Abstract
There are relatively few population-based studies on prescription drug use during pregnancy. Hawai‘i Pregnancy Risk Assessment Monitoring System (PRAMS) survey data from 4,735 respondents were used to estimate statewide prevalence of overall non-vitamin prescription drug use during and in the month before pregnancy. Data were weighted to be representative of all pregnancies resulting in live births in Hawai‘i in 2009–2011. Of women with recent live births in Hawai‘i, 14.2% (95% CI: 13.0 – 15.5) reported prescription drug use before pregnancy and 17.6% (95% CI: 16.2 – 19.0) reported prescription drug use during pregnancy. Prevalence of prescription drug use both before and during pregnancy was highest among women who had a pre-pregnancy chronic disease, were White, and had a pregnancy-related medical problem. Pain relievers (2.82%; 95% CI: 2.28 – 3.47), psychiatric medications (2.34%; 95% CI: 1.85 – 2.95), and anti-infectives (1.91%; 95% CI: 1.46 – 2.48) were the most common types of medications used before pregnancy. The most commonly-reported prescription medication types taken during pregnancy were anti-infectives (4.00%; 95% CI: 3.34 – 4.79), pain relievers (3.18%; 95% CI: 2.56 – 3.94), and gastrointestinal drugs (3.08%; 95% CI: 2.47 – 3.83). Of women who reported prescription drug use during pregnancy and attended prenatal care, 10.3% (95% CI: 8.0 – 13.2) reported that their healthcare provider had not counseled them during prenatal care on which medicines are safe to use during pregnancy.
Keywords: Prescription Drug Use, Pregnancy
Introduction
Despite the fact that some medications have documented teratogenic or otherwise harmful effects when used during pregnancy,1,2 prescription drug use among pregnant women is increasingly common.3,4 There are likely numerous factors that are influencing the increase in prescription drug use in pregnancy, with proposed explanations including rising prevalence of chronic disease in reproductive age populations,5 a greater number of pharmaceutical options for treating chronic diseases,5,6 and increasing maternal age at pregnancy.5,7 Although women with chronic diseases pre-pregnancy are more likely to report prescription drug use during pregnancy than women without chronic diseases, women without chronic diseases also report high usage of prescription medications during pregnancy.8 Another complicating factor is the fact that approximately half of all pregnancies in the United States are not intended.9 These unintended pregnancies often lead to accidental in utero exposures to prescription medication early in pregnancy, before the woman recognizes that she is pregnant.2,4,10
There are few population-based studies on prescription drug use during pregnancy.11 The research findings that do exist typically come from data sources with limited generalizability, such as electronic medical records,12 pharmacy dispensing records,13 or health insurance claims databases.11 This study aimed to use a population-based dataset to (1) determine the prevalence of non-vitamin prescription drug use before and during pregnancy in Hawai‘i, (2) identify the types of medications used during these time periods, and (3) describe differences in non-vitamin prescription drug use during and immediately before pregnancy in Hawai‘i by maternal demographic characteristics.
Methods
Data Source
A secondary analysis was conducted using Hawai‘i Pregnancy Risk Assessment Monitoring System (PRAMS) survey data from 2009 to 2011. The PRAMS survey collects self-reported information on maternal behaviors, attitudes, and experiences before, during, and immediately following pregnancy. PRAMS programs operate according to a standardized data collection protocol developed by the Centers for Disease Control and Prevention (CDC), consisting of a mailed questionnaire (self-administered) with telephone follow-up for non-responders. Mothers are selected for the Hawai‘i PRAMS survey using a stratified sample drawn from certificates of live birth in Hawai‘i, and complete the survey 3–8 months postpartum. The majority of participants complete the Hawai‘i PRAMS survey 3–4 months postpartum. The Hawai‘i PRAMS analytic dataset includes information collected from Hawai‘i PRAMS survey questions in addition to selected linked variables extracted from birth certificates. If PRAMS programs are able to achieve a minimum weighted response rate of 65% in each sampling stratum, survey results are considered generalizable to all live births in the state in a given year. Responses are then weighted according to CDC protocol to be representative of all pregnancies resulting in live births in Hawai‘i in a given year. Hawai‘i PRAMS weighted response rates for the years presented in this analysis ranged from 71%–73%. Additional information on PRAMS methodology can be found at: http://www.cdc.gov/prams/methodology.htm.
