Abstract
Background: Dysfunction in the kinetic chain caused by poor scapula stabilization can contribute to shoulder injuries and Shoulder Impingement Syndrome (SIS). The purpose of this study was to compare the effectiveness of two treatment approaches scapular stabilization based exercise therapy and physical therapy in patients with SIS.
Methods: The study is a randomized clinical trial in which 68 patients with SIS were randomly assigned in two groups of exercise therapy (ET) and physical therapy (PT) and received 18 sessions of treatment. Pain, shoulders' range of abduction and external rotation, shoulder protraction, scapular rotation and symmetry as well as postural assessment and Pectoralis minor length were evaluated pre and post intervention. The paired-sample t test and the independent sample t test were applied respectively to determine the differences in each group and between two groups.
Results: Our findings indicated significant differences in abduction and external rotation range, improvement of forward shoulder translation and increase in the flexibility of the involved shoulder between the two groups (respectively ; p=0.024, p=0.001, p<0/0001, p<0/0001). No significant difference was detected in pain reduction between the groups (p=0.576). Protraction of the shoulder (p<0.0001), forward head posture (p<0/0001) and mid thoracic curvature (p<0.0001) revealed a significant improvement in the ET group. Apparent changes occurred in scapular rotation and symmetry in both groups but no significant differences were observed between the two groups (respectively; p=0.183, p=0.578).
Conclusion: The scapular stabilization based exercise intervention was successful in increasing shoulder range, decreasing forward head and shoulder postures and Pectoralis minor flexibility.
Keywords: Shoulder Impingement Syndromes, Posture, Exercise Therapy, Physical Therapy
Introduction
Shoulder impingement syndrome (SIS) is a common complaint for patients of all ages and different activity levels. It has been defined as compression and mechanical abrasion of the rotator cuff structures as they pass beneath the coracoacromial arch during elevation of the arm (1). A wide range of different factors is involved in causing SIS: including anatomic abnormalities of the coracoacromial arch or humeral head (2), tension overload ischemia (3), repetitive eccentric overload (2-3), aberrant kinematic patterns due to poor rotator cuff or scapular muscles function (2,4-5), and poor posture and scapular kinematic abnormalities (2) . People who are constantly doing repetitive overhead motions relate to their occupations or athletic activities are also at risk of SIS (1, 6). Pain and dysfunction of patient with SIS occur when the shoulder is placed in positions of elevation, an activity that is commonplace during many sporting and daily living activities. Patients usually complain a general loss of strength in shoulder girdle muscles during working. Thus, the patients are at risk of losing their physical independence and jobs which have important socioeconomic implications.
The scapular position and motions on the thorax is a critical component of the normal glenohumeral function and plays great roles in facilitating optimal shoulder movements (6-8). In normal upper-quarter function, the scapula provides a stable base from which glenohumeral mobility occurs. Stability of the scapula depends on the surrounding musculature. These muscles must dynamically position the glenoid so that efficient glenohumeral movement can occur. During all movements of the glenohumeral joint especially overhead elevation of the arm, it is of great importance that the scapular-stabilizing musculature should be strong enough to properly position the scapula. The main scapula stabilizers are the Levator Scapulae, Rhomboids major and minor, Serratus anterior, and Trapezii. These muscle groups function through synergistic co-contraction with rotator cuff to control the scapular movement (9). When weakness or dysfunction is present in the scapular musculature, normal scapular positioning and mechanics may become altered which result in abnormal stresses to the capsular structures, rotator cuff compression and reduced performance (7).
There are some evidences suggesting that kinematic of scapulothoracic motions were impaired in SIS (2, 4, 9-10).
The scapulothoracic kinematics can be altered in response to inappropriate or incorrect movement pattern, macro and micro traumatic injuries, abnormal scapulohumeral rhythm and other shoulder pathologies (8,10). Altered muscle activity in the scapular muscles is commonly believed to be a crucial factor contributing to SIS (2,11-12). The scapulothoracic kinematics are also affected by abnormal posture of thoracic and cervical spine (13). Warner et al. demonstrated a pattern of increased scapular winging with glenohumeral elevation. This winging pattern appears to represent scapular internal rotation and anterior tilting (14). Recently, 3-dimensional kinematic analysis has demonstrated decreased scapular posterior tilt, decreased upward rotation, and decreased scapular external rotation during glenohumeral elevation in SIS patients (2,5).
The treatment of SIS is % 90 -95 conservative and often includes rotator cuff strengthening exercises (6,15), stretching exercises (16), immobilization, passive, active and active assisted range of motion exercises (ROM), various mobilization techniques, home exercise programs (17) and various physical therapy methods such as heat, transcutaneous electrical nerve stimulation (TENS) and ultrasound (US) and etc (18-19). In a conservative approach, exercise therapy is often being used and has an important role in shoulder rehabilitation. New insights in shoulder rehabilitation emphasize the dynamic stabilization of the scapula as an essential part of the management because the ability to position and control movements of the scapula is very important for optimal upper limb function. When the scapula fails to perform its stabilization role, shoulder function is inefficient, which can result not only in decreased neuromuscular performance , but also may predispose the individual to shoulder injuries (20).
Unfortunately, the scapular musculature is often neglected in the treatment of SIS. This lack of attention may often lead into the incomplete treatment (7), therefore, reestablishment of normal shoulder function and restoring normal scapular muscle activation patterns by scapular stabilization based exercises, in our view, are the keys to a successful rehabilitation program.
The purpose of our investigation was to compare the effectiveness of two treatment approaches for impingement syndrome of the shoulder: (1) a 6-week scapular stabilization based exercises, and (2) a ROM exercise program combined with physical modalities on pain, posture, flexibility and mobility of SIS patients.
Methods
The study design was a randomized clinical trial. Ethical approval for this study was granted by the Research Ethics Committee of Tehran University of Medical Sciences (grant number 90-9-28-1992). Subjects were provided with information booklets explaining the purpose of the study and signed informed consent documents prior to participation. Subjects were free to withdraw from the study at any time. This study was conducted in Hazrat Rasool-e-Akram Hospital located in Tehran (Iran) between 2011and 2012. All measurements were taken before and after a 6-week intervention period.
