ABSTRACT
The Ebola virus (EBOV) surface glycoprotein (GP1,2) mediates host cell attachment and fusion and is the primary target for host neutralizing antibodies. Expression of GP1,2 at high levels disrupts normal cell physiology, and EBOV uses an RNA-editing mechanism to regulate expression of the GP gene. In this study, we demonstrate that high levels of GP1,2 expression impair production and release of EBOV virus-like particles (VLPs) as well as infectivity of GP1,2-pseudotyped viruses. We further show that this effect is mediated through two mechanisms. First, high levels of GP1,2 expression reduce synthesis of other proteins needed for virus assembly. Second, viruses containing high levels of GP1,2 are intrinsically less infectious, possibly due to impaired receptor binding or endosomal processing. Importantly, proteolysis can rescue the infectivity of high-GP1,2-containing viruses. Taken together, our findings indicate that GP1,2 expression levels have a profound effect on factors that contribute to virus fitness and that RNA editing may be an important mechanism employed by EBOV to regulate GP1,2 expression in order to optimize virus production and infectivity.
IMPORTANCE The Ebola virus (EBOV), as well as other members of the Filoviridae family, causes severe hemorrhagic fever that is highly lethal, with up to 90% mortality. The EBOV surface glycoprotein (GP1,2) plays important roles in virus infection and pathogenesis, and its expression is tightly regulated by an RNA-editing mechanism during virus replication. Our study demonstrates that the level of GP1,2 expression profoundly affects virus particle production and release and uncovers a new mechanism by which Ebola virus infectivity is regulated by the level of GP1,2 expression. These findings extend our understanding of EBOV infection and replication in adaptation of host environments, which will aid the development of countermeasures against EBOV infection.
INTRODUCTION
The Ebola virus (EBOV), a member of the order of enveloped viruses Mononegavirales, is the etiologic agent of Ebola hemorrhagic fever (EHF), a highly lethal disease with up to 90% mortality (1). The EBOV surface glycoprotein (GP1,2) is the virion structural component that mediates attachment to and fusion with host cells. EBOV GP1,2 is a type 1 transmembrane protein that is presented on the virion envelope as a homotrimeric spike, similar to HIV Env and influenza virus hemagglutinin (HA) (2). Also like Env and HA, EBOV GP1,2 is first translated as a preprotein (GP0), which is then cleaved into two disulfide-linked subunits (GP1,2) in the Golgi complex by the protease furin (3). The N-terminal GP1 subunit has a mass of over 150 kDa and contains a putative receptor binding domain (RBD) as well as a highly glycosylated mucin-like domain, while the C-terminal GP2 has a mass of roughly 20 kDa and contains the fusion machinery as well as the transmembrane anchor. It is thought that EBOV GP1,2 mediates initial attachment to host cells by binding to lectins such as DC-SIGN, L-SIGN, and hMGL (4–6). These initial attachment events are followed by internalization of the virus via macropinocytosis and trafficking of virus-containing macropinosomes to the endolysosomal pathway (7–9). Within the acidified endosome, GP1 is digested by the cysteine proteases cathepsins B and L, which cleave off the mucin-like domain as well as other regions of GP1, producing a 20-kDa core and exposing the putative receptor binding domain (7, 10, 11). Binding of the RBD to a host receptor then triggers GP2 to insert its fusion loop into the host cell membrane, at which point a series of conformational changes bring the host and viral membranes together, resulting in fusion (12). While the definitive host receptor has not yet been determined, recent studies have identified the Niemann-Pick cholesterol transporter NPC1 as indispensable for the escape of virus from the acidified endosome following internalization (13–16).
EBOV GP1,2 is also an important virulence factor and has been implicated in many facets of EHF pathogenesis, including cytopathicity, endothelial dysfunction, and immune suppression (17, 18). Previous studies have indicated that EBOV GP1,2 is metabolically costly to synthesize and process and that high levels of GP1,2 expression are toxic to host cells (18, 19). While the exact mechanism of toxicity has been debated, it has been observed that overexpression of GP1,2 leads to cell rounding and detachment as well as loss of detection of some cell surface markers (20–22). Importantly, EBOV regulates GP1,2 expression via an RNA-editing mechanism whereby full-length GP1,2 mRNA is produced by slippage of the viral polymerase at an editing site (23, 24). Only around 20% of transcripts are edited, while unedited transcripts contain a premature stop codon and encode a truncated glycoprotein (sGP), which is secreted in large quantities by EBOV-infected cells. While the production of sGP has previously been implicated in modulation of host immunity (25–28), it is possible that RNA editing is also a mechanism by which EBOV could regulate expression of GP1,2 in order to moderate GP1,2-mediated toxicity. Indeed, recombinant EBOV in which the editing site was mutated to produce only GP1,2 exhibited enhanced cytopathicity and grew to much lower titers in cell culture than wild-type virus (19). It is therefore of significant importance to understand how regulation of GP1,2 expression by EBOV contributes to aspects of viral fitness such as infectivity, virus release, and immune evasion, as this information will help to elucidate how EBOV disseminates within a host and causes disease. Furthermore, a better understanding of how GP1,2 expression affects virus production and infectivity may enable us to identify vulnerabilities in the virus life cycle that can be targeted by vaccines and antivirals.
While a great deal of work has examined how modifications to EBOV GP1,2 affect its ability to mediate host cell attachment and fusion (5, 29, 30), there is little information on the effect of GP1,2 expression levels on virus production and infectivity. EBOV, like other members of Mononegavirales, employs a very simple regulatory mechanism for gene expression, in which the order of genes from 3′ to 5′ on the negative-sense genome largely dictates the level of each gene's expression (31). It has previously been shown that negative-strand RNA viruses are extremely sensitive to rearrangement of the gene order, indicating that the stoichiometry of protein expression has a profound effect on viral fitness (32, 33). However, few studies have directly examined the effect of glycoprotein expression on viral fitness. One such study used recombinant rabies viruses, in which the surface glycoprotein gene was codon optimized or deoptimized, to demonstrate that lowering glycoprotein expression levels adversely affects the kinetics of virus growth in vitro and pathogenicity in vivo (34). Considerable work has also been done regarding the mechanisms by which HIV and other retroviruses regulate Env expression, presumably to balance the generation of infectious virus while minimizing the immune profile of infected cells and progeny virions (35, 36). Two studies in particular demonstrated that very low levels of Env incorporation were sufficient to mediate infectivity, while increasing Env incorporation significantly enhanced infectivity until a plateau was reached (37, 38). These findings are consistent with the idea that because viral glycoproteins are primary targets for host antibodies, viruses must strike a fine balance between optimizing infectivity and evading host immunity. Importantly, EBOV GP1,2 has many properties that differentiate it from glycoproteins of other related viruses, including its cytotoxicity, its ability to bind to a nearly ubiquitously expressed host receptor, and the unique RNA editing mechanism that regulates its expression. Thus, it is of interest to better characterize how expression and incorporation of GP1,2 contribute to viral fitness.
In this study, we examined the effect of GP1,2 expression levels on production of Zaire EBOV (ZEBOV) virus-like particles (VLPs) as well as the infectivity of GP1,2-pseudotyped viruses. We demonstrate that high levels of GP1,2 expression impair both VLP production and pseudovirus infectivity and that expression of sGP may help to optimize virus production and infectivity by attenuating GP1,2 expression levels. We further examined how high levels of GP1,2 expression affect synthesis of other proteins, virus release, and specific infectivity of pseudoviruses. Additionally, we studied GP1,2 from several other filoviruses, as well as mucin-deleted and proteolyzed ZEBOV GP1,2, in order to identify the requirements for GP1,2-mediated regulation of virus production and infectivity.
MATERIALS AND METHODS
Cell lines and plasmids.
293T cells and JC53 cells were maintained in Dulbecco's modified Eagle's medium (DMEM; Mediatech) supplemented with 10% fetal bovine serum (FBS; HyClone; ThermoFisher) and penicillin-streptomycin. The primary Ebola glycoprotein construct used was wild-type Ebola virus strain Zaire (ZEBOV, subtype Mayinga; GenBank accession number U23187.1). Other filovirus GP1.2 constructs used were codon optimized and included Sudan ebolavirus (SEBOV; Gulu subtype; GenBank accession number AY316199.1), Marburg marburgvirus (MARV; Musoke subtype; GenBank accession number NC_001608.3), and Lloviu cuevavirus (LLOV; GenBank accession number NC_016144.1). Codon optimization was performed, and the genes were produced by Biomatik Corporation using proprietary technology. Other plasmids used include Ebola VP40 (ZEBOV, Mayinga subtype; GenBank accession number NC_002549.1) and HIV-1 Env (SF162 isolate; GenBank accession number EU123924.1). Additionally, we generated an Ebola VP40-GFP (where GFP is green fluorescent protein) fusion protein by fusing codon-optimized Pontellina plumata GFP (GenBank accession number AAQ01184) to the C-terminal end of EBOV VP40 as described previously (39). All constructs were subcloned into the pCAGGS.MCS mammalian expression vector. Plasmids were grown and purified using the EndoFree Plasmid Mega kit (Qiagen) as per manufacturer instructions, redissolved in pure endotoxin-free water at a concentration of 4 to 6 μg/μl, and purity verified by restriction analysis and spectrophotometry.
Pseudovirus generation and titration.