Data were available for 4,735 respondents, representing a weighted population of approximately 55,690 women with live births. Secondary analysis of Hawai‘i PRAMS data is covered under pre-existing approvals granted by the Institutional Review Board of the Human Research Protection Office of the CDC, as well as by the Hawai‘i State Department of Health Institutional Review Board.
Measures
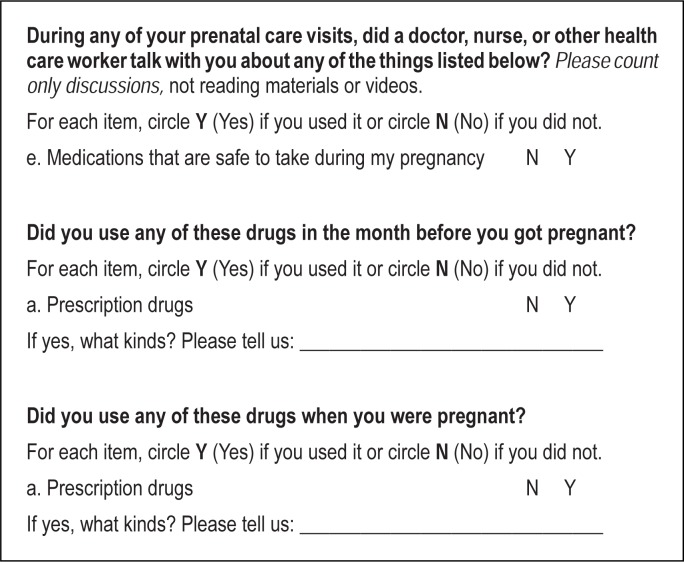
The following questions pertaining to prescription drug use were used for this analysis:
Write-in responses were manually reviewed in order to properly adjust for misspellings, multiple drugs listed, and other factors. Responses were then coded into groups by medical indication using SAS 9.2 (SAS Institute Inc., Cary, NC) “string” and “upcase” commands. Medications with possible indications in multiple groups were cross-checked with maternal and/or birth certificate report of diagnoses to determine most likely group for categorization. An example of this would be the drug lamotrigine, which may be prescribed for psychiatric conditions,14 or for non-psychiatric seizure disorders.15 In this situation, the medication use was cross-checked with maternal report of medical conditions in order to determine the most likely categorization. Write-in entries that were larger than thirty characters were listed in separate comment file; these responses were also manually reviewed and coded into groups by unique ID number. In a very few cases, determination of which drug was being referenced was not possible. For each time period examined, there were fewer than five unweighted cases in which a drug listed was not reliably identified due to spelling errors, fewer than ten unweighted cases in which a respondent did not remember or state what type of medication was used, and/or did not provide additional information that could aid in drug identification, and fewer than twenty unweighted cases in which a participant selected “Yes” for prescription drug use, but then left the write-in box blank and did not provide additional information that could aid in drug identification. In cases where classifying an entry was not possible, it was coded as “Unknown”. Coding accuracy was verified on an ongoing basis throughout the analysis by manual review of SAS and SUDAAN outputs listing responses included and not included in each grouping.
