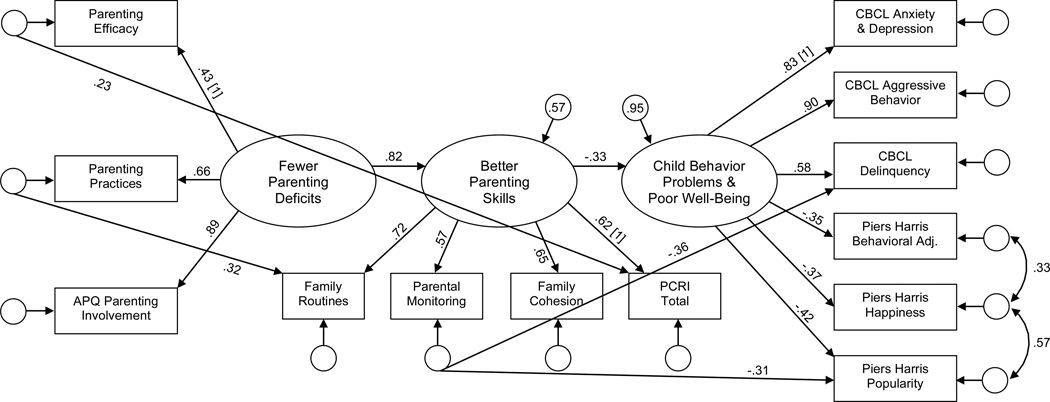
The revised model (see Figure 2) showed improved fit, with a χ2 = 85.88 (df = 57), CFI = .91, IFI = .91, and RMSEA = .091. All estimated parameters were significant at the .05 or better level. Overall, the latent construct reflecting fewer parenting deficits was positively associated with better parenting skills, which in turn was found to be negatively associated with poor child behavior outcomes (i.e., better parenting skills reduced problematic child behaviors). In essence, fewer parenting deficits were associated with better parenting skills, and better parenting skills were associated with better child behavior and well-being.
Figure 2.
Final covariance structural model with standardized parameter estimates.
Note: Paths with “[1]” indicate values fixed at 1 for identification purposes.
An evaluation of the indirect association between the parenting deficits construct and the endogenous outcome of child behaviors was made using a Sobel-test extension (Bentler, 2006). The latent construct reflecting fewer parenting deficits was found to have an indirect association with child behaviors (standardized indirect effect [SIE] = −.27, p < .05). Along with the direct effect that fewer parenting deficits were associated with better parenting skills, the indirect effect suggests that fewer parenting deficits also led to fewer child behavior problems and better well-being.
Discussion
The purpose of this preliminary study was to further investigate whether: (1) MLH exhibit parenting deficits, and if so to describe those deficits in more detail than previous studies; (2) determine if the deficits are, in fact, associated with poorer parenting skills; and (3) to confirm previous studies that poorer parenting skills are associated with poorer child outcomes. As previously noted, a majority of our sample mothers evidenced some type of parenting deficiencies (i.e., parenting deficits or parenting skills) across at least one of the analysis variables.
Our findings also may be due, at least in part, to the fact MLH lack the confidence to implement basic parenting skills. In terms of self-efficacy, only 34% were completely confident in their ability to add and adapt new family routines as their child age or as new situations arise, and only 39% were completely confident they could make sure daily routines were indeed implemented on a regular basis. (Other variables that were not specifically investigated in this study may also play a part [e.g., attitudes towards parenting, competing demands, and normative beliefs.])
Physical limitations imposed by HIV also partially explain these findings. Over one-third (37%) report being too worn out to do something fun with their child more than half of the time (18% on all or most of the time). However, our experience teaching MLH parenting skills indicates in addition to the limitations they have parenting as a function of their illness, much of the parenting deficits result simply from lack of basic knowledge or practice of skills. They enjoy learning about developmental changes across childhood, communication techniques, and appropriate monitoring, and are motivated by the desire to have the best outcomes for their children.
Finally, in addition, these findings are not surprising given that these women had limited resources (53% have less than a high school education; more than two-thirds are unemployed). No classes are typically offered in parenting during middle school or high school to prepare and assist young women who will go on to become mothers and struggle with parenting issues. However, even MLH with higher levels of education struggle with parenting issues, due to a lack of preparation and the associated demands of dealing with their illness in this study, correlations showed no relationship between parenting deficits variables and mother's education (data not shown). In addition, MLH struggle with their disease, side effects from the treatment of their disease, issues of self-esteem as a mother, and with the impact of the disease on their energy for functioning as a parent.
