ABSTRACT
Alphaviruses represent a significant public health threat worldwide. They are transmitted by mosquitoes and cause a variety of human diseases ranging from severe meningoencephalitis to polyarthritis. To date, no efficient and safe vaccines have been developed against any alphavirus infection. However, in recent years, significant progress has been made in understanding the mechanism of alphavirus replication and virus-host interactions. These data have provided the possibility for the development of new rationally designed alphavirus vaccine candidates that combine efficient immunogenicity, high safety, and inability to revert to pathogenic phenotype. New attenuated variants of Venezuelan equine encephalitis virus (VEEV) designed in this study combine a variety of characteristics that independently contribute to a reduction in virulence. These constructs encode a noncytopathic VEEV capsid protein that is incapable of interfering with the innate immune response. The capsid-specific mutations strongly affect neurovirulence of the virus. In other constructs, they were combined with changes in control of capsid translation and an extensively mutated packaging signal. These modifications also affected the residual neurovirulence of the virus, but it remained immunogenic, and a single immunization protected mice against subsequent infection with epizootic VEEV. Similar approaches of attenuation can be applied to other encephalitogenic New World alphaviruses.
IMPORTANCE Venezuelan equine encephalitis virus (VEEV) is an important human and animal pathogen, which causes periodic outbreaks of highly debilitating disease. Despite a continuous public health threat, no safe and efficient vaccine candidates have been developed to date. In this study, we applied accumulated knowledge about the mechanism of VEEV replication, RNA packaging, and interaction with the host to design new VEEV vaccine candidates that demonstrate exceptionally high levels of safety due to a combination of extensive modifications in the viral genome. The introduced mutations did not affect RNA replication or structural protein synthesis but had deleterious effects on VEEV neuroinvasion and virulence. In spite of dramatically reduced virulence, the designed mutants remained highly immunogenic and protected mice against subsequent infection with epizootic VEEV. Similar methodologies can be applied for attenuation of other encephalitogenic New World alphaviruses.
INTRODUCTION
The Alphavirus genus in the Togaviridae family contains a variety of human and animal pathogens, which are widely distributed on all continents, including South, Central, and North America (1). In natural conditions, most alphaviruses are transmitted by mosquito vectors, in which they cause a persistent, lifelong infection characterized by high levels of virus accumulation in the salivary glands (2). Upon transmission to vertebrate hosts, alphaviruses cause acute infections and induce diseases of various severities, with symptoms ranging from severe meningoencephalitis to mild rash and polyarthritis (3).
The New World (NW) alphaviruses, such as eastern, western, and Venezuelan (VEEV) equine encephalitis viruses represent a significant public health threat. The epizootic strains of VEEV are lethal for equids and cause very severe diseases in humans (4). The NW alphaviruses were also developed during the Cold War as biological warfare agents due to numerous user-friendly characteristics, such as an ability to grow to very high titers in many commonly used cell lines, stability in lyophilized form and efficient transmission by aerosol (5). Accordingly, these viruses are classified as category B select agents by the CDC. Thus far, no therapeutic means or safe and efficient vaccines have been designed for use against any of the NW alphaviruses. The only live experimental vaccine for VEEV infection, VEEV TC-83, was developed more than 4 decades ago by serial passaging of the wild-type (wt) VEEV TRD strain in cultured guinea pig heart cells (6, 7). Its attenuated phenotype relies entirely on two point mutations, one located in the 5′ untranslated region (5′UTR) of the viral genome, and the other in the E2 glycoprotein (8, 9). VEEV TC-83 has demonstrated a potential for rapid reversion to the wt phenotype (10). In addition to the risk of reversion, this vaccine also causes adverse reactions, which often result in a disease with the symptoms similar to the wt virus infection (6, 11). An inactivated vaccine, C-84, was developed on the basis of VEEV TC-83. It is safe but less immunogenic, and it requires boosters to support high levels of neutralizing antibodies (Abs) (12). Thus, the need for safe and efficient vaccines against alphaviruses, and VEEV in particular, remains urgent.
In the last number of years, significant progress has been made in understanding the mechanism of VEEV genome replication and its packaging into infectious virions. In particular, much new information has been generated regarding the interaction of alphaviruses with their hosts on molecular and cellular levels. These data have provided new opportunities to develop novel vaccine strategies to combat alphavirus infections. For example, it was shown that the VEEV capsid protein is an important player not only in the virion assembly process but is also an inhibitor of cellular transcription, type I interferon (IFN) induction, and activation of interferon-stimulated genes (ISGs) (13–16). However, the capsid protein of the Old World (OW) alphaviruses does not exhibit these nuclear functions (17, 18). The latter viruses use their nonstructural protein, nsP2, to induce degradation of one of the subunits of cellular RNA polymerase II through the ubiquitin pathway and thus also inhibit the antiviral response (19, 20). This difference between the NW and the OW alphaviruses was used to develop chimeric viruses, which do not exhibit nuclear inhibitory functions (18, 21–23). VEE/CHIKV or VEE/SINV chimeras, which encode VEEV-specific nonstructural proteins and chikungunya virus (CHIKV)- or Sindbis virus (SINV)-specific structural proteins, respectively, produce no proteins capable of interfering with cellular transcription. They were found to be highly attenuated, noncytopathic and very potent type I IFN inducers (21). VEE/CHIKV chimeras were also found to be exceptionally safe and induced a very efficient protective immune response against CHIKV infection in a small animal model (22). Importantly, the attenuated phenotype appeared to be irreversible, since a combination of fragments from very different viruses in the same genome makes evolution to a pathogenic phenotype a highly unlikely event.
Unfortunately, it is impossible to apply a similar chimeric virus approach for the development of vaccine candidates against NW alphaviruses. However, other possibilities for manipulations of their genome and modification of virus biology became recently available. The transcription inhibitory functions of VEEV capsid protein were found to be dependent on binding of importin-α/β and CRM1 (14). The binding sites of both receptors were mapped to a small peptide located in the amino-terminal fragment of capsid protein (14). Multiple redundant mutations in this peptide did not affect nucleocapsid assembly but made capsid protein noncytopathic and incapable of inducing transcriptional shutoff or interfering with development of the innate immune response (16).
Another possibility for virus attenuation was suggested by studies of the mechanism of VEEV genomic RNA packaging (24) and identification of the RNA packaging signal (PS) (25, 26). Numerous synonymous mutations were made in the PS-containing RNA fragment, which did not change the nsP1-specific amino acid sequence but completely modified the nucleotide sequence and secondary structure of the VEEV PS (26). This in turn strongly affected the release of infectious, genome-containing virions and infectious titers.
In this study, we have applied these and other recent findings in the mechanism of VEEV replication and its interactions with cellular proteins to introduce additional levels of safety to the previously developed VEEV TC-83 experimental vaccine. The extended modifications were designed in a way to cause little or no negative effect on RNA replication and expression of virus-specific proteins. However, the designed viruses were expected to be attenuated and incapable of interfering with the innate immune response or development of high titer viremia, which could potentially lead to their transmission to mosquitoes. We have characterized the newly designed VEEV TC-83-based variants in terms of their replication in vitro and compared their safety and abilities to induce protective immune response against an epizootic strain of VEEV.
MATERIALS AND METHODS
Cell cultures.
The BHK-21 cells were kindly provided by Paul Olivo (Washington University, St. Louis, MO). The NIH 3T3 cells were obtained from the American Type Tissue Culture Collection (Manassas, VA). Vero cells were kindly provided by Scott Weaver (University of Texas Medical Branch, Galveston, TX). These cell lines were maintained at 37°C in alpha minimum essential medium supplemented with 10% fetal bovine serum (FBS) and vitamins.
Plasmid constructs.
Standard recombinant DNA techniques were used for all plasmid constructions. The pVEEV-TC83 plasmid encoding VEEV TC-83 genome was described elsewhere (16, 27). pVEEV/Cm, pVEEV/PS−/Cm, and pVEEV/IRES-Cm contained mutations in capsid protein (16), which are presented in Fig. 1B. pVEEV/PS−/Cm contained 135 mutations in VEEV PS (26), which are presented in Fig. 1C. pVEEV/IRES-Cm had essentially the same design as the plasmid pVEEV/IRES/C, which we have described elsewhere (10), but encoded the mutated VEEV capsid protein. Maps and sequences are available from the authors upon request. Plasmid encoding the infectious cDNA of VEEV strain 3908 was provided by Scott Weaver (University of Texas Medical Branch at Galveston). All of the work with VEEV 3908 RNA, virus rescue, and infections was performed in BSL3 and ABSL3 facilities of the UAB SEBLAB.
