Abstract
Intake of the mainly plant derived n-3 polyunsaturated fatty acid (PUFA) α-linolenic acid (ALA) has been associated with lower risk of coronary heart disease (CHD). However, the results have been inconsistent. Therefore, the objective of this study was to examine the association between ALA consumption and risk of CHD. Potential effect modification by long-chain n-3 PUFA (n-3 LCPUFA) was also investigated. Data from eight American and European prospective cohort studies including 148,675 women and 80,368 men were used. The outcome measure was incident CHD (CHD event and death). During follow-up of 4-10 years, 4,493 CHD events and 1,751 CHD deaths occurred. Among men we found an inverse association (not significant) between intake of ALA and CHD event and death. For each additional gram of ALA, there was a 15% lower risk of CHD events (HR: 0.85; 95% CI: 0.72, 1.01) and a 23% lower risk of CHD deaths (HR: 0.77; 95% CI 0.58, 1.01). We found no consistent associations among women. No effect modification by intake of n-3 LCPUFA was found.
Keywords: Alpha-linolenic acid, coronary heart disease, epidemiology
Introduction
Coronary heart disease (CHD) is the leading cause of morbidity and mortality in the world (1). CHD arises from genetic and modifiable lifestyle factors including diet. One of the important dietary components identified is a low intake of n-3 (omega-3) polyunsaturated fatty acid (PUFA). The marine derived long-chain n-3 PUFA(n-3 LCPUFA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have for long been the main focus of research on the importance of n-3 PUFAs in relation to CHD. Since the pioneering studies among Greenland Eskimos suggested that high intakes of EPA and DHA can protect against CHD (2), many studies and meta-analysis have confirmed these associations (3-7). However, the long-term association of mainly plant derived n-3 PUFA, alpha-linolenic acid (ALA) with CHD is not clear (8-11). A recent meta-analysis from 2012 of 3 prospective studies suggested that each 1 g/d of ALA intake was associated with a 20% lower risk of CHD event (11).
Intake of fish and other marine products is limited in many countries and ALA primarily from plant oils and nuts (e.g. canola oils, walnuts, and soybean) are the predominant source of n-3 PUFA in the typical Western diet. In the human body, ALA is converted to n-3 LCPUFA by desaturation and elongation but this conversion is limited and generally much lower in men than in women (12;13). The effect of ALA on risk of CHD may be influenced by n-3 LCPUFA, because they via feedback inhibition of the activity of delta-6-desaturase (the key limiting enzyme) regulate the conversion of ALA into n-3 LCPUFA. It is therefore possible that ALA may particularly reduce the risk of CHD among those subjects who have a low n-3 LCPUFA intake (14).
We investigated the association between ALA intake and risk of CHD in populations with different diets and over a wide range of ALA intakes, by using data from eight prospective cohort studies from the United States and Europe included in the Pooling Project of Cohort Studies on Diet and Coronary Disease. We hypothesized that the intake of ALA was inversely associated with risk of CHD and that the inverse association between intake of ALA and risk of CHD was stronger in subjects with low intake of n-3 LCPUFA compared to those with high intake of n-3 LCPUFA.
Subjects and Methods
Study populations
Eleven prospective cohort studies (the Adventist Health Study (AHS) (15); Atherosclerosis Risk In Communities Study (ARIC) (16); the Alpha-Tocopherol and Beta-Carotene Cancer Prevention Study (ATBC) (17); the Finnish Mobile Clinic Health Study (FMC) (18); the Glostrup Population Study (GPS) (19); the Health Professionals Follow-up Study (HPFS) (20); the Israeli Ischemic Heart Disease Study (IIHD) (21); the Iowa Women's Health Study (IWHS) (22); the Nurses' Health Study (NHS) (23); the Västerbotten Intervention Program (VIP) (24); and the Women's Health Study (WHS) (25)) met the following criteria and were included in the Pooling Project of Cohort studies on Diet and Coronary Disease: (1) a published prospective study with at least 150 incident CHD cases; (2) usual dietary intake determined by a food frequency questionnaire (FFQ), a dietary history interview, or a seven-day weighed food record at baseline; and (3) a validation or a repeatability study of the dietary assessment method. Three studies; AHS, GPS, and IIHD, were excluded from the present analysis due to lack of information on ALA intake. The remaining eight studies, five from the United States, two from Finland and one from Sweden, are presented in Table 1. From the cohorts we excluded individuals who were less than 35 years of age, had a history of cardiovascular disease, diabetes, or cancer (except non-melanoma skin cancer), and an extreme energy intake, i.e. intakes greater or less than three standard deviations from the study specific log-transformed mean energy intake of the baseline populations. The final population consisted of 229 043 persons (65 % women).
