Abstract
Background
Pedicle screws are biomechanically superior over other spinal fixation devices. When improperly positioned, they lose this advantage and put adjacent structures at risk. Accurate placement is therefore critical. Postoperative computed tomography (CT) scans are the imaging gold standard and have shown malposition rates ranging from 2% to 41%. The O-arm (Medtronic Navigation, Louisville, Colorado) is an intraoperative CT scanner that may allow intervention for malpositioned screws while patients are still in the operating room. However, this has not yet been shown in clinical studies. The primary objective of this study was to assess the usefulness of the O-arm for evaluating pedicle screw position by answering the following question: What is the rate of intraoperative pedicle screw revision brought about by O-arm imaging information? A secondary question was also addressed: What is the rate of unacceptable thoracic and lumbar pedicle screw placement as assessed by intraoperative O-arm imaging?
Methods
This is a case series of consecutive patients who have undergone spine surgery for which an intraoperative 3-dimensional (3D) CT scan was used to assess pedicle screw position. The study comprised 602 pedicle screws (235 thoracic and 367 lumbar/sacral) placed in 76 patients, and intraoperative 3D (O-arm) imaging was obtained to assess screw position. Action taken at the time of surgery based on imaging information was noted. An independent review of all scans was also conducted, and all screws were graded as either optimal (no breach), acceptable (breach ≤2 mm), or unacceptable (breach >2 mm). The rate of pedicle screw revision, as detected by intraoperative 3D CT scan, was determined.
Results
On the basis of 3D imaging information, 17 of 602 screws (2.8%) in 14 of 76 cases (18.4%) were revised at the time of surgery. On independent review of multiplanar images, 11 screws (1.8%) were found to be unacceptable, 32 (5.3%) were acceptable, and 559 (92.9%) were optimal. All unacceptable screws were revised to an optimal or acceptable position, and an additional 6 acceptable screws were revised to an optimal position. Thus, by the end of the cases, none of the 602 pedicle screws in the 76 surgical procedures was in an unacceptable position.
Conclusion
The new-generation intraoperative 3D imaging system (O-arm) is a useful tool that allows more accurate assessment of pedicle screw position than plain radiographs or fluoroscopy alone. It prompted intraoperative repositioning of 2.8% of pedicle screws in our series. Most importantly, it allowed identification and revision of all unacceptably placed pedicle screws without the need for reoperation.
Keywords: Pedicle screw, Pedicle screw revision, Pedicle screw malposition, O-arm, Intraoperative 3-D imaging
Over the past decade, pedicle screws have become the preferred spinal fixation method, initially for the lumbar spine and increasingly for the thoracic spine as well. They have superior biomechanics over other fixation devices,1, 2 and clinical experience has yielded improved fusion rates and reduced need for postoperative immobilization.3, 4 One drawback, however, is the possibility of screw malposition with consequent injury to vital structures, such as the neural elements and major vessels.5–7 A recent meta-analysis of studies published from 1966 to 2006 showed that the median malposition rates for non-navigated and navigated pedicle screws were 9.7% and 4.8%, respectively.8
Screw malposition that produces neurologic deficit is a clear indication for bringing the patient back to the operating room, to either remove or reposition the screw. Fortunately, only a small percentage of malpositioned screws are symptomatic.9, 10 Nonetheless, a misplaced screw compromises construct stability and may offset whatever biomechanical advantage pedicle screw fixation offers.11, 12 Moreover, there is still potential for late complications, such as when a screw abutting against a major vessel gradually erodes through its wall.13, 14 Although there are distinct benefits to revising a malpositioned screw, these should be weighed against the risks and added cost of a return trip to the operating room.
The clinical standard for evaluating screw position is a computed tomography (CT) scan.15 Compared with plain radiographs, CT gives 3-dimensional (3D) information (sagittal, coronal, and axial).16, 17 However, this modality is not readily available in most operating suites, and only plain radiography and C-arm fluoroscopy are usually available. Often, a malpositioned screw is only detected on a postoperative CT study,10, 16 thus presenting a dilemma of whether to reoperate.