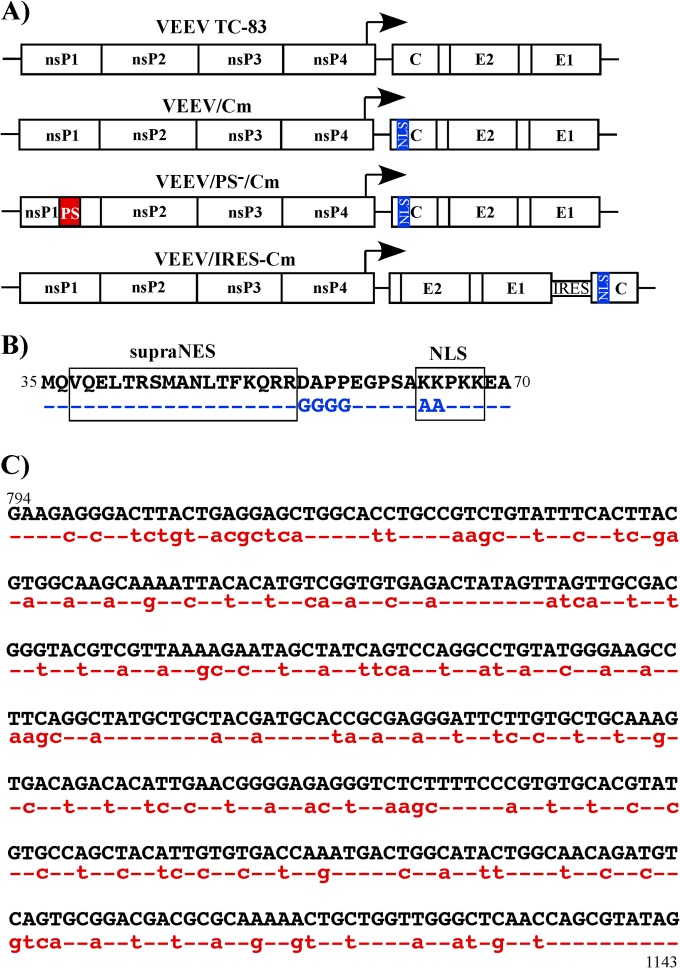
FIG 1.
Schematic representation of recombinant VEEV genomes used in the present study (A) and mutations introduced into the NLS and supraNES-NLS-connecting peptide (B) and into the PS of VEEV. Capsid-specific mutations are indicated in blue, and PS-specific mutations are indicated in red. Dashed lines indicate identical nucleotides and amino acids.
RNA transcription.
Plasmids were purified by centrifugation in CsCl gradients. They were linearized by MluI digestion, and RNAs were synthesized by using SP6 RNA polymerase in the presence of cap analog according to the manufacturer's recommendations (Invitrogen). The yield and integrity of the transcripts were analyzed by gel electrophoresis under nondenaturing conditions. Aliquots of transcription reactions were used for electroporation without additional purification.
RNA transfections.
Electroporation of BHK-21 cells was performed under previously described conditions (28). To rescue the viruses, 1 μg of in vitro-synthesized viral genome RNA was electroporated into the cells, which were then seeded into 100-mm dishes and incubated for 20 to 24 h. Under these incubation conditions, VEEV/Cm, VEEV/PS−/Cm, and VEEV/IRES-Cm did not develop any noticeable cytopathic effect (CPE) in BHK-21 cells, but the infectious titers were similar to those of rescued VEEV TC-83. Virus titers were determined using a standard plaque assay on BHK-21 cells, since these viruses remained capable of forming distinguishable plaques under agarose cover. To assess the RNA infectivity, 10-fold dilutions of electroporated BHK-21 cells were seeded in six-well Costar plates containing subconfluent naive cells. After 1 h of incubation at 37°C, cells were overlaid with 2 ml of 0.5% Ultra-Pure agarose (Invitrogen) supplemented with minimal essential medium and 3% FBS. Plaques were stained with crystal violet after 2 days' incubation at 37°C, and infectivity was determined as the PFU per μg of transfected RNA.
Viral replication analysis.
Vero or NIH 3T3 cells were seeded into 35-mm dishes at a concentration of 5 × 105 cells per well. Cells were infected at the multiplicities of infection (MOIs) indicated in the corresponding figures for 1 h at 37°C in phosphate-buffered saline (PBS) supplemented with 1% FBS, and then incubation continued in complete growth medium at 37°C. At the times indicated, the medium was replaced by fresh medium, and virus titers in the harvested samples were determined by plaque assay on BHK-21 cells.
Analysis of protein synthesis.
Cells were seeded into six-well Costar plates at a concentration of 5 × 105 cells per well. They were infected at an MOI of 20 PFU/cell, and at the times indicated in the figure legend, the cells were incubated for 30 min in 0.8 ml of Dulbecco modified Eagle medium (DMEM) lacking methionine, supplemented with 0.1% FBS and 20 μCi of [35S]methionine/ml. After this incubation, the cells were scraped, collected by centrifugation, and dissolved in 100 μl of standard protein loading buffer. Equal amounts of proteins were loaded onto each lane of the sodium dodecyl sulfate–10% polyacrylamide gels for SDS-PAGE analysis. After electrophoresis, the gels were dried, autoradiographed, and analyzed on a Storm 860 PhosphorImager (Molecular Dynamics).
Analysis of presence of viral structural proteins in the infected cells and released viral particles.
Totals of 5 × 105 NIH 3T3, Vero, and BHK-21 cells were infected at an MOI of 20 PFU/cell. At 22 h postinfection, the cells and media were harvested before the development of CPE even in VEEV TC-83-infected cells. Media were additionally clarified by centrifugation at 21,000 × g for 10 min. Viral particles were pelleted from 0.8 ml of media by ultracentrifugation through a 20% (wt/wt) sucrose cushion in a TLA55 rotor (Beckman) at 54,000 rpm for 2 h at 4°C. The cells were pelleted by centrifugation at 1,500 × g for 5 min. Cells and viral particle pellets were suspended in gel loading buffer and analyzed by SDS-PAGE, followed by Western blotting. Blots were stained with anti-VEEV TC-83 (a generous gift from R. Tesh, University of Texas Medical Branch at Galveston) and anti-β-actin antibodies, followed by a treatment of the membranes with infrared dye-labeled secondary antibodies. Quantitative analysis of the membranes was performed on a LI-COR imager. The signals were quantified in the capsid and glycoprotein bands in samples from three independent experiments, and the means and standard deviations were calculated.
Analysis of RNA synthesis.
To analyze the synthesis of the virus-specific RNAs, the infected cells were metabolically labeled with [3H]uridine (20 μCi/ml) in the presence of actinomycin D (ActD; 1 μg/ml) for 4 h, beginning at 3 h postinfection. Total cellular RNA was isolated by TRIzol, according to the procedure recommended by the manufacturer (Invitrogen), and then denatured with glyoxal in dimethyl sulfoxide and analyzed by agarose gel electrophoresis, using previously described conditions (29). Gels were impregnated with 2,5-diphenyloxazole (PPO), dried, and autoradiographed.
IFN-β measurement.
NIH 3T3 cells were infected with different viruses at MOIs indicated in the figures. Media were harvested at different times postinfection. Concentrations of IFN-β in the samples were measured with a VeriKine mouse interferon beta ELISA kit (PBL Interferon Source) according to the manufacturer's recommendations.
Animal studies.
To assess the residual virulence of the designed variants, 6-day-old NIH Swiss mice (Harlan) were inoculated subcutaneously (s.c.) with 2 × 105 or 106 PFU of the viruses diluted in PBS in a volume of 20 μl. The 6-week-old female NIH Swiss mice were infected s.c. with 106 PFU of the tested viruses in 50 μl of PBS. Animals were checked twice daily for signs of the disease or death. For some of the experiments, weight was evaluated on a daily basis. At the times indicated in the figures, randomly selected mice were euthanized, and titers of the viruses were evaluated in the serum and brain. To test the concentration of neutralizing antibodies, blood was collected from the retro-orbital sinus. For challenge experiments, mice were transferred into the ABSL3 facility of the UAB SEBLAB and challenged with 104 PFU (∼104 50% lethal dose [LD50]) of VEEV 3908. Animals were also observed twice daily. All of the protocols were approved by the UAB IBC and IACUC.
Titers of neutralizing antibodies.
