Abstract
A brain tumor is an intracranial neoplasm within the brain or in the central spinal canal. Primary malignant brain tumors affect about 200,000 people worldwide every year. Brain cells have special characters. Due to the specific properties of brain tumors, including epidemiology, growth, and division, investigation of brain tumors and the interpretation of results is not simple. Research to identify the genetic alterations of human tumors improves our knowledge of tumor biology, genetic interactions, progression, and preclinical therapeutic assessment. Obtaining data for prevention, diagnosis, and therapy requires sufficient samples, and brain tumors have a wide range. As a result, establishing the bank of brain tumors is very important and essential.
Keywords: Banking, brain, tumor
INTRODUCTION
Brain tumor is an intracranial neoplasm that occurs in the brain or the central spinal canal. An abnormal and uncontrolled cell division, usually in the brain, involving neurons or glial cells (which include astrocytes, oligodendrocytes, and ependymal cells) or occasionally in the lymphatic tissue, blood vessels, cranial nerves, brain envelopes (meninges), skull, pituitary gland, or pineal gland is the main leading cause of formation of primary brain tumors (PBTs). Majority of the brain tumors in adults are secondary or metastatic tumors, i.e. cancers that are primarily located in other organs may spread to the brain and create brain tumors.[1]
Primary central nervous system tumors (PCNSTs) reflect different pathologic entities and indicate a major heterogeneity which may be of benign, malignant, or unpredictable evolution.[2,3]
CLASSIFICATION OF TUMORS OF THE CENTRAL NERVOUS SYSTEM
The tumors of the central nervous system (CNS) have been classified from benign and localized tumors to malignant and infiltrating tumors. This classification indicates the rate of tumor progressiveness and is accepted for use worldwide. The most-well known classification is the World Health Organization's (WHO) classification of tumors of the CNS [Table 1].[4] Different types of tumors of the CNS exist. Each of them may be classified into diverse grades, including neuroepithelial and non-neuroepithelial tumors.[5]
Table 1.
Histologic classification of primary brain tumors*
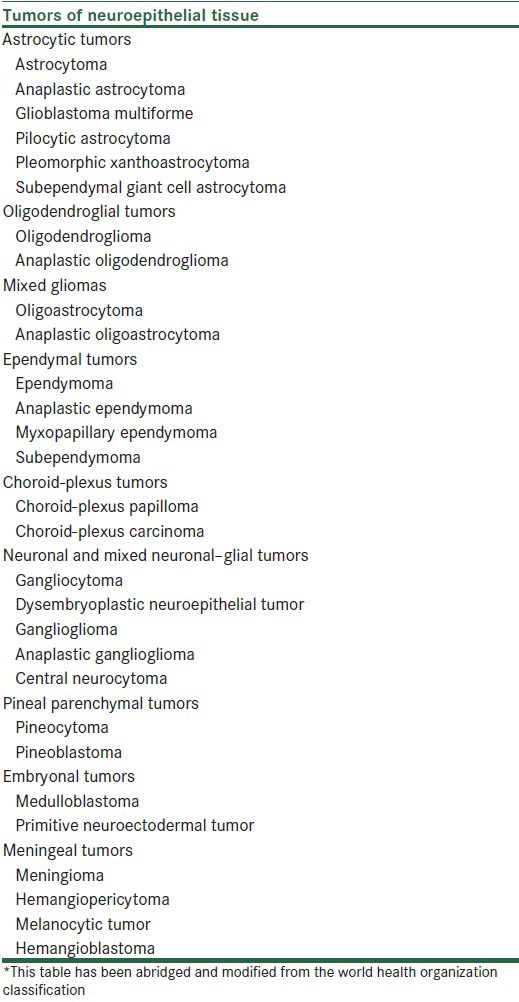
The first edition of the international classification of human nervous system tumors was prepared by Zόlch and published in 1979. Its specific aim has not changed until now. This classification has been updated over the years. The fourth (the last) edition of the WHO classification of tumors of the CNS was published in 2007.[5]
The International Classification of Diseases for Oncology (ICD-O) evolved more than 30 years ago which shows the relationship between pathologists and cancer registries. The histopathologic stratification based on population incidence and mortality data is used for epidemiological and oncological researches.
With time and understanding of the genetic characteristics of neoplasms, histology codes have been completed. The College of American Pathologists (CAP) published the systematized nomenclature of medicine (SNOMED) which uses the ICD-O histology codes.[5] The fourth edition of ICD-O (ICD-O-4) was published in the summer of 2007 and basic codes were identified for several new entities and variants.[5] The application of histologic grading helps to predict the biological behavior of a neoplasm. In fact, tumor grading assists the clinician in choosing the best method of treatment. The WHO classification of tumors of the nervous system determines the malignancy scale ranging across a wide variety of neoplasms.[6,7]
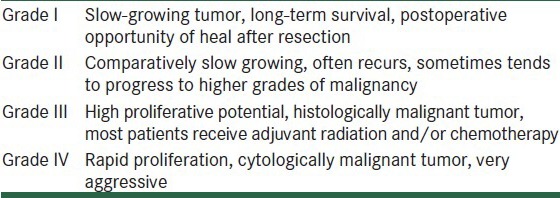
Combining the clinical status, tumor location, genetic alterations, and the extent of surgical resection which are associated with WHO tumor grade, may be used for the prognosis. Survival rate in patients with WHO grade II, III, and IV tumors is different. It is typically more than 5 years, 2-3 years, and rapidly fatal if untreated, respectively [Table 2].[5]
Table 2.