Maternal age, race/ethnicity, nativity, education, and parity were determined based on linked birth certificate variables included in the Hawai‘i PRAMS analytic dataset. Approximately 23% of the population of Hawai‘i identifies as mixed race,16 however the maternal race/ethnicity variables included in the Hawai‘i PRAMS analytic dataset were sorted into single race groups based on a standard algorithm used by the Hawai‘i Department of Health Office of Health Status and Monitoring prior to their inclusion in the dataset.17 Federal Poverty Level (FPL) was based on maternal reports of household annual income and number of dependents in the year before delivery and was calculated according to Hawai‘i-specific threshold guidelines.18–21 Prenatal counseling regarding medication safety, pre-pregnancy chronic disease, and pregnancy-related medical problems were based on maternal reports in the Hawai‘i PRAMS survey. The created variable for pre-pregnancy chronic disease included the following conditions, as reported in the Hawai‘i PRAMS survey only: Type 1 or Type 2 diabetes at any point before pregnancy; and asthma, hypertension, heart problems, epilepsy, thyroid problems, depression, and anxiety in the three months before pregnancy. The created variable for pregnancy-related medical problems included the following conditions, as reported in the Hawai‘i PRAMS survey: gestational diabetes, vaginal bleeding, kidney or bladder infection, severe nausea, vomiting or dehydration, cervical cerclage, hypertension, preeclampsia, toxemia during pregnancy, placental problems, preterm labor, or blood transfusion during pregnancy. SAS-callable SUDAAN 10.0 (RTI International, Research Triangle Park, NC) was used to generate prevalence estimates, confidence intervals, and P-values.
Results
Maternal demographic characteristics and prescription drug use before and during pregnancy are shown in Table 1. Of women with recent live births in Hawai‘i, 14.2% (95% CI: 13.0 – 15.5) reported non-vitamin prescription use (NVPU) immediately before pregnancy and 17.6% (95% CI: 16.2 – 19.0) reported NVPU during pregnancy. Women who had a pre-pregnancy chronic disease had the highest prevalence of NVPU both before (37.7%) and during (36.1%) pregnancy. By race-ethnicity, White women reported the highest prevalence of NVPU (22.9% before and 26.2% during pregnancy). Also, women who had a pregnancy-related medical problem were more likely to report NVPU both before (18.6%) and during (24.5%) pregnancy. Differences by demographic variables listed in Table 1 were statistically significant at the P < .001 level, with the exception of differences in use during pregnancy by maternal age (P = .002) and differences by parity, both before pregnancy (P = .891) and during pregnancy (P = .869).
Table 1.
Non-vitamin prescription use (NVPU) by maternal characteristics, Hawai‘i PRAMS, 2009–2011
| Percent of total birth population* (95% CI) | Percent reporting NVPU before pregnancy* (95% CI) | Percent reporting NVPU duringpregnancy* (95% CI) | |
| Total | 100 (N/A) | 14.2 (13.0 – 15.5) | 17.6 (16.2 – 19.0) |
| Age (years) | |||
| Less than 20 | 7.3 (6.4 – 8.3) | 7.1 (4.5 – 11.0) | 10.3 (6.9 – 15.2) |
| 20–24 | 23.6 (22.1 – 25.3) | 10.9 (8.7 – 13.4) | 16.1 (13.4 – 19.3) |