Serum samples were incubated at 50°C for 1 h and then serially (2-fold) diluted in PBS containing 1% FBS and 2.5 × 102 PFU of VEEV TC-83 virus/ml. Samples were incubated at 37°C for 2.5 h with continuous shaking, and 0.2-ml aliquots were applied to BHK-21 cell monolayers. After 1 h of incubation at 37°C, the cells were covered with 0.5% agarose supplemented with DMEM and 3% FBS. Plaques were stained with crystal violet in 48 h, and the percentage of titer reduction was calculated.
RESULTS
Construct design and analysis of virus replication in vitro.
In our previous studies, we identified a number of specific sequences in capsid-coding gene and other fragments of VEEV genome, which play critical roles in virus replication and in its interaction with the host (14, 26, 28). Two of these sequences provide important targets for therapeutic development. The first is a short amino acid sequence in the VEEV capsid protein that was found to interact with importin-α/β and CRM1 and to determine VEEV's ability to cause transcriptional shutoff and interfere with the innate immune response (Fig. 1A and B). The second is a sequence between nucleotides 856 and 1150, located in the VEEV nsP1 gene and identified as a PS, which determines specificity of viral genomic RNA packaging (Fig. 1A and C). Supplementary to these findings, we also found that encephalomyocarditis virus (EMCV) internal ribosome entry site (IRES) and IRESs derived from hepatitis C virus and bovine viral diarrhea virus were nonfunctional in insect cells and could be used to modify the expression strategy of alphavirus-specific proteins (Fig. 1A) (10, 21, 30), thus restricting virus replication to vertebrate cells. These three findings provided a basis for the design of a new vaccine candidate against VEEV. Our goal in the present study was to utilize the accumulated data for designing recombinant variants of VEEV that would be more attenuated than the currently available VEEV TC-83 live experimental vaccine. In addition to being significantly attenuated, these variants would need to induce a protective immune response, produce high levels of RNA replication and structural protein production, and have a stable attenuated phenotype.
Since VEEV TC-83 is already significantly attenuated compared to wt virus, its infectious cDNA clone was used for further modifications. VEEV TC-83 was also used as a control to demonstrate the residual level of pathogenicity. The first designed variant VEEV/Cm contained six redundant mutations in the capsid protein (Fig. 1A and B), which were located in the nuclear localization sequence (NLS) and a short peptide connecting the capsid-specific supraNES and NLS. The second recombinant VEEV/PS−/Cm contained the same capsid-specific mutations and 135 mutations in the PS, which did not change the encoded amino acid sequence (Fig. 1). In the third variant, VEEV/IRES-Cm, the capsid gene was again mutated, but was also positioned under the control of the EMCV IRES downstream of the E1 gene at the 3′ end of the genomic RNA (Fig. 1A and B). Thus, the capsid protein of all of these viruses had no nuclear functions, and they additionally differed either in the efficiency of viral genomic RNA packaging or in the capsid expression strategy.
All of the designed variants were viable and, based on the equally high infectivity of the in vitro-synthesized RNA, their rescue did not require additional adaptive mutations (data not shown). The characteristic feature of these recovered viruses was a less cytopathic phenotype, which resulted in their inability to cause CPE in BHK-21, NIH 3T3, and Vero cells in liquid media or to develop distinguishable plaques in Vero cells under agarose cover (Fig. 2A). However, they were able to produce detectable plaques in BHK-21 cells under agarose with medium supplemented with a low concentration of FBS (see Materials and Methods for details). Thus, in this and other sections, the virus titers are presented as PFU/ml.
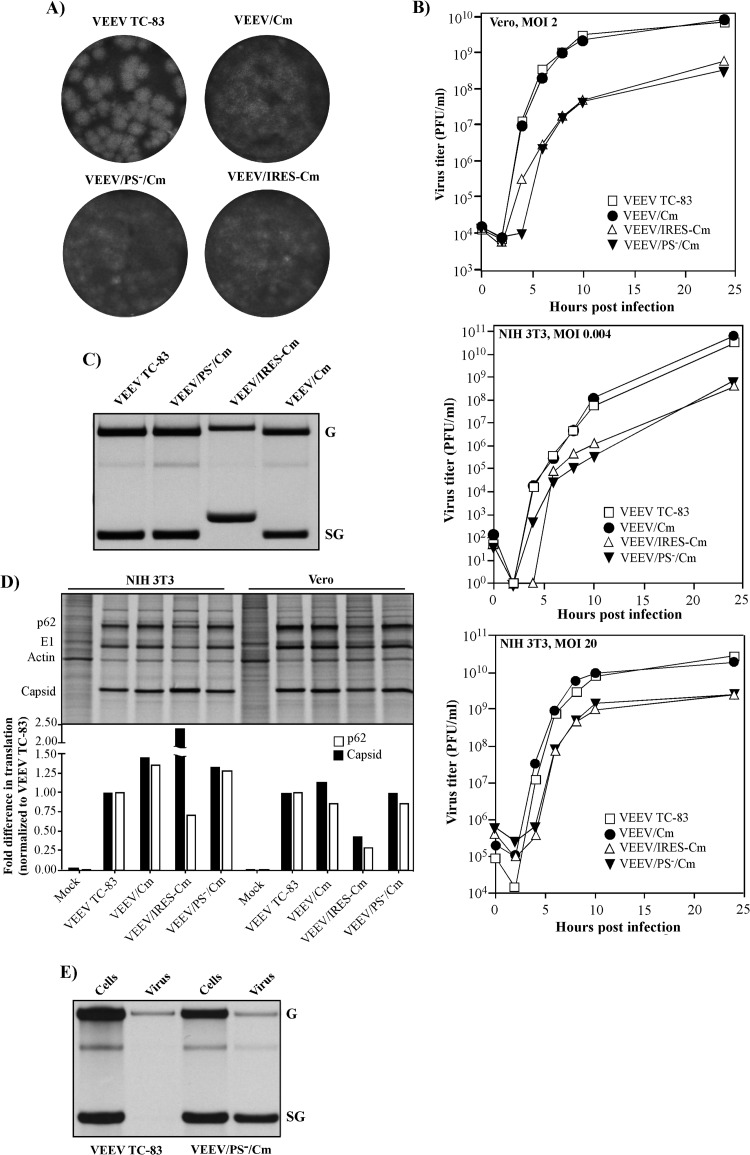
FIG 2.
Introduced mutations differentially affect in vitro replication characteristics of VEEV TC-83. (A) Capsid-specific mutations made recombinant viruses incapable of forming plaques in Vero cells. The indicated variants were titrated on Vero cells as described in Materials and Methods, and cell monolayers were stained with Crystal violet at 2 days postinfection. (B) Vero and NIH 3T3 cells were infected at the indicated MOIs, and media were replaced at the indicated time points. Virus titers were determined by plaque assay on BHK-21 cells. (C) 5 × 105 Vero cells in six-well Costar plates were infected at an MOI of 20 PFU/cell with the indicated viruses. RNAs were metabolically labeled with [3H]uridine in the presence of ActD between 3 and 7 h postinfection and analyzed by agarose gel electrophoresis in denaturing conditions (see Materials and Methods for details). (D) 5 × 105 NIH 3T3 and Vero cells in six-well Costar plates were infected with the indicated viruses at an MOI of 20 PFU/cell. At 7 h postinfection, they were metabolically labeled with [35S]methionine for 30 min, and cell lysates were analyzed by SDS-PAGE. Quantitative analysis of radioactivity in capsid and p62 glycoprotein bands was performed on a Storm phosphorimager. The data were normalized to radioactivity detected in VEEV TC-83-specific bands. (E) 5 × 105 BHK-21 cells in six-well Costar plates were infected at an MOI of 20 PFU/cell with the indicated viruses. RNAs were metabolically labeled with [3H]uridine in the presence of ActD between 14 and 20 h postinfection. The released viral particles were pelleted from the media by ultracentrifugation through 25% sucrose (see Materials and Methods for details), and RNAs were isolated from the virus pellet and cells and analyzed by agarose gel electrophoresis in denaturing conditions (see Materials and Methods for details).