A new-generation intraoperative CT scanner (O-arm; Medtronic Navigation, Louisville, Colorado) designed to give 3D imaging information in a timely fashion has recently become available.18 The imaging information given by the O-arm system had been shown to be highly accurate in terms of identifying screw malposition.19 The major potential advantage of this system in the context of pedicle screw fixation is that the timeliness of the information given allows the surgeon to revise nonoptimal screws in the same surgical setting and without added risk to the patient. However, there have not yet been studies to substantiate this claim.
The primary objective of this study was to assess the usefulness of the O-arm for evaluating pedicle screw position by answering the following question: What is the rate of intraoperative pedicle screw revision brought about by O-arm imaging information? A secondary question was also addressed: What is the rate of unacceptable thoracic and lumbar pedicle screw placement as assessed by intraoperative O-arm imaging?
Methods
Between October 2006 and January 2008, 105 consecutive spine surgeries were performed with intraoperative O-arm imaging. Of these, 76 cases performed by 2 orthopaedic spine surgeons underwent pedicle screw fixation (602 screws), wherein the O-arm was used to assess screw position. Cases were identified by a prospective surgical database maintained since acquisition of the O-arm system. A review of operative reports and intraoperative images was conducted after we obtained institutional review board approval for review of existing records.
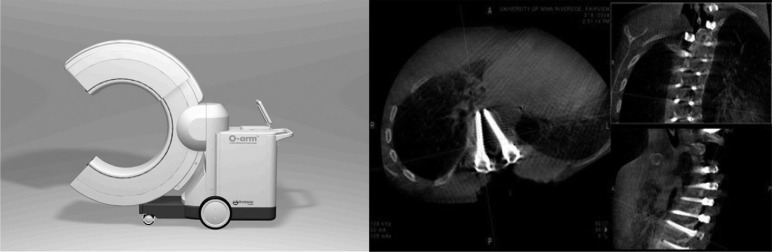
The new-generation intraoperative 3D imaging system (O-arm) is a multidimensional surgical imaging platform with an O-shaped gantry that allows for 2-dimensional fluoroscopy and 3D imaging. The gantry has a telescoping feature that opens to 70 cm, enabling lateral patient access. The ring has an inner diameter of 97 cm, outer diameter of 172 cm, and width of 54 cm (Fig. 1). The gantry can be positioned with robotic control within a range of 45.8 cm mediolaterally, 35.6 cm craniocaudally, and 45.8 cm anteroposteriorly, with reference to the patient lying on the table. It allows programming of up to 5 views to memory, including a “park” position. A digital flat-panel detector provides image quality with 2.0 K × 1.5 K of resolution and a field of view of 40 cm × 30 cm for fluoroscopy and 20 cm in diameter × 15 cm in length for 3D imaging. Image acquisition for 3D scans takes 13 seconds in standard-definition mode (391 projections around a 360° circumference) or 26 seconds in high-definition mode (750 projections around a 360° circumference). It takes an additional 13 seconds (standard definition) or 35 seconds (high definition) for processing and image reconstruction. The software enables the surgeon to perform multiplanar reformatting on the workstation screen; thus the viewing plane is not limited to the projection plane.
Fig. 1.
Left, New-generation intraoperative CT imaging system (O-arm) designed to provide 3D imaging information in a timely fashion. (Used with permission from Medtronic Navigation.) Right, Snapshot of imaging system workstation screen showing ability to assess spinal elements and pedicle screws in all 3 planes (axial, coronal, and sagittal).
The mean patient age was 48.8 years (range, 9 months to 94 years). Of the patients, 9 were aged younger than 18 years and 2 were aged younger than 10 years. There were 30 male and 46 female patients. The most common diagnoses were degenerative conditions (disk disease, degenerative spondylolisthesis/scoliosis, stenosis, and acquired kyphosis), comprising 42 cases. The other diagnoses were deformities (16), postsurgical complications (9), fractures including osteoporotic compression fractures (4), tumors or tumor-like conditions (3), and infection (2). The 16 cases of deformities included adolescent idiopathic scoliosis (6), congenital scoliosis (4), dysplastic spondylolisthesis (2), lytic spondylolisthesis (1), neurofibromatosis with dystrophic scoliosis (1), Scheuermann kyphosis (1), and spinal dysgenesis (1) (Table 1).