Table 1. Characteristics of the cohort studies included in the Pooling Project of Diet and Coronary Heart Disease1.
| Study | Country | Year of inception | Baseline cohort sample size* | Median age at baseline (80% central range) | Median follow-up time | Number of CHD events | Dietary assessment method## | Median dietary PUFA intake (80% central range) Energy adjusted g/d | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Years | Total CHD events | CHD deaths | Total CHD events | CHD Deaths | ALA | EPA + DHA | |||||
| Women | |||||||||||
|
| |||||||||||
| ARIC | US | 1987 | 6,481 | 53 (47-62) | 9.2 | - | 123 | - | FFQ | 0.70 (0.54-0.90) | 0.21 (0.05-0.62) |
| FMC | Finland | 1966 | 2,481 | 49 (38-65) | 10.0 | 10.0 | 162 | 48 | DH | 0.53 (0.42-0.87) | 0.15 (0.06-0.36) |
| IWHS | US | 1986 | 30,180 | 61 (56-67) | - | 10.0 | - | 294 | FFQ | 0.94 (0.71-1.25) | 0.13 (0.02-0.35) |
| NHS | US | 1986 | 61,706 | 52 (43-62) | 10.0 | 10.0 | 696 | 208 | FFQ | 0.97 (0.72-1.33) | 0.18 (0.06-0.42) |
| VIP | Sweden | 1992 | 10,555 | 50 (40-60) | 4.1 | - | 23 | - | FFQ | 1.26 (0.96-1.81) | 0.10 (0.03-0.23) |
| WHS | US | 1993 | 37,272 | 52 (46-64) | 5.3 | 5.3 | 152 | 10 | FFQ | 0.92 (0.69-1.26) | 0.15 (0.05-0.36) |
|
| |||||||||||
| Men | |||||||||||
|
| |||||||||||
| ARIC | US | 1987 | 5,240 | 54 (47-63) | 9.2 | 9.2 | 269 | 51 | FFQ | 0.93 (0.72-1.20) | 0.20 (0.03-0.62) |
| ATBC | Finland | 1985 | 21,141 | 57 (51-65) | 6.0 | 6.1 | 1339 | 534 | FFQ | 1.20 (0.74-1.92) | 0.34 (0.16-0.66) |
| FMC | Finland | 1966 | 2,712 | 47 (37-63) | 10.0 | 10.0 | 322 | 147 | DH | 0.68 (0.55-0.98) | 0.23 (0.09-0.59) |
| HPFS | US | 1986 | 41,754 | 53 (42-67) | 9.7 | 9.7 | 1273 | 421 | FFQ | 1.12 (0.83-1.54) | 0.26 (0.07-0.58) |
| VIP | Sweden | 1992 | 9,521 | 50 (40-60) | 4.1 | 4.1 | 134 | 38 | FFQ | 1.73 (1.27-2.51) | 0.12 (0.03-0.30) |
|
| |||||||||||
| Women, total | 148 675 | 1,156 | 560 | 1.01 (0.58-1.64) | 0.15 (0.04-0.42) | ||||||
| Men, total | 80368 | 3,337 | 1191 | 1.17 (0.64-1.62) | 0.26 (0.06-0.66) | ||||||
| Total | 229 043 | 4,493 | 1,751 | 1.06 (0.60-1.06) | 0.19 (0.05-0.50) | ||||||
ARIC, Atherosclerosis risk in Communities Study; ATBC, Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study; FMC, Finnish Mobile Clinic Health Examination Survey; HPFS, Health Professionals Follow-up Study; IWHS, Iowa Women's Health Study; NHS, Nurses' Health Study; VIP, Västerbotten Intervention Program; WHS, Women's Health Study.
Sample size after exclusion of subjects with a baseline age <35 years, baseline cardiovascular disease, cancers, diabetes mellitus, very high or low reported caloric intake and missing information on dietary polyunsaturated fatty acid intake.