WHO grading of tumors of the central nervous system
MOLECULAR EPIDEMIOLOGY OF PBTs
Primary malignant brain tumors affect about 200,000 people worldwide every year. These tumors include the worst elements of cancer with the most serious neurological diseases. Brain tumors can affect anyone at any age with devastating and lethal effects. So, a major public health problem is caused by these tumors.[4,8]
The incidence rate of PBTs in the United States is high. Data obtained from different surveys indicate that about 77% of PBTs are gliomas. These types of brain tumors are very lethal with poor survival.[9]
PBTs are multifactorial disorders. Therefore, a combination of genetic and environmental factors is involved. Apart from vinyl chloride, ionizing radiation, and HIV infection, the environmental factors associated with brain tumors are not known. Although studies have not revealed an association between brain tumors and cell phone radiation, according to the classification of WHO, the radiation is possibly carcinogenic.[9] In addition, some reports have mentioned radiation to head as an environmental factor for brain tumor. Being affected by some inherited diseases, such as von Hippel-Lindau syndrome, multiple endocrine neoplasia, and neurofibromatosis type 2, increases the risk of developing brain tumors.[10] Many susceptible loci may contribute to the development of PBTs, and mutations and deletions of some genes such as tumor suppressor genes are thought to be the cause of some types of brain tumors.
One of the important tools for identifying genes having a role in common human genetic diseases is genome-wide association studies (GWAS) which are carried out with very large sample sizes. With this technology, it is possible to examine polymorphisms at the single nucleotide level. Most likely, single nucleotide polymorphisms (SNPs) exhibit changes during the process of carcinogenesis. Thus, SNPs could be used as appropriate biomarkers. The major pathways in the initiation of gliomas are related to DNA repair and inflammation mechanisms. However, the polymorphisms in cell cycle and metabolic pathways may be important. In general, unknown somatic mutations and the interaction between mutations and environmental exposure are the major critical risk factors for PBTs’ initiation.[3,11,12]
SPECIAL CHARACTERS OF BRAIN CELLS AND BRAIN TUMORS
There are basic symptoms associated with the diagnosis of a brain tumor. The most common symptom is neurologic disability, and in an advanced condition, progressive functional impairment, cognitive decline, and death may be seen. Despite the progress that has been made in the treatment and survival, there remains substantial symptom burden associated with the diagnosis of a brain tumor. In order to alleviate symptoms, decelerate neurologic impairment, and prolong life, palliative therapy, tumor removal surgery, radiotherapy, and chemotherapy are given, but many therapies consequently have severe secondary symptoms that can diminish the quality of life.[13,14]
Despite the histopathologic classification being accurate, tumor growth does not always correspond with the tumor grade. For instance, some low-grade gliomas unexpectedly exhibit malignancies, although they generally are benign. Some meningiomas recur after surgical excision. Therefore, additional indicators are used for strict prediction of the brain tumor status and the malignant potential of these tumors.[15]
The molecular components of brain endothelial tight junctions include transmembrane proteins occludin and claudin 1 and 5, and junctional adhesion molecules that bind the neighboring cells together and create the blood-brain barrier (BBB). A normal BBB is maintained by normal astrocytes. So, deficiency of endothelial tight junctions is a result of astrocyte deficiency, leading to BBB disruption, causing fluid leaking out into the extracellular space.[16,17,18]
Once a neuron is created, it loses the ability to divide and differentiate. This process is a unique contribution to form the basic wiring format that determines a neuronal system. It is necessary to protect this pattern for the overall generation and storage of memories and also attainment of other brain skills. It seems that the differentiated neurons are irreversibly post-mitotic; perhaps the cytoskeleton and synapses are impaired by a hypothetical cell division. This event can cause disruption in the neuronal connectivity and function. Therefore, it is reasonable that when a nerve cell is differentiated, cell division is halted.[19]
GENETICS OF BRAIN TUMORS
Understanding the genetic alterations of human tumors improves our knowledge of tumor biology, genetic interactions, progression, and preclinical therapeutic assessment. Genetic disorders cause 5-10% of PBTs. So, some of the syndromes and associated genes are related to brain tumor, including Von Recklinghausen disease (also called neurofibromatosis 1 encoded by NF1 gene), neurofibromatosis 2 (NF2 gene), Turcot syndrome (APC gene), Gorlin syndrome (also called basal cell nevus syndrome encoded by PTCH gene), tuberous sclerosis (TSC1 and TSC2 genes), and Li-Fraumeni syndrome (TP53 gene).[20,21] In addition, many oncogenes (like growth factors) are involved in brain tumors. Epidermal growth factor receptor (EGFR) plays an important role in high-grade brain tumors such as glioblastoma multiforme (GBM).[22]
Several genetic mutations in tumor suppressor genes have been found in gliomas. Mutations in the tumor suppressor protein 53 (p53) occur as an early event, and when p53 is mutated, other mutations can survive. Phosphatase and tensin homolog (PTEN) that helps to destroy cells with dangerous mutations is lost or mutated in brain tumors.[23]
Mitochondria are involved in apoptosis and the isocitrate dehydrogenase 1 (IDH1) and isocitrate dehydrogenase 2 (IDH2) genes play a role in the mitochondrial citric acid cycle and apoptosis. Therefore, mutations of these two genes may lead to lack of apoptosis and vascularization in gliomas.[22]