Glycoprotein-pseudotyped HIV was generated as described elsewhere (40). Briefly, 90% confluent 293T cells in 6-well plates were cotransfected with 500 ng of an Env-defective HIV backbone (SG3) DNA, as well as viral glycoprotein DNA in pCAGGS vector (in amounts varying between 4 μg and 4 ng). Unless otherwise stated, the total DNA amount was brought to 5 μg per well by addition of empty pCAGGS vector. Fugene HD was used as the transfection reagent, and transfection complexes were generated in serum-free medium with 3 μl Fugene HD per 1 μg DNA. Supernatants were harvested 48 h posttransfection, clarified, and filtered using a 0.45-μm filter. The titers of the pseudoviruses were determined by infecting JC53 cells (41), which express β-galactosidase and luciferase under a tat-activated promoter. A standard curve was generated by diluting a standard virus and comparing β-galactosidase staining (which requires visual counting of individual blue plaques) with luciferase activity (as measured by a luminometer). Luciferase activity measured from cells infected with pseudovirus was then converted to PFU/ml using a standard curve. Pseudoviruses pelleted through a 20% sucrose cushion demonstrated infectivity levels similar to those determined directly from producer cell supernatant. Thus, all titration experiments reported were performed with cell supernatant unless otherwise stated.
p24 ELISA.
p24 was measured in supernatant and cell lysate of producer cells using a p24 sandwich enzyme-linked immunosorbent assay (ELISA) kit (ABL Inc.). Supernatant was diluted between 1:1,000 and 1:10,000 in DMEM–10% FBS. Cell lysate was collected by lysis with ice-cold radioimmunoprecipitation assay (RIPA) buffer, followed by centrifugation at 20,000 × g for 15 min at 4°C. Lysate was collected and normalized for β-actin using a β-actin sandwich ELISA kit (Signosis). Lysate was then diluted in DMEM–10% FBS. Diluted samples were analyzed by ELISA as per manufacturer instructions.
EBOV virus-like particle generation and analysis.
EBOV VLPs were generated by cotransfection of 293T cells with 100 ng VP40 DNA plus various amounts of EBOV GP1,2 DNA. VP40-GFP VLPs were generated with 100 ng of VP40-GFP DNA instead of VP40 DNA. Total DNA transfected per well was normalized to 5 μg with empty pCAGGS plasmid. Supernatants were harvested 48 h posttransfection, clarified, and filtered using a 0.45-μm filter. Cell lysates were collected by lysis with ice-cold RIPA buffer, followed by centrifugation at 20,000 × g for 15 min at 4°C. Lysate was normalized for β-actin using a sandwich ELISA kit (Signosis). Cell culture supernatant and cell lysate were run on SDS-PAGE under denaturing conditions and analyzed by Western blotting using a polyclonal rabbit antibody that recognizes EBOV GP1,2 and VP40.
Fluorescence microscopy and flow cytometry of VLP and pseudovirus producer cells.
For analysis of VP40-GFP VLP producer cells, cells were fixed at 48 h posttransfection in 0.1% paraformaldehyde and stained for ZEBOV GP1,2 using mouse polyclonal anti-GP1,2 antisera, followed by incubation with tetramethyl rhodamine isocyanate (TRITC)-conjugated anti-mouse antibody (Southern Biotech). Confocal fluorescence micrographs were captured using an LSM 510 (Carl Zeiss) laser scanning microscope (LSM). LSM software was used for three-dimensional (3D) reconstruction of z-stacked images.
For analysis of EBOV GP1,2 pseudovirus producer cells cotransfected with GFP DNA, cells were visualized at 48 h posttransfection using a Nikon Eclipse TE200 microscope and photographed. Cells were then treated with 20 mM EDTA, collected, and stained for ZEBOV GP1,2 using mouse polyclonal anti-GP1,2 antisera, followed by incubation with a phycoerythrin (PE)-conjugated anti-mouse antibody (Sigma). Cells were then analyzed for GP1,2 and GFP expression by flow cytometry using an Accuri C6 flow cytometer (BD). Live, single cells were gated by forward and side scatter, and GP1,2 and GFP expressions were recorded as mean fluorescence intensity (MFI) of gated cells.
Trypsinization of VLP and pseudovirus producer cells.
293T cells producing either GP1,2-pseudotyped viruses or EBOV VLPs were washed twice in phosphate-buffered saline (PBS) (without Ca2+/Mg2+) and then trypsinized for 10 min with 200 μl of 0.25% Trypsin–0.05% EDTA in PBS (without Ca2+/Mg2+). Trypsinization was stopped by addition of DMEM–10% FBS, at which point the supernatant was separated from cells by centrifugation and collected for p24 ELISA or for SDS-PAGE and Western blot analysis.
Thermolysin treatment of pseudoviruses.
Lyophilized thermolysin (Sigma) was dissolved to 1 mg/ml in 50 mM Tris–0.5 mM CaCl2. Thermolysin was then mixed 1:1 with pseudovirus-containing supernatant and incubated at 37° for 5 min. Digestion was stopped with 20 mM EDTA, at which point viruses were titrated for infectivity on JC53 cells or denatured and run on SDS-PAGE for Western blot analysis.
Real-time RT-PCR analysis.
RNA isolation and reverse transcription (RT) were performed as previously described (42). Quantitative real-time PCR was performed by using a CFX96 thermal cycler (Bio-Rad, Hercules, CA) and measuring the SYBR green incorporation into double-stranded amplicons. Reactions were performed with 25-μl volumes containing forward and reverse primers at a final concentration of 100 nM. Primer sequences were as follows: VP40 forward primer, 5′-AGGCTTTCCTCCAGGAGTTC-3′; VP40 reverse primer, 5′-TGGTTGGGTGATCAGTTTGA-3′; GP1,2 forward primer, 5′-TTGTCAATGCTCAACCCAAA-3′; and GP1,2 reverse primer, 5′-TATGGTATCCAGGCCAGTCC-3′. The PCR conditions included a denaturing step at 95°C for 3 min followed by 45 cycles of a two-step cycling reaction as follows: 95°C for 10 s and then 54.4°C for 30 s. Melt curve analysis revealed a single peak for each primer set. Normalized expression levels of steady-state mRNA levels were calculated using the threshold cycle (ΔΔCT) mode within the gene expression module of CFX Manager 3.1 software (Bio-Rad, Hercules, CA) and were normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH) and adjusted for individual primer efficiencies calculated using a standard curve with known amounts of plasmid DNA containing these sequences.
RESULTS
High levels of GP1,2 expression result in lower titers of infectious pseudovirus.
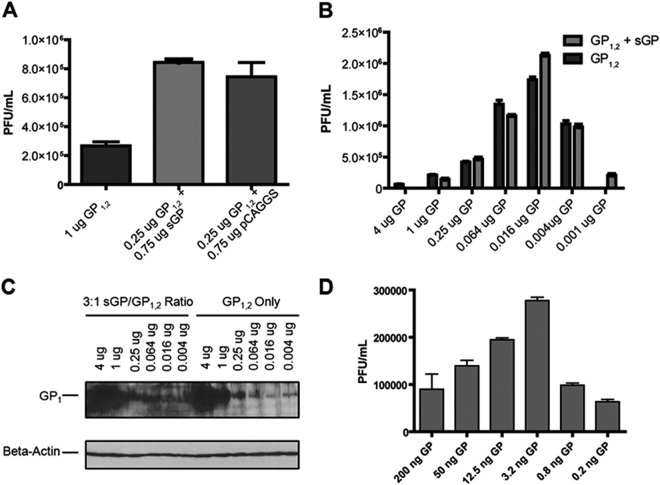
One unique feature of Ebola viruses is that the expression of EBOV GP1,2 is tightly regulated through RNA editing of the GP gene. We have previously shown that RNA editing and sGP production may be important in evading host immunity. In this study, we further investigated whether these mechanisms may also serve to regulate virus production and infectivity. We generated GP1,2-pseudotyped viruses using envelope-defective HIV-1 (SG3), by transfection of 293T cells with a fixed amount of SG3 HIV core DNA plus either 1 μg of GP1,2 DNA alone or 0.25 μg of GP1,2 DNA with 0.75 μg of sGP DNA, in order to recapitulate the ratio of GP isoforms produced during natural infection. As a control, we also generated viruses with 0.25 μg of GP1,2 plus 0.75 μg of empty pCAGGS plasmid. Pseudovirus-containing supernatants were collected at 48 h posttransfection, and infectivity was measured in JC53 cells by both β-galactosidase staining and luciferase assay. Surprisingly, viruses generated by coexpression of sGP and GP1,2 (sGP+GP1,2) displayed roughly 3-fold-higher infectivity than viruses generated with GP1,2 only (Fig. 1A). Furthermore, sGP+GP1,2 viruses demonstrated infectivity almost identical to that of viruses produced by transfection with GP1,2 DNA plus empty pCAGGS vector, indicating that the enhancement of infectivity was due more to the absence of GP1,2 than to the coexpression of sGP.
FIG 1.