Subjects: A total of 98 subjects was initially recruited from Hazrat Rasool-e-Akram hospital sports medicine and orthopedic clinics and judged to meet the criteria for the study. Twenty six subjects did not fulfill the inclusion criteria (Fig 1). Inclusion and exclusion criteria were assessed for each subject based on a clinical examination performed by the first author. The inclusion criteria were as follows: (1) Male and female mentally fitted between the ages of 18 to 75 years; (2) Unilateral shoulder pain of more than one month localized (anterior and/or anterolateral) to the acromion; (3) Tenderness to palpation of the rotator cuff tendons; (4) Positive impingement tests, or a painful arc of movement (60°–120°) ; (5) Pain produced or increased during flexion and/or abduction of the symptomatic shoulder.
Fig. 1 .

Forward shoulder translation measurement
All subjects tested positive for impingement tests (which included the Hawkins, Neer, and Empty can tests) and underwent a full screening of cervical and shoulder ROM, resisted motions, and special tests. No single impingement test has 100% sensitivity or 100% specificity. Therefore, to correctly identify patients with shoulder impingement, a combination of clinical tests is recommended. According to Ure et al. findings , multiple tests were able to correctly distinguish SIS from other shoulder pathologies in 86% of cases (21-22).
Exclusion criteria were as follows: (1) cervical or shoulder symptoms reproduced by a cervical screening exam; (2) abnormal results with reflex or thoracic outlet tests; (3) symptoms of numbness or tingling in the upper extremity; (4) pregnancy, or (5) a history of the followings: onset of symptoms due to traumatic injury, glenohumeral joint dislocation, acromioclavicular joint separation, shoulder fracture, surgery on the shoulder, fibromyalgia, use of any treatment within three months. Main participants were 72 SIS patients who were randomly allocated into two groups: (1) Scapular Stabilization based Exercise Therapy group (ET) and (2) Physical therapy group (PT).
Random allocation of the subjects was done by using a random number table and block random sampling; A: ET; B: PT (a block size of 4).
Block Size:
Block 1: AABB
Block 2: ABAB
Block 3: BBAA
Block 4: BABA
Block 5: ABBA
Block 6: BAAB
The subjects who were included in the study signed university-approved informed consent forms and completed demographic data sheets. Four subjects were excluded at the intervention stage and three subjects in ET group due to irregular attendance at therapy sessions, travel and an accident and one subject in PT group due to irregular attendance at therapy sessions (Flowchart. 1).
Flowchart 1 .
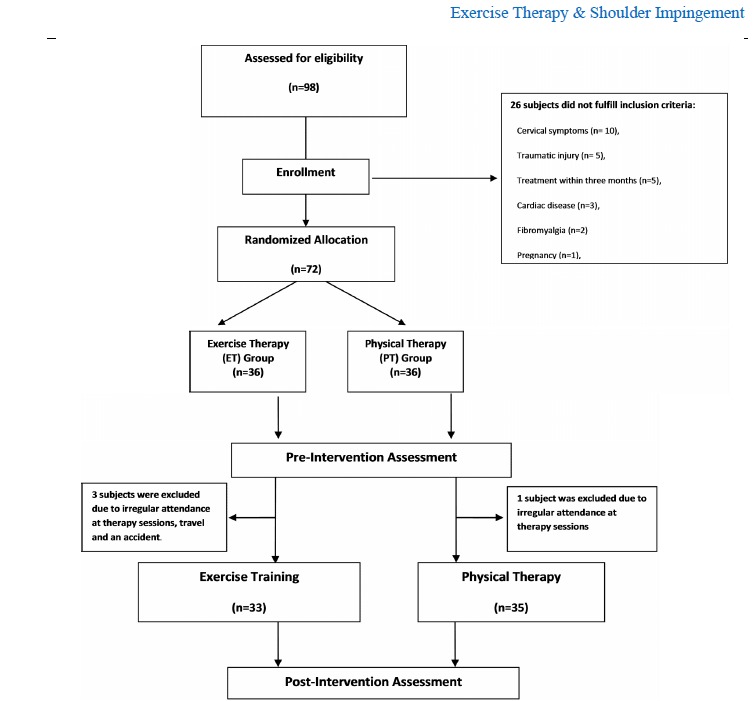
Study profile for participants in ET and PT groups.
In addition to inclusion-exclusion criteria, the clinical evaluation included assessment of pain, active shoulder external rotation and abduction range, forward head posture, mid-thoracic curve, forward shoulder translation, scapular protraction & rotation and Pectoralis minor length were done pre and post intervention.
It must be noted that the participants were blinded in each block. The patients were treated on different days and unaware of the other group. Also, the examiner who assessed was blinded to group allocation and clinical data. The interventions for both groups were done by two clinicians that were unaware of the treatments groups. One supervised exercise therapy for ET group on even days and the other did physical therapy for PT group on odd days.
The power analysis of the study was performed to detect a 10% differences in pain and shoulder abduction with α=0/05 and a power of 80%, a sample size of 36 per group was required.
Pain: Subjects were asked to record their maximal pain during the movements based on visual analogue scale (VAS) for pain. The VAS used in the study was a 10-cm line where the 0 was marked as no pain and the 10 as the worst pain imaginable (23).
Shoulder Range of Motion (ROM): The ranges of active external rotation and abduction were measured by a standard goniometer in both symptomatic and asymptomatic shoulders as follows: Shoulder abduction was measured in the seated chair position, as in flexion, with the trunk upright. The arm was actively elevated in the strict coronal plane with the thumb pointed up toward the ceiling to allow the required external rotation necessary to avoid impingement of the greater tuberosity on the acromion process. Once active end-range was achieved the measurements were documented. Shoulder external rotation was measured in supine with the hips and knees flexed to approximately 45 degrees. The tested arm was supported on the table in 90 degrees of abduction, elbow flexed to 90 degrees, the forearm in midway between pronation/supination and the wrist in neutral. A towel roll was placed under the humerus to ensure neutral horizontal positioning; which required the humerus to be level to the acromion process based on visual inspection. Once positioned, the participant was asked to rotate the arm into external rotation to the end available range without discomfort. The participant was instructed not to lift the lower back during this measurement. Once active end-range was achieved the measurement was recorded (24).