Meningiomas are categorized into three grades: Benign (Grade I, slow growing), atypical (Grade II), and anaplastic (Grade III). The causes of meningiomas are not well understood. Most cases are sporadic and random, while some of them are familial.[24,25,26]
Some genetic alterations in sporadic meningiomas including mutations in NF2 (22q12), chromosomal losses (1p, 6q, 10, 14q, and 18q), and chromosomal gains (1q, 9q, 12q, 15q, 17q, and 20q) have been observed. In addition, mutations in other possible genes/loci including MN1, PTEN, AKT1, SMO, and an unknown gene at 1p13 have also been reported. PTEN inactivation leads to activation of AKT gene and defects in mitochondrial respiration. Some deletions and insertions among the genes involved in DNA repair, cell cycle regulation, detoxification, and hormone metabolic pathways (like variants in the GST and CYP450 genes) are very important in the progression of meningioma. For example, the EPB41L3 or DAL1 gene is located at 18p11.3 and encodes protein 4.1B, a regulator of proliferation and apoptosis. Loss of protein 4.1B has been demonstrated in meningiomas.[27,28,29,30]
Genetic analysis of meningioma has revealed loss of 1p, 10q, 14q, 6q, and 18q. The latter two are less common. Higher grades of meningioma are also associated with chromosomal gains on 1q, 9q, 12q, 15q, 17q, and 20q. Anaplastic meningiomas show more frequent loss on 6q, 10q, 14q, and 9p, with amplification on 17q23.[23,31,32,33,34]
Atypical and anaplastic meningiomas reveal more complex genetic alteration than their benign counterparts, with 1p, 10q, and 14q deletions and less frequent 6q and 18q deletions. Higher grades are also associated with gain of 1q, 9q, 12q, 15q, 17q, and 20q. In addition, anaplastic meningiomas show more frequent loss on 6q, 10q, 14q, and 9p, with amplification on 17q23.[23,35,36]
Loss of chromosome 1p is the second most common chromosomal abnormality in meningiomas and is more frequent in higher grade tumors. CDKN2C, RAD54L, EPB41, GADD45A, RAD54L, TP73, and ALPL have been candidate genes in this arm.[23,35]
Deletion of chromosome 14 happens similar to 1p deletion, which is vital in meningioma progression.[23,37] Loss of 1p and 14q is common in anaplastic meningiomas. NDRG2 is a tumor suppressor gene on 14q. Inactivated NDRG2 was observed in anaplastic meningiomas and a subset of lower grade, yet clinically aggressive atypical meningiomas. The loss of gene 3 (MEG3; candidate tumor suppressor on 14q32) is associated with higher tumor grades.[23]
Although mutations of TP53 (17q) are found in many other cancers, direct alterations in TP53 are rare in meningiomas; instead, regulators of the pathway are often mutated.[36,38]
Alterations of 9p have an association with specific loss of CDKN2A/p16INKa (encoding p16), p14ARF (encoding p14), and CDKN2B/p15ARF (encoding p15). All three tumor suppressor genes are located on 9p21. p14 is a tumor suppressor gene that regulates apoptosis through the modulation of the p53 pathway. Cell cycle progression is controlled by p16 and p15 through the G1/S-phase checkpoint.[36,39]
Some genes such as PTEN, MXI1, and DMBT1 have been identified on chromosome 10q23-q25 and deletions of these genes are associated with progression of meningiomas. Though changes in PTEN (tumor suppressor gene) have been identified in Cowden syndrome, they are rare in meningiomas.[1,2] Higher grades of meningiomas show amplification of proto-oncogene S6 kinase (RPS6K) gene on 17q233.[33,37]
In atypical and anaplastic meningioma, some deletions on chromosome 18 are frequently seen. Loss of MADH2, MADH4, APM-1, and DCC tumor suppressor genes on chromosome 18 has been identified in the progression of meningioma.[23]
Loss of heterozygosity at 1p, 9p, 10q, 17p, and 19q occurs in granular cell astrocytoma (GCA) tumors. Especially, deletion of 9p and 10q was identified in almost all cases of GCA. Furthermore, TP53 mutations and p14 and p16 combined deletions were determined in some high-grade GCA tumors.[23]
In human malignant astrocytoma cells, loss of the transcription factor GATA6 (glial fibrillary acidic protein; GFAP) leads to enhanced proliferation and transformation of astrocytes. Loss of GATA6 expression in human malignant astrocytoma cells can reduce their tumorigenic growth with decrease in VEGF expression. Loss-of-function mutations in human malignant astrocytoma have been detected in GATA6 gene. Expression of GATA6 and p53−/− leads to increase in the rate of tumorigenesis.[23,40]
GBM is the most aggressive malignant primary human brain tumor with different grades. Expression of oncogene Ha-Ras (V12Ha-Ras) under the control of the astrocyte-specific human GFAP promoter is caused glioblastoma. Loss of the transcription factor GATA6 (tumor suppressor gene in human astrocytomas) leads to astrocytoma progression rather than initiation.[40]
CYTOGENETICS OF HUMAN BRAIN TUMORS
The most common cytogenetic mutations in PBTs are gains or losses of entire chromosomes, intrachromosomal deletion, gene amplification with the presence of double minute chromosomes (DMs), or unbalanced translocation. These alterations vary in different types of tumors and are individual specific. Lack of specific genes or chromosomes may lead to loss of function of tumor suppressor genes and initiate brain tumors. In addition, gene amplification may result in gain of function of proto-oncogenes and cell proliferation.[41]
Some of the most common cytogenetic alterations are as follows. Gain of chromosome 7 and loss of chromosome 10 are the most frequent changes in malignant gliomas, although loss of chromosome 22, short arm of chromosome 9 (9p), and the sex chromosomes takes place in some cases. Epidermal growth factor receptor gene is the most common gene amplified with DMs in tumor. Loss of 17p and c-myc gene amplification with DMs is observed in medulloblastomas. Deletions of chromosome 22 occur in meningiomas. Evaluation of cytogenetic abnormalities in human brain tumors can help to determine tumor suppressor genes and proto-oncogenes that are crucial in the development of these tumors.[41]