Effects of coexpressing sGP with GP1,2 on production of infectious pseudovirus. (A) Pseudovirus infectivity titers. 293T cells were transfected with 500 ng of plasmid encoding HIVΔEnv (SG3) backbone and either 1 μg of GP1,2 DNA or 0.25 μg GP1,2 DNA plus 0.75 μg sGP DNA. A control well was transfected with 0.25 μg GP1,2 DNA plus 0.75 μg empty pCAGGS vector. Infectivity titers were measured at 48 h posttransfection by luciferase assay and converted to PFU/ml as described in Materials and Methods. Results reported are representative of those obtained in three separate experiments and are the means and standard deviations for samples run in triplicate. (B) Effects of varying GP1,2 expression on pseudovirus infectivity. Pseudoviruses were generated as described for panel A, except that the amount of transfected GP DNA varied from 4 μg to 4 ng. GP1,2+sGP pseudoviruses (light gray) were generated with a 3:1 ratio of sGP to GP1,2 DNA, while GP1,2 pseudoviruses (dark gray) were generated with only GP1,2 DNA. Infectivity titers were measured at 48 h posttransfection. (C) Levels of GP1,2 expression by transfection with different amounts of GP1,2 DNA. 293T cells were transfected with 500 ng of plasmid encoding HIVΔEnv (SG3) backbone together with different amounts of GP1,2 DNA only or GP1,2+sGP at a 3:1 ratio of sGP to GP1,2 DNA, varying from 4 μg to 4 ng as described for panel B. Cell lysate was harvested at 48 h posttransfection, normalized for β-actin, and analyzed by Western blotting using polyclonal rabbit antiserum against EBOV (top panel) or a mouse monoclonal antibody against β-actin (bottom panel). (D) Reduction of total transfected DNA. Pseudoviruses were generated by transfecting 293T cells with 25 ng of plasmid encoding HIVΔEnv (SG3) backbone plus GP1,2 DNA. GP1,2 DNA was varied from 200 ng to 0.2 ng, and infectivity was measured at 48 h posttransfection by luciferase assay and converted to PFU/ml as described in Materials and Methods.
To extend our findings, we determined how GP1,2 expression levels affected the production of infectious pseudoviruses. We generated a panel of GP1,2-pseudotyped viruses, varying the amount of transfected GP1,2 DNA over a 1,000-fold range while keeping the amount of the SG3 backbone DNA constant. In parallel, pseudoviruses were also generated with a 1:3 ratio of GP1,2 to sGP DNA. Unexpectedly, infectious titers of GP1,2-pseudotyped viruses were maximal using 16 ng of transfected GP1,2 DNA (Fig. 1B). When GP1,2 DNA was increased 256-fold to 4 μg, titers of the resulting pseudoviruses dropped by a factor of over 25. Virus infectivity also dropped when GP1,2 transfection was reduced below 16 ng of DNA. Interestingly, when matched levels of transfected GP1,2 DNA were used, viruses generated from sGP+GP1,2-expressing cells displayed infectivity virtually identical to that of viruses generated with GP1,2 DNA alone. Western blot analysis showed that the level of GP1,2 expression correlated with the amount of GP1,2 plasmid DNA used in transfection and was not affected by cotransfection with sGP plasmid DNA (Fig. 1C). Taken together, these data indicate that high levels of GP1,2 expression significantly impair the production of infectious pseudovirions. Furthermore, the ability of sGP coexpression to rescue production of infectious pseudovirus results from the reduction of GP1,2 expression rather than sGP-mediated enhancement of infectivity.
We further investigated the impact of GP expression levels on pseudovirus production using reduced levels of total DNA to mimic initial stages of virus replication, when viral protein levels are low. We generated pseudoviruses using 1/20 of the total DNA used in the above pseudovirus experiments (0.25 μg DNA/well) while keeping the ratios of SG3 to GP1,2 DNA the same. As shown in Fig. 1D, infectious titers of pseudoviruses were maximal using 3.2 ng of transfected GP1,2 DNA, while increasing or decreasing transfected GP1,2 DNA significantly decreased pseudovirus production. This result indicates that the ratio of GP1,2 to SG3 core expression levels has a greater impact on virus infectivity than does the absolute level of GP1,2 expression.
GP1,2 expression levels in different filovirus species have a similar effect on virus production and infectivity.
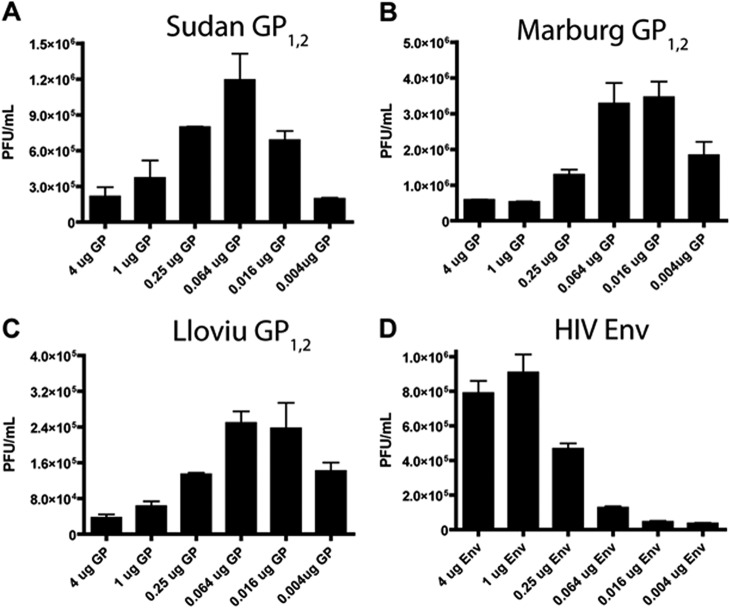
In order to determine if impaired infectious virus production under conditions of high GP1,2 expression is a common feature of other filoviruses, we generated pseudoviruses with GP1,2 from several different filovirus species. The pseudoviruses generated with all filovirus glycoproteins tested exhibited a similar infectivity pattern, in which infectivity was maximized at an intermediate level of glycoprotein expression, while increasing or decreasing GP1,2 DNA from this optimal level significantly decreased infectious pseudovirus titers (Fig. 2A to C). Interestingly, the maximum infectivity titer varied among pseudoviruses generated with different glycoproteins, with Lloviu cuevavirus (LLOV) GP1,2 exhibiting the lowest peak infectivity, and Marburg virus (MARV) GP1,2 exhibiting the highest. We were interested to know if the infectivity pattern that we observed with titration of filovirus GP1,2 expression levels also held true for glycoproteins from an unrelated virus. To address this, we generated pseudoviruses with HIV Env and determined their infectivity. In marked contrast to filovirus GP1,2-pseudotyped viruses, Env-pseudotyped viruses yielded the highest titers with the highest levels of Env plasmid transfection, while decreasing amounts of Env-encoding DNA dramatically decreased infectious virus production. These data demonstrate that impaired production of infectious virus at high glycoprotein expression levels is a phenomenon exhibited by filoviruses but is not shared with other enveloped viruses.
FIG 2.
Effects on pseudovirus infectivity of variation in glycoprotein expression levels for different filovirus strains as well as for HIV Env. (A to D) 293T cells were cotransfected with 500 ng of plasmid encoding HIVΔEnv (SG3) backbone plus plasmids encoding GP1,2 from Sudan ebolavirus (A), Marburg virus (B), Lloviu cuevavirus (C), or HIV Env (SF162) (D). The amounts of glycoprotein-encoding DNA plasmids varied from 4 μg to 4 ng, and infectivity was measured at 48 h posttransfection by luciferase assay and converted to PFU/ml as described in Materials and Methods. Results reported are representative of those obtained in three separate experiments and are the means and standard deviations for samples run in triplicate.
In order to elucidate the mechanism by which high EBOV GP1,2 expression reduces the production of infectious virus, we measured supernatant p24 levels by ELISA in the GP1,2- and HIV Env-pseudotyped viruses and calculated “specific infectivity” for both GP1,2- and HIV Env-pseudotyped viruses, which was defined as PFU per pg p24. Surprisingly, GP1,2-pseudotyped viruses generated at high levels of GP1,2 expression (4 μg and 1 μg of GP1,2 DNA) demonstrated a 10-fold decrease in specific infectivity compared to viruses generated with 16 ng GP1,2 DNA (Fig. 3). In contrast, HIV Env-pseudotyped viruses displayed the highest specific infectivity under conditions of high Env expression. This finding indicates that even when correcting for impaired pseudovirus production and release under conditions of high EBOV GP1,2 expression, pseudoviruses containing high levels of GP1,2 are intrinsically less infectious than their low-GP1,2-containing counterparts. Importantly, this pattern does not hold true for HIV Env.
FIG 3.
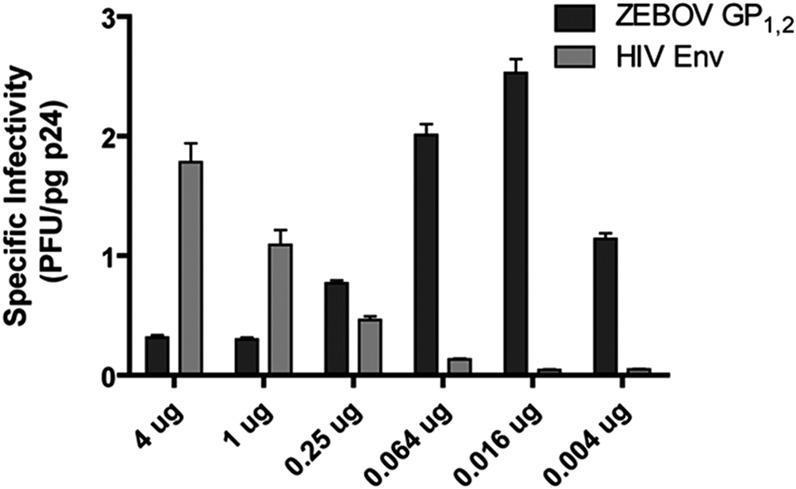
Effects of glycoprotein expression levels on specific infectivity of EBOV GP1,2 and HIV Env-pseudotyped viruses. 293T cells were cotransfected with 500 ng of plasmid encoding HIVΔEnv (SG3) backbone plus plasmids encoding GP1,2 from Zaire ebolavirus or HIV Env (SF162). The amounts of glycoprotein-encoding DNA plasmids varied from 4 μg to 4 ng, and pseudovirus infectivity in supernatant was measured at 48 h posttransfection by luciferase assay and converted to PFU/ml as described in Materials and Methods. In parallel, the level of p24 in supernatant was determined by a sandwich ELISA. Based on the obtained results, the specific infectivity of EBOV GP1,2 as well as HIV Env-pseudoviruses, defined as PFU/pg p24, was calculated and plotted versus the amount of transfected GP1,2 or HIV Env DNA, respectively.