| 25–29 | 27.3 (25.7 – 29.0) | 15.5 (13.1 – 18.2) | 17.3 (14.8 – 20.1) |
| 30–34 | 24.4 (22.9 – 26.0) | 15.7 (13.3 – 18.5) | 18.6 (15.9 – 21.7) |
| 35 or older | 17.4 (16.1 – 18.8) | 17.5 (14.5 – 20.9) | 21.5 (18.2 – 25.2) |
| Race/Ethnicity | |||
| Hawaiiana | 30.1 (28.4 – 31.7) | 13.2 (11.2 – 15.5) | 15.3 (13.1 – 17.8) |
| White | 23.0 (21.5 – 24.6) | 22.9 (19.8 – 26.4) | 26.2 (23.0 – 29.8) |
| Filipino | 17.8 (16.5 – 19.3) | 12.3 (9.8 – 15.4) | 16.1 (13.1 – 19.6) |
| Japanese | 9.3 (8.3 – 10.5) | 12.0 (8.8 – 16.3) | 14.8 (11.2 – 19.4) |
| Other Pacific Islanderb | 7.4 (6.4 – 8.5) | 3.1 (1.6 – 5.9) | 5.7 (3.2 – 10.1) |
| Other Asianc | 7.2 (6.3 – 8.3) | 10.2 (6.7 – 15.1) | 15.9 (11.5 – 21.6) |
| Other or unknownd | 5.2 (4.4 – 6.1) | 12.7 (8.4 – 18.8) | 21.6 (15.5 – 29.3) |
| Nativity | |||
| Born in United States | 74.8 (73.1 – 76.4) | 16.5 (15.0 – 18.1) | 19.9 (18.3 – 21.7) |
| Born outside United States | 25.2 (23.7 – 26.9) | 7.3 (5.6 – 9.4) | 10.6 (8.5 – 13.2) |
| Education Level | |||
| Less than high school | 7.5 (6.6 – 8.5) | 6.3 (4.0 – 10.0) | 7.4 (4.7 – 11.3) |
| High school graduate | 39.7 (37.9 – 41.5) | 12.8 (11.0 – 14.9) | 15.5 (13.5 – 17.8) |
| 1–3 years of college | 23.5 (22.0 – 25.1) | 15.5 (13.0 – 18.4) | 21.4 (18.4 – 24.7) |
| 4 or more years of college | 29.3 (27.7 – 31.0) | 17.4 (15.0 – 20.1) | 20.3 (17.7 – 23.2) |
| Federal Poverty Level (%) | |||
| 100% or less | 29.3 (27.6 – 31.0) | 10.9 (9.1 – 13.1) | 11.5 (9.6 – 13.8) |
| 101% – 200% | 26.0 (24.4 – 27.7) | 13.0 (10.7 – 15.7) | 17.9 (15.1 – 21.1) |
| 201% or greater | 44.7 (42.8 – 46.6) | 17.9 (15.8 – 20.1) | 21.8 (19.5 – 24.3) |
| Parity | |||
| Primipara | 40.6 (38.8 – 42.4) | 14.1 (12.3 – 16.1) | 17.7 (15.6 – 20.0) |
| Multipara | 59.4 (57.6 – 61.2) | 14.2 (12.7 – 16.0) | 17.5 (15.7 – 19.4) |
| Pre-pregnancy Chronic Diseasee | |||
| Yes | 19.7 (18.3 – 21.1) | 37.7 (34.0 – 41.7) | 36.1 (32.4 – 40.1) |
| No | 80.3 (78.9 – 81.7) | 8.4 (7.4 – 9.6) | 13.0 (11.7 – 14.5) |
| Pregnancy-related Medical Problemf | |||
| Yes | 52.8 (50.9 – 54.6) | 18.6 (16.8 – 20.6) | 24.5 (22.4 – 26.7) |
| No | 47.2 (45.4 – 49.1) | 9.2 (7.8 – 10.9) | 9.8 (8.3 – 11.6) |
Weighted estimates;
Hawaiian includes part Hawaiian;
Other Pacific Islander includes: Samoan, Guamanian, and other Pacific Islander;
Other Asian includes: Chinese, Korean, Vietnamese, Asian Indian, and other Asian;
Other or unknown includes: African American, American Indian, Puerto Rican, Cuban, Mexican, and all others;
Pre-pregnancy chronic disease includes: diabetes, asthma, hypertension, heart problems, epilepsy, thyroid problems, depression, and anxiety;
Pregnancy-related medical problem includes: gestational diabetes, vaginal bleeding, kidney or bladder infection, severe nausea, vomiting, or dehydration, cervical cerclage, hypertension, preeclampsia, or toxemia during pregnancy, placental problems, preterm labor, and blood transfusion during pregnancy.
Differences by demographic variables listed in this table were statistically significant at the P < .001 level, with the exception of differences in use during pregnancy by maternal age (P = .002) and differences by parity, both before pregnancy (P = .891) and during pregnancy (P = .869).