Table 1.
Diagnoses of 76 surgical cases with pedicle screw placement and with screw position verified by intraoperative 3D imaging
| No. of cases | |
|---|---|
| Degenerative spine disease (eg, degenerative disk disease, degenerative spondylolisthesis/scoliosis, acquired kyphosis) | 42 |
| Spine deformities | |
| Adolescent idiopathic scoliosis | 6 |
| Congenital scoliosis | 4 |
| Dysplastic spondylolisthesis | 2 |
| Lytic spondylolisthesis | 1 |
| Neurofibromatosis with dystrophic scoliosis | 1 |
| Scheuermann kyphosis | 1 |
| Spinal dysgenesis | 1 |
| Postsurgical complications | 9 |
| Fractures, including osteoporotic compression fractures | 4 |
| Spine tumors or tumor-like conditions | 3 |
| Infection | 2 |
| Total | 76 |
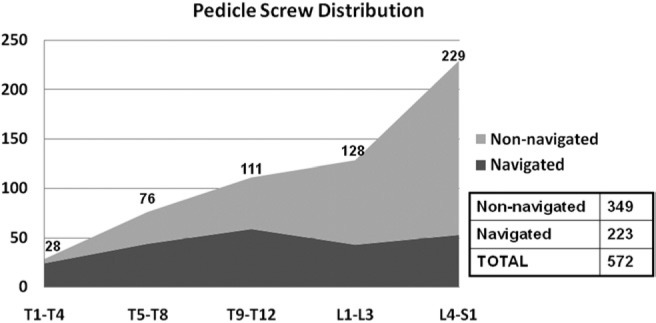
Of the 602 pedicle screws, 34 were placed at the upper thoracic levels (T1-4), 84 at the midthoracic levels (T5-8), 117 at the lower thoracic levels (T9-12), 132 at the upper lumbar levels (L1-3), and 235 at the lower lumbar/sacral levels (L4-S1) (Fig. 2).
Fig. 2.
Graph showing pedicle screw distribution according to anatomic region (T1-4, T5-8, T9-12, L1-3, and L4-S1) and further broken down based on whether navigation was used in screw placement. Two findings in this graph are worth noting: (1) A greater number of pedicle screws in this series were placed at the more distal (lumbar) levels. (2) Although the absolute number of screws placed with navigation remained fairly constant across different spinal regions, the proportion of navigated screw placement was much higher at more proximal levels.
The following different methods of screw placement were used: (1) 2-dimensional C-arm or O-arm fluoroscopy (37 cases), (2) computer navigation (23 cases), (3) anatomic landmarks (9 cases), and (4) previous screw tracks in revisions (14 cases). In 7 cases more than 1 placement method was used (eg, previous screw tracks at levels where screws were previously placed, as well as anatomic landmarks for additional levels) (Table 2, Fig. 2).
Table 2.
Methods used for placement of 602 pedicle screws verified by intraoperative 3D imaging
| No. of cases | |
|---|---|
| 2-Dimensional fluoroscopy (C-arm or O-arm) | 37 |
| Computer navigation (O-arm image guidance) | 23 |
| Anatomic landmarks | 9 |
| Previous screw tracks | 14 |
| Total | 76 (7 cases used >1 method) |
Regardless of the screw placement method, an intraoperative 3D O-arm scan taken after screw placement was used in all cases included in this review for the purpose of evaluating screw position. The images were reviewed by the surgeon on the O-arm workstation screen as soon as they became available. The standard screen format shows 3 windows: a large left window showing the axial plane image and small upper right and lower right windows showing the coronal and sagittal plane images, respectively (Fig. 1). Using a sterile infrared control device, the surgeon can scroll through the images in one window and can jump from one window to the next. Scout lines show the location of the image in relation to other planes. An unscrubbed assistant can also alter the orientation of the image planes using the keyboard control on the workstation. This feature allows viewing the screws along specific planes (eg, along the longitudinal axis of the screw) as desired.