Many different genes that control proliferation, differentiation, maintenance of ion and solute homeostasis, and apoptosis are involved in cancer. Broad patterns of gene expression in tumor cells versus normal tissue can be identified with new technologies such as cDNA and oligonucleotide microarray analysis. Although several reports have indicated the application of DNA microarray analysis in human brain tumors, the heterogeneity of the tumors that results from complex and variable nature of them l eads to lack of a consistent genetic blueprint for describing a specific brain tumor. Although by examining the gene expression profiles of many more samples more precise results can be obtained, tumor-specific genes can be identified and make it possible to distinguish distinct subclass of any tumor type and select the appropriate treatment strategy for each tumor type. For example, in a study about GBMs, overexpression of the pro-inflammatory cytokine, macrophage migration inhibitory factor (MIF), and aquaporin-1 (AQP-1) genes and underexpression of a variety of ion and solute transport related proteins, including NMDAR2A (a subunit of N-methyl-D-aspartate) and 2C, GABAA (g-aminobutyric acid), and AMPA-2 (α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) receptors, as well as the glutamate/aspartate transporter II and NHE-1 were reported. More likely, these alterations in expression are associated with brain tumor development, proliferation, and infiltration into surrounding tissues.[42,43,44,45,46]
EPIGENETIC ALTERATIONS OF BRAIN TUMORS
In addition to genetic changes, epigenetic alteration is tumor subtype and tumor grade specific. CpG island hypermethylation is one of the epigenetic alterations in brain tumors which can lead to silencing of tumor suppressor gene. For example, in gliomas, CpG island promoters of different genes with various functions such as cell cycle regulation, DNA repair, apoptosis, angiogenesis, invasion, and drug resistance that are related to tumorigenesis and tumor progression are hypermethylated. Some of these genes are CDKN2/p16, RB, PTEN, TP53, and p14ARF.[17,47,48]
Another epigenetic alteration in brain tumors is gene-specific hypomethylation that causes aberrant gene activation and genome-wide hypomethylation that is associated with loss of imprinting, chromosomal instability, and cellular hyperproliferation. For instance, in primary GBMs hypomethylation and transcriptional activation of oncogene MAGEA1 exists leading to cellular proliferation. Changes in histone modifications and changes in the position of histone variants have been also seen as other epigenetic alterations in brain tumor. Medication therapy and using appropriate drugs and diets may theoretically reverse epigenetic alteration. However, drug targeting is a controversial issue for epigenetic therapy of cancer and may lead to unwanted gene activation or unintentional gene silence. Both DNA hypermethylation and hypomethylation are seen in cancer genomes. Thus, drug treatment for reactivating silenced tumor suppressors may result in undesired activation of oncogenes through hypomethylation. Even though, with promoting of our knowledge and awareness about molecular events resulting from epigenetic-based therapy might be control unwanted effects. Hypermethylated cancer genes are found in the blood plasma of cancer patients and are dependent on the methylation patterns. They could act as tumor-specific biomarkers and can be detected in a sample by methylation-sensitive polymerase chain reaction (PCR).[18,47,49]
MARKERS IN BRAIN TUMORS
Although there are no single or specific clinical signs for brain tumors, the combination of symptoms and the absence of relevant clinical indications of infections or other corresponding factors can be an indicator to redirect diagnostic investigation toward the possibility of intracranial tumor. Brain tumors have similar characteristics when it comes to diagnosis and treatment of tumors located elsewhere in the body. However, they have specific issues that follow closely the properties of the organ that contains them.[50]
Also, both low-grade and high-grade brain tumors can invade normal brain tissue. So, surgery is usually not successful in removing all the cancerous cells. Since cell cycle behavior and limitations of growth and proliferation in CNS cells are very important, expression of some involved cell cycle genes in patients affected with brain tumors might be considered as a biomarker which would enable us to diagnose cancerous cells in future. Many studies have been conducted in different areas with regard to brain tumors. For instance, genes encoding cyclin D2, p53, and Rb, and ATM as cell cycle genes which regulate cell growth and proliferation were examined in two types of brain tumors, including astrocytoma and meningioma.[51]
Moreover, proper markers are needed for finding the accurate stage of tumor growth and the malignant potential of brain tumors due to lack of accurate histopathologic classification for tumor growth prediction in some cases. Using predisposing factor(s) and novel bio- and molecular markers of brain tumor is essential for an early applicable, effective, and translatable diagnostic-prognostic-predictive package. Furthermore, telomere length is considered as a key element for prognosis because of the variation in telomere length at genomic-tumor cells of the same patient, accompanied by the mode of action of telomerase. It seems that telomere length is influenced by a network of different profiles at cellular and molecular levels, and the contribution of human chromosomes can lead to evolution through alteration of telomere length. Genomic-tumor heterogeneity and instability in brain tumors might be traced by the evolutionary hypothesis of telomere length.[52]
Although telomerase activity is associated with tumor malignancy, obviously, activation of telomerase has been observed in some low-grade brain tumors including meningioma and astrocytoma.[53,54,55]