Types of prescription drugs used before and during pregnancy are shown in Table 2. Pain relievers (2.82%; 95% CI: 2.28 – 3.47), psychiatric medications (2.34%; 95% CI: 1.85 – 2.95), and anti-infectives (1.91%; 95% CI: 1.46 – 2.48) were the most common types of medications used before pregnancy. The most commonly-reported prescription medication types taken during pregnancy were anti-infectives (4.00%; 95% CI: 3.34 – 4.79), pain relievers (3.18%; 95% CI: 2.56 – 3.94), and gastrointestinal drugs (3.08%; 95% CI: 2.47 – 3.83). Overall, 13.9% (95% CI: 12.7 – 15.2) of women reported not being counseled about medication safety during prenatal care. This estimate was lower among women who reported NVPU during pregnancy, with 10.3% (95% CI: 8.0 – 13.2) reporting that their healthcare provider had not counseled them during prenatal care on which medicines are safe to use during pregnancy. This difference was statistically significant at P = .004 (data not shown). Approximately 1% of women reported that they did not attend prenatal care (0.98%; 95% CI: 0.68 – 1.42). These women were not included in the analysis of medication safety counseling during prenatal care, but were included in the other analyses.
Table 2.
Prescription drug use before and during pregnancy by type, Hawai‘i PRAMS, 2009–2011
| Prescription Type | Percent reporting use before pregnancy* (95% CI) | Percent reporting use during pregnancy* (95% CI) |
| Allergy medications | 1.52 (1.12 – 2.07) | 1.71 (1.28 – 2.28) |
| Anti-infectivesa | 1.91 (1.46 – 2.48) | 4.00 (3.34 – 4.79) |
| Asthma medications | 1.40 (1.05 – 1.86) | 1.44 (1.07 – 1.93) |
| Birth control medications | 0.80 (0.53 – 1.20) | N/Ab |
| Cardiovascular medications | 1.42 (1.05 – 1.92) | 1.69 (1.29 – 2.21) |
| Diabetes medications | 0.83 (0.56 – 1.22) | 1.39 (1.02 – 1.89) |
| Fertility treatment medications | 0.81 (0.56 – 1.18) | N/A |
| Gastrointestinal medications | 0.88 (0.58 – 1.33) | 3.08 (2.47 – 3.83) |
| Other medicationsb | 1.27 (0.92 – 1.74) | 1.28 (0.92 – 1.76) |
| Pain relievers | 2.82 (2.28 – 3.47) | 3.18 (2.56 – 3.94) |
| Pregnancy support medications | N/A | 0.74 (0.50 – 1.10) |
| Psychiatric medicationsc | 2.34 (1.85 – 2.95) | 1.38 (1.01 – 1.87) |
| Thyroid medications | 0.86 (0.61 – 1.22) | 1.02 (0.74 – 1.41) |
| Unknown medications | 0.34 (0.20 – 0.58) | 0.66 (0.41 – 1.05) |
| Vitamins/supplementsd | 1.88 (1.42 – 2.47) | 6.81 (5.94 – 7.81) |
Weighted estimates;
Anti-infectives group includes: antibiotic, antiviral, antifungal, and antiparasitic medications;
bOther group includes all identifiable medications not otherwise grouped; for drugs taken during pregnancy, Other group also includes birth control;
Psychiatric group includes antidepressant, antianxiety, and antipsychotic medications, as well as medications used to treat attention deficit disorder and attention deficit hyperactivity disorder;
Vitamins/supplements group estimates include nonspecific responses indicating vitamin/supplement use (eg, prenatal vitamins) as well as specific references to individual supplements (eg, iron pills) and reflect only responses to the prescription drug use before and during pregnancy questions on the Hawai‘i PRAMS survey, not responses to other survey questions specifically addressing prenatal or multivitamin use.