The mutations introduced into capsid protein did not affect the replication rates of VEEV/Cm: its growth curves were indistinguishable from those of the original VEEV TC-83 both in Vero and NIH 3T3 cells regardless of the MOI (Fig. 2B). Mutations in the PS of VEEV/PS−/Cm and repositioning of the capsid-coding sequence under the control of the EMCV IRES in VEEV/IRES-Cm had detectable negative effects on the rates of infectious virus release in both cell lines with defects in type I IFN release (Vero) and those with no defects in IFN production and signaling (NIH 3T3). Titers of the designed mutants were always 20- to 100-fold below those of VEEV TC-83 and VEEV/Cm (Fig. 2B). Thus, all of the designed viruses demonstrated the same inability to cause CPE, at least in the tested cell lines, but differed in terms of efficiency of producing infectious virus in cell cultures.
Replication of viral RNA and synthesis of viral structural proteins.
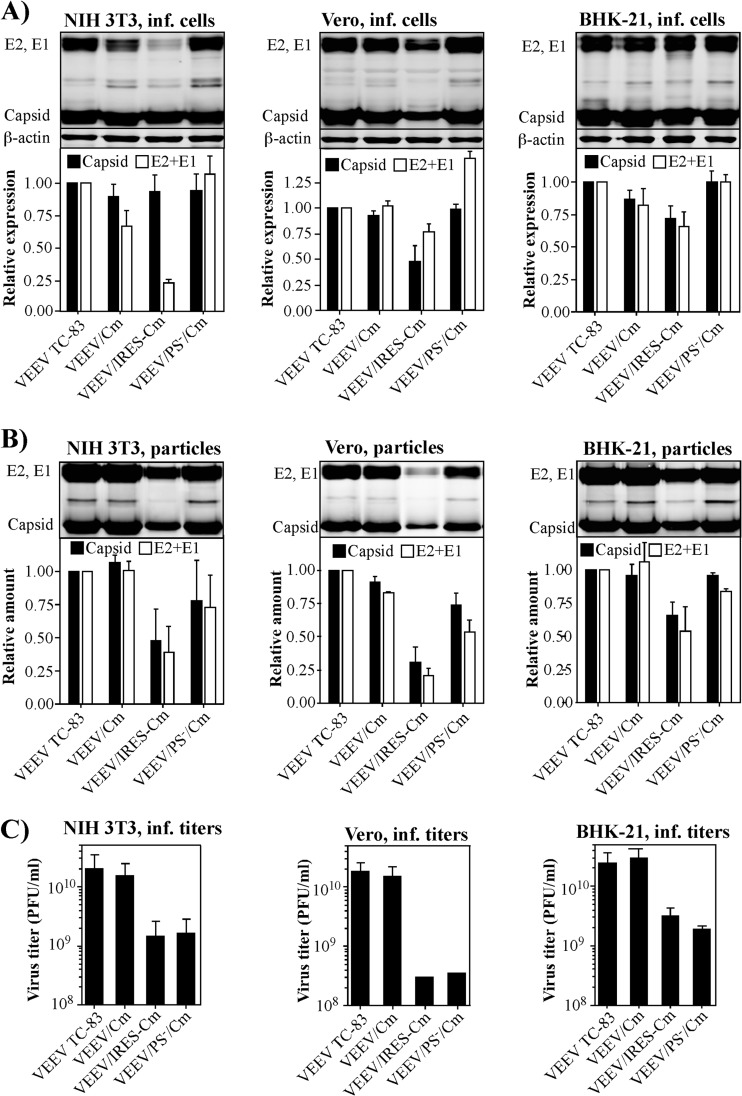
Infectious virus titers do not necessarily reflect the RNA replication rates, the rate of protein synthesis, and the rate of particle release. Since these characteristics are important for our understanding of attenuation, we assessed them in the designed mutants and the original VEEV TC-83. The results presented in Fig. 2C demonstrate that VEEV/Cm and VEEV/PS−/Cm mutants and original VEEV TC-83 were very similar in terms of rates of virus-specific RNA synthesis in Vero cells, whereas replication of VEEV/IRES-Cm genome was found to be 3-fold less efficient. The molecular basis for this difference was not further investigated, but this result correlated with lower replication rates of other previously designed, IRES-containing alphavirus mutants (21, 30). VEEV TC-83, VEEV/Cm, and VEEV/PS−/Cm demonstrated similar rates of structural protein synthesis (Fig. 2D), and only VEEV/IRES-Cm differed by exhibiting different ratios of capsid and glycoprotein translation rates (Fig. 2D). The dependence of the efficiency of capsid protein expression on the cell type suggested a cell-dependent mode of EMCV IRES function. Cell- and virus type-specific rates of synthesis of all viral structural proteins (Fig. 2D) led to different levels of accumulation of capsid and glycoproteins in VEEV/IRES-Cm-infected cells (Fig. 3A). However, the release of viral and virus-like particles (VLPs) did not exactly correlate with either structural protein synthesis or infectious titers (Fig. 3B and C). VEEV/Cm produced particles as efficiently as VEEV TC-83 and, based on the equal infectious titers, they were most likely standard genome-containing infectious virions. VEEV/PS−/Cm, in contrast, produced merely the same amount of particles, but, depending on the cell line, infectious titers were 10- to 100-fold lower. This was an indication that most of the particles did not contain viral genomic RNA but packaged large amounts of other RNAs (26). Indeed, the SG RNA, which is the most abundant mRNA in the infected cells, was found in the released virions at a molar concentration ∼30-fold higher than that of genomic RNA (Fig. 2E). In the media of VEEV/IRES-Cm-infected cells, particles were present at 2- to 4-fold lower levels, but infectious titers were lower than that, suggesting that this decrease was most likely also a result of less efficient genomic RNA packaging.
FIG 3.
PS-specific mutations and IRES-mediated capsid expression differentially affect infectious titers and structural protein expression. Totals of 5 × 105 NIH 3T3, Vero, and BHK-21 cells in six-well Costar plates were infected with the indicated viruses at an MOI of 20 PFU/cell. At 22 h postinfection, both cells and media were harvested. (A) Accumulation of VEEV structural proteins in the cells was evaluated by Western blotting with VEEV-specific Abs. Quantitative data were generated on a LI-COR imager. (B) Viral particles were pelleted from 0.8 ml of medium by ultracentrifugation (see Materials and Methods for details) and analyzed by Western blotting with VEEV-specific Abs. Quantitative data were generated on a LI-COR imager. Signals in the capsid and glycoprotein bands were determined in three independent experiments. The means and standard deviations were calculated. (C) Titers of the viruses in the same harvested media were determined by plaque assay on BHK-21 cells.
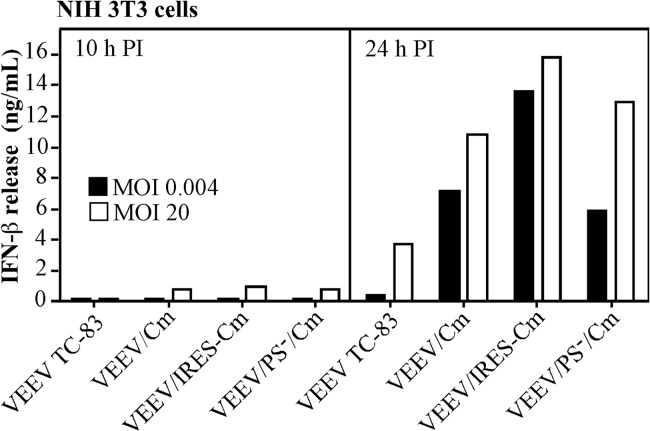
Importantly, all of the newly designed variants were unable to interfere with the development of the innate immune response. Previously, we have demonstrated that mutated VEEV capsid protein is unable to cause transcriptional shutoff (31). In accordance with these data, replication of the newly designed mutants in murine cells, which had no defects in type I IFN induction and signaling, induced release of IFN-β more efficiently than replication of VEEV TC-83. IFN-β was detectable at 10 h postinfection with mutant viruses, but not VEEV TC-83, at an MOI of 20 PFU/cell (Fig. 4), and at 24 h postinfection, particularly at low MOI, it accumulated to levels higher than that in the media of cells infected with the original VEEV TC-83. Thus, these data suggested a possibility that compared to VEEV TC-83, the VEEV/Cm variant would demonstrate an additional level of attenuation resulting from its inability to efficiently interfere with the innate immune response. VEEV/PS−/Cm and VEEV/IRES-Cm could be even more attenuated because of their inefficient packaging of the viral genome and thus decreased ability to cause viremia.
FIG 4.
Recombinant viruses are more potent inducers of IFN-β than VEEV TC-83. A total of 5 × 105 NIH 3T3 cells in six-well costar plates were infected with the indicated viruses at MOIs of 20 and 0.004 PFU/cell. Media were harvested at the indicated time points, and the concentrations of IFN-β were measured by ELISA as described in Materials and Methods.