Although any correlation between telomerase activity and telomere length has not been found, obviously, the regulation of telomerase activity and telomere length is an intricate and dynamic event that is strongly related to cell cycle regulation in human stem cells and telomerase activation is not the only mechanism for the elongation of telomere.[56]
Accordingly, alterations in telomere length and telomerase activity together in human brain tumors may be considered as an essential prognostic marker.[54,57]
GENETIC STRATEGIES FOR BRAIN TUMOR THERAPY
Gene therapy is a potentially beneficial approach for human brain tumors. Human brain tumors such as gliomas are resistant to conventional treatment, which consists of aggressive surgical resection, radiation, and chemotherapy. Their highly infiltrative characteristic prevents complete resection, resulting in recurrence. As a promising alternative therapy, gene therapy has been introduced. This enables us to target tumor cells specifically. Most studies have been conducted on gliomas. Despite the success obtained in animal models, there is little efficiency in the clinical trial because of low levels of gene transduction in patients.[58,59,60]
In cancers with poor prognosis, such as glioblastoma, where conventional surgery, chemotherapy, and radiation regimens constitute little more than palliative measures, the use of replicating viruses as a promising experimental treatment strategy may be warranted, especially if the benefits outweigh the potential risks.[61]
Conventional surgery, chemotherapy, and radiation therapy constitute little more than palliative measures in the case of tumors with poor prognosis such as glioblastoma. In this case, the use of replicating viruses such as murine leukemia virus (MLV)-based replication-competent retroviral (RCR) vectors may be as a promising and warranted experimental treatment strategy, particularly if the therapeutic benefits outweigh the potential risk. Significant advantages for virotherapy, including inherent tumor selectivity due to an absolute inability to infect quiescent normal cells, a relatively small genome size which makes it easy to manipulate, and an ability to transduce tumor cells efficiently and stably in vivo are considered.[61] There is high hope for the bright future of gene therapy because of recent advances in viral vectors, the development of stem cell technology, and increased understanding of the mechanism of action of therapeutic transgenes. Recent advances in several areas of the bioloy have been very influential in developing successful therapeutic strategies. For example, data from the human genome sequencing project will enable us to identify new candidates for gene therapy and will improve tumor-specific treatment. Noninvasive imaging techniques, leading to better assessment of continuous quantitative data, have helped us in the in vivo study of tumors in animals and patients. Three-dimensional neuronavigation techniques and automated slow-speed injection/infusion devices enable constant injection into the tumor and prevent the spread of vectors around the tumor site. New technologies, such as RNAi and stem cells, have improved our ability to probe new therapeutic strategies.[58,59,60]
ESTABLISHING A BRAIN TUMOR BANK
Tumor bank is a term usually used to describe a service that collects, stores, and distributes fresh human tumor tissue for biomedical and cancer research. Most tumor banks provide their tumor samples from discarded tissues not needed for pathologic diagnosis, after the tumor is removed by surgery. The tissue is immediately snap frozen in liquid nitrogen, or may also be preserved in special fixatives. Many cancer centers have a tumor bank that has samples of tumor from patients, and associated adjacent normal tissue as control. Advances in diagnostic methods and biomarker detection techniques need access to a sufficient number of samples and creating a tumor bank is an essential step in this case.[62,63] Annually, a large number of surgical procedures are performed on the tumors that are a vast treasure of cancer cells. These cells are suitable to research and it is possible to collect them, establishing tumor banks.[64]
Also, on the one hand, cells and brain tumors have special characters. These particular properties include several items such as the epidemiology of brain tumors, growth, and division. Therefore, research in brain tumors and interpretation of results is not simple. On the other hand, research to obtain extensive data for prevention, diagnosis, and therapy requires sufficient samples. However, brain tumors have a wide range with different stages. According to what has been mentioned earlier, the formation of the bank of brain tumors is very important and essential to conduct a comprehensive investigation.
Based on what has been mentioned earlier, it is essential and critical to encourage establishing banks of brain tumor that had been resected during neurosurgery from the brain tissue of patients. In addition, the exchange of tissue among researchers will lead to more comprehensive understanding of the makeup of these neoplasms and ultimately better treatments can be considered for them.
It should be noted that only a small amount of tumor tissue is needed for the pathological diagnosis to determine the type and grade of neoplasm. The remaining tumor tissue is often discarded which means precious research material is wasted.
Maintaining optimal brain tumor tissue, which is a correctly catalogued and encoded sample, with proper consent will create the building blocks for the next generation of therapies. Moral development and management of samples with carefully implemented quality assurance measures will hopefully ensure that the removed brain tumor sample can be utilized to discover and validate investigations which will benefit those patients who are diagnosed with this disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Barrow Neurological Institute: About Brain Tumors. [Last accessed on 2013 May 30]. Available from: http://www.thebarrow.org .