Forward Head Posture (FHP): To measure FHP, a lateral photograph was then taken of the cervicothoracic region, using a Canon Camera (Model: IXY digital 3000 IS).The camera was placed 2 meters from the subject and mounted on a tripod, leveled with a bubble spirit level to control frontal and sagittal angles. This procedure has been used in previous published studies (25-27) . The method chosen to measure the FHP for the current investigation was direct measurement from lateral view photographs of head and shoulder posture. To measure the angles, an A4-sized sheet of graph paper was photocopied onto transparency film for photocopiers. The graph paper had vertical and horizontal lines spaced at 1-mm intervals. The transparency film was then placed over the photograph and aligned so that one of the vertical lines was placed over the plumb line and the intersection of two vertical and horizontal lines coincided with the point the C7 marker came in contact with the skin. To calculate the position of the head in relation to C7 (C7-tragus angle), the angle between the horizontal line and the line connecting tragus of the ear to spinous process of C7 , was measured with a goniometer and documented in degrees.
Mid-Thoracic Curve: This curvature was measured by palpating and marking the spinous processes of the second thoracic vertebra (T2) and the twelfth thoracic vertebra (T12) by counting spinous processes, beginning with C7. The researcher placed the tip of the flexi ruler on T2 and conform it to the subject's spine, marking the flexi ruler at T12. The flexi ruler was transferred to a sheet of white paper, and the curve of the flexi ruler was traced. A metric ruler was used to measure the length and the flexi ruler was used to measure the height of the curve in centimeters. The following formula was used to determine mid-thoracic curvature:
Mid - thoracic curvature = θ = 4 × [arc tan (2 × H/L)]
where H = the height of the curve and L = the length of the curve (Fig 3) (25). Mid-thoracic curvature was measured and documented in degrees for each subject.
Fig. 3 .

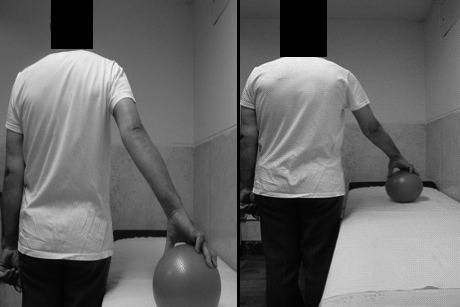
Anthropometric Measurement of Pectoralis
Forward Shoulder Translation(FST): FST was measured using a combination square ruler (CL-01 model, E-Base measuring Tools Co, Taiwan) consists of a 40-cm to measure the distance from the wall to the anterior tip of the subject's acromion process. The patient stood in a relaxed position with their heels against a wall. The anterior tip of acromion process was marked and the distance of the point and wall was measured and documented in millimeter to determine the amount of FST. FST was assessed for both shoulders. This measurement was done three times for each shoulder and the average was recorded as FST (28) (Fig.1).
Scapular Protraction & Rotation: Scapular protraction and rotation were measured with the subject standing, subjects nodded the head and neck forward and backward five times, then inhaled and exhaled deeply to produce a natural, reproducible standing posture and head and neck position (25). For determining scapular protraction, subjects were asked to adopt a comfortable and natural standing position. After palpation, non-allergenic adhesive markers 6 mm in diameter were attached to the following points (Fig. 2):
Fig. 2 .
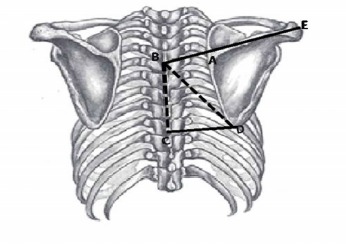
Scapular protraction measurement
A= the root of the scapular spine
B= A mark on the thoracic spine corresponding to the root of the scapular spine
C= A mark on the thoracic spine corresponding to the inferior angle of the scapula
D= the inferior angle of the scapula
E= the tip of the acromion of the scapula.
The following formula was used to determine scapular protraction:
Line BAE = the distance from the mark on the thoracic spine corresponding to the root of the scapular spine to the tip of the acromion.
Line AE= the distance from the root of the scapular spine to the tip of the acromion.
Scapular rotation was measured by palpating and marking the inferior angle of the scapula (D) and the corresponding mark on the thoracic spine (C).
The following formula was used to determine scapular rotation:
Line CD= the distance between the inferior angle of the scapula and the corresponding mark on the thoracic spine.
Line BC= the distance between the marks on the thoracic spine corresponding to the root of the scapular spine and the inferior angle of the scapula (Fig. 2).
Scapular rotation was measured and documented in degrees.Scapular protraction and scapular rotation were measured bilaterally on each subject. The symmetry of the scapular was determined for each subject using the following formula:
Where L= the ratio of left scapular protraction to left scapular rotation, And R= the ratio of right scapular protraction to right scapular rotation.
Anthropometric Measurement of Pectoralis Minor (PM) Length: The anthropometric measurement of the PM length was performed according to the protocol, described by Borstad (29). Before the PM length measurement, two anatomical landmarks were determined first the medial-inferior angle of the coracoid process and a second landmark just lateral to the sternocostal junction of the inferior aspect of the fourth rib. A caliper was used to measure the distance between both bony reference points (Fig. 3). The PM length measurement was done three times for each method and the average was recorded.
Intervention protocols: Following the evaluation, Participants of ET and PT groups began a six-week program (three times per week).