Discussion
To the knowledge of the authors, this study is the first examining prescription drug use before and during pregnancy using maternally reported, population-based data from the Hawai‘i PRAMS survey. This data source provides a different perspective from other research findings relying on data from electronic medical records, pharmacy dispensing records, or health insurance claims databases. Data from those sources do not directly address what is arguably the most important question with regards to this line of research: what prescription drugs did women use? Instead, these data sources use proxy measures such as: what drugs were women prescribed, what prescriptions were filled, and what prescriptions were submitted for insurance coverage. However, many people are prescribed medication that they never fill, fill medication that they never use, or use medication that they never submit for insurance coverage.22–25 Also, none of these data sources address the usage of prescription medication not prescribed to the woman herself. This means that any use of medications provided by friends, family, or other means would not be captured. This is of concern because sharing and borrowing of prescription medication is exceedingly common among American women of reproductive age, with recent estimates indicating that more than one in four have shared or borrowed prescription drugs.26,27
Limitations of this study related to the Hawai‘i PRAMS survey itself include that the data are self-reported, and consequently subject to bias due to recall or reporting factors. This could affect the results of this study, as previous research has shown that women are more likely to recall use of some types of medications than others when retrospectively asked about medication use during pregnancy.28 Reporting of medication use on the PRAMS survey might also have been affected by individual-level factors related to patient compliance or noncompliance with medical recommendations, possibly resulting in underreporting, overreporting, or misclassification of prescription drug usage.23,29–31 Additionally, PRAMS nonresponse weights are calculated based on assumptions that women in a particular subgroup who responded would be predicted to have similar responses to those who did not respond. It is unclear how valid this assumption may be for the outcomes examined in this study.32
There are also limitations related to the Hawai‘i PRAMS prescription drug use questions in particular. Issues with comprehension of these specific questions might have posed problems for some individual respondents. For example, some medications listed as responses were likely not prescribed, and may have in fact been over-the-counter medications. However, because many drugs are available both over the counter and by prescription (eg, ibuprofen), no attempt was made to exclude responses that may have been over the counter. This could mean that estimates for certain indication groups might include use of over the counter drugs, in addition to prescription drugs. The Hawai‘i PRAMS survey questions related to prescription drug use also did not have information on drug dosages, frequency of use, or pregnancy trimester of usage, all of which have important implications related to the effects of specific drugs on pregnancy and birth outcomes.
Conclusion
As prescription drug use among the general public becomes more widespread, there is an increased need for careful monitoring by health care providers of usage in pregnant and reproductive-aged women. The finding that 10.3% of women who report using prescription medication during pregnancy also reported not receiving counseling on medication safety during prenatal care is especially concerning for this reason. Counseling on potential risks to mother and fetus should be emphasized during prenatal care visits to assure that women are informed and empowered to make the best decisions for themselves and their infants.
Acknowledgements
The researchers would like to thank all of the women who have responded to the Hawai‘i PRAMS survey since the program began as a pilot project in 1999. Without their willingness to share information about their experiences before, during, and after pregnancy, this research would not be possible. Additionally, Tonya Lowery St. John and Ranjani Starr of the Hawai‘i State Department of Health, and Indu Ahluwalia of the Centers for Disease Control and Prevention provided valuable review and comment on an early version of this manuscript. The researchers would also like to acknowledge the Hawai‘i State Department of Health, and specifically the Family Health Services Division and Maternal and Child Health Branch, for supporting the Hawai‘i PRAMS program. This study was made possible in part by CDC grant #1U01DP003145.
Disclaimer
The findings and conclusions described in this article are those of the authors and do not necessarily represent the official position of the Hawai‘i State Department of Health, the Centers for Disease Control and Prevention, or any other organization.
Conflict of Interest
None of the authors have any financial or other conflict of interests to disclose.