FFQ, food frequency questionnaire; DH, dietary history interview.
Diet
Habitual dietary intake was determined at baseline by a FFQ in seven of the cohorts and by a dietary history interview in one cohort (table 1). The FFQs that were used in ARIC, NHS, HPFS, WHS, and IWHS were similar or a modified version of the original 61-item Willett FFQ developed in 1980 (23). However, as the FFQs are modified, the number of items in each study differs; the FFQs in ARIC, HPFS, WHS and IWHS contained 66, 131, 131 and 116 items, respectively. As the ARIC study used the oldest version of the FFQ with only 66 items, it did not have the same details on e.g. cooking oil. Within NHS, in 1980, a 61-item FFQ was included, to assess the dietary intake. The questionnaire was expanded to 116 items in 1984 and repeated in 1986 and 1990. The data from NHS used in this study were those from 1986. The participants were asked to indicate how often, on average, they had consumed given amounts of various specified foods during the past year. The average daily intake of nutrients was then computed by multiplying the frequency of intake by the nutrient composition of the specified portion size. Composition values of ALA (and other nutrients) were obtained from Harvard University food composition database and US Department of Agriculture (26). The Finnish FFQ used in ATBC included 276 food items, and participants were asked about their usual intake and portion size of foods during the past year (17;27). The type of fat used on bread, which is an important source of fat in the Finnish diet, was specified by the brand name of the product (28). The fatty acid content of the foods was based on analyses of 77 fatty acids in Finnish foods carried out at the Department of Food Chemistry, University of Helsinki (28). The questionnaire used in the VIP (24) included 84 food items. The subjects were asked about their habitual dietary intake during the previous year and typical portion sizes were indicated using color photographs. The average daily intake was calculated by multiplying the frequency of intake by a portion size value using the Swedish national food composition database (24). The FMC study used a dietary history interview where the interviewer asked the participants about their habitual diet during the previous year (29). The subjects reported their food consumption on a daily, weekly or monthly basis. The ingredients of mixed foods were broken down into components by use of a recipe file and the consumption of fruits and berries, vegetables, and cereals as well as the subgroups of these food categories, and separate food items such as dairy and meat products were calculated per day. The total energy intake was calculated from the intake of protein, fat and available carbohydrate according to Finnish food composition tables (29).
Outcome
The outcome of interest was incident CHD events (fatal and nonfatal). Because the Iowa Women's Health Study only had self-reported data on incident CHD, we only used fatal CHD from this study. All studies have used standardized criteria to define nonfatal and fatal CHD cases (30).
Statistical analyses
Within each study, hazard ratios (HR) with 95% CIs for the incidence of fatal and nonfatal CHD events were calculated using Cox proportional hazard regression with time in study (y) as the time metric (31). The observation time for each participant was defined by the date on which information on the diet was obtained and until CHD occurrence, death of another cause, disappearance, or end of follow-up, whichever came first. Studies with follow-up periods of more than 10 years were truncated to reduce possible effect modification by time. The analyses were carried out separately for men and women. ALA intake was adjusted for total energy with the residuals method, and modeled as a continuous variable followed by analyses with ALA intake as categorical variable, in quintiles and as well as binary variable (below/above the median). Subsequently, to assess possible effect modification by n-3 LCPUFA, we stratified analyses with ALA and n-3 LCPUFA intake by using combined categories of higher (≥median) compared to lower (<median) intake. Furthermore, analyses were made to explore possible age-related differences in the associations between ALA intake and risk of CHD. The study population was divided into two age groups in further analyses; less than 60 years at baseline and 60 years or more at baseline. The study-specific logs of HRs were weighted by the inverse of their variances, and a pooled (combined) estimate of the HRs was computed by using a random-effects model. Evidence for between-studies heterogeneity among study-specific HRs was examined using the estimated between-studies variance component Q statistic (31).