Exercise therapy intervention-After a brief explanation about the exercises protocol, The ET subjects participated in three supervised exercise sessions per week over a 6-week period (16, 20, 30-32). This exercises protocol consisted of a 10 minute walking warm up on a treadmill (DK city- DX3-B1), flexibility, strengthening, scapular stabilization and postural exercises. The patients were asked to avoid any other exercises and severe daily activities during their treatment. At the first session, the subjects were introduced to the different levels of tubing exercises with Theraband. Therabands (The Hygienic Corp, Akron, Ohio) are color-coded, with each color representing a different resistance. Strength Training with Theraband consisted of exercises for rotator cuffs, scapular retractors, shoulder external rotators (Figs 4, 5), D2- PNF pattern (Fig .6) and Serratus anterior punches (Fig .7). The level of difficulty of exercises was increased based on quality of shoulder motion and perceived intensity of pain. The level of tubing resistance was adjusted accordingly for all subjects throughout the treatment process. At the first session, the ET subjects were asked to do five repetitions of each of the tubing exercises to see if they were too hard or too easy; Then the appropriate Theraband was chosen based on feedback from the subject, observation and palpation of the target muscles by the investigator. Five subjects of the ET group used Tan (Ultrathin), sixteen used yellow (thin), and the remaining subjects used red (medium) Theraband. Each tubing exercise was performed as 3 sets of 10 repetitions with a 60-second rest period between each set. At the end of every week, the subjects were evaluated and progressed to the next higher level of resistance using yellow (thin), red (medium), green (heavy), blue (extra-heavy) and Black (Special Heavy) Therabands according to each subject.
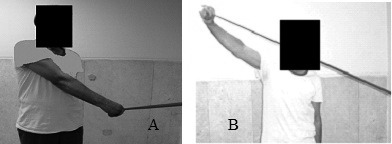
Fig. 4 .

External rotation of shoulder with arm abducted to 90° and elbow flexed to 90°
Fig. 5 .

External rotation of shoulder with arm at side and elbow flexed to 90°
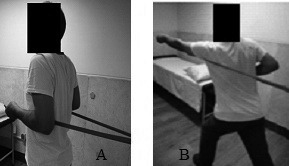
Fig. 6 .
Proprioceptive Neuromuscular Facilitation (PNF) D2 pattern.(A)Starting and (B) Ending position.
Fig. 7 .
Serratus anterior punches. (A)Starting and (B) Ending position
Another exercises program was applied in this study (Table 1) targeted the periscapular muscle to improve stabilization of the scapula (Fig .8). These exercises were done on a medium sized swiss ball.
Table 1 . Description of scapular stabilization exercises .
| Exercises | Description | |
| T to Y | Patient was positioned in a prone on swiss ball with arms abducted to 90° (the letter T); Then flexed the elbows to 90°, retracted his scapulas and externally rotated his arms while keeping his arm in 90° abduction. Maintaining retraction of scapula, the patient raised his arms above the head and extended the elbow while arm flexed and abducted to 120° (the letter Y). | |
| T to Y to W | Patient was positioned in a prone on swiss ball and formed the letter T (as previous description) Then he changed his position to letter Y with his thumbs up. He retracted and depressed scapulas while he raised his arms 10-15 cm. Maintaining retraction of scapula, he flexed his elbows and extended his shoulders to form the letter W.(Fig 11) | |
| Scapular Protraction | Patient was positioned in a prone with toes and forearms supported the body, Then he pushed up 1-2cm and protracted his scapulas. |
Fig. 8 .
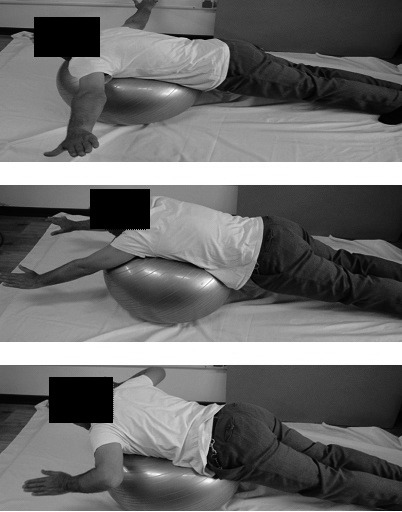
T to Y to W Exercise on swiss ball
Scapular-clock exercise was the other training we used in this study to facilitate the scapular motions of elevation, depression, protraction, and retraction as well as joint kinesthesia and range of motion. The subject stood beside a plinth and put his hand on a ball and moved it to show 3, 6, 9 or 12 o'clock based on an imaginary clock he had on his mind (Fig .9). This exercise also was done by pressing a ball and replacing it on a wall (Fig .10).
Fig. 9 .
Scapular-clock exercise on the table
Fig. 10 .

Scapular-clock exercises on a wall
The flexibility exercises of our program consisted of sleeper stretch (Fig .11), crossed arm stretch (Fig .12), corner stretch (Fig .13) and pectorals stretches (Fig .14) which aimed to elongate Pectoralis major/ minor muscles and stretch of shoulder capsule. Two sets of stretching exercises were performed with a minimum of 10 repetitions for 30 seconds.
Fig. 11 .

Sleeper Stretch
Fig. 12 .

Crossed Arm Stretch (Posterior Capsule Stretch)
Fig. 13 .

Corner Stretch (Posterior Capsule Stretch)
Fig. 14 .

Pectorals Stretches. (Left)Starting and (Right) Ending position
Physical therapy intervention: A combination of physical modalities and range of motion exercises was chosen as a conventional physical therapy in this study for PT group. Their protocol included pendulum and ROM exercises (Scaption, Abduction, Flexion, Extension, Horizontal Abduction, Horizontal Adduction and Rotations), infrared therapy (33) (500 Watt IR lamp, Philips Co, Nederland); ultrasound therapy and TENS (Combined BTL-4825 S Topline, UK) (32) which performed three times per week for 6 weeks. Infrared lamp was in distance of 45-50 cm from pain area according to the patient tolerance. Ultrasound therapy was applied on the subacromial region (US frequency: 1 MHz; US mode: continuous; time: 5 minutes; probe size: 5 cm2; and an intensity of 1 W/cm2).We also used two- electrode TENS (pulse width: 50-250 ms, pulse rate: 90 – 130 Hz) over painful area according to the patient with the most comfortable intensity level. Obviously, these modalities were chosen to reduce pain, improve tissue extensibility and increase range of shoulder motions.