The designed mutants are more attenuated than VEEV TC-83.
All of the in vitro-generated data of this and previous studies have shown an attenuation of VEEV capsid mutants in terms of their inability to cause CPE while also producing more efficient induction of type I IFN (13, 16). Such results strongly suggested that these mutants would also have an attenuated phenotype in vivo. To experimentally test this, the 6-day-old NIH Swiss mice were s.c. infected with 2 × 105 PFU of VEEV TC-83, VEEV/Cm, VEEV/PS−/Cm, and VEEV/IRES-Cm. At this dose, the VEEV TC-83 experimental vaccine was universally lethal, and all of the mice succumbed to the infection within 6 days postinfection (Fig. 5A). By the time of death, in these mice, VEEV TC-83 was present in the brain at concentrations ranging from 0.2 × 1010 to 2 × 1010 PFU/g. It also caused the highest levels of viremia (Fig. 5B) and was present at high concentrations in the brains starting from day 1 postinfection.
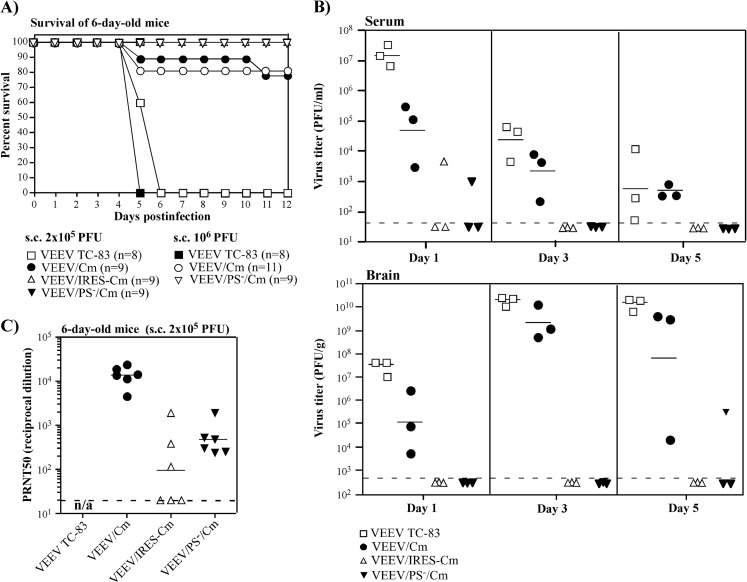
FIG 5.
Extensive mutations in VEEV capsid protein and PS, and changes in the mode of capsid protein expression, have strong negative effects on residual virulence of VEEV TC-83. Six-day-old NIH Swiss mice were infected via the s.c. route by indicated viruses and monitored for 21 days for death or signs of the disease (A). No deaths were detected after day 12 postinfection. (B) Randomly selected mice were euthanized at days 1, 3, and 5 postinfection, and virus titers in the serum and brains were evaluated. (C) At day 21 postinfection, the titers of neutralizing Abs were evaluated as described in Materials and Methods. n/a, not applicable. Dashed lines indicate the limits of detection.
As demonstrated above, mutations in capsid protein did not affect virus replication in vitro. However, they had a strong negative effect on its pathogenicity. After s.c. inoculation, VEEV/Cm caused viremia that was a few orders of magnitude lower in 6-day-old mice (Fig. 5B) but was still capable of neuroinvasion. All of the tested mice had a high concentration of virus in their brains. However, VEEV/Cm replication was fatal only in a small percentage of mice (Fig. 5A), and the surviving mice demonstrated no presence of virus in their brains at day 12 postinfection. In additional experiments, a further increase in the inoculation dose to 106 PFU did not cause higher lethality and, once again, 20% of mice succumbed to the infection within 12 days (Fig. 5A). All of the mice that received the same s.c. dose of VEEV TC-83 were either dead or euthanized due to the development of severe paralysis within 5 days.
Additional mutations in the PS (VEEV/PS−/Cm) or expression of the mutated capsid protein from the EMCV IRES (VEEV/IRES-Cm) led to higher virus attenuation. No mice died in experiments with these VEEV variants at either 2 × 105 or 2 × 106 PFU inoculation doses. These viruses rarely induced detectable viremia, and in these experiments, the low level of viremia that was present could only be detected at day 1 postinoculation. Only one mouse demonstrated presence of low titer of VEEV/PS−/Cm in the brain at day 5 postinfection, and one mouse was positive for the presence of VEEV/IRES-Cm in the brain at day 8 postinfection (data not shown). Thus, VEEV/PS−/Cm and VEEV/IRES-Cm had dramatically reduced neuroinvasion potential and were less pathogenic than VEEV TC-83 and even than VEEV/Cm.
After s.c. infection with 2 × 105 PFU of VEEV/Cm and VEEV/PS−/Cm, all of the suckling mice seroconverted (Fig. 5C). At day 21 postinfection, they demonstrated presence of high levels of VEEV TC-83-neutralizing Abs. Based on the inability to cause viremia, it was not surprising to find that VEEV/PS−/Cm induced lower levels of neutralizing Abs. VEEV/IRES-Cm was less efficient again in antibody induction. Only half of the infected mice seroconverted, and the use of higher infectious doses did not produce a noticeable increase in Abs.
Thus, the results of the experiments with suckling mice demonstrated that capsid-specific mutations strongly attenuated VEEV TC-83. They did not make VEEV/Cm incapable of invading the brain but caused a profound decrease in its virulence. Additional mutations, such as inactivation of PS or relocation of capsid protein gene under the control of the EMCV IRES additionally affected viremia development. This likely resulted in reduced neuroinvasiveness.
VEEV TC-83 mutants develop protective immune response in adult mice.
Safety is an important characteristic for any vaccine candidate, but another critical parameter is the efficiency of the induced immune response against subsequent infection, which strongly depends on the level of neutralizing Abs. In subsequent experiments, 6-week-old NIH Swiss mice were infected with 106 PFU of VEEV TC-83, VEEV/Cm, VEEV/PS−/Cm, and VEEV/IRES-Cm via the s.c. route. The original VEEV TC-83 produced viremia, which was readily detectable at days 1 and 2 postinfection (Fig. 6A). At day 2, it was also found in the brains of tested mice (Fig. 6A). Mutations in capsid-encoded NLS made VEEV/Cm, VEEV/PS−/Cm, and VEEV/IRES-Cm incapable of inducing viremia in adult mice (Fig. 6A), and no virus presence was detected in the brains. None of the mice demonstrated any visible signs of disease and maintained their weight at all times postinfection (Fig. 6B). Nevertheless, all of the mutants remained immunogenic (Fig. 6C). After single immunization with VEEV/Cm, titers of neutralizing antibodies were indistinguishable from those induced by immunization with VEEV TC-83. VEEV/PS−/Cm and VEEV/IRES-Cm were less efficient in terms of antibody induction. The lower 50% plaque reduction neutralization test (PRNT50) titers generally correlated with less efficient virus replication in vitro (Fig. 2B), and in vivo (Fig. 6A). Neutralizing antibodies were present at high concentrations in adult mice by day 14 postinfection, and by day 35 postinfection, no obvious increase in PRNT50 titers was detected.
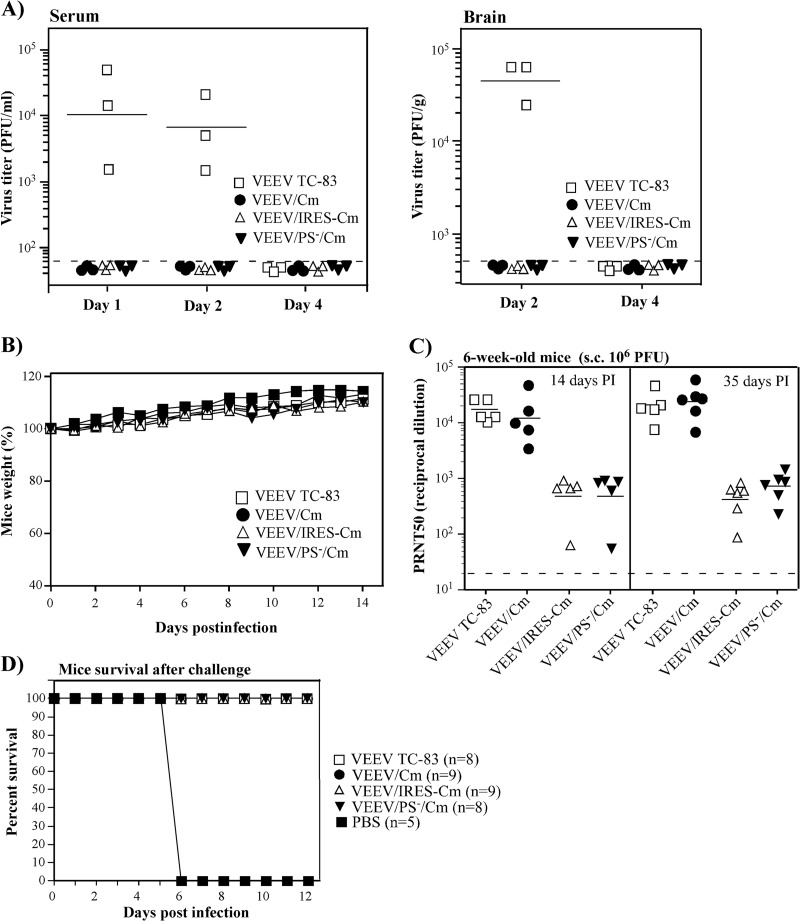
FIG 6.