- 2.McCarthy BJ, Surawicz T, Bruner JM, Kruchko C, Davis F. Consensus conference on brain tumor definition for registration. November 10, 2000. Neuro Oncol. 2002;4:134–45. doi: 10.1215/15228517-4-2-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wrensch M, Minn Y, Chew T, Bondy M, Berger MS. Epidemiology of primary brain tumors: Current concepts and review of the literature. Neuro Oncol. 2002;4:278–99. doi: 10.1093/neuonc/4.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeAngelis LM. Brain tumors. N Engl J Med. 2001;344:114–23. doi: 10.1056/NEJM200101113440207. [DOI] [PubMed] [Google Scholar]
- 5.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993;3:255–68. doi: 10.1111/j.1750-3639.1993.tb00752.x. [DOI] [PubMed] [Google Scholar]
- 7.Zulch KJ. International histological classification of tumours. Geneva: World Health Organization; 1979. Histological typing of tumours of the central nervous system. [Google Scholar]
- 8.The First Walk Around the World for Brain Tumours. International Brain Tumour Alliance; 2008. In 2007 the International Brain Tumour Alliance (IBTA) commissioned research from the Central Brain Tumor Registry of the United States (CBTRUS) which projected that in 2010 the worldwide incidence of malignant primary brain tumours may climb to 220,568; p. 38. ISBN 9780646494814. [Google Scholar]
- 9.Frei P, Poulsen AH, Johansen C, Olsen JH, Steding-Jessen M, Schüz J. Use of mobile phones and risk of brain tumours: Update of Danish cohort study. BMJ. 2011;343:d6387. doi: 10.1136/bmj.d6387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huson SM, Harper PS, Hourihan MD, Cole G, Weeks RD, Compston DA. Cerebellar haemangioblastoma and von Hippel-Lindau disease. Brain. 1986;109:1297–310. doi: 10.1093/brain/109.6.1297. [DOI] [PubMed] [Google Scholar]
- 11.Inskip PD, Linet MS, Heineman EF. Etiology of brain tumors in adults. Epidemiol Rev. 1995;17:382–414. doi: 10.1093/oxfordjournals.epirev.a036200. [DOI] [PubMed] [Google Scholar]
- 12.Gu J, Liu Y, Kyritsis AP, Bondy ML. Molecular epidemiology of primary brain tumors. Neurotherapeutics. 2009;6:427–35. doi: 10.1016/j.nurt.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lovely MP. Symptom management of brain tumor patients. Semin Oncol Nurs. 2004;20:273–83. [PubMed] [Google Scholar]
- 14.Lovely MP, Miaskowski C, Dodd M. Relationship between fatigue and quality of life in patients with glioblastoma multiformae. Oncol Nurs Forum. 1999;26:921–5. [PubMed] [Google Scholar]
- 15.Hiraga S, Ohnishi T, Izumoto S, Miyahara E, Kanemura Y, Matsumura H, et al. Telomerase activity and alterations in telomere length in human brain tumors. Cancer Res. 1998;58:2117–25. [PubMed] [Google Scholar]
- 16.Papadopoulos MC, Saadoun S, Binder DK, Manley GT, Krishna S, Verkman AS. Molecular mechanisms of brain tumor edema. Neuroscience. 2004;129:1011–20. doi: 10.1016/j.neuroscience.2004.05.044. [DOI] [PubMed] [Google Scholar]
- 17.Bello MJ, Rey JA. The p53/Mdm2/p14ARF cell cycle control pathway genes may be inactivated by genetic and epigenetic mechanisms in gliomas. Cancer Genet Cytogenet. 2006;164:172–3. doi: 10.1016/j.cancergencyto.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Cadieux B, Ching TT, VandenBerg SR, Costello JF. Genome-wide hypomethylation in human glioblastomas associated with specific copy number alteration, methylenetetrahydrofolate reductase allele status, and increased proliferation. Cancer Res. 2006;66:8469–76. doi: 10.1158/0008-5472.CAN-06-1547. [DOI] [PubMed] [Google Scholar]
- 19.Currais A, Hortobágyi T, Soriano S. The neuronal cell cycle as a mechanism of pathogenesis in Alzheimer's disease. Aging (Albany NY) 2009;1:363–71. doi: 10.18632/aging.100045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neglia JP, Robison LL, Stovall M, Liu Y, Packer RJ, Hammond S, et al. New primary neoplasms of the central nervous system in survivors of childhood cancer: A report from the childhood cancer survivor study. J Natl Cancer Inst. 2006;98:1528–37. doi: 10.1093/jnci/djj411. [DOI] [PubMed] [Google Scholar]
- 21.Ricard D, Idbaih A, Ducray F, Lahutte M, Hoang-Xuan K, Delattre JY. Primary brain tumours in adults. Lancet. 2012;379:1984–96. doi: 10.1016/S0140-6736(11)61346-9. [DOI] [PubMed] [Google Scholar]
- 22.Goodenberger ML, Jenkins RB. Genetics of adult glioma. Cancer Genet. 2012;205:613–21. doi: 10.1016/j.cancergen.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Choy W, Kim W, Nagasawa D, Stramotas S, Yew A, Gopen Q, et al. The molecular genetics and tumor pathogenesis of meningiomas and the future directions of meningioma treatments. Neurosurg Focus. 2011;30:E6. doi: 10.3171/2011.2.FOCUS1116. [DOI] [PubMed] [Google Scholar]