Data Analysis
The Data were analyzed using the Statistical Package for the Social Sciences (SPSS, version 19, SPSS Inc, and Chicago, IL). Descriptive statistics (mean, SD, range) were computed for each study variable. Normal distribution of data was determined by observing histograms and One-Sample Kolmogorov-Smirnov test and parametric tests were used to analyze the data. A paired-sample t test was applied to determine the differences in each group. An independent sample t test was used to compare the baseline measurements between the groups at the beginning and at the end of training and also to analysis change scores of both groups after the test. The change scores of a group were defined as the increase or decrease of each variable from pre-test to post-test. The level of significance was set at p<0.05. In order to study the improvement process of participants, the Change Score of all data were also calculated using the following equation:
Change Score= Post Test Average - Pre Test Average
The change scores will reveal the increase or decrease of each variable from pre-test to post-test.
To assess the Intra-tester reliability of objective tests, 10 SIS subjects, who completed informed consent documentation, had repeated measurements a week apart in a pilot study. Test-retest reliability of variables was assessed using Paired Match T-Test (p≤0.05) and the correlation between the first and second assessing was also obtained (Table 2).
Table 2 . The Correlation between first and second measurements .
| Measurement | Correlation Rate | (p<0.05) |
| Right Abduction Range | 100% | <0/0001 * |
| Left Abduction Range | 100% | <0/0001 * |
| Right External Rotation Range | 100% | <0/0001 * |
| left External Rotation Range | 100% | <0/0001 * |
| Right Protraction | 100% | <0/0001 * |
| Left Protraction | 100% | <0/0001 * |
| Right Rotation | 100% | <0/0001* |
| Left Rotation | 100% | <0/0001 * |
| Symmetry of Scapula | 100% | <0/0001 * |
| Right Forward Shoulder Translation | 99% | <0/0001 * |
| Left Forward Shoulder Translation | 99% | <0/0001 * |
| Forward Head Posture | 97% | <0/0001 * |
| Mid Thoracic Curve | 98% | <0/0001 * |
| Right PML | 100% | <0/0001 * |
| Left PML | 100% | <0/0001 * |
*= Significant
Results
Demographic data of subjects in both groups has been shown in Table 3. There were no significant differences between PT and ET groups for the demographic variables (Table 3), indicating that the groups were well matched. There were 55 females and 13 males, with ages ranging from 21 to 78 years, 75.8% of subjects in ET group and 87.7% of PT group were female.
Table 3 . Basic characteristics and the baseline measurements of the PT and ET groups .
| Groups |
PT Group (n=35) Mean±SD |
ET Group (n=33) Mean±SD |
P value P<0.05 |
|
|
Demographic Variables & Baseline Measurements |
||||
| Age(yr) | 47.77±7.85 | 48.15 ±13.81 | 0.85 | |
| Mass(kg) | 70.26±7.72 | 68.82 ±10.38 | 0.61 | |
| Height(m) | 161.94±7.62 | 161.52 ±6.85 | 0.89 | |
| BMI(kg.m2 ) | 26.77±2.71 | 26.38 ±3.38 | 0.90 | |
| Duration of SIS (mon) | 6.64±4.08 | 5.31±4.46 | 0.36 | |
| VAS | 7.57±1.24 | 7.45±1.14 | 0.689 | |
| Abduction | 136.57±25.66 | 143.03±26.15 | 0.308 | |
| External Rotation | 65.29±18.5 | 64.55±20.93 | 0.878 | |
| Protraction | 1.79±0.12 | 1.78±0.15 | 0.929 | |
| Rotation | 39.00 ±2.11 | 39.33±1.97 | 0.505 | |
| Symmetry | 0.98±0.03 | 0.996±0.03 | 0.437 | |
| Forward Shoulder Translation | 14.84±0.94 | 14.88±1.41 | 0.910 | |
| Forward Head Posture | 46.57±2.45 | 45.55±2.87 | 0.117 | |
| Mid Thoracic Curve | 43.98±5.08 | 40.98±4.24 | 0.888 | |
| PML | 11.53±1.17 | 11.49±1.15 | 0.791 |
The majority of subjects in both groups were right dominant and right shoulder was affected in them (Table 4).
Table 4 . Descriptive statistics for subjects of the PT and ET groups .
| PT Group | ET Group | |
|
Dominant side : Right Left |
94.3% 6.1% |
93.9% 5.7% |
|
Impaired side: Right Left |
74.3% 25.7% |
60.6% 39.4% |
Pre Test Results: Independent- sample t test revealed no significant differences (p<0.05) between two groups at the beginning of the study (Table 3).
Post Test Results: There were significant differences in VAS, abduction, external rotation, forward shoulder translation, Pectoralis minor length in the PT group (Table 5) between pre and posttests (p<0.05) in PT Group. All variables showed significant differences in ET group except scapular rotation and symmetry (Table 5) between pre and posttests (p<0.05).
Table 5 . Training effect within ET (n=33) and PT group (n=35) .
| Group | PT Group | ET Group | |||
| Variables |
Post-test Mean±SD |
P value (P<0.05) |
Post-test Mean±SD |
P value (P< 0.05) |
|
| VAS | 3.14±2.08 | <0/0001 * | 2.76±2.16 | <0/0001 * | |
| Abduction | 155.71±16.32 | <0/0001 * | 171.82±12.36 | <0/0001 * | |
| External Rotation | 72.29±16.64 | <0/0001 * | 80.3±11.31 | <0/0001 * | |
| Protraction | 1.79±0.12 | - | 1.77±0.14 | <0/0001 * | |
| Rotation | 39.00±2.11 | - | 39.18±1.96 | 0.201 | |
| Symmetry | 0.98±0.03 | - | 0.994±0.03 | 0.591 | |
| Forward Shoulder Translation | 14.74±0.92 | <0/0001 * | 14.47±1.27 | <0/0001 * | |
| Forward Head Posture | 46.69±2.41 | 0.103 | 46.76±2.37 | <0/0001 * | |
| Mid Thoracic Curve | 43.85±4.99 | 0.209 | 39.58±4.07 | <0/0001 * | |
| PML | 11.77±1.18 | <0/0001 * | 11.96±1.10 | <0/0001 * | |
*= Significant
Comparison between Change scores in Training Groups: The improvement of shoulder abduction and external rotation ranges, postural parameters (forward shoulder translation, forward head posture, mid-thoracic curve and Pectoralis minor length) in ET group was significantly greater than that the PT group. VAS did not have significant difference between both groups. Moreover, scapular rotation and symmetry had no or very little changes between PT and ET groups (Table 6).