High levels of EBOV GP1,2 expression impair production of EBOV virus-like particles.
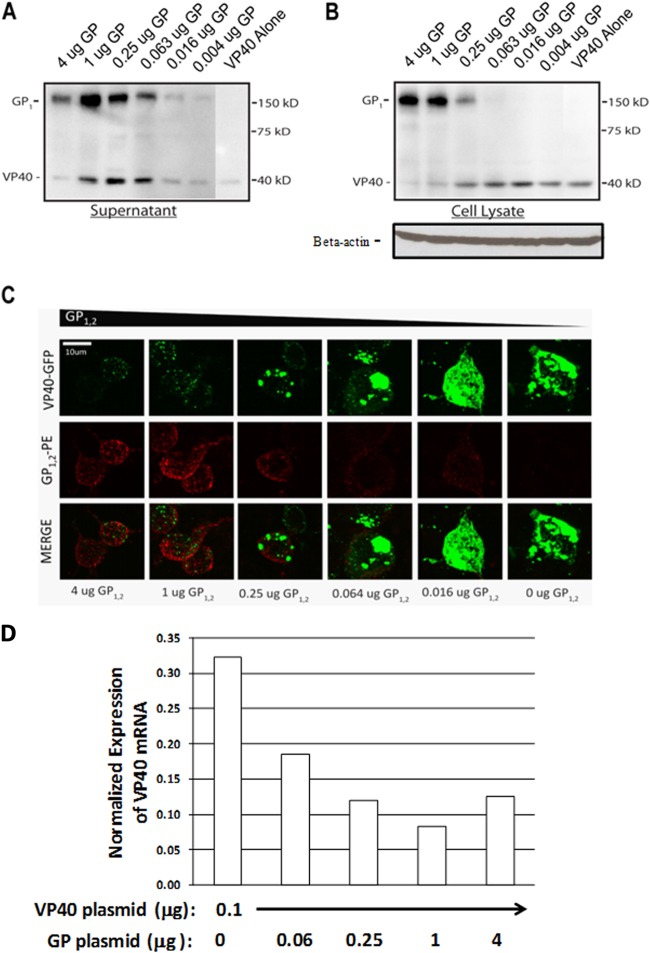
While our data clearly demonstrate that high levels of EBOV GP1,2 expression impair production of infectious pseudovirus, we also wanted to determine whether this effect also held true for EBOV virus-like particles. We generated EBOV VLPs by cotransfecting 293T cells with plasmids encoding ZEBOV GP1,2 as well as ZEBOV VP40, the primary EBOV matrix protein. We varied the amount of transfected GP1,2 DNA over a 1,000-fold range while keeping the amount of VP40 DNA constant. VLPs and cell lysates were collected at 48 h and analyzed by Western blotting. Consistent with the results of our pseudovirus experiments, high expression levels of GP1,2 resulted in drastic attenuation of VLP release into the supernatant as well as VP40 present in the cell lysate (Fig. 4A and B). Interestingly, moderate levels of GP1,2 expression resulted in increased release of VP40 into the supernatant compared to very low levels of GP1,2, a finding consistent with the previously published observation that GP1,2 enhances EBOV virion budding (43). Unexpectedly, the highest level of GP1,2 expression also appeared to drastically decrease levels of GP1,2 in the supernatant, indicating that GP1,2 overexpression may impair proper release or processing of GP1,2 or may otherwise interfere with virion budding. Under these conditions, large amounts of GP1,2 accumulated in the cell lysate (Fig. 4B).
FIG 4.
High levels of GP1,2 expression impair EBOV VLP production. (A, B) Production of EBOV VLPs with various GP1,2 expression levels. 293T cells were transfected with 100 ng of EBOV VP40 DNA plus various amounts of GP1,2 DNA (4 μg to 4 ng). Supernatant (A) and cell lysate (B) were assayed by Western blotting at 48 h posttransfection using polyclonal rabbit antiserum recognizing all Zaire EBOV proteins (tops of panels) or a mouse monoclonal antibody against β-actin (bottom of panel B). (C) Fluorescence microscopy of EBOV VLP-producing cells. 293T cells were transfected with 100 ng of VP40-GFP fusion protein DNA, plus various amounts of GP1,2 DNA (4 μg to 16 ng). At 48 h posttransfection, cells were fixed and stained for GP1,2 using mouse anti-GP1,2 immune sera, followed by a PE-conjugated anti-mouse antibody. Cells were then visualized by fluorescence microscopy for GP1,2 (PE, in red) and VP40 (GFP, in green). Scale bar, 10 μm. (D) Coexpression of GP1,2 reduces VP40 mRNA levels. 293T cells were transfected with VP40 DNA and GP1,2 DNA at the amounts indicated along the x axis. At 48 h following transfection, steady-state levels of VP40 mRNA were measured using quantitative real-time RT-PCR. The y axis represents normalized expression levels of VP40 relative to GAPDH. The results from one of two independent experiments are shown.
In order to visualize the coexpression of VP40 and GP1,2 within VLP producer cells, we transfected cells as described above and substituted wild-type VP40 with a VP40-GFP fusion protein that was previously demonstrated to generate VLPs morphologically similar to those produced with wild-type VP40 (44). At 48 h, cells were stained and visualized by confocal microscopy. We observed that high levels of GP1,2 expression resulted in reduced expression VP40-GFP, similar to what is shown by Western blotting in Fig. 4B. To further investigate the effect of GP1,2 on VP40 expression, we determined the levels of VP40 mRNA in cells that were transfected with VP40 DNA along with different amounts of GP1,2 DNA. As shown in Fig. 4D, cotransfection with large amounts of GP1,2 DNA, at 1 or 4 μg, significantly reduced VP40 mRNA levels compared to cotransfection with small amounts of GP1,2 DNA, at 0.06 μg or no GP1,2, indicating that GP1,2 affects VP40 expression through decreasing the amount of VP40 mRNA transcription. Notably, we also observed that high levels of GP1,2 expression also resulted in a more punctate cytoplasmic distribution of VP40-GFP, whereas lower levels of GP1,2 expression resulted in significantly increased levels of VP40-GFP expression, which was localized to large regions near the periphery of the cell (Fig. 4C). Taken together, our findings indicate that high GP1,2 expression results both in decreased virion release and in decreased expression and altered distribution of the matrix protein VP40 within cells. This suggests that at least part of the mechanism by which high GP1,2 expression attenuates production of infectious virus operates by impairing the synthesis and assembly of other viral proteins.
Inhibition of protein synthesis by GP1,2.
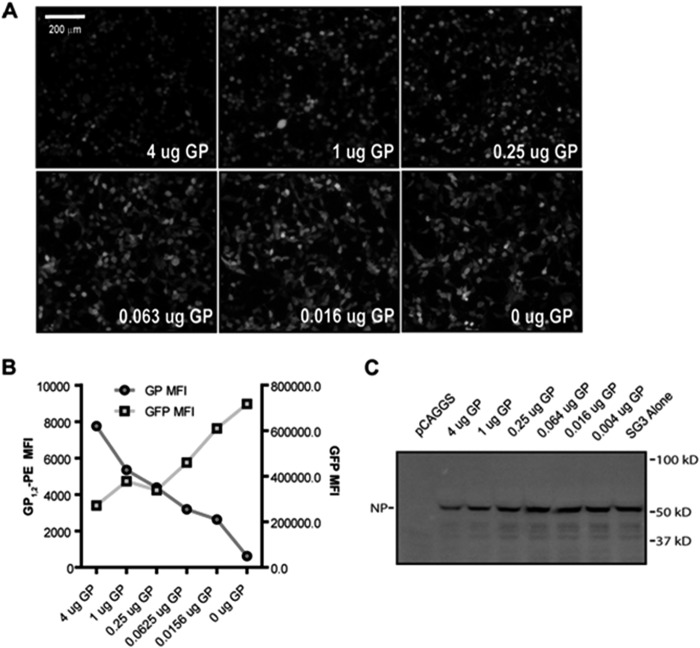
It has been previously suggested that EBOV GP1,2 is metabolically costly to synthesize and process and that overexpression of GP1,2 can overwhelm the protein-processing machinery of cells (19). Because high GP1,2 expression reduces intracellular levels of other viral proteins, it is possible that impaired protein synthesis may be partly responsible for decreased release and infectivity of viruses produced in cells expressing high levels of GP1,2. In order to test this hypothesis, we generated EBOV GP1,2-pseudotyped viruses as shown in Fig. 1, except that we also cotransfected cells with fixed amounts of plasmid encoding either GFP or influenza virus PR8 nucleoprotein (NP). We chose foreign, nonexported proteins instead of endogenous housekeeping proteins in order to mimic the kinetics of protein synthesis during viral infection. GFP-transfected cells expressing high levels of GP1,2 showed lower levels of GFP than those expressing low levels of GP1,2, as observed by fluorescence microscopy (Fig. 5A). Cells were collected at 48 h posttransfection and stained for surface GP1,2 expression and analyzed by flow cytometry. Consistent with previous results, surface GP1,2 MFI increased with the amount of transfected GP1,2 DNA, while GFP MFI decreased (Fig. 5B). Similar to GFP-transfected cells, cells transfected with large amounts of GP1,2 DNA also expressed lower levels of influenza NP intracellularly, while cells transfected with small amounts of GP1,2 DNA expressed higher levels of NP (Fig. 5C). These data indicate that EBOV GP1,2 impairs synthesis of other proteins, possibly contributing to decreased virus production and release under conditions of high GP1,2 expression.