The designed mutants are more attenuated than VEEV TC-83 but remain immunogenic in 6-week-old NIH Swiss mice. Six-week-old NIH Swiss mice were infected via s.c. route with 106 PFU of the indicated viruses. (A) At days 1, 2, and 4 postinfection, randomly selected mice were euthanized, and virus titers in the brain and viremia levels were evaluated. (B) Mice were monitored daily in terms of weight change. (C) The titers of neutralizing, anti-VEEV TC-83 Abs were evaluated at days 14 and 35 postinfection (see Materials and Methods for details). At day 45 postinfection, mice were s.c. infected with 104 PFU of epizootic VEEV strain 3908. The mice were monitored for 21 days for signs of the disease and death. No death was detected after day 6 postinfection. Dashed lines indicate the limits of detection in these experiments.
Considering the high titers of neutralizing antibodies, it was not surprising to find that mice immunized with any of the above constructs were protected against subsequent infection with the highly pathogenic epizootic VEEV strain 3908 (Fig. 6D). Immunized mice, infected via the s.c. route with 104 PFU of VEEV 3908 (∼104 LD50) developed none of the indications of disease, such as ruffled fur, change in behavior or paralysis. Sham-vaccinated mice succumbed to the infection within 5 days.
Taken together, the accumulated data demonstrate that additional extensive modifications introduced into the VEEV TC-83 genome strongly diminished the residual reactogenicity of this experimental vaccine. Despite introduced extensive changes in nucleotide and protein sequences, these combinations of mutations did not lead to overattenuation. These viruses remained capable of inducing high titers of neutralizing antibodies in mice, and they were sufficient for protection against high doses of virulent, epizootic VEEV 3908.
DISCUSSION
Despite the continuous public health threat, no safe and efficient vaccine has been developed thus far against any alphavirus infection. Inactivated and subunit vaccine candidates demonstrate poor efficacy, are very expensive, and require multiple boosters for continuous support of detectable levels of neutralizing Abs. The designed live attenuated vaccine candidates, such as VEEV TC-83 (6, 7), and genetically modified VEEV with inactivated cleavage sites between E3 and E2 (32) exhibit significant levels of reactogenicity (33) and can cause symptomatic diseases in humans. The experimental VEEV TC-83 vaccine is efficient in terms of induction of a protective immune response (6, 7, 10, 34), but its attenuated phenotype relies on two point mutations in the 5′UTR and E2 glycoprotein-coding sequence (9). Thus, VEEV TC-83 readily reverts to a wt pathogenic phenotype within a few passages in vivo (10). TC-83 also retains the possibility for transmission by mosquito vectors, which represent a reservoir for its evolution (35). There is ongoing research to develop DNA vaccines (36, 37) or VLP vaccines (38), but it is difficult to expect that they will be able to induce protective immunity comparable to that produced by live VEEV TC-83.
Previously, a widely used approach for the selection of vaccine candidates was based on serial passage of the originally pathogenic viruses in cultured cells, chicken embryos, or the brains of newborn mice (6, 39). Sometimes, chemical mutagenesis was also applied to increase the diversity of virus variants in the original population (40). However, these methods rely on the selection of limited numbers of point mutations and do not provide plausible mechanistic explanation for attenuation, and the final variants have strong potential for reversion to a pathogenic phenotype.
Construction of infectious cDNA clones of VEEV and other alphaviruses (41, 42) and the efficient means of genetic manipulations and virus rescue (43) provided an opportunity for application of new approaches to design safe and efficient vaccine candidates. In plasmid form, viral genomes can be strongly modified to ultimately achieve higher levels of attenuation. However, a very important characteristic of alphaviruses was found to be their outstanding plasticity and strong tendency to rapid evolution, resulting in the accumulation of adaptive mutations and development of more efficiently replicating phenotypes in vitro and/or higher pathogenesis in vivo (44, 45). Thus, neither modification of the promoters (45) nor modification of the cleavage site between E3 and E2 (46) made VEEV incapable of further evolution to a more pathogenic phenotype.
In the present study, we applied recent advances in the understanding of alphavirus replication to design new nonpathogenic VEEV variants, which have a potential for application as live vaccine candidates. Their most important characteristics are summarized in Table 1. The general strategy was to combine extensive sets of attenuating mutations affecting different aspects of virus replication and virus-host interactions and thus to reduce the possibility of the reversion to pathogenic phenotype. In order to minimize possible negative effects on the immunogenicity of the virus, the introduced mutations were expected to cause little or no effect on the efficiency of viral RNA and protein synthesis. The basic strain used for modification was VEEV TC-83, which is already at least partially attenuated for humans and adult mice. However, it is universally lethal for <6-day-old mice and causes a disease of varying severity in 40% of vaccinees (11). Based on the results of studies of the molecular basis of VEEV pathogenesis (14, 15), the first set of additional attenuating mutations was introduced into capsid protein. These mutations would make capsid protein incapable of interfering with nucleocytoplasmic traffic and cellular transcription, without affecting the ability to form nucleocapsids and viral particles. These redundant mutations made VEEV TC-83 dramatically less cytopathic (Fig. 2A) and incapable of interfering with the innate immune response (Fig. 4). It retained an ability to replicate in vitro as efficiently as the original VEEV TC-83 but induced lower levels of viremia in suckling mice and no viremia in older mice. It also lost the ability for neuroinvasion in adult mice and became dramatically less virulent in suckling mice. However, it remained highly immunogenic, and a single immunization elicited levels of neutralizing Abs, which were comparable to those induced by TC-83. They protected mice against high doses of challenge virus. This was not the first attempt to attenuate RNA viruses by making them incapable of interfering with the induction of the innate immune response. The most representative examples are probably attenuation of the Rift Valley fever virus via deletions of NSs fragments or the entire gene (47), and variants of influenza virus with deletions in the NS1 gene (48, 49). Similar to these deletion mutants, VEEV/Cm became a more potent type I IFN inducer and became incapable of developing a spreading infection in cells without defects in type I IFN production and signaling. Our previous studies also demonstrated noncytopathic clearance of such mutants from already infected IFN-competent cells (16).
TABLE 1.
Summary of characteristics of the newly designed variants and the original VEEV TC-83
| Condition | Mouse age group | VEEV variant |
|||
|---|---|---|---|---|---|
| VEEV TC-83 | VEEV/Cm | VEEV/PS−/Cm | VEEV/IRES-Cm | ||
| Viremia | Suckling | +++ | +++ | ++ | ++ |
| Adult | +++ | −−− | −−− | −−− | |
| Neuroinvasiveness | Suckling | +++ | +++ | +−− | +−− |
| Adult | +++ | −−− | −−− | −−− | |
| Virulence | Suckling | +++ | −−− | −−− | −−− |
| Adult | −−− | −−− | −−− | −−− | |
| Seroconversion | Suckling | +++ | +++ | ++ | + |
| Adult | +++ | +++ | ++ | ++ | |
In an attempt to further attenuate VEEV, we introduced numerous mutations into PS of VEEV/Cm. These mutations did decrease the infectious titers of the released virions in vitro but did not affect structural protein expression and appeared to have a very small effect on the numbers of released particles. Thus, as we described previously, most of the released virions were probably genome-free (26). The 135 mutations in PS introduced an additional level of attenuation (Table 1). They strongly affected both viremia development and neuroinvasiveness of the virus, even in suckling mice. VEEV/PS−/Cm induced a rarely detectable, low-level viremia in 6-day-old mice, and no viremia was ever detected in older mice. Suckling mice demonstrated no visible signs of the disease, and no death was detected among these or older mice even when infected with 106 PFU. The inability to cause viremia had a negative effect on the titers of induced neutralizing Abs. They became 10-fold lower than those induced by VEEV TC-83 or VEEV/Cm. However, VEEV/PS−/Cm remained immunogenic with all of the mice seroconverting, and a single immunization protected them against challenge with VEEV 3908. An important benefit of the lack of viremia was the reduced possibility for transmission of VEEV/PS−/Cm to mosquitoes. Without a high concentration of virus in the blood, it is highly unlikely that such a mutant can be transmitted to mosquitoes during the blood meal. However, this possibility should be further investigated.