Table 6 . Comparison of change scores between ET (n=33) and PT group (n=35) .
| Group |
Group PT Change Score |
Group ET Change Score |
P value | |
| Variables | Mean±SD | Mean±SD | (P< 0.05) | |
| VAS | -4.42 ± 1.86 | -4.69 ± 2.06 | 0.576 | |
| Abduction | 19.14± 14.42 | 28.78 ± 19.8 | 0.024 * | |
| External Rotation | 7.00 ± 8.06 | 15.75 ± 12.99 | 0.001 * | |
| Protraction | 0.0000 | -0.016 ± 0.01 | <0/001 * | |
| Rotation | 0.0000 | -0.15 ± 0.66 | 0.183 | |
| Symmetry | 0.0000 | -0.001 ± 0.01 | 0.578 | |
| Forward Shoulder Translation | -0.10 ± 0.09 | -0.40 ± 0.24 | <0/001 * | |
| Forward Head Posture | 0.11 ± 0.40 | 1.21 ± 0.92 | <0/001 * | |
| Mid Thoracic Curve | -0.13 ± 0.61 | -1.40 ± 1.33 | <0/001 * | |
| PML | 0.23 ± 0.08 | 0.46 ± 0.20 | <0/001 * |
*= Significant
Discussion
The purpose of the current study was to investigate the effect of a 6-week supervised scapular stabilization exercise therapy on pain, scapular position, head and back posture, and shoulder mobility in comparison with physical therapy in patients with SIS. Our findings indicate that the exercise protocol suggested in this study significantly decreased pain, improved scapular protraction, head and back posture and increased shoulder mobility. However, we did not observe between-group differences for scapular rotation and symmetry following the exercise therapy.
Pain: An equal effectiveness of physiotherapy and exercise therapy in decreasing pain was obtained in this study and no significant difference was found in the VAS score and the shoulder pain was decreased in subjects of both groups. The effect of exercise therapy in reducing pain alone or in combination with other treatments has been shown in the previous studies (15, 34-36).
Rotator cuff muscles stabilize the humeral head in the glenoid, causing humerus to rotate outside while protecting the distance between large tubercle and acromion and preventing compression. It was why that the resistance training (Theraband) used in this study, was effective in reducing pain in ET group subjects. Furthermore, the stretching exercises of our program improved the flexibility of shoulder tight tissue that could be effective in pain decrease. It seems that our exercise therapy protocol is effective as a treatment for the reduction of pain in SIS patients.
In the present study, ultrasound and TENS was used for the treatment of PT group subjects. Despite the fact that ultrasound has been used in the treatment of shoulder pain for decades, There are evidences showed that US alone has no benefit in decreasing SIS pain (18, 34, 37-39) and also no available evidence for efficacy of TENS alone for patients with SIS pain (38). Başkurt et al. did not find any statistically significant difference in studying the immediate effects of TENS and heat on the pain related to stage one of SIS. (40) Herrera-Lasso et al. found positive effects of continuous ultrasound with high frequency TENS in decreasing pain and improving range of movement. (38) Therefore, in this study, a therapeutic package of continuous ultrasound with high frequency TENS and superficial heat (IR) was used which was effective in reducing pain between pre and post intervention in PT group due to the thermal effect of US and IR in combination with analgesic effect of TENS.
Shoulder Range of Motion (ROM): The findings of this study demonstrated the significant differences of affected shoulder abduction and external rotation between pre and post intervention in both group. Also there were significant differences in shoulder ROM and its progression rate between PT and ET groups; which imply that ET group had remarkable improvement in shoulder ROM due to stretching exercises used in this study for decreasing tight shoulder capsule and shortened muscles especially pectoral muscles. Also increasing shoulder ROM may be due to decreasing patients' pain. Our findings agree with those of other researchers (37,41-42) who have documented improvements in ROM following an exercise program in patients with SIS.
Posture: The effect of a six-week exercise intervention was evaluated in changing head, shoulder and back posture in comparison with physical modalities in this study. A decrease was observed in FHP, FST and mid-thoracic curve in both groups pre and post intervention but there was a significant difference between ET and PT groups. The results revealed that the exercise protocol used in current study significantly decreased FHP, FST and mid-thoracic curve, suggesting that our exercises have improved patients' posture. The flexibility exercises of this study were chosen based on the results that indicate tightness of levator scapulae , pectorals in SIS (28) and also a previous study findings which has showed selective activation of deep cervical flexors, Middle and Lower Trapezes and also Serratus Anterior in SIS patient (43). It seems that the supervised stretching of the tight anterior shoulder muscles with strengthening of the relatively weaker muscles in present protocol could have a significant synergistic effect on patients' posture. Our findings are similar to Kluemper et al. and Lynch et al. findings who have studied the effect exercise intervention on FHP and FSP in swimmers (16,28).
Scapular Protraction & Rotation: Another purpose of present study was to examine the effect of our exercise program on the position of scapula. The abnormal position of scapula in SIS patients may lead to instability of shoulder joint. The results of our study revealed significant differences in the scapular protraction of the ET group compared to the PT group within six-week exercise therapy, indeed there was no change in scapular protraction in PT group. But scapular rotation and symmetry did not indicate any significant difference between pre and post intervention in both group and also between groups. We expected to find more substantial changes in scapular rotation and symmetry after exercise based on Alizadeh et al. study (30). A significant changes in scapular symmetry and rotation might require a long term practice, perhaps due to short term duration of our exercise protocol or low accuracy of the measurement methods used in this study, scapular symmetry and rotation showed no significant changes.
Pectoralis Minor Length (PML): Abnormal kinematic of scapula in SIS might be lead to Pectoralis minor shortening and tightness, therefore in this study PML in patient involved shoulder was measured with anthropometric method .The results of this assessment indicate a significant difference in PML between pre and post intervention in both group and also between groups. PML was increased more in ET group compared to PT group because of applying stretching exercises. Our findings are similar to those of other researchers (44-46).