Images and operative reports were reviewed to look for evidence of intraoperative screw revision (removal or repositioning) that was influenced by information gleaned from the O-arm scan.
An independent observer (J.N.S.), who was not involved in any of the surgeries, likewise reviewed all the 3D images and graded each pedicle screw, regardless of whether it was subsequently revised. A modification of the grading system of Gertzbein et al. was used: optimal (no breach), acceptable (breach ≤2 mm), and unacceptable (breach >2 mm).
Results
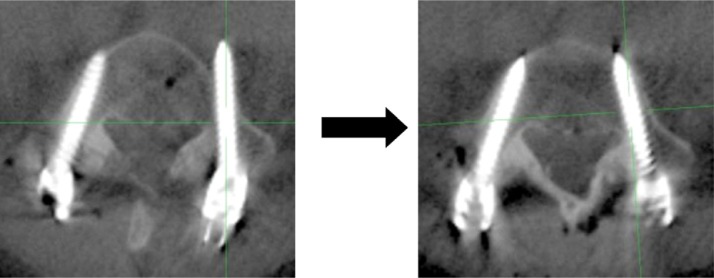
Of the 602 screws placed, 17 (2.8%) were revised based on O-arm imaging information (Table 3). Nine laterally malpositioned screws (one each at T6, L2, and L3 and two each at T7, T8, and L5) were redirected medially (Fig. 3), and six medially malpositioned screws (one each at T6, T7, L2, and L5 and two at S1) were redirected laterally. One laterally malpositioned screw (L4) in a patient with neurofibromatosis and dystrophic scoliosis and one medially malpositioned screw (T12) in a patient with a fracture-dislocation at the thoracolumbar junction were removed altogether. In both instances the surgeon deemed that the aberrant anatomy precluded safe and optimal screw repositioning. Overall, revision of at least 1 screw was performed in 14 of 76 cases (18.4%).
Table 3.
Details on 17 of 602 screw revisions (2.8%) performed based on 3D imaging information
| Spine level | Direction of malposition | Action performed |
|---|---|---|
| T6 | Lateral | Repositioned medially |
| T6 | Medial | Repositioned laterally |
| T7 | Lateral | Repositioned medially |
| T7 | Lateral | Repositioned medially |
| T7 | Medial | Repositioned laterally |
| T8 | Lateral | Repositioned medially |
| T8 | Lateral | Repositioned medially |
| T12 | Medial | Removed |
| L2 | Lateral | Repositioned medially |
| L2 | Medial | Repositioned laterally |
| L3 | Lateral | Repositioned medially |
| L4 | Lateral | Removed |
| L5 | Lateral | Repositioned medially |
| L5 | Lateral | Repositioned medially |
| L5 | Medial | Repositioned laterally |
| S1 | Medial | Repositioned laterally |
| S1 | Medial | Repositioned laterally |
Fig. 3.
Example of a malpositioned pedicle screw with significant breach of the anterolateral vertebral body wall (left), which was detected intraoperatively with the CT scanner. This timely information allowed prompt repositioning of the screw to an optimal position (right) without the need for reoperation.
On independent review of the 3D scans to evaluate individual screw position, 559 screws (92.9%) were judged optimal, 32 (5.3%) were acceptable, and 11 (1.8%) were unacceptable (Table 4). All unacceptable screws turned out to have been subsequently revised by the surgeon. In addition, 6 screws that were deemed acceptable were revised to an optimal position. None of the optimal screws was revised.
Table 4.
Results of independent review of 3D scans for assessment of position of 602 pedicle screws
| Grade | No. of screws (%) | Intraoperative action performed |
|---|---|---|
| Optimal (no breach) | 559 (92.9) | None revised |
| Acceptable (breach ≤2 mm) | 32 (5.3) | 6 of 32 (19%) revised to optimal position |
| Unacceptable (breach >2 mm) | 11 (1.8) | All revised to optimal/acceptable position |
| Total | 602 (100) |
Discussion
To achieve optimal biomechanics and to avoid injury to surrounding structures, accurate placement of pedicle screws is critical. Several methods of screw placement are widely used: anatomic landmarks,20, 21 intraoperative fluoroscopy, 22 and computer navigation.23, 24 Adjunctive methods, such as palpation of the screw track25 and electrical stimulation with neurologic monitoring,26 have also been shown to be useful. Nonetheless, a meta-analysis by Kosmopoulos and Schizas27 showed overall malposition rates of 4.8% for navigated screw placement and 9.7% for non-navigated placement.