The following potential confounders were included in the statistical models: body mass index (BMI) (<23, 23-25, 25-30, or ≥30 kg/m2); highest attained educational level (<high school, high school, or >high school); smoking (never, ex, and current smokers and in the latter 1-4, 5-14, 15-24, or ≥25 cigarettes/day); physical activity (five levels); alcohol intake (0, 0-<5, 5-<10, 10-<15, 15-<30, 30-<50, or ≥50 g/d); total energy (the sum of energy intake derived from fat, carbohydrates and protein in kJ/d); saturated fatty acids (SFA), trans fatty acids (TFA), monounsaturated fatty acids (MUFA), linoleic acid (LA), and n-3 LCPUFA intake in g/d; quintiles of dietary fibre intake; and history of hypertension (yes or no). Three models were used to investigate the associations between intake of ALA and risk of CHD. Model 1 included energy-adjusted intake of ALA in g/d and age at baseline (y), as well as the calendar year in which the baseline diet questionnaire was returned. The variables were entered into the model through the strata statement. Model 2 included the variables of model 1 and the following known risk factors for CHD: BMI, educational level, smoking habits, physical activity, and history of hypertension. Model 3 included the variables of model 2 and the following dietary risk factors: alcohol intake, total energy intake, quintiles of fibre intake, TFA, SFA, MUFA, LA, andn-3 LCPUFA intake. We tested ALA intake for nonlinearity by including energy adjusted ALA variable squared to the model and pooled the effect estimate for this term. Analyses were performed using SAS 9.2 statistical software (SAS Institute Inc).
Results
Characteristics of the cohort studies are given in Table 1. During 4-10 year of follow-up, 4,493 CHD events and 1,751 CHD deaths occurred among the 229 043 subjects. The 10th, 50th, and 90th percentiles of energy-adjusted intake of ALA were 0.58, 1.01, and 1.64 g/d in women, respectively and 0.64, 1.17, and 1.62 g/d in men. The intake of ALA was modestly correlated with intake of LA (Pearson correlation =0.42, p<0.0001), but there was no correlation between intakes of ALA and n-3 LCPUFA (Pearson correlation =-0.005, p=0.007).
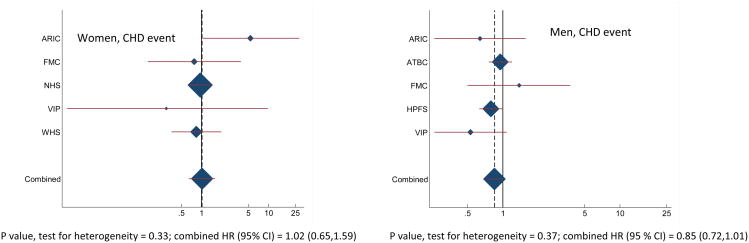
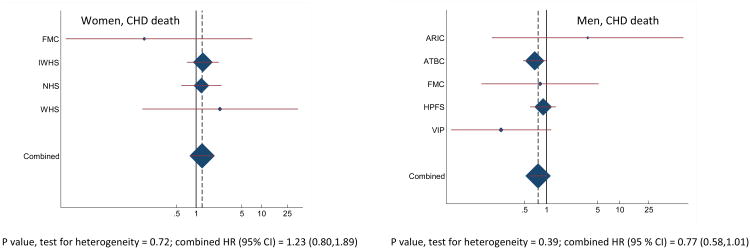
Combined HRs and 95% CI for CHD events and deaths for an increase of 1g/din intake of ALA are shown in Table 2. There was a tendency towards a significant effect modification by gender for ALA vs. CHD death (P for interaction = 0.07). Among men, we found a non-significant inverse association between intake of ALA and CHD events and deaths. For each additional gram of ALA, there was a 15 % lower risk of CHD events (HR: 0.85; 95% CI: 0.72, 1.01) and a 23% lower risk of CHD deaths (HR: 0.77; 95% CI 0.58, 1.01). Among women, we found no consistent association between intake of ALA and risk of CHD events (HR: 1.02; 95% CI 0.65, 1.59) or CHD deaths (HR: 1.23; 95% CI 0.80, 1.89). Due to the fact that ARIC study used the FFQ with only 66 items, we made additional analysis where we excluded ARIC; however, this did not change the findings (data not shown). The study-specific and combined HRs and 95% CI for CHD events and deaths for an increase of 1 g/d in intake of ALA are shown in Figure 1 and Figure 2. The test for presence of heterogeneity among the individual studies did not indicate any significant differences (among women, P for heterogeneity between studies were 0.33 and 0.72 for CHD events and deaths, respectively, and among men, 0.37 and 0.39 for CHD events and deaths, respectively). In analyses with ALA intake in quintiles, the lowest risk of CHD events was among those in the fifth quintile compared with those in the first quintile, among both women and men, but the differences were not significant (data shown in supplementary material, figure 1s). Among men, the lowest risk of CHD death was also found in the fifth quintile compared to those in the first quintile, but this too was not significant (data shown in supplementary material, figure 1s). When ALA intake was evaluated as higher (≥median) compared to lower (<median) intake among men, there was a significantly lower risk of CHD event among men with an ALA intake above median (1.17 g/d) compared to those with an intake below the median ALA intake (HR: 0.91; 95% CI: 0.83,1.00). No significant differences were found among women when intake of ALA was evaluated as higher (≥median) compared to lower (<median), or among men when the outcome was CHD death(data shown in supplementary material, table 1s).