References
- 1.Malm H, Martikainen J, Klaukka T, Neuvonen PJ. Prescription of hazardous drugs during pregnancy. Drug Safety: An International Journal of Medical Toxicology and Drug Experience. 2004;27(12):899–908. doi: 10.2165/00002018-200427120-00006. [DOI] [PubMed] [Google Scholar]
- 2.van Gelder MM, van Rooij IA, Miller RK, Zielhuis GA, de Jong-van den Berg LT, Roeleveld N. Teratogenic mechanisms of medical drugs. Human Reproduction Update. 2010 Jul-Aug;16(4):378–394. doi: 10.1093/humupd/dmp052. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell AA, Gilboa SM, Werler MM, Kelley KE, Louik C, Hernandez-Diaz S. Medication use during pregnancy, with particular focus on prescription drugs: 1976-2008. American Journal of Obstetrics and Gynecology. 2011 Jul;205(1):51.e51–58. doi: 10.1016/j.ajog.2011.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parisi MA, Spong CY, Zajicek A, Guttmacher AE. We don't know what we don't study: the case for research on medication effects in pregnancy. American Journal of Medical Genetics. Part C, Seminars in Medical Genetics. 2011 Aug 15;157c(3):247–250. doi: 10.1002/ajmg.c.30309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowen ME, Ray WA, Arbogast PG, Ding H, Cooper WO. Increasing exposure to angiotensin-converting enzyme inhibitors in pregnancy. American Journal of Obstetrics and Gynecology. 2008 Mar;198(3):291.e291–295. doi: 10.1016/j.ajog.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Kulaga S, Zargarzadeh AH, Berard A. Prescriptions filled during pregnancy for drugs with the potential of fetal harm. BJOG: An International Journal of Obstetrics and Gynaecology. 2009 Dec;116(13):1788–1795. doi: 10.1111/j.1471-0528.2009.02377.x. [DOI] [PubMed] [Google Scholar]
- 7.Cooper WO, Hickson GB, Ray WA. Prescriptions for contraindicated category X drugs in pregnancy among women enrolled in TennCare. Paediatric and Perinatal Epidemiology. 2004 Mar;18(2):106–111. doi: 10.1111/j.1365-3016.2003.00542.x. [DOI] [PubMed] [Google Scholar]
- 8.Yang T, Walker MC, Krewski D, et al. Maternal characteristics associated with pregnancy exposure to FDA category C, D, and X drugs in a Canadian population. Pharmacoepidemiology and Drug Safety. 2008 Mar;17(3):270–277. doi: 10.1002/pds.1538. [DOI] [PubMed] [Google Scholar]
- 9.Guttmacher Institute, author. Facts on Unintended Pregnancy in the United States. New York: Guttmacher Institute; 2012. [Google Scholar]
- 10.Desai G, Babu GN, Chandra PS. Unplanned pregnancies leading to psychotropic exposure in women with mental illness - Findings from a perinatal psychiatry clinic. Indian Journal of Psychiatry. 2012 Jan;54(1):59–63. doi: 10.4103/0019-5545.94649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daw JR, Mintzes B, Law MR, Hanley GE, Morgan SG. Prescription drug use in pregnancy: a retrospective, population-based study in British Columbia, Canada (2001–2006) Clinical Therapeutics. 2012 Jan;34(1):239–249.e232. doi: 10.1016/j.clinthera.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 12.Andrade SE, Gurwitz JH, Davis RL, et al. Prescription drug use in pregnancy. American Journal of Obstetrics and Gynecology. 2004 Aug;191(2):398–407. doi: 10.1016/j.ajog.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 13.Irvine L, Flynn RW, Libby G, Crombie IK, Evans JM. Drugs dispensed in primary care during pregnancy: a record-linkage analysis in Tayside, Scotland. Drug Safety: An International Journal of Medical Toxicology and Drug Experience. 2010 Jul 1;33(7):593–604. doi: 10.2165/11532330-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 14.Katayama Y, Terao T, Kamei K, et al. Therapeutic window of lamotrigine for mood disorders: a naturalistic retrospective study. Pharmacopsychiatry. 2014 May;47(3):111–114. doi: 10.1055/s-0034-1375618. [DOI] [PubMed] [Google Scholar]
- 15.Rheims S, Ryvlin P. Pharmacotherapy for tonic-clonic seizures. Expert Opinion on Pharmacotherapy. 2014 May 6; doi: 10.1517/14656566.2014.915029. [DOI] [PubMed] [Google Scholar]
- 16.State & County Quickfacts: Hawaii. 2010. [7 August 2013]. http://quickfacts.census.gov/qfd/states/15000.html.