CT has been shown to be a more accurate and reliable imaging method for evaluating screw position than plain radiography.16, 17 However, this modality is not readily available in most operating rooms. Early-generation mobile CT scanners have suffered from difficulty of use and poor image quality.28, 29 The O-arm is an example of a new-generation intraoperative imaging system that is capable of providing 3D images. We set out to assess its usefulness in spine surgery, specifically in the setting of pedicle screw fixation, by determining the intraoperative screw revision rate brought about by O-arm imaging information.
Our results show that in a series of 602 pedicle screw placements, intraoperative screw revision was performed in 2.8%. Most reports on the accuracy of pedicle screw placement graded the screws based on imaging assessment. Those that included data on screw revision have reported revision rates of 0.3% to 4.3%.10, 30, 31 Although our rate of 2.8% falls well within this range, it should be kept in mind that ours were all intraoperative revisions. It could be hypothesized that a surgeon's threshold for revising a screw in this setting would be much lower than if a second surgical procedure and a possible readmission will be required. Furthermore, although most of the revisions reported in the literature were performed for symptomatic and thus grievous screw malpositions, it is difficult to determine whether the screws that were revised in our series would have caused symptoms otherwise. No screw-related complications developed in any of our patients who had screw revision. It may well be that at least some of these 14 patients would have been asymptomatic and not have required a second procedure anyway. Nonetheless, in light of the low risk involved in revising a screw, acceptance of an unacceptable screw position detected intraoperatively is not justified.
When we looked at the action taken by the surgeon in relation to the results of screw position grading by an independent reviewer, 11 of the screws (1.8%) were unacceptable and they were all revised. In addition, 6 of the 32 acceptable screws were revised to an optimal position. Although it would be very difficult to prove the benefit of revising an acceptable screw to an optimal screw, it is intuitive that any difference between the two, if such a difference exists, would be in favor of the latter.
The limitations of our study relate to its retrospective and nonrandomized study design. In particular, a meaningful comparison of screw revision rates between navigated and non-navigated screws, as well as between thoracic and lumbar regions, cannot be reliably made. Although more screws in the navigated group were revised compared with the non-navigated group (10 of 243 [4.1%] vs 7 of 359 [1.9%]), this is not a fair comparison because navigation was preferentially used for cases where screw placement was deemed more difficult, such as thoracic spine placement, as well as cases with deformities or congenital abnormalities. In addition, although revision rates between thoracic and lumbar screws were similar (8 of 235 [3.4%] vs 9 of 367 [2.5%]), any potential difference may have been tempered by the fact that more thoracic screws were placed using navigation.
In addition to the use of the O-arm system as an intraoperative advanced imaging device for assessment of pedicle screw position, the O-arm system has been used in conjunction with navigation or image guidance systems for pedicle screw placement. Recently published clinical studies have shown increased screw placement accuracy using intraoperative 3D (O-arm) image-guided navigation.32–34 Although this method of pedicle screw placement was used in some of the patients in our series, mainly in the latter portion of the study, the accuracy of navigated screw placement is not the focus of this particular study.
In summary, the results of this study indicate that the O-arm imaging system is useful in spine surgery, particularly in the setting of pedicle screw fixation. Use of the O-arm allowed timely identification and revision of all unacceptably positioned screws. In addition, acceptably but non–optimally placed screws may be revised to an optimal position, with minimal added risk to the patient.