FIG 5.
High levels of GP1,2 expression impair protein production. (A, B) Decreased GFP expression correlates with increased GP1,2 expression levels. 293T cells were transfected with 500 ng of a plasmid encoding HIVΔEnv (SG3) backbone and 100 ng of a plasmid encoding GFP, as well as various amounts of GP1,2 DNA (4 μg to 4 ng). (A) At 48 h posttransfection, cells were imaged by fluorescence microscopy to visualize GFP expression. Results are representative of those obtained in three separate experiments. (B) Cells were harvested by EDTA treatment and stained for surface GP1,2 expression using mouse anti-GP1,2 immune sera, followed by a PE-conjugated anti-mouse antibody. Cells were then analyzed by flow cytometry, and MFI was plotted for GP1,2 and GFP versus the amount of transfected GP1,2 plasmid. (C) 293T cells were transfected as described for panel A, except that instead of using GFP, cells were cotransfected with 100 ng of plasmid expressing PR8 influenza virus A nucleoprotein (NP). Cell lysate was harvested at 48 h posttransfection, normalized for β-actin, and analyzed by Western blotting using a mouse monoclonal anti-NP antibody.
High GP1,2 expression levels do not restrict virus budding.
In order to elucidate the mechanism of impaired virus production under conditions of high GP1,2 expression, we investigated whether high GP1,2 expression levels impaired the release of virus into the supernatant. It is known that GP1,2 mediates initial virus attachment to host cells by binding to lectins such as DC-SIGN. Thus, we hypothesized that nascent virions with higher GP1,2 content might be trapped at the cell surface by these interactions instead of escaping into the supernatant. To test this hypothesis, we generated pseudoviruses as previously described, except that after collecting the supernatant, cells were washed with EDTA, trypsinized, and then lysed. Analysis of p24 in each of these fractions revealed that high GP1,2 expression resulted in very little retention of p24 at the cell surface, while more p24 was retained under conditions of low GP1,2 expression (Fig. 6A). A similar pattern was observed with EBOV VLPs, in which higher levels of VP40 were liberated by trypsinization from low-GP1,2-expressing cells, while increasing GP1,2 expression resulted in reduced release of VP40 in the trypsinized fraction (Fig. 6B). Taken together, these data indicate that high levels of GP1,2 expression do not restrict virus release but that increased GP1,2 levels actually reduce retention of viruses at the cell surface. This finding is consistent with previously published studies in which EBOV GP was demonstrated to aid in budding of virus-like particles while antagonizing host factors that restrict release of virions (43, 44).
FIG 6.

High levels of GP1,2 expression do not restrict virus release from producer cells. (A) Levels of p24 liberated by EDTA treatment and by trypsinization. 293T cells were transfected with 500 ng of HIVΔEnv (SG3) backbone DNA and various amounts of GP1,2 DNA (4 μg to 0 ng). At 48 h posttransfection, supernatants were collected, at which points cells were washed and treated with 20 mM EDTA in PBS for 10 min at 37°C, followed by trypsinization for 5 min at 37°C. Trypsinized cells were then lysed, and cell lysate was collected. Supernatants, EDTA wash, trypsin fraction, and cell lysate were all analyzed in parallel for p24 content by ELISA. Lysate p24 levels reported were normalized for β-actin. Results are representative of those obtained in two separate experiments and are the means and standard deviations for samples run in triplicate. (B) Levels of VP40 liberated by trypsinization of EBOV VLP-producing cells. 293T cells were transfected with 100 ng of EBOV VP40 DNA plus various amounts of GP1,2 DNA (4 μg to 4 ng). At 48 h posttransfection, producer cells were trypsinized and the trypsinized fraction was analyzed by Western blotting using polyclonal rabbit anti-EBOV antiserum specific for all Zaire EBOV proteins.
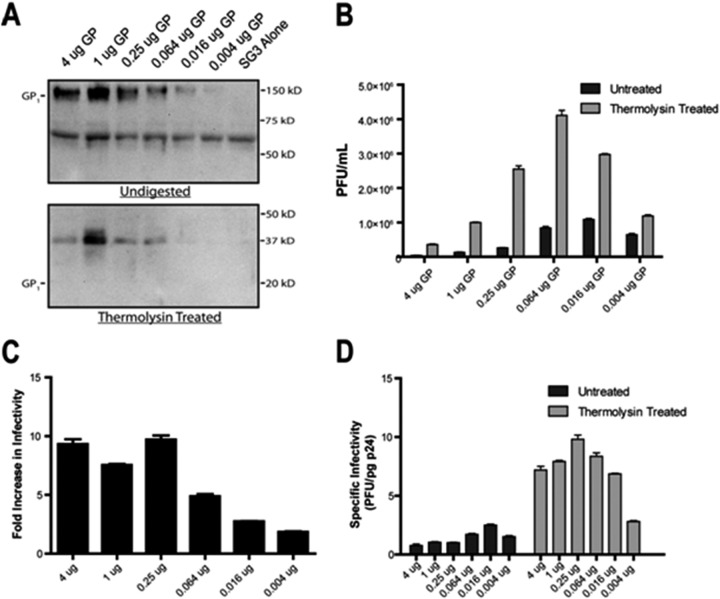
Infectivity of viruses containing high levels of GP1,2 can be enhanced by proteolysis.
As demonstrated above, pseudoviruses containing high GP1,2 levels exhibited 10-fold-lower specific infectivity (PFU/pg p24) than pseudoviruses containing lower levels of GP1,2. It has previously been determined that proteolysis of EBOV GP1,2 can enhance the binding and infectivity of pseudotyped viruses by removing regions of the glycoprotein that may interfere with optimal attachment to host cells (45). Thus, we hypothesized that the density of GP1,2 expression also might have an effect on optimal binding to host cells and that proteolysis would differentially enhance the infectivity of high- versus low-GP1,2-containing viruses. To test this hypothesis, ZEBOV GP1,2-pseudotyped viruses were digested with thermolysin, a protease that has previously been demonstrated to cleave GP1 and enhance infectivity in a manner similar to that of cathepsins B and L (11, 45, 46). Viruses were digested for 5 min and analyzed by SDS-PAGE, which revealed proteolysis of GP1 from 150 kDa to a 37-kDa intermediate (Fig. 7A). Digested viruses were then titrated for infectivity alongside untreated viruses. Thermolysin treatment enhanced virus infectivity for all viruses regardless of GP1,2 expression level (Fig. 7B). However, the infectivity of high-GP1,2-expressing viruses was enhanced by a factor of 10, while that of low-GP1,2-expressing viruses was enhanced by only a factor of 2 (Fig. 7C). Importantly, specific infectivity, as measured by PFU/pg p24, appeared to plateau for proteolyzed viruses, suggesting a theoretical upper limit for pseudovirus infectivity (Fig. 7D). Taken together, our data indicate that high GP1,2 content interferes with infectivity of viruses and that proteolysis of GP1,2 can rescue infectivity.
FIG 7.
Proteolysis of high-GP1,2-containing pseudoviruses enhances infectivity. (A) Thermolysin digestion of GP1,2. Released pseudoviruses were treated for 5 min at 37°C with 0.5 mg/ml thermolysin. Reactions were then terminated with protease inhibitor cocktail, and samples were analyzed by Western blotting using polyclonal rabbit anti-EBOV antiserum. Untreated pseudoviruses were also analyzed as a control. (B) Thermolysin-treated pseudoviruses were normalized for p24 content and then titrated on JC53 cells by luciferase assay, followed by conversion to PFU/ml as described in Materials and Methods. Treated viruses were titrated alongside untreated viruses as a control. Results reported are representative of those obtained from three separate experiments and are the means and standard deviations for samples run in triplicate. (C) The fold increase in infectivity of pseudoviruses with thermolysin treatment was calculated from the data reported in panel B and plotted versus amounts of transfected GP1,2 DNA. (D) Specific infectivity of untreated versus thermolysin-treated pseudoviruses. Based on results reported in panel B and supernatant p24 ELISA (data not shown), specific infectivity, defined as PFU/pg p24, was calculated for untreated versus thermolysin-treated pseudoviruses and plotted versus amounts of transfected GP1,2 DNA.