This study had several limitations. A major limitation of our work is that we have no follow-up period. May be if the subjects were followed-up, a significant difference in pain might be found after several weeks. Therefore, more high-quality trials with longer follow-ups are recommended. Also scapular and shoulder muscles strength was not assessed in this study and further research is needed, however, to evaluate shoulder girdle muscles strength.
Conclusion
The scapula plays a vital role in shoulder function, thus this study highlights exercise prescription to enhance scapular stabilization during the SIS rehabilitation. The scapular stabilization based exercise intervention was successful at increasing shoulder range of abduction and external rotation, decreasing forward head and shoulder postures and Pectoralis minor flexibility. This study supports basis for scapular stabilization based exercise therapy in the rehabilitation of SIS. Also be noted that exercise therapy is effective as a treatment for the reduction of pain in these patients.
Acknowledgments
This project was supported by a grant from Research Deputy of Tehran University of Medical Sciences with ID number for IRCT201111025486N2. The authors thank the participants for their excellent cooperation. The authors would like to acknowledge the generous assistance of the academic members and the staff of the Sports Medicine Clinic of Hazrat Rasool-e-Akram hospital, Tehran, Iran.
Cite this article as: Moezy A, Sepehrifar S, Solaymani Dodaran M. The Effects of Scapular Stabilization Based Exercise Therapy on Pain, Posture, Flexibility and Shoulder Mobility in Patients with Shoulder Impingement Syndrome: A Controlled Randomized Clinical Trial. Med J Islam Repub Iran 2014 (27 August). Vol. 28:87.
References
- 1.Koester MC, George MS, Kuhn JE. Shoulder impingement syndrome. The American journal of medicine. 2005;118(5):452–5. doi: 10.1016/j.amjmed.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 2.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Physical therapy. 2000;80(3):276–91. [PubMed] [Google Scholar]
- 3.Cook TM, Ludewig P. Translations of the humerus in persons with shoulder impingement symptoms. Journal of Orthopaedic & Sports Physical Therapy. 2002;32(6):248. doi: 10.2519/jospt.2002.32.6.248. [DOI] [PubMed] [Google Scholar]
- 4.Graichen H, Stammberger T, Bonel H, Englmeier K-H, Reiser M, Eckstein F. Glenohumeral translation during active and passive elevation of the shoulder—a 3D open-MRI study. Journal of biomechanics. 2000;33(5):609–13. doi: 10.1016/s0021-9290(99)00209-2. [DOI] [PubMed] [Google Scholar]
- 5.Lukasiewicz A, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. The Journal of orthopaedic and sports physical therapy. 1999;29(10):574. doi: 10.2519/jospt.1999.29.10.574. [DOI] [PubMed] [Google Scholar]
- 6.Brumitt J. Scapular-stabilization exercises: early-intervention prescription. Athletic Therapy Today. 2006;11(5):15–8. [Google Scholar]
- 7.Voight ML, Thomson BC. The role of the scapula in the rehabilitation of shoulder injuries. Journal of Athletic training. 2000;35(3):364. [PMC free article] [PubMed] [Google Scholar]
- 8.Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. The Journal of orthopaedic and sports physical therapy. 2009;39(2):90. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yano Y, Hamada J, Tamai K, Yoshizaki K, Sahara R, Fujiwara T. et al. Different scapular kinematics in healthy subjects during arm elevation and lowering: glenohumeral and scapulothoracic patterns. Journal of shoulder and elbow surgery. 2010;19(2):209–15. doi: 10.1016/j.jse.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Han KJ, Cho JH, Han SH, Hyun HS, Lee DH. Subacromial impingement syndrome secondary to scapulothoracic dyskinesia. Knee Surg Sports Traumatol Arthrosc. 2012 Oct;20(10):1958–60. doi: 10.1007/s00167-011-1805-5. [DOI] [PubMed] [Google Scholar]
- 11.McQuade K, Dawson J, Smidt G. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. The Journal of orthopaedic and sports physical therapy. 1998;28(2):74. doi: 10.2519/jospt.1998.28.2.74. [DOI] [PubMed] [Google Scholar]
- 12.Cools AM, Witvrouw EE, Declercq GA, Danneels LA, Cambier DC. Scapular Muscle Recruitment Patterns: Trapezius Muscle Latency with and without Impingement Symptoms. The American journal of sports medicine. 2003;31(4):542–9. doi: 10.1177/03635465030310041101. [DOI] [PubMed] [Google Scholar]
- 13.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clinical Biomechanics (Bristol, Avon) 2003;18(5):369–79. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 14.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndromeA study using Moire topographic analysis. Clin Orthop Relat Res. 1992;285:191–9. [PubMed] [Google Scholar]
- 15.Celik D, Akyuz G, Yeldan I. Comparison of the effects of two different exercise programs on pain in subacromial impingement syndrome. Acta Orthop Traumatol Turc. 2004;43(6):504–9. doi: 10.3944/AOTT.2009.504. [DOI] [PubMed] [Google Scholar]
- 16.Kluemper M, Uhl T, Hazelrigg H. Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. Journal of Sport Rehabilitation. 2006;15(1):58. [Google Scholar]
- 17.Faber E, Kuiper JI, Burdorf A, Miedema HS, Verhaar JA. Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. Journal of occupational rehabilitation. 2006;16(1):6–24. doi: 10.1007/s10926-005-9003-2. [DOI] [PubMed] [Google Scholar]
- 18.Van der Heijden G, Van der Windt D, de Winter AF. Physiotherapy for patients with soft tissue shoulder disorders: a systematic review of randomised clinical trials. BMJ :British Medical Journal. 1997;315(7099):25. doi: 10.1136/bmj.315.7099.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soibam I. Comparative study on the effectiveness of ultrasound (us) to transcutaneous electrical stimulation (tens) in the treatment of periarticular shoulder pain (psp) 2005 [Google Scholar]