References
- 1.Ferguson RL, Tencer AF, Woodard P, Allen BL. Biomechanical comparisons of spinal fracture models and the stabilizing effects of posterior instrumentations. Spine. 1988;13:453–60. doi: 10.1097/00007632-198805000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Wood KB, Wentorf FA, Ogilvie JW, Kim KT. Torsional rigidity of scoliosis constructs. Spine (Phila Pa 1976) 2000;25:1893–8. doi: 10.1097/00007632-200008010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kuklo TR, Potter BK, Lenke LG, Polly DW, Sides B, Bridwell KH. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2007;32:2258–64. doi: 10.1097/BRS.0b013e31814b1ba6. [DOI] [PubMed] [Google Scholar]
- 4.Ransom N, La Rocca SH, Thalgott J. The case for pedicle fixation of the lumbar spine. Spine (Phila Pa 1976) 1994;19:2702–6. [PubMed] [Google Scholar]
- 5.Whitecloud TS, III, Butler JC, Cohen JL, Candelora PD. Complications with the variable spinal plating system. Spine (Phila Pa 1976) 1989;14:472–6. doi: 10.1097/00007632-198904000-00027. [DOI] [PubMed] [Google Scholar]
- 6.West JL, III, Ogilvie JW, Bradford DS. Complications of the variable screw plate pedicle screw fixation. Spine (Phila Pa 1976) 1991;16:576–9. doi: 10.1097/00007632-199105000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Yuan HA, Garfin SR, Dickman CA, Mardjetko SM. A historical cohort study of pedicle screw fixation in thoracic, lumbar, and sacral spinal fusions. Spine (Phila Pa 1976) 1994;19(Suppl):2279S–96S. doi: 10.1097/00007632-199410151-00005. [DOI] [PubMed] [Google Scholar]
- 8.Kosmopoulos V, Theumann N, Binaghi S, Schizas C. Observer reliability in evaluating pedicle screw placement using computed tomography. Int Orthop. 2007;31:531–6. doi: 10.1007/s00264-006-0230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schulze CJ, Munzinger E, Weber U. Clinical relevance of accuracy of pedicle screw placement. A computed tomographic-supported analysis. Spine (Phila Pa 1976) 1998;23:2215–20. doi: 10.1097/00007632-199810150-00014. discussion 2220–1. [DOI] [PubMed] [Google Scholar]
- 10.Belmont PJ, Jr, Klemme WR, Dhawan A, Polly DW. In vivo accuracy of thoracic pedicle screws. Spine (Phila Pa 1976) 2001;26:2340–6. doi: 10.1097/00007632-200111010-00010. [DOI] [PubMed] [Google Scholar]
- 11.Acikbas SC, Arslan FY, Tuncer MR. The effect of transpedicular screw misplacement on late spinal stability. Acta Neurochir (Wien) 2003;145:949–54. doi: 10.1007/s00701-003-0116-0. discussion 954–5. [DOI] [PubMed] [Google Scholar]
- 12.George DC, Krag MH, Johnson CC, Van Hal ME, Haugh LD, Grobler LJ. Hole preparation techniques for transpedicle screws. Effect on pull-out strength from human cadaveric vertebrae. Spine (Phila Pa 1976) 1991;16:181–4. [PubMed] [Google Scholar]
- 13.Wegener B, Birkenmaier C, Fottner A, Jansson V, Dürr HR. Delayed perforation of the aorta by a thoracic pedicle screw. Eur Spine J. 2008;17(Suppl):S351–4. doi: 10.1007/s00586-008-0715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kakkos SK, Shepard AD. Delayed presentation of aortic injury by pedicle screws: report of two cases and review of the literature. J Vasc Surg. 2008;47:1074–82. doi: 10.1016/j.jvs.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Rao G, Brodke DS, Rondina M, Dailey AT. Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg. 2002;97(Suppl):223–6. doi: 10.3171/spi.2002.97.2.0223. [DOI] [PubMed] [Google Scholar]
- 16.Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine (Phila Pa 1976) 1995;20:1494–9. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Choma TJ, Denis F, Lonstein JE, et al. Stepwise methodology for plain radiographic assessment of pedicle screw placement: a comparison with computed tomography. J Spinal Disord Tech. 2006;19:547–53. doi: 10.1097/01.bsd.0000211221.74307.57. [DOI] [PubMed] [Google Scholar]