DISCUSSION
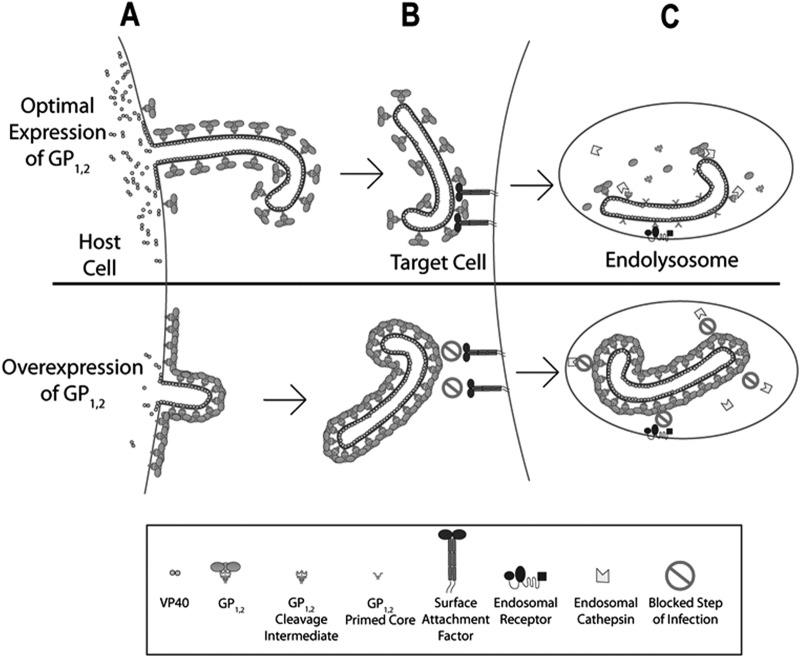
In this study, we investigated the effect that EBOV GP1,2 expression levels have on the production and infectivity of EBOV VLPs and pseudoviruses. We demonstrated that there is a low level of GP1,2 expression at which virus release and infectivity are maximized. Importantly, we observed that higher levels of GP1,2 expression can profoundly impair both the production of VLPs and the infectivity of pseudoviruses, indicating that tight regulation of GP1,2 expression is of critical importance to the EBOV life cycle. We further demonstrated that high GP1,2 expression levels impair production of VP40 required for viral assembly, through reducing the mRNA levels of coexpressed VP40. In addition, we observed that viruses containing large amounts of GP1,2 are intrinsically less infectious whereas proteolysis of these viruses with thermolysin can enhance infectivity, possibly by relieving the steric shielding resulting from dense packing of GP1,2 on the virus surface.
It has long been hypothesized that RNA editing and the production of sGP by EBOV-infected cells was a mechanism of host immune evasion. Indeed, sGP has been implicated in modulation of host immunity and in interference with the host antibody response (25–28). However, the present findings indicate that RNA editing may also be a mechanism of modulating GP1,2 expression levels to optimize virus production and infectivity. A recent study found that when serially passaged in vitro in Vero E6 cells, EBOV rapidly mutated the editing site of the GP gene to adopt a predominantly GP1,2-forming phenotype (47). The mutant virus rapidly reverted back to a predominantly sGP-forming phenotype when reintroduced to a naive guinea pig host. The fact that this reversion occurred within 6 days of infection suggests that adaptive immunity had little to do with this phenotypic transformation. Instead, it is possible that different host environments select for high-GP1,2- versus low-GP1,2-expressing viruses, depending on factors within that environment that restrict virus budding and dissemination. These factors may include tetherin expression (which restricts virus budding but is antagonized by GP1,2) as well as other interferon-inducible antiviral factors (44, 48, 49). It would be revealing to examine how passage in different cell types, as well as treatment with interferons or other inflammatory cytokines, affects the emergence of editing-site mutants.
GP1,2 has a variety of toxic effects on cells, including induction of cell rounding, detachment, and loss of detection of surface markers (18, 50). The exact mechanism of these effects has been debated. Some studies have indicated that GP1,2 induces active internalization of surface molecules required for attachment and communication with the immune system and also promotes cell death (51, 52). Other studies have suggested that GP1,2 sterically occludes surface factors without actually reducing cell viability (20, 53). In one study, it was reported that overexpression of GP1,2, through mutation of the GP editing site, resulted in enhanced cytopathicity, with the recombinant virus growing to lower infectivity titers (19). The authors noted the accumulation of incompletely processed GP1,2 in the endoplasmic reticulum (ER) and early Golgi cisternae and hypothesized that toxicity of high-GP1,2 expression was at least partly due to saturation of the protein-processing machinery. This hypothesis is consistent with our finding that high expression levels of GP1,2 resulted in reduced synthesis of other proteins required to assemble VLPs or pseudoviruses. Furthermore, GP1,2-mediated reduction in protein expression is not specific to exported viral proteins, since high GP1,2 expression levels also impaired production of nonexported proteins such as influenza virus NP and GFP. However, as shown in Fig. 5 for coexpression of GP and GFP, cells transfected with high GP DNA amounts showed lower GFP expression but no significant cell loss. We also stained 293T cells at 48 h by trypan blue and observed no difference in cell death rates for cells transfected with either high or small amounts of GP or no GP (data not shown). Further, at this time point (48 h posttransfection), very few detached cells were detected in the culture medium and the vast majority of the cells were still attached to the cell culture plate. Thus, these observations indicate that the drastic reduction of protein synthesis at high GP expression levels is not primarily a result of loss of cells by detachment and death under our experimental settings. Nonetheless, as illustrated in Fig. 8A, impaired protein synthesis represents one mechanism by which high levels of GP1,2 expression could reduce production of infectious virus. Future studies are needed to elucidate the exact mechanisms of impaired protein production as well as the specific features of GP1,2 required to mediate this effect.
FIG 8.
Proposed model for impairment of virus production and infectivity at high levels of GP1,2 expression. (A) Optimal levels of GP1,2 expression result in efficient production, trafficking, and assembly of other viral proteins such as VP40. Nascent virions bud efficiently from the host cell membrane, with optimal incorporation of GP1,2 peplomers. On the other hand, overexpression of GP1,2 results in impaired synthesis of other viral proteins. Thus, viruses do not efficiently assemble, and those viruses that do bud from the host cell contain very high levels of GP1,2. (B) Optimal levels of GP1,2 incorporation into virions result in proper engagement with target cell attachment factors and efficient virion internalization. High density of GP1,2 on the virion envelope results in steric shielding of domains that normally bind host cell surface factors, thus interfering with attachment and internalization of virus. (C) Optimal levels of GP1,2 incorporation allow endosomal cathepsins to properly process GP1,2 peplomers, generating the primed core capable of binding to the endosomal receptor and mediating fusion with the host membrane. In contrast, high levels of GP1,2 incorporation result in impaired endosomal processing. Unprocessed GP1,2 does not engage with the endosomal receptor and thus cannot mediate fusion with the host membrane, preventing viral egress from the acidified endosome.
A significant finding of this study is that, even when normalized for p24 content, high-GP1,2-containing viruses have lower specific infectivity than their low-GP1,2 counterparts. Because GP1,2 mediates viral attachment and fusion, it would be expected that higher GP1,2 expression levels should translate into higher efficiency of infection. Indeed, HIV Env-pseudotyped viruses with high Env content displayed much higher specific infectivity than those with low Env content, a finding consistent with previously published studies (37). However, GP1,2-pseudotyped viruses were maximally infectious at intermediate levels of GP1,2 expression, while increasing or decreasing GP1,2 expression levels from the optimal level resulted in drastic attenuation of infectivity. It is possible that a high density of GP1,2 interferes with proper GP1,2 function through steric hindrance, as depicted schematically in Fig. 8B and C. Packing of GP1,2 trimers at high density on the virion surface may result in enhanced shielding of GP1,2 receptor binding motifs, while a lower density of GP1,2 results in increased exposure of receptor binding motifs (Fig. 8B). Alternatively, as shown in Fig. 8C, steric shielding due to high GP1,2 density may also interfere with endosomal processing required for the final steps of infection (7, 10, 11). Either of these mechanisms is consistent with our observation that proteolytic processing of GP1,2 was able to rescue infectivity of high-GP1,2-containing viruses, and these two possible mechanisms are not mutually exclusive. In either case, these results suggest that high GP1,2 expression may reduce virus fitness through impairment of virus infectivity, and RNA editing may be a mechanism employed by Ebola virus to control GP1,2 expression levels for optimized replication.
Proteolysis may relieve steric hindrance resulting from GP1,2 packing, promoting more-efficient receptor binding and possibly obviating the need for endosomal proteolysis. This is similar to the way in which removal of the GP1 mucin domain also enhances infectivity by alleviating shielding of receptor binding epitopes and by enhancing attachment to host cells (45). Once proteolyzed, high-GP1,2-containing viruses actually have higher specific infectivity than their low-GP1,2 counterparts, indicating that GP1,2 generated under conditions of high expression is still intrinsically functional and that it is likely an effect of high density of GP1,2 on the virion surface that impairs proper function. Interestingly, it has been demonstrated that GP1,2 lacking a transmembrane domain (GP1,2ΔTM) is efficiently shed by host cells through cleavage by tumor necrosis factor alpha (TNF-α)-converting enzyme (TACE) at the membrane-proximal external region (54). Similar to the production of sGP, TACE-mediated secretion of GP1,2ΔTM has also been hypothesized to result in absorption of host anti-GP antibodies. In light of our present findings, it is also possible that gradual TACE-mediated cleavage of GP1,2 may enable the virus to modulate its infectivity by decreasing the surface density of GP1,2 on virions. Further, the proteolytic cleavage of GP1,2 may function as a timing mechanism to ensure that virions are less infectious when they first bud, to allow for efficient release, but have increased infectivity after release.