- 20.Roy J-S, Moffet H, Hébert LJ, Lirette R. Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: A single-subject study design. Manual therapy. 2009;14(2):180–8. doi: 10.1016/j.math.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Ure B, Tiling T, Kirchner R, Rixen D. [Reliability of clinical examination of the shoulder in comparison with arthroscopyA prospective study] Der Unfallchirurg. 1993;96(7):382. [PubMed] [Google Scholar]
- 22.Leroux J, Thomas E, Bonnel F, Blotman F. Diagnostic value of clinical tests for shoulder impingement syndrome. Revue du rhumatisme (English ed) 1995;62(6):423. [PubMed] [Google Scholar]
- 23.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152(10):2399–404. doi: 10.1016/j.pain.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Kolber MJ, Hanney WJ. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: A technical report. International journal of sports physical therapy. 2012;7(3):306. [PMC free article] [PubMed] [Google Scholar]
- 25.Greenfield B, Catlin P, Coats P, Green E, McDonald J, North C. Posture in patients with shoulder overuse injuries and healthy individuals. The Journal of orthopaedic and sports physical therapy. 1995;21(5):287. doi: 10.2519/jospt.1995.21.5.287. [DOI] [PubMed] [Google Scholar]
- 26.Raine S, Twomey LT. Head and shoulder posture variations in 160 asymptomatic women and men. Archives of physical medicine and rehabilitation. 1997;78(11):1215–23. doi: 10.1016/s0003-9993(97)90335-x. [DOI] [PubMed] [Google Scholar]
- 27.Lewis JS, Wright C, Green A. Subacromial impingement syndrome: the effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35(2):72–87. doi: 10.2519/jospt.2005.35.2.72. [DOI] [PubMed] [Google Scholar]
- 28.Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. British journal of sports medicine. 2010;44(5):376–81. doi: 10.1136/bjsm.2009.066837. [DOI] [PubMed] [Google Scholar]
- 29.Borstad JD. Measurement of Pectoralis minor muscle length: validation and clinical application. The Journal of orthopaedic and sports physical therapy. 2008;38(4):169. doi: 10.2519/jospt.2008.2723. [DOI] [PubMed] [Google Scholar]
- 30.Alizadeh M, Daneshmandi H, Shademan B, Ahmadizad S. The Effects of Exercise Training on Scapula Position of Muscle Activity Measured by EMG. World. 2009;2(1):48–52. [Google Scholar]
- 31.De Mey K, Danneels L, Cagnie B, Cools AM. Scapular Muscle Rehabilitation Exercises in Overhead Athletes With Impingement Symptoms: Effect of a 6-Week Training Program on Muscle Recruitment and Functional Outcome. The American journal of sports medicine. 2012 August 1,2012;40(8):1906–15. doi: 10.1177/0363546512453297. [DOI] [PubMed] [Google Scholar]
- 32.Ginn K, Cohen M. Exercise therapy for shoulder pain aimed at restoring neuromuscular control: a randomized comparative clinical trial. Journal of Rehabilitation Medicine. 2005;37(2):115–22. doi: 10.1080/16501970410023443. [DOI] [PubMed] [Google Scholar]
- 33.Leung MS, Cheing GL. Effects of deep and superficial heating in the management of frozen shoulder. Journal of Rehabilitation Medicine. 2008;40(2):145–50. doi: 10.2340/16501977-0146. [DOI] [PubMed] [Google Scholar]
- 34.Kromer TO, Tautenhahn UG, de Bie RA, Staal JB, Bastiaenen CH. Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. Journal of Rehabilitation Medicine. 2009;41(11):870–80. doi: 10.2340/16501977-0453. [DOI] [PubMed] [Google Scholar]
- 35.Ginn KA, Herbert RD, Khouw W, Lee R. A randomized, controlled clinical trial of a treatment for shoulder pain. Physical therapy. 1997;77(8):802–9. doi: 10.1093/ptj/77.8.802. [DOI] [PubMed] [Google Scholar]
- 36.Bang MD. Comparison of Supervised Exercise With and Without anual Physical Therapy for Patients With Shoulder Impingement Syndrome. Journal of Orthopaedic & Sports Physical Therapy. 2000;30(3):126–37. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 37.Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. Journal of hand therapy. 2004;17(2):152–64. doi: 10.1197/j.jht.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 38.Johansson K, Oberg B, Adolfsson L, Foldevi M. A combination of systematic review and clinicians' beliefs in interventions for subacromial pain. The British Journal of General Practice. 2002;52(475):145. [PMC free article] [PubMed] [Google Scholar]
- 39. Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain (Review). 2010. [DOI] [PMC free article] [PubMed]
- 40.Başkurt Z, Başkurt F, Özcan A, Yilmaz Ö. The immediate effects of heat and TENS on pressure pain threshold and pain intensity in patients with Stage I shoulder impingement syndrome. The Pain Clinic. 2006;18(1):81–5. [Google Scholar]
- 41.McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Physical therapy. 2004;84(9):832–48. [PubMed] [Google Scholar]
- 42.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. Journal of shoulder and elbow surgery. 2009;18(1):138–60. doi: 10.1016/j.jse.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 43.Moseley J JF, Pink M, Perry J, Tibone J. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992;20:128–34. doi: 10.1177/036354659202000206. [DOI] [PubMed] [Google Scholar]
- 44.Borstad JD, Ludewig PM. Comparison of three stretches for the Pectoralis minor muscle. Journal of shoulder and elbow surgery. 2006;15(3):324–30. doi: 10.1016/j.jse.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 45.Cools AM, Johansson FR, Cambier DC, Velde AV, Palmans T, Witvrouw EE. Descriptive profile of scapulothoracic position, strength and flexibility variables in adolescent elite tennis players. British journal of sports medicine. 2010;44(9):678–84. doi: 10.1136/bjsm.2009.070128. [DOI] [PubMed] [Google Scholar]
- 46.Muraki T, Aoki M, Izumi T, Fujii M, Hidaka E, Miyamoto S. Lengthening of the Pectoralis minor muscle during passive shoulder motions and stretching techniques: a cadaveric biomechanical study. Physical therapy. 2009;89(4):333–41. doi: 10.2522/ptj.20080248. [DOI] [PubMed] [Google Scholar]