- 18.Holly LT, Foley KT. Image guidance in spine surgery. Orthop Clin North Am. 2007;38:451–61. doi: 10.1016/j.ocl.2007.04.001. abstract viii. [DOI] [PubMed] [Google Scholar]
- 19.Santos ER, Ledonio CG, Castro CA, Truong WH, Sembrano JN. The accuracy of intraoperative O-arm images for the assessment of pedicle screw postion. Spine (Phila Pa 1976) 2012;37:E119–25. doi: 10.1097/BRS.0b013e3182257cae. [DOI] [PubMed] [Google Scholar]
- 20.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986:7–17. [PubMed] [Google Scholar]
- 21.Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 1988;13:1012–8. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Steinmann JC, Herkowitz HN, el-Kommos H, Wesolowski DP. Spinal pedicle fixation. Confirmation of an image-based technique for screw placement. Spine (Phila Pa 1976) 1993;18:1856–61. [PubMed] [Google Scholar]
- 23.Berlemann U, Monin D, Arm E, Nolte LP, Ozdoba C. Planning and insertion of pedicle screws with computer assistance. J Spinal Disord. 1997;10:117–24. [PubMed] [Google Scholar]
- 24.Holly LT, Foley KT. Intraoperative spinal navigation. Spine (Phila Pa 1976) 2003;28(Suppl):S54–61. doi: 10.1097/01.BRS.0000076899.78522.D9. [DOI] [PubMed] [Google Scholar]
- 25.Lehman RA, Potter BK, Kuklo TR, et al. Probing for thoracic pedicle screw tract violation(s): is it valid? J Spinal Disord Tech. 2004;17:277–83. doi: 10.1097/01.bsd.0000095399.27687.c5. [DOI] [PubMed] [Google Scholar]
- 26.Glassman SD, Dimar JR, Puno RM, Johnson JR, Shields CB, Linden RD. A prospective analysis of intraoperative electromyographic monitoring of pedicle screw placement with computed tomographic scan confirmation. Spine (Phila Pa 1976) 1995;20:1375–9. [PubMed] [Google Scholar]
- 27.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32:E111–20. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 28.Butler WE, Piaggio CM, Constantinou C, et al. A mobile computed tomographic scanner with intraoperative and intensive care unit applications. Neurosurgery. 1998;42:1304–10. doi: 10.1097/00006123-199806000-00064. discussion 1310–1. [DOI] [PubMed] [Google Scholar]
- 29.Hum B, Feigenbaum F, Cleary K, Henderson FC. Intraoperative computed tomography for complex craniocervical operations and spinal tumor resections. Neurosurgery. 2000;47:374–80. doi: 10.1097/00006123-200008000-00019. discussion 380–1. [DOI] [PubMed] [Google Scholar]
- 30.Belmont PJ, Jr, Klemme WR, Robinson M, Polly DW. Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine (Phila Pa 1976) 2002;27:1558–66. doi: 10.1097/00007632-200207150-00015. [DOI] [PubMed] [Google Scholar]
- 31.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine (Phila Pa 1976) 2007;32:1655–61. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 32.Larson AN, Santos ER, Polly DW, Jr, et al. Pediatric pedicle screw placement using intraoperative computed tomography and 3-dimensional image-guided navigation. Spine (Phila Pa 1976) 2012;37:E188–94. doi: 10.1097/BRS.0b013e31822a2e0a. [DOI] [PubMed] [Google Scholar]
- 33.Houten JK, Nasser R, Baxi N. Clinical assessment of percutaneous lumbar pedicle screw placement using the O-arm multidimensional surgical imaging system. Neurosurgery. 2011 doi: 10.1227/NEU.0b013e318237a829. In press. [DOI] [PubMed] [Google Scholar]
- 34.Silbermann J, Riese F, Allam Y, Reichert T, Koeppert H, Gutberlet M. Computer tomography assessment of pedicle screw placement in lumbar and sacral spine: comparison between free-hand and O-arm based navigation techniques. Eur Spine J. 2011;20:875–81. doi: 10.1007/s00586-010-1683-4. [DOI] [PMC free article] [PubMed] [Google Scholar]