- 17.Sorensen C, Wood B, Prince EW. Race & ethnicity data: developing a common language for public health surveillance in Hawaii. California Journal of Health Promotion. 2003;1(Special Issue: Hawaii):91–104. [Google Scholar]
- 18.Department of Health and Human Services, author. Annual Update of the HHS Poverty Guidelines. 2011;76:3637–3638. From the Federal Register Online via GPO Access [ wais.access.gpo.gov] [Google Scholar]
- 19.Department of Health and Human Services, author. 2009 HHS Poverty Guidelines Extended Until March 1, 2010. 2010;75:3734–3735. From the Federal Register Online via GPO Access [ wais.access.gpo.gov] [Google Scholar]
- 20.Department of Health and Human Services, author. Delayed Update of the HHS Poverty Guidelines for the Remainder of 2010. 2010;75:45628–45629. From the Federal Register Online via GPO Access [ wais.access.gpo.gov] [Google Scholar]
- 21.Department of Health and Human Services, author. Annual Update of the HHS Poverty Guidelines. 2009;74:4199–4201. From the Federal Register Online via GPO Access [ wais.access.gpo.gov] [Google Scholar]
- 22.DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care. 2004 Mar;42(3):200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 23.Osterberg L, Blaschke T. Adherence to medication. The New England Journal of Medicine. 2005 Aug 4;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 24.Solomon MD, Majumdar SR. Primary non-adherence of medications: lifting the veil on prescription-filling behaviors. Journal of General Internal Medicine. 2010 Apr;25(4):280–281. doi: 10.1007/s11606-010-1286-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. Journal of General Internal Medicine. 2010 Apr;25(4):284–290. doi: 10.1007/s11606-010-1253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petersen EE, Rasmussen SA, Daniel KL, Yazdy MM, Honein MA. Prescription medication borrowing and sharing among women of reproductive age. Journal of Women's s Health (2002) 2008 Sep;17(7):1073–1080. doi: 10.1089/jwh.2007.0769. [DOI] [PubMed] [Google Scholar]
- 27.Beyene KA, Sheridan J, Aspden T. Prescription medication sharing: a systematic review of the literature. American Journal of Public Health. 2014 Apr;104(4):e15–26. doi: 10.2105/AJPH.2013.301823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Gelder MM, van Rooij IA, de Walle HE, Roeleveld N, Bakker MK. Maternal recall of prescription medication use during pregnancy using a paper-based questionnaire: a validation study in the Netherlands. Drug Safety: An International Journal of Medical Toxicology and Drug Experience. 2013 Jan;36(1):43–54. doi: 10.1007/s40264-012-0004-8. [DOI] [PubMed] [Google Scholar]
- 29.Matsui D. Adherence with drug therapy in pregnancy. Obstetrics and Gynecology International. 2012;2012:796590. doi: 10.1155/2012/796590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stuart GS, Grimes DA. Social desirability bias in family planning studies: a neglected problem. Contraception. 2009 Aug;80(2):108–112. doi: 10.1016/j.contraception.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Farmer KC. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clinical Therapeutics. 1999 Jun;21(6):1074–1090. doi: 10.1016/S0149-2918(99)80026-5. discussion 1073. [DOI] [PubMed] [Google Scholar]
- 32.Halbesleben JR, Whitman MV. Evaluating survey quality in health services research: a decision framework for assessing nonresponse bias. Health Services Research. 2013 Jun;48(3):913–930. doi: 10.1111/1475-6773.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]