- 24.Goldsmith BJ, Wara WM, Wilson CB, Larson DA. Postoperative irradiation for subtotally resected meningiomas: A retrospective analysis of 140 patients treated from 1967 to 1990. J Neurosurg. 1994;80:195–201. doi: 10.3171/jns.1994.80.2.0195. [DOI] [PubMed] [Google Scholar]
- 25.Longstreth WT, Jr, Dennis LK, McGuire VM, Drangsholt MT, Koepsell TD. Epidemiology of intracranial meningioma. Cancer. 1993;72:639–48. doi: 10.1002/1097-0142(19930801)72:3<639::aid-cncr2820720304>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 26.Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957;20:22–39. doi: 10.1136/jnnp.20.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barnholtz-Sloan JS, Kruchko C. Meningiomas: Causes and risk factors. Neurosurg Focus. 2007;23:E2. doi: 10.3171/FOC-07/10/E2. [DOI] [PubMed] [Google Scholar]
- 28.Pelicano H, Xu RH, Du M, Feng L, Sasaki R, Carew JS, et al. Mitochondrial respiration defects in cancer cells cause activation of Akt survival pathway through a redox-mediated mechanism. J Cell Biol. 2006;175:913–23. doi: 10.1083/jcb.200512100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Staal FJ, van der Luijt RB, Baert MR, van Drunen J, van Bakel H, Peters E, et al. A novel germline mutation of PTEN associated with brain tumours of multiple lineages. Br J Cancer. 2002;86:1586–91. doi: 10.1038/sj.bjc.6600206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lekanne Deprez RH, Riegman PH, Groen NA, Warringa UL, van Biezen NA, Molijn AC, et al. Cloning and characterization of MN1, a gene from chromosome 22q11, which is disrupted by a balanced translocation in a meningioma. Oncogene. 1995;10:1521–8. [PubMed] [Google Scholar]
- 31.Ozaki S, Nishizaki T, Ito H, Sasaki K. Comparative genomic hybridization analysis of genetic alterations associated with malignant progression of meningioma. J Neurooncol. 1999;41:167–74. doi: 10.1023/a:1006086723607. [DOI] [PubMed] [Google Scholar]
- 32.Riemenschneider MJ, Perry A, Reifenberger G. Histological classification and molecular genetics of meningiomas. Lancet Neurol. 2006;5:1045–54. doi: 10.1016/S1474-4422(06)70625-1. [DOI] [PubMed] [Google Scholar]
- 33.Weber RG, Boström J, Wolter M, Baudis M, Collins V, Reifenberger G, et al. Analysis of genomic alterations in benign, atypical, and anaplastic meningiomas: Toward a genetic model of meningioma progression. Proc Natl Acad Sci U S A. 1997;94:14719–24. doi: 10.1073/pnas.94.26.14719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lamszus K, Lengler U, Schmidt NO, Stavrou D, Ergün S, Westphal M. Vascular endothelial growth factor, hepatocyte growth factor/scatter factor, basic fibroblast growth factor, and placenta growth factor in human meningiomas and their relation to angiogenesis and malignancy. Neurosurgery. 2000;46:938–48. doi: 10.1097/00006123-200004000-00033. [DOI] [PubMed] [Google Scholar]
- 35.Liu Y, Pang JC, Dong S, Mao B, Poon WS, Ng HK. Aberrant CpG island hypermethylation profile is associated with atypical and anaplastic meningiomas. Hum Pathol. 2005;36:416–25. doi: 10.1016/j.humpath.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 36.Mawrin C, Perry A. Pathological classification and molecular genetics of meningiomas. J Neurooncol. 2010;99:379–91. doi: 10.1007/s11060-010-0342-2. [DOI] [PubMed] [Google Scholar]
- 37.Lamszus K. Meningioma pathology, genetics, and biology. J Neuropathol Exp Neurol. 2004;63:275–86. doi: 10.1093/jnen/63.4.275. [DOI] [PubMed] [Google Scholar]
- 38.Zhang X, Gejman R, Mahta A, Zhong Y, Rice KA, Zhou Y, et al. Maternally expressed gene 3, an imprinted noncoding RNA gene, is associated with meningioma pathogenesis and progression. Cancer Res. 2010;70:2350–8. doi: 10.1158/0008-5472.CAN-09-3885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perry A, Banerjee R, Lohse CM, Kleinschmidt-DeMasters BK, Scheithauer BW. A role for chromosome 9p21 deletions in the malignant progression of meningiomas and the prognosis of anaplastic meningiomas. Brain Pathol. 2002;12:183–90. doi: 10.1111/j.1750-3639.2002.tb00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kamnasaran D, Qian B, Hawkins C, Stanford WL, Guha A. GATA6 is an astrocytoma tumor suppressor gene identified by gene trapping of mouse glioma model. Proc Natl Acad Sci U S A. 2007;104:8053–8. doi: 10.1073/pnas.0611669104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bigner SH, Mark J, Bigner DD. Cytogenetics of human brain tumors. Cancer Genet Cytogenet. 1990;47:141–54. doi: 10.1016/0165-4608(90)90024-5. [DOI] [PubMed] [Google Scholar]
- 42.Markert JM, Fuller CM, Gillespie GY, Bubien JK, McLean LA, Hong RL, et al. Differential gene expression profiling in human brain tumors. Physiol Genomics. 2001;5:21–33. doi: 10.1152/physiolgenomics.2001.5.1.21. [DOI] [PubMed] [Google Scholar]