Our results demonstrate that the ratio between EBOV GP and viral core protein expression has an important impact on production of infectious virus pseudotype particles. Notably, this observation was made under both high and low total DNA transfection conditions (Fig. 1), indicating that regulation of GP expression levels may affect the infectivity of virus particles produced during early as well as late stages of virus replication, when viral protein expression levels differ. Of note, Marburg virus does not express sGP, and an early study showed that even a very small amount of Marburg virus GP DNA (0.01 μg) is sufficient to produce VLPs and maximum production of VLPs was observed by using 0.5 to 1 μg GP DNA (55). However, the effect of a further increase of GP DNA on VLP production was not investigated. Nonetheless, the results showed that increased Marburg virus GP expression resulted in reduced viral NP expression. In the present study, we also made similar observations for other filovirus species, including Sudan ebolavirus as well as Lloviu cuevavirus, indicating that the ratio between GP and viral core proteins may affect the production of virus particles with optimal infectivity for all filoviruses. How regulation of GP1,2 expression contributes to overall viral fitness remains a complex question. Viruses, including Ebola virus, do not necessarily evolve to optimize infectivity. Indeed, it has been previously demonstrated that single amino acid mutations, as well as deletions of regions of GP1,2, can significantly enhance infectivity of GP1,2-pseudotyped viruses (29). While it may seem intuitive that enhanced infectivity is synonymous with optimizing viral fitness, this is probably not the case, given that EBOV would have likely adopted these simple infectivity-enhancing mutations if they had conferred a selective advantage. Instead, it is possible that EBOV has evolved mechanisms such as steric shielding of receptor binding regions as well as regulation of glycoprotein expression levels to actively modulate infectivity. There are several possible arguments to support this hypothesis. First, moderation of infectivity may be necessary to facilitate effective dissemination of virus within the host. While viruses that exhibit low infectivity may be less efficient at finding and infecting host cells, viruses that bind very effectively to receptors may not be efficiently released from producer cells or may be unable to spread to distal locations. This is particularly important for viruses such as EBOV, which infect a wide range of host cell types and whose life cycle evolves rapidly when establishing a systemic infection. A second reason why infectivity may be sacrificed for increased viral fitness is due to host immune evasion. HIV expresses very low levels of Env to avoid immune detection (36). On the other hand, when expressed at sufficiently high levels, EBOV GP1,2 can shield cell surface molecules involved in immune recognition, as well as sensitive epitopes on GP1,2 itself (20, 53, 56). The density of GP1,2 required to mediate these effects is unknown, but it likely requires close packing of GP1,2 trimers to form a continuous glycan canopy. Finally, GP1,2 has been demonstrated to directly modulate host immunity through a variety of mechanisms. The GP2 subunit contains an immunosuppressive sequence similar to that of many retroviruses, which causes lymphocytes to downregulate markers of activation, inhibits elaboration of inflammatory cytokines, and even induces lymphocyte apoptosis (57, 58). Additionally, GP1,2 can antagonize the activity of tetherin (CD317), an interferon-induced molecule that normally prevents budding of enveloped viruses by “tethering” them to the cell surface (44). It appears that these immunomodulatory effects are dose dependent, though the expression levels of GP1,2 required for these effects are unknown.
Our findings, combined with previous studies of the role of EBOV GP1,2 in host immune evasion, argue for a model in which expression levels of GP1.2 represent a finely negotiated balance between optimizing virus production and infectivity while also evading innate and adaptive host immune responses. It has been hypothesized that HIV regulates Env expression levels to be high enough that viruses can mediate infection but low enough that viruses can avoid host neutralizing antibodies (59). Our data, on the other hand, suggest that EBOV may face the inverse problem because high levels of GP1,2 expression actually impair infectivity and virus production. It is possible that EBOV must maintain GP1,2 expression at low enough levels that it can produce large quantities of infectious virus while maintaining sufficient sGP expression to effectively modulate the host immune response. Future studies using recombinant EBOV, in which expression levels of GP1,2 are altered, will enable further understanding of how EBOV negotiates trade-offs in infectivity versus host immune evasion to optimize fitness. Nevertheless, our findings represent the first demonstration, to our knowledge, that high levels of glycoprotein expression suppress virus infectivity. These results add yet another dimension to our understanding of the complex balance that viruses must strike as they evolve to survive in changing host environments.
ACKNOWLEDGMENTS
We acknowledge Thuc Vy Le, Elena Vassilieva, and Yingchun Wang for assistance and Thuc Vy Le and Elena Vassilieva for helpful discussions.
This work was supported by NIAID grant AI093406.
Author contributions: C.Y., G.S.M., R.W.C., and L.Y. conceived and designed the experiments. G.S.M., L.Y., W.L., A.M., X.L., and B.S. performed the experiments. C.Y., G.S.M., L.Y., A.M., R.W.C., and B.P.P. analyzed the data. G.S.M., C.Y., and R.W.C. prepared the manuscript.
We declare that we have no known competing commercial interests, or any other conflicts of interest, with respect to the manuscript and the data contained therein.
REFERENCES
- 1.Feldmann H, Geisbert TW. 2011. Ebola haemorrhagic fever. Lancet 377:849–862. doi: 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White JM, Delos SE, Brecher M, Schornberg K. 2008. Structures and mechanisms of viral membrane fusion proteins: multiple variations on a common theme. Crit Rev Biochem Mol Biol 43:189–219. doi: 10.1080/10409230802058320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Volchkov VE, Feldmann H, Volchkova VA, Klenk HD. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci U S A 95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alvarez CP, Lasala F, Carrillo J, Muniz O, Corbi AL, Delgado R. 2002. C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in trans. J Virol 76:6841–6844. doi: 10.1128/JVI.76.13.6841-6844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marzi A, Akhavan A, Simmons G, Gramberg T, Hofmann H, Bates P, Lingappa VR, Pohlmann S. 2006. The signal peptide of the ebolavirus glycoprotein influences interaction with the cellular lectins DC-SIGN and DC-SIGNR. J Virol 80:6305–6317. doi: 10.1128/JVI.02545-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takada A, Fujioka K, Tsuiji M, Morikawa A, Higashi N, Ebihara H, Kobasa D, Feldmann H, Irimura T, Kawaoka Y. 2004. Human macrophage C-type lectin specific for galactose and N-acetylgalactosamine promotes filovirus entry. J Virol 78:2943–2947. doi: 10.1128/JVI.78.6.2943-2947.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller EH, Chandran K. 2012. Filovirus entry into cells—new insights. Curr Opin Virol 2:206–214. doi: 10.1016/j.coviro.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. 2010. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog 6:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. 2010. Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog 6:e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schornberg K, Matsuyama S, Kabsch K, Delos S, Bouton A, White J. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol 80:4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poumbourios P, Center RJ, Wilson KA, Kemp BE, Kobe B. 1999. Evolutionary conservation of the membrane fusion machine. IUBMB Life 48:151–156. [DOI] [PubMed] [Google Scholar]
- 13.Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Dal Cin P, Dye JM, Whelan SP, Chandran K, Brummelkamp TR. 2011. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cote M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, Cunningham J. 2011. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 477:344–348. doi: 10.1038/nature10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, Ruthel G, Pfeffer SR, Dye JM, Whelan SP, Brummelkamp TR, Chandran K. 2012. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 31:1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White JM, Schornberg KL. 2012. A new player in the puzzle of filovirus entry. Nat Rev Microbiol 10:317–322. doi: 10.1038/nrmicro2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohamadzadeh M, Chen L, Schmaljohn AL. 2007. How Ebola and Marburg viruses battle the immune system. Nat Rev Immunol 7:556–567. doi: 10.1038/nri2098. [DOI] [PubMed] [Google Scholar]
- 18.Yang ZY, Duckers HJ, Sullivan NJ, Sanchez A, Nabel EG, Nabel GJ. 2000. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med 6:886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- 19.Volchkov VE, Volchkova VA, Muhlberger E, Kolesnikova LV, Weik M, Dolnik O, Klenk HD. 2001. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science 291:1965–1969. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- 20.Francica JR, Matukonis MK, Bates P. 2009. Requirements for cell rounding and surface protein down-regulation by Ebola virus glycoprotein. Virology 383:237–247. doi: 10.1016/j.virol.2008.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simmons G, Wool-Lewis RJ, Baribaud F, Netter RC, Bates P. 2002. Ebola virus glycoproteins induce global surface protein down-modulation and loss of cell adherence. J Virol 76:2518–2528. doi: 10.1128/jvi.76.5.2518-2528.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Takada A, Watanabe S, Ito H, Okazaki K, Kida H, Kawaoka Y. 2000. Downregulation of beta1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology 278:20–26. doi: 10.1006/viro.2000.0601. [DOI] [PubMed] [Google Scholar]