There are a number of caveats to the current study that warrant mention. First, we offered evidence in the Results that some MLH in our sample lacked basic parenting skills, illustrating these findings with items from the Parenting Practices Scale. Unfortunately, normative data specific to this scale's individual items have not been reported in the literature, and thus we cannot be certain that our study means are below normative standards. However, there is evidence to suggest that populations similar in demographics to our sample of MLH generally report positive practices as measured by this scale. Calzada and Eyberg (2002) report that greater than 80% of Hispanic mothers use praise and affection at least several times per day, suggesting that these parent-child relationships are characterized by a high degree of warmth. In addition, higher levels of warm involvement overall, as measured by the scale, have been found to be associated with having children with lower levels of oppositional behaviors and impulsivity (Brannigan, Gemmell, Pevalin, & Wade, 2002; Stormshak et al., 2000).
Another caveat regards power of detecting effects given our study sample size. A power estimate for detecting ill-fit of our final model (i.e., power to reject a model based on RMSEA; see Loehlin, 2004; also see MacCallum, Browne, & Sugawara, 1996, for methodology) reveals an estimated power value of .60 assuming a RMSEA cutoff of .05 for very good fit, and a poor-fit cutoff set at .10. However, since the lower bound of good fit for RMSEA can be as low at .10 (see Loehlin for RMSEA cutoffs), using a .11 RMSEA as a poor-fit cutoff for power estimates yields a power value of .76 for our final model. While power was also limited due to our small sample, we included child outcomes to validate the model: more parenting deficits -> poorer parenting skills -> poorer child outcomes. In addition, we did limit the number of measured variables in the model, and the resulting parameter estimates and standard errors appeared appropriate. Given our small analysis size, generalization of results to other MLH populations should be done with caution. Further, these data are cross-sectional, and though our model suggests a sequential flow from deficits to skills to outcomes, longitudinal data if available would have provided a stronger and more generalizable assessment. Another caveat is that many of the outcome measures were based on maternal reports; it is possible that child reports of the various measures would yield a slightly different set of associations.
An additional limitation includes our reported indirect effect findings; though we were careful not to over interpret the indirect effects as evidence of complete or partial mediation (see James, Mulaik, & Brett, 2006), these effects should be interpreted with caution. Another caveat concerns the construct arrangement within our model; alternative models to the one we tested are possible and thus the current model should not be viewed as definitive. As with any covariance structural model, it is possible that unmeasured confounding variables may have influenced our overall findings. Future research should consider adding additional variables to the latent constructs to temper such concerns. And finally, external validity may be an issue. This was a small pilot study conducted with a sample of MLH in Los Angeles County, and while many of the family issues would appear generalizable, cultural and regional differences may limit this.
What has been missing in the literature on the impact of maternal HIV on child outcomes is detailed study aimed at identification of mothers’ parenting deficits, and how they affect parenting skills and thus child outcomes. This study delineates further the parenting issues with which MLH struggle, providing information on the interventions needed in this population. We established direct links between parenting deficits and poorer parenting skills, which makes conceptual sense, but has received little investigation or documentation. MLH who have little confidence they can enact parenting skills, and who do not know basic parenting practices, are less likely to be able to provide family routines consistently, to monitor their children, or to engender family cohesion or a close parent-child relationship. All of these findings on parenting deficits indicate that parent skills training—including some basic parenting knowledge and self-efficacy training prior to skills training—could improve MLH parenting and thus positively impact child outcomes. Such training may even impact maternal health, as it could reduce parenting stress (e.g., Murphy, Marelich, Armistead, Herbeck, & Payne, 2010). Future intervention research should develop and/or adapt parenting interventions for MLH to improve both mother and child outcomes.