The third mutant was designed according to a strategy that we had previously developed for alphaviruses to reduce their replication levels and place capsid production under the control of an IRES (10, 21, 22, 30). This was achieved by positioning mutated capsid, but not the glycoprotein genes under the control of the EMCV IRES. IRES-dependent capsid expression completely abolishes virus replication in mosquito cells. However, it has also detectable negative effects on the balance of expression of viral structural proteins, particle formation and release. This balance of expression is also dependent on the cell type used in the experiments. This in turn affects induction of neutralizing Abs. Compared to similar constructs encoding wt VEEV capsid protein (10), the newly developed variant, was less virulent in suckling mice and less efficient in neutralizing antibody induction. VEEV/IRES-Cm demonstrated no ability to cause viremia or invade the brain of adult mice, caused very rare, low-level viremia in suckling mice, and was found in the brain of only one mouse, which exhibited no sign of the disease. However, we consider its performance below those of VEEV/Cm and VEEV/PS−/Cm, because not all of the suckling mice demonstrated seroconversion.
Taken together, this new study demonstrates that VEEV can be strongly attenuated while remaining immunogenic (see Table 1 for details). The new levels of attenuation can be achieved by using novel approaches, which are based on the results of basic research. The newly designed variants combine a variety of characteristics, each of which contribute to a reduction in their virulence. (i) They all contain the point mutation in the 5′UTR that makes replication of the originally developed VEEV TC-83 less resistant to type I IFN (50). (ii) They also contain mutations in the E2 glycoprotein, which make it more efficient in binding to heparin sulfate and consequently, more infectious for cultured cells and additionally attenuated in vivo. (iii) The new constructs encode a noncytopathic capsid protein, which is incapable of interfering with the innate immune response. The introduced mutations strongly affected the residual neurovirulence of TC-83. (iv) Two variants, VEEV/PS−/Cm and VEEV/IRES-Cm, contained additional extensive mutations, which lead to less efficient packaging of viral genomes and lower infectious titers, but have only a minor effect on particle release. They also produce no detectable viremia in adult mice, with rare and short-term viremia in suckling mice. Their ability for neuroinvasion in suckling mice is strongly affected.
Thus, all of the newly designed VEEV mutants are less neurovirulent than the original VEEV TC-83, and at least two of them, VEEV/PS−/Cm and VEEV/IRES-Cm, are less neuroinvasive. Nevertheless, all of them retained immunogenicity, at least in the mouse model used here. It is likely that similar approaches can be applied to other encephalitogenic NW alphaviruses since they are similar to VEEV in terms of replication strategy and virus-host interactions.
ACKNOWLEDGMENTS
We thank Niall J. Foy for helpful discussions, critical readings, and editing of the manuscript. We also thank Scott Weaver for providing plasmid encoding infectious cDNA of VEEV 3908 strain genome.
This study was supported by Public Health Service grants AI095449, AI093592, AI073301, and AI070207.
REFERENCES
- 1.Strauss JH, Strauss EG. 1994. The alphaviruses: gene expression, replication, evolution. Microbiol Rev 58:491–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weaver SC, Barrett AD. 2004. Transmission cycles, host range, evolution and emergence of arboviral disease. Nat Rev Microbiol 2:789–801. doi: 10.1038/nrmicro1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin DE. 2001. Alphaviruses, p 917–962. In Knipe DM, Howley PM (ed), Fields virology, 4th ed. Lippincott/Williams & Wilkins Co, New York, NY. [Google Scholar]
- 4.Weaver SC, Frolov I. 2005. Togaviruses, p 1010–1024. In Mahy BWJ, Meulen VT (ed), Virology, vol 2 ASM Press, Salisbury, United Kingdom. [Google Scholar]
- 5.Bronze MS, Huycke MM, Machado LJ, Voskuhl GW, Greenfield RA. 2002. Viral agents as biological weapons and agents of bioterrorism. Am J Med Sci 323:316–325. doi: 10.1097/00000441-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Alevizatos AC, McKinney RW, Feigin RD. 1967. Live, attenuated Venezuelan equine encephalomyelitis virus vaccine. I. Clinical effects in man. Am J Trop Med Hyg 16:762–768. [PubMed] [Google Scholar]
- 7.Berge TO, Banks IS, Tigertt WD. 1961. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea pig heart cells. Am J Hyg 73:209–218. [Google Scholar]
- 8.Kinney RM, Johnson BJ, Welch JB, Tsuchiya KR, Trent DW. 1989. The full-length nucleotide sequences of the virulent Trinidad donkey strain of Venezuelan equine encephalitis virus and its attenuated vaccine derivative, strain TC-83. Virology 170:19–30. doi: 10.1016/0042-6822(89)90347-4. [DOI] [PubMed] [Google Scholar]
- 9.Kinney RM, Chang GJ, Tsuchiya KR, Sneider JM, Roehrig JT, Woodward TM, Trent DW. 1993. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J Virol 67:1269–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guerbois M, Volkova E, Forrester NL, Rossi SL, Frolov I, Weaver SC. 2013. IRES-driven expression of the capsid protein of the Venezuelan equine encephalitis virus TC-83 vaccine strain increases its attenuation and safety. PLoS Negl Trop Dis 7:e2197. doi: 10.1371/journal.pntd.0002197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKinney RW, Berge TO, Sawyer WD, Tigertt WD, Crozier D. 1963. Use of an attenuated strain of Venezuelan equine encephalomyelitis virus for immunization in man. Am J Trop Med Hyg 12:597–603. [DOI] [PubMed] [Google Scholar]
- 12.Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. 1996. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine 14:337–343. doi: 10.1016/0264-410X(95)00168-Z. [DOI] [PubMed] [Google Scholar]
- 13.Atasheva S, Kim DY, Akhrymuk M, Morgan DG, Frolova EI, Frolov I. 2013. Pseudoinfectious Venezuelan equine encephalitis virus: a new means of alphavirus attenuation. J Virol 87:2023–2035. doi: 10.1128/JVI.02881-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atasheva S, Fish A, Fornerod M, Frolova EI. 2010. Venezuelan equine Encephalitis virus capsid protein forms a tetrameric complex with CRM1 and importin alpha/beta that obstructs nuclear pore complex function. J Virol 84:4158–4171. doi: 10.1128/JVI.02554-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Atasheva S, Garmashova N, Frolov I, Frolova E. 2008. Venezuelan equine encephalitis virus capsid protein inhibits nuclear import in Mammalian but not in mosquito cells. J Virol 82:4028–4041. doi: 10.1128/JVI.02330-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atasheva S, Krendelchtchikova V, Liopo A, Frolova E, Frolov I. 2010. Interplay of acute and persistent infections caused by Venezuelan equine encephalitis virus encoding mutated capsid protein. J Virol 84:10004–10015. doi: 10.1128/JVI.01151-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garmashova N, Gorchakov R, Frolova E, Frolov I. 2006. Sindbis virus nonstructural protein nsP2 is cytotoxic and inhibits cellular transcription. J Virol 80:5686–5696. doi: 10.1128/JVI.02739-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garmashova N, Gorchakov R, Volkova E, Paessler S, Frolova E, Frolov I. 2007. The Old World and New World alphaviruses use different virus-specific proteins for induction of transcriptional shutoff. J Virol 81:2472–2484. doi: 10.1128/JVI.02073-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akhrymuk I, Kulemzin SV, Frolova EI. 2012. Evasion of the innate immune response: the Old World alphavirus nsP2 protein induces rapid degradation of Rpb1, a catalytic subunit of RNA polymerase II. J Virol 86:7180–7191. doi: 10.1128/JVI.00541-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gorchakov R, Frolova E, Sawicki S, Atasheva S, Sawicki D, Frolov I. 2008. A new role for ns polyprotein cleavage in Sindbis virus replication. J Virol 82:6218–6231. doi: 10.1128/JVI.02624-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim DY, Atasheva S, Foy NJ, Wang E, Frolova EI, Weaver S, Frolov I. 2011. Design of chimeric alphaviruses with a programmed, attenuated, cell type-restricted phenotype. J Virol 85:4363–4376. doi: 10.1128/JVI.00065-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang E, Kim DY, Weaver SC, Frolov I. 2011. Chimeric Chikungunya viruses are nonpathogenic in highly sensitive mouse models but efficiently induce a protective immune response. J Virol 85:9249–9252. doi: 10.1128/JVI.00844-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang E, Volkova E, Adams AP, Forrester N, Xiao SY, Frolov I, Weaver SC. 2008. Chimeric alphavirus vaccine candidates for Chikungunya. Vaccine 26:5030–5039. doi: 10.1016/j.vaccine.2008.