- 23.Sanchez A, Trappier SG, Mahy BW, Peters CJ, Nichol ST. 1996. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci U S A 93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Volchkov VE, Becker S, Volchkova VA, Ternovoj VA, Kotov AN, Netesov SV, Klenk HD. 1995. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology 214:421–430. doi: 10.1006/viro.1995.0052. [DOI] [PubMed] [Google Scholar]
- 25.Ito H, Watanabe S, Takada A, Kawaoka Y. 2001. Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J Virol 75:1576–1580. doi: 10.1128/JVI.75.3.1576-1580.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kindzelskii AL, Yang Z, Nabel GJ, Todd RF III, Petty HR. 2000. Ebola virus secretory glycoprotein (sGP) diminishes Fc gamma RIIIB-to-CR3 proximity on neutrophils. J Immunol 164:953–958. doi: 10.4049/jimmunol.164.2.953. [DOI] [PubMed] [Google Scholar]
- 27.Mohan GS, Li W, Ye L, Compans RW, Yang C. 2012. Antigenic subversion: a novel mechanism of host immune evasion by Ebola virus. PLoS Pathog 8:e1003065. doi: 10.1371/journal.ppat.1003065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wahl-Jensen VM, Afanasieva TA, Seebach J, Stroher U, Feldmann H, Schnittler HJ. 2005. Effects of Ebola virus glycoproteins on endothelial cell activation and barrier function. J Virol 79:10442–10450. doi: 10.1128/JVI.79.16.10442-10450.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brindley MA, Hughes L, Ruiz A, McCray PB Jr, Sanchez A, Sanders DA, Maury W. 2007. Ebola virus glycoprotein 1: identification of residues important for binding and postbinding events. J Virol 81:7702–7709. doi: 10.1128/JVI.02433-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jeffers SA, Sanders DA, Sanchez A. 2002. Covalent modifications of the Ebola virus glycoprotein. J Virol 76:12463–12472. doi: 10.1128/JVI.76.24.12463-12472.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conzelmann KK. 1998. Nonsegmented negative-strand RNA viruses: genetics and manipulation of viral genomes. Annu Rev Genet 32:123–162. doi: 10.1146/annurev.genet.32.1.123. [DOI] [PubMed] [Google Scholar]
- 32.Flanagan EB, Ball LA, Wertz GW. 2000. Moving the glycoprotein gene of vesicular stomatitis virus to promoter-proximal positions accelerates and enhances the protective immune response. J Virol 74:7895–7902. doi: 10.1128/JVI.74.17.7895-7902.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lowen AC, Boyd A, Fazakerley JK, Elliott RM. 2005. Attenuation of bunyavirus replication by rearrangement of viral coding and noncoding sequences. J Virol 79:6940–6946. doi: 10.1128/JVI.79.11.6940-6946.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wirblich C, Schnell MJ. 2011. Rabies virus (RV) glycoprotein expression levels are not critical for pathogenicity of RV. J Virol 85:697–704. doi: 10.1128/JVI.01309-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bowers K, Pelchen-Matthews A, Honing S, Vance PJ, Creary L, Haggarty BS, Romano J, Ballensiefen W, Hoxie JA, Marsh M. 2000. The simian immunodeficiency virus envelope glycoprotein contains multiple signals that regulate its cell surface expression and endocytosis. Traffic 1:661–674. doi: 10.1034/j.1600-0854.2000.010810.x. [DOI] [PubMed] [Google Scholar]
- 36.Postler TS, Desrosiers RC. 2013. The tale of the long tail: the cytoplasmic domain of HIV-1 gp41. J Virol 87:2–15. doi: 10.1128/JVI.02053-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bachrach E, Dreja H, Lin YL, Mettling C, Pinet V, Corbeau P, Piechaczyk M. 2005. Effects of virion surface gp120 density on infection by HIV-1 and viral production by infected cells. Virology 332:418–429. doi: 10.1016/j.virol.2004.11.031. [DOI] [PubMed] [Google Scholar]
- 38.Bachrach E, Marin M, Pelegrin M, Karavanas G, Piechaczyk M. 2000. Efficient cell infection by Moloney murine leukemia virus-derived particles requires minimal amounts of envelope glycoprotein. J Virol 74:8480–8486. doi: 10.1128/JVI.74.18.8480-8486.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harty RN, Brown ME, Wang G, Huibregtse J, Hayes FP. 2000. A PPxY motif within the VP40 protein of Ebola virus interacts physically and functionally with a ubiquitin ligase: implications for filovirus budding. Proc Natl Acad Sci U S A 97:13871–13876. doi: 10.1073/pnas.250277297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ye L, Lin J, Sun Y, Bennouna S, Lo M, Wu Q, Bu Z, Pulendran B, Compans RW, Yang C. 2006. Ebola virus-like particles produced in insect cells exhibit dendritic cell stimulating activity and induce neutralizing antibodies. Virology 351:260–270. doi: 10.1016/j.virol.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 41.Wei X, Decker JM, Wang S, Hui H, Kappes JC, Wu X, Salazar-Gonzalez JF, Salazar MG, Kilby JM, Saag MS, Komarova NL, Nowak MA, Hahn BH, Kwong PD, Shaw GM. 2003. Antibody neutralization and escape by HIV-1. Nature 422:307–312. doi: 10.1038/nature01470. [DOI] [PubMed] [Google Scholar]
- 42.Pollack BP, Sapkota B, Boss JM. 2009. Ultraviolet radiation-induced transcription is associated with gene-specific histone acetylation. Photochem Photobiol 85:652–662. doi: 10.1111/j.1751-1097.2008.00485.x. [DOI] [PubMed] [Google Scholar]
- 43.Licata JM, Johnson RF, Han Z, Harty RN. 2004. Contribution of Ebola virus glycoprotein, nucleoprotein, and VP24 to budding of VP40 virus-like particles. J Virol 78:7344–7351. doi: 10.1128/JVI.78.14.7344-7351.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaletsky RL, Francica JR, Agrawal-Gamse C, Bates P. 2009. Tetherin-mediated restriction of filovirus budding is antagonized by the Ebola glycoprotein. Proc Natl Acad Sci U S A 106:2886–2891. doi: 10.1073/pnas.0811014106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaletsky RL, Simmons G, Bates P. 2007. Proteolysis of the Ebola virus glycoproteins enhances virus binding and infectivity. J Virol 81:13378–13384. doi: 10.1128/JVI.01170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dube D, Brecher MB, Delos SE, Rose SC, Park EW, Schornberg KL, Kuhn JH, White JM. 2009. The primed ebolavirus glycoprotein (19-kilodalton GP1,2): sequence and residues critical for host cell binding. J Virol 83:2883–2891. doi: 10.1128/JVI.01956-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Volchkova VA, Dolnik O, Martinez MJ, Reynard O, Volchkov VE. 2011. Genomic RNA editing and its impact on Ebola virus adaptation during serial passages in cell culture and infection of guinea pigs. J Infect Dis 204(Suppl 3):S941–S946. doi: 10.1093/infdis/jir321. [DOI] [PubMed] [Google Scholar]
- 48.Evans DT, Serra-Moreno R, Singh RK, Guatelli JC. 2010. BST-2/tetherin: a new component of the innate immune response to enveloped viruses. Trends Microbiol 18:388–396. doi: 10.1016/j.tim.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kuhl A, Banning C, Marzi A, Votteler J, Steffen I, Bertram S, Glowacka I, Konrad A, Sturzl M, Guo JT, Schubert U, Feldmann H, Behrens G, Schindler M, Pohlmann S. 2011. The Ebola virus glycoprotein and HIV-1 Vpu employ different strategies to counteract the antiviral factor tetherin. J Infect Dis 204(Suppl 3):S850–S860. doi: 10.1093/infdis/jir378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alazard-Dany N, Volchkova V, Reynard O, Carbonnelle C, Dolnik O, Ottmann M, Khromykh A, Volchkov VE. 2006. Ebola virus glycoprotein GP is not cytotoxic when expressed constitutively at a moderate level. J Gen Virol 87:1247–1257. doi: 10.1099/vir.0.81361-0. [DOI] [PubMed] [Google Scholar]
- 51.Sullivan NJ, Peterson M, Yang ZY, Kong WP, Duckers H, Nabel E, Nabel GJ. 2005. Ebola virus glycoprotein toxicity is mediated by a dynamin-dependent protein-trafficking pathway. J Virol 79:547–553. doi: 10.1128/JVI.79.1.547-553.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zampieri CA, Fortin JF, Nolan GP, Nabel GJ. 2007. The ERK mitogen-activated protein kinase pathway contributes to Ebola virus glycoprotein-induced cytotoxicity. J Virol 81:1230–1240. doi: 10.1128/JVI.01586-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Francica JR, Varela-Rohena A, Medvec A, Plesa G, Riley JL, Bates P. 2010. Steric shielding of surface epitopes and impaired immune recognition induced by the ebola virus glycoprotein. PLoS Pathog 6:e1001098. doi: 10.1371/journal.ppat.1001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dolnik O, Volchkova V, Garten W, Carbonnelle C, Becker S, Kahnt J, Stroher U, Klenk HD, Volchkov V. 2004. Ectodomain shedding of the glycoprotein GP of Ebola virus. EMBO J 23:2175–2184. doi: 10.1038/sj.emboj.7600219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wenigenrath J, Kolesnikova L, Hoenen T, Mittler E, Becker S. 2010. Establishment and application of an infectious virus-like particle system for Marburg virus. J Gen Virol 91:1325–1334. doi: 10.1099/vir.0.018226-0. [DOI] [PubMed] [Google Scholar]
- 56.Reynard O, Borowiak M, Volchkova VA, Delpeut S, Mateo M, Volchkov VE. 2009. Ebolavirus glycoprotein GP masks both its own epitopes and the presence of cellular surface proteins. J Virol 83:9596–9601. doi: 10.1128/JVI.00784-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Volchkov VE, Blinov VM, Netesov SV. 1992. The envelope glycoprotein of Ebola virus contains an immunosuppressive-like domain similar to oncogenic retroviruses. FEBS Lett 305:181–184. doi: 10.1016/0014-5793(92)80662-Z. [DOI] [PubMed] [Google Scholar]
- 58.Yaddanapudi K, Palacios G, Towner JS, Chen I, Sariol CA, Nichol ST, Lipkin WI. 2006. Implication of a retrovirus-like glycoprotein peptide in the immunopathogenesis of Ebola and Marburg viruses. FASEB J 20:2519–2530. doi: 10.1096/fj.06-6151com. [DOI] [PubMed] [Google Scholar]
- 59.Klein JS, Bjorkman PJ. 2010. Few and far between: how HIV may be evading antibody avidity. PLoS Pathog 6:e1000908. doi: 10.1371/journal.ppat.1000908. [DOI] [PMC free article] [PubMed] [Google Scholar]