- 43.Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403:503–11. doi: 10.1038/35000501. [DOI] [PubMed] [Google Scholar]
- 44.Lal A, Lash AE, Altschul SF, Velculescu V, Zhang L, McLendon RE, et al. A public database for gene expression in human cancers. Cancer Res. 1999;59:5403–7. [PubMed] [Google Scholar]
- 45.Scherf U, Ross DT, Waltham M, Smith LH, Lee JK, Tanabe L, et al. A gene expression database for the molecular pharmacology of cancer. Nat Genet. 2000;24:236–44. doi: 10.1038/73439. [DOI] [PubMed] [Google Scholar]
- 46.Michiels EM, Oussoren E, Van Groenigen M, Pauws E, Bossuyt PM, Voûte PA, et al. Genes differentially expressed in medulloblastoma and fetal brain. Physiol Genomics. 1999;1:83–91. doi: 10.1152/physiolgenomics.1999.1.2.83. [DOI] [PubMed] [Google Scholar]
- 47.Nagarajan RP, Costello JF. Molecular epigenetics and genetics in neuro-oncology. Neurotherapeutics. 2009;6:436–46. doi: 10.1016/j.nurt.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Costello JF, Berger MS, Huang HS, Cavenee WK. Silencing of p16/CDKN2 expression in human gliomas by methylation and chromatin condensation. Cancer Res. 1996;56:2405–10. [PubMed] [Google Scholar]
- 49.De Smet C, De Backer O, Faraoni I, Lurquin C, Brasseur F, Boon T. The activation of human gene MAGE-1 in tumor cells is correlated with genome-wide demethylation. Proc Natl Acad Sci U S A. 1996;93:7149–53. doi: 10.1073/pnas.93.14.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Herholz K, Langen KJ, Schiepers C, Mountz JM. Brain tumors. Semin Nucl Med. 2012;42:356–70. doi: 10.1053/j.semnuclmed.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kheirollahi M, Mehr-Azin M, Kamalian N, Mehdipour P. Expression of cyclin D2, P53, Rb and ATM cell cycle genes in brain tumors. Med Oncol. 2011;28:7–14. doi: 10.1007/s12032-009-9412-8. [DOI] [PubMed] [Google Scholar]
- 52.Mehdipour P, Kheirollahi M, Mehrazin M, Kamalian N, Atri M. Evolutionary hypothesis of telomere length in primary breast cancer and brain tumour patients: A tracer for genomic-tumour heterogeneity and instability. Cell Biol Int. 2011;35:915–25. doi: 10.1042/CBI20100560. [DOI] [PubMed] [Google Scholar]
- 53.Langford LA, Piatyszek MA, Xu R, Schold SC, Jr, Shay JW. Telomerase activity in human brain tumours. Lancet. 1995;346:1267–8. doi: 10.1016/s0140-6736(95)91865-5. [DOI] [PubMed] [Google Scholar]
- 54.Kheirollahi M, Mehrazin M, Kamalian N, Mohammadi-asl J, Mehdipour P. Telomerase activity in human brain tumors: Astrocytoma and meningioma. Cell Mol Neurobiol. 2013;33:569–74. doi: 10.1007/s10571-013-9923-x. [DOI] [PubMed] [Google Scholar]
- 55.Falchetti ML, Pallini R, Larocca LM, Verna R, D’Ambrosio E. Telomerase expression in intracranial tumours: Prognostic potential for malignant gliomas and meningiomas. J Clin Pathol. 1999;52:234–6. doi: 10.1136/jcp.52.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hiyama E, Hiyama K. Telomere and telomerase in stem cells. Br J Cancer. 2007;96:1020–4. doi: 10.1038/sj.bjc.6603671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kheirollahi M, Mehrazin M, Kamalian N, Mehdipour P. Alterations of telomere length in human brain tumors. Med Oncol. 2011;28:864–70. doi: 10.1007/s12032-010-9506-3. [DOI] [PubMed] [Google Scholar]
- 58.Lawler SE, Peruzzi PP, Chiocca EA. Genetic strategies for brain tumor therapy. Cancer Gene Ther. 2006;13:225–33. doi: 10.1038/sj.cgt.7700886. [DOI] [PubMed] [Google Scholar]
- 59.Söling A, Rainov NG. Bioluminescence imaging in vivo-application to cancer research. Expert Opin Biol Ther. 2003;3:1163–72. doi: 10.1517/14712598.3.7.1163. [DOI] [PubMed] [Google Scholar]
- 60.Chiocca EA, Broaddus WC, Gillies GT, Visted T, Lamfers ML. Neurosurgical delivery of chemotherapeutics, targeted toxins, genetic and viral therapies in neuro-oncology. J Neurooncol. 2004;69:101–17. doi: 10.1023/b:neon.0000041874.02554.b3. [DOI] [PubMed] [Google Scholar]
- 61.Tai CK, Wang WJ, Chen TC, Kasahara N. Single-shot, multicycle suicide gene therapy by replication-competent retrovirus vectors achieves long-term survival benefit in experimental glioma. Mol Ther. 2005;12:842–51. doi: 10.1016/j.ymthe.2005.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Qualman SJ, France M, Grizzle WE, LiVolsi VA, Moskaluk CA, Ramirez NC, et al. Establishing a tumour bank: Banking, informatics and ethics. Br J Cancer. 2004;90:1115–9. doi: 10.1038/sj.bjc.6601678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morente MM, Alonso S. Current challenges of human tumour banking. Hematol Oncol. 2005;23:54–6. doi: 10.1002/hon.749. [DOI] [PubMed] [Google Scholar]
- 64.Kheirollahi M, Khalaj Z, Nazem-Roaia F, Dashti S, Khorvash F, Kazemi M. Establishing a tumor bank and challenges [Google Scholar]