Acknowledgments
This research was supported by Grant Number 5R01MH086329 from the National Institute of Mental Health to the first author.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Edelbrock C. The Child Behavior Profile: II. Boys aged 12–16 and girls aged 6–11 and 12–16. Journal of Consulting and Clinical Psychology. 1979;47:223–233. doi: 10.1037//0022-006x.47.2.223. [DOI] [PubMed] [Google Scholar]
- Altschuler J, Dale B. On being an ill parent. Clinical Child Psychology and Psychiatry. 1999;4:23–37. [Google Scholar]
- Armistead L, Klein K, Forehand R. Parental physical illness and child functioning. Special Issue: The impact of the family on child adjustment and psychopathology. Clinical Psychology Review. 1995;15:409–422. [Google Scholar]
- Bauman LJ, Silver EJ, Draimin BH, Hudis J. Children of Mothers With HIV/AIDS: Unmet Needs for Mental Health Services. Pediatrics. 2007;120:e1141–e1147. doi: 10.1542/peds.2005-2680. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Latent variable structural models for separating specific from general effects. In: Sechrest L, Perrin E, Bunker J, editors. Research methodology: Strengthening causal interpretation of nonexperimental data. Rockville, MD: Department of Health and Human Services; 1990. pp. 61–83. [Google Scholar]
- Bentler PM. EQS 6 Structural equations modeling program manual. Encino, CA: Multivariate Software, Inc; 2006. [Google Scholar]
- Bloom BL, Naar S. Self-report measures of family functioning: Extensions of a factorial analysis. Family Process. 1994;33:203–216. doi: 10.1111/j.1545-5300.1994.00203.x. [DOI] [PubMed] [Google Scholar]
- Brannigan A, Gemmell W, Pevalin DJ, Wade TJ. Self-control and social control in childhood misconduct and aggression: The role of family structure, hyperactivity, and hostile parenting. Canadian Journal of Criminology. 2002;44:119–142. [Google Scholar]
- Byrne BM, Baron P. The Beck Depression Inventory: Testing and cross-validating a hierarchical factor structure for nonclinical adolescents. Measurement and Evaluation in Counseling and Development. 1993;26:164–178. [Google Scholar]
- Calzada EJ, Eyberg SM. Self-reported parenting practices in Dominican and Puerto Rican mothers of young children. Journal of Clinical Child & Adolescent Psychology. 2002;31:354–363. doi: 10.1207/S15374424JCCP3103_07. [DOI] [PubMed] [Google Scholar]
- Darling N, Steinberg L. Parenting style as context: An integrative model. Psychological Bulletin. 1993;113:487–496. [Google Scholar]
- Dorsey S, Klein K, Forehand R Family Health Project Research Group. Parenting self-efficacy of HIV-infected mothers: The role of social support. Journal of Marriage and Family. 1999;61:295–305. [Google Scholar]
- Esposito S, Musetti LE, Musetti MC, Tornaghi R, Corbella S, Massironi E, Marchisio P, Guareschi A, Principi N. Behavioral and psychosocial disorders in uninfected children age 6 to 11 years born to human immunodeficiency virus-seropositive mothers. Developmental and Behavioral Pediatrics. 1999;20:411–417. doi: 10.1097/00004703-199912000-00002. [DOI] [PubMed] [Google Scholar]
- Evans S, Shipton EA, Keenan T. The relationship between maternal chronic pain and child adjustment: The role of parenting as a mediator. The Journal of Pain. 2006;7:236–243. doi: 10.1016/j.jpain.2005.10.010. [DOI] [PubMed] [Google Scholar]
- Forehand R, Jones DJ, Kotchick BA, Armistead L, Morse E, Morse PS, Stock M. Noninfected children of HIV-infected mothers: A 4-year longitudinal study of child psychosocial adjustment and parenting. Behavior Therapy. 2002;33:579–600. [Google Scholar]
- Forehand R, Steele R, Armistead L, Morse E, Simon P, Clark L. The Family Health Project: Psychosocial adjustment of children whose mothers are HIV infected. Journal of Consulting and Clinical Psychology. 1998;66:513–520. doi: 10.1037//0022-006x.66.3.513. [DOI] [PubMed] [Google Scholar]
- Frick PJ. The Alabama Parenting Questionnaire. University of Alabama; 1991. Unpublished rating scale. [Google Scholar]
- Gerard AB. Parent-Child Relationship Inventory (PCRI) manual. Los Angeles: Western Psychological Services; 1994. [Google Scholar]
- Hough ES, Brumitt G, Templin T, Saltz E, Mood D. A model of mother-child coping and adjustment to HIV. Social Science & Medicine. 2003;56:643–655. doi: 10.1016/s0277-9536(02)00061-8. [DOI] [PubMed] [Google Scholar]
- Hoyle RH, Smith GT. Formulating clinical research hypotheses as structural equation models: A conceptual overview. Journal of Consulting and Clinical Psychology. 1994;62:429–440. doi: 10.1037//0022-006x.62.3.429. [DOI] [PubMed] [Google Scholar]
- Hughes HM. Measures of self-concept and self-esteem for children ages 3 – 12 years: A review and recommendations. Clinical Psychology Review. 1984;4:657–692. [Google Scholar]
- James LR, Mulaik SA, Brett JM. A tale of two methods. Organizational Research Methods. 2006;9:233–244. [Google Scholar]