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Volkova E, Gorchakov R, Frolov I. 2006. The efficient packaging of Venezuelan equine encephalitis virus-specific RNAs into viral particles is determined by nsP1-3 synthesis. Virology 344:315–327. doi: 10.1016/j.virol.2005.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frolova E, Frolov I, Schlesinger S. 1997. Packaging signals in alphaviruses. J Virol 71:248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim DY, Firth AE, Atasheva S, Frolova EI, Frolov I. 2011. Conservation of a packaging signal and the viral genome RNA packaging mechanism in alphavirus evolution. J Virol 85:8022–8036. doi: 10.1128/JVI.00644-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petrakova O, Volkova E, Gorchakov R, Paessler S, Kinney RM, Frolov I. 2005. Noncytopathic replication of Venezuelan equine encephalitis virus and eastern equine encephalitis virus replicons in mammalian cells. J Virol 79:7597–7608. doi: 10.1128/JVI.79.12.7597-7608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garmashova N, Atasheva S, Kang W, Weaver SC, Frolova E, Frolov I. 2007. Analysis of Venezuelan equine encephalitis virus capsid protein function in the inhibition of cellular transcription. J Virol 81:13552–13565. doi: 10.1128/JVI.01576-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bredenbeek PJ, Frolov I, Rice CM, Schlesinger S. 1993. Sindbis virus expression vectors: packaging of RNA replicons by using defective helper RNAs. J Virol 67:6439–6446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volkova E, Frolova E, Darwin JR, Forrester NL, Weaver SC, Frolov I. 2008. IRES-dependent replication of Venezuelan equine encephalitis virus makes it highly attenuated and incapable of replicating in mosquito cells. Virology 377:160–169. doi: 10.1016/j.virol.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Atasheva S, Akhrymuk M, Frolova EI, Frolov I. 2012. New PARP gene with an anti-alphavirus function. J Virol 86:8147–8160. doi: 10.1128/JVI.00733-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis NL, Powell N, Greenwald GF, Willis LV, Johnson BJB, Smith JF, Johnston RE. 1991. Attenuating mutations in the E2 glycoprotein gene of Venezuelan equine encephalitis: construction of single and multiple mutants in a full-length clone. Virology 183:20–31. doi: 10.1016/0042-6822(91)90114-Q. [DOI] [PubMed] [Google Scholar]
- 33.Wang E, Petrakova O, Adams AP, Aguilar PV, Kang W, Paessler S, Volk SM, Frolov I, Weaver SC. 2007. Chimeric Sindbis/eastern equine encephalitis vaccine candidates are highly attenuated and immunogenic in mice. Vaccine 25:7573–7581. doi: 10.1016/j.vaccine.2007.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paessler S, Fayzulin RZ, Anishchenko M, Greene IP, Weaver SC, Frolov I. 2003. Recombinant Sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. J Virol 77:9278–9286. doi: 10.1128/JVI.77.17.9278-9286.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pedersen CE Jr, Robinson DM, Cole FE Jr. 1972. Isolation of the vaccine strain of Venezuelan equine encephalomyelitis virus from mosquitoes in Louisiana. Am J Epidemiol 95:490–496. [DOI] [PubMed] [Google Scholar]
- 36.Donnelly JJ, Wahren B, Liu MA. 2005. DNA vaccines: progress and challenges. J Immunol 175:633–639. doi: 10.4049/jimmunol.175.2.633. [DOI] [PubMed] [Google Scholar]
- 37.Dupuy LC, Richards MJ, Ellefsen B, Chau L, Luxembourg A, Hannaman D, Livingston BD, Schmaljohn CS. 2011. A DNA vaccine for venezuelan equine encephalitis virus delivered by intramuscular electroporation elicits high levels of neutralizing antibodies in multiple animal models and provides protective immunity to mice and nonhuman primates. Clin Vaccine Immunol 18:707–716. doi: 10.1128/CVI.00030-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akahata W, Yang ZY, Andersen H, Sun S, Holdaway HA, Kong WP, Lewis MG, Higgs S, Rossmann MG, Rao S, Nabel GJ. 2010. A virus-like particle vaccine for epidemic Chikungunya virus protects nonhuman primates against infection. Nat Med 16:334–338. doi: 10.1038/nm.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee T, Komiya T, Watanabe K, Aizawa C, Hashimoto H. 1995. Immune response in mice infected with the attenuated Japanese encephalitis vaccine strain SA14-14-2. Acta Virol 39:161–164. [PubMed] [Google Scholar]
- 40.Morrill JC, Carpenter L, Taylor D, Ramsburg HH, Quance J, Peters CJ. 1991. Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine 9:35–41. doi: 10.1016/0264-410X(91)90314-V. [DOI] [PubMed] [Google Scholar]
- 41.Davis NL, Willis LV, Smith JF, Johnston RE. 1989. In vitro synthesis of infectious Venezuelan equine encephalitis virus RNA from a cDNA clone: analysis of a viable deletion mutant. Virology 171:189–204. doi: 10.1016/0042-6822(89)90526-6. [DOI] [PubMed] [Google Scholar]
- 42.Rice CM, Levis R, Strauss JH, Huang HV. 1987. Production of infectious RNA transcripts from Sindbis virus cDNA clones: mapping of lethal mutations, rescue of a temperature-sensitive marker, and in vitro mutagenesis to generate defined mutants. J Virol 61:3809–3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liljeström P, Lusa S, Huylebroeck D, Garoff H. 1991. In vitro mutagenesis of a full-length cDNA clone of Semliki Forest virus: the small 6,000-molecular-weight membrane protein modulates virus release. J Virol 65:4107–4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Michel G, Petrakova O, Atasheva S, Frolov I. 2007. Adaptation of Venezuelan equine encephalitis virus lacking 51-nt conserved sequence element to replication in mammalian and mosquito cells. Virology 362:475–487. doi: 10.1016/j.virol.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gorchakov R, Hardy R, Rice CM, Frolov I. 2004. Selection of functional 5′ cis-acting elements promoting efficient Sindbis virus genome replication. J Virol 78:61–75. doi: 10.1128/JVI.78.1.61-75.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pratt WD, Davis NL, Johnston RE, Smith JF. 2003. Genetically engineered, live attenuated vaccines for Venezuelan equine encephalitis: testing in animal models. Vaccine 21:3854–3862. doi: 10.1016/S0264-410X(03)00328-1. [DOI] [PubMed] [Google Scholar]
- 47.Lihoradova O, Ikegami T. 2014. Countermeasure development for Rift Valley fever: deletion, modification or targeting of major virulence factor. Future Virol 9:27–39. doi: 10.2217/fvl.13.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chambers TM, Quinlivan M, Sturgill T, Cullinane A, Horohov DW, Zamarin D, Arkins S, Garcia-Sastre A, Palese P. 2009. Influenza A viruses with truncated NS1 as modified live virus vaccines: pilot studies of safety and efficacy in horses. Equine Vet J 41:87–92. doi: 10.2746/042516408X371937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Quinlivan M, Zamarin D, Garcia-Sastre A, Cullinane A, Chambers T, Palese P. 2005. Attenuation of equine influenza viruses through truncations of the NS1 protein. J Virol 79:8431–8439. doi: 10.1128/JVI.79.13.8431-8439.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.White LJ, Wang JG, Davis NL, Johnston RE. 2001. Role of alpha/beta interferon in Venezuelan equine encephalitis virus pathogenesis: effect of an attenuating mutation in the 5′ untranslated region. J Virol 75:3706–3718. doi: 10.1128/JVI.75.8.3706-3718.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]