- Kotchick BA, Forehand R, Brody G, Armistead L, Simon P, Morse E, Clark L. The impact of maternal HIV-infection on parenting in inner-city African American families. Journal of Family Psychology. 1997;11:447–461. [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural equation modeling. 4th ed. Mahwah, NJ: Erlbaum; 2004. [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structural modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- McLaughlin DP, Harrison CA. Parenting practices of mothers of children with ADHD: The role of maternal and child factors. Child and Adolescent Mental Health. 2006;11:82–88. doi: 10.1111/j.1475-3588.2005.00382.x. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Armistead L, Marelich WD, Payne DL, Herbeck DM. Pilot trial of a disclosure intervention for HIV+ mothers: The TRACK program. Journal of Consulting and Clinical Psychology. 2011;79:203–214. doi: 10.1037/a0022896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Greenwell L, Mouttapa M, Brecht ML, Schuster MA. Physical health of mothers with HIV/AIDS and the mental health of their children. Journal of Developmental and Behavioral Pediatrics. 2006;27:386–395. doi: 10.1097/00004703-200610000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD. Resiliency in young children whose mothers are living with HIV/AIDS. AIDS Care. 2008;20:284–291. doi: 10.1080/09540120701660312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Amaro H. Maternal HIV/AIDS and adolescent depression: A covariance structure analysis of the “Parents and children Coping Together” (PACT) model. Vulnerable Children and Youth Studies. 2009;4:67–82. doi: 10.1080/17450120802385729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Armistead L, Herbeck DM, Payne DL. Anxiety/Stress among mothers living with HIV: Effects on parenting skills & child outcomes. AIDS Care. 2010;22:1449–1458. doi: 10.1080/09540121.2010.487085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Graham J, Payne DL. Children affected by maternal HIV/AIDS: Feasibility and acceptability trial of the Children United with Buddies (CUB) intervention. Clinical Child Psychology and Psychiatry. doi: 10.1177/1359104513499357. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Herbeck DM. Impact of maternal HIV health: A 12-year study of children in the parents and children coping together project. Journal of Adolescent Health. 2012;51:313–318. doi: 10.1016/j.jadohealth.2011.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Herbeck DM, Payne DL. Family routines and parental monitoring as protective factors among early/middle adolescents affected by maternal HIV/AIDS. Child Development. 2009;80:1676–1691. doi: 10.1111/j.1467-8624.2009.01361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Hoffman D. A longitudinal study of the impact on young children of maternal HIV serostatus disclosure. Clinical Child Psychology and Psychiatry. 2002;7:55–70. [Google Scholar]
- Murphy DA, Marelich WD, Hoffman DA, Schuster MA. Parental HIV/AIDS: An empirical model of the impact on children in the United States. In: Crane DR, Marshall ES, editors. Handbook of families and health: Interdisciplinary perspectives. Thousand Oaks, CA: Sage; 2006. pp. 178–194. [Google Scholar]
- Onyskiw JE, Hayduk LA. Process underlying children’s adjustment in families characterized by physical aggression. Family Relations. 2001;50:376–385. [Google Scholar]
- Piers EV. Piers-Harris Children’s Self-Concept Scale: Revised Manual 1984. Los Angeles: Western Psychological Services; 1993. [Google Scholar]
- Reyland SA, McMahon TJ, Higgins-Delessandro A, Luthar SS. Inner-city children living with an HIV-Seropositive mother: Parent-child relationships, perception of social support, and psychological disturbance. Journal of Child & Family Studies. 2002;11:313–329. [Google Scholar]
- Romer G, Barkmann C, Schulte-Markwort M, Thomalla G, Riedesser P. Children of somatically ill parents: A methodological review. Clinical Child Psychology & Psychiatry. 2002;7:17–38. [Google Scholar]
- Russell KS, Rauch PK. Parenting with cancer I: Developmental perspective, communication, and coping. Advances in Experimental Medicine and Biology. 2012;732:131–140. doi: 10.1007/978-94-007-2492-1_10. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25:317–329. [Google Scholar]
- Shively M, Smith TL, Bormann J, Gifford AL. Evaluating self-efficacy for HIV disease management skills. AIDS and Behavior. 2002;6:371–379. [Google Scholar]
- Steinberg L, Fletcher A, Darling N. Parental monitoring and peer influences on adolescent substance use. Pediatrics. 1994;93:1060–1064. [PubMed] [Google Scholar]
- Steinberg L, Lamborn SD, Dornbusch SM, Darling N. Impact of parenting practices on adolescent achievement: Authoritative parenting, school involvement, and encouragement to succeed. Child Development. 1992;63:1266–1281. doi: 10.1111/j.1467-8624.1992.tb01694.x. [DOI] [PubMed] [Google Scholar]
- Stormshak EA, Bierman KL, McMahon RJ, Lengua LJ. Parenting practices and child disruptive behavior problems in early elementary school. Journal of Clinical Child Psychology. 2000;29:17–29. doi: 10.1207/S15374424jccp2901_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strayhorn J, Weidman C. A parent practices scale and its relation to parent and child mental health. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:613–618. doi: 10.1097/00004583-198809000-00016. [DOI] [PubMed] [Google Scholar]
- Tanaka JS, Huba GJ. Confirmatory hierarchical factor analyses of psychological distress measures. Journal of Personality and Social Psychology. 1984;46:621–635. [Google Scholar]