Table 2. Combined risk of coronary heart (CHD) events and deaths for an additional intake of 1 g/d of alpha-linolenic acid (ALA).
| All | Women | Men | ||
|---|---|---|---|---|
|
| ||||
| HR (95 % CI) | P for effect modification by gender | HR (95 % CI) | HR (95 % CI) | |
| ALA, CHD events | ||||
|
| ||||
| Model 1 | 0.94 (0.82,1.08) | 0.95 | 1.07 (0.66,1.74) | 0.95 (0.86,1.05) |
| Model 2 | 0.93 (0.84,1.04) | 0.88 | 0.96 (0.67,1.39) | 0.95 (0.86,1.05) |
| Model 3 | 0.88 (0.75,1.02) | 0.42 | 1.02 (0.65,1.59) | 0.85 (0.72,1.01) |
|
| ||||
| ALA, CHD deaths | ||||
|
| ||||
| Model 1 | 0.95 (0.82,1.09) | 0.62 | 1.04 (0.64,1.68) | 0.93 (0.80,1.09) |
| Model 2 | 0.96 (0.83,1.11) | 0.97 | 0.96 (0.64,1.45) | 0.96 (0.82,1.13) |
| Model 3 | 0.88 (0.68,1.14) | 0.07 | 1.23 (0.80,1.89) | 0.77 (0.58,1.01) |
Data are given as hazard ratios (HR) and 95% confidence intervals (CI) by using Cox proportional hazards regression. Model 1 included intake of ALA expressed in energy adjusted g/d. Age at baseline (y) and the calendar year in which the baseline questionnaire was returned were entered into the model through the strata statement. Model 2 included the variables of model 1 and the following known risk factors for CHD: smoking habits, body mass index, physical activity, educational level, history of hypertension. Model 3 included the variables of model 2 and the following dietary risk factors: alcohol intake, total energy intake (where alcohol is excluded), fibre intake, monounsaturated fatty acid, saturated fatty acid, trans fatty acids, long-chain n-3 fatty acids, and linoleic acid intake
Figure 1.
Study-specific and combined risk of coronary heart (CHD) events for each additional g/d intake of alpha-linolenic acid (ALA) in men and women in the Pooling Project of Cohort Studies on Diet and Coronary Disease. Data are given as hazard ratios (HR) and 95% confidence intervals (CI) by using Cox proportional hazards regression. The multivariate model was adjusted for age at baseline and the calendar year in which the baseline questionnaire was returned, smoking habits, body mass index, physical activity, educational level, history of hypertension, alcohol intake, total energy intake, fibre intake, monounsaturated fatty acid, trans fatty acid, saturated fatty acid, linoleic acid and n-3 LCPUFA intake. Within each study HRs with 95% CI for the incidence of a CHD event and CHD death were calculated by using Cox proportional hazard regression. The squares and horizontal lines represent the study-specific HRs and 95% CI, respectively. The area of the squares reflects the study-specific weight. The “total square” represents the pooled HRs and 95% CI. ARIC, Atherosclerosis risk in Communities Study; ATBC, Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study; FMC, Finnish Mobile Clinic Health Examination Survey; HPFS, Health Professionals Follow-up Study; IWHS, Iowa Women's Health Study; NHS, Nurses' Health Study; VIP, Västerbotten Intervention Program; WHS, Women's Health Study.
Figure 2.
Study-specific and combined risk of coronary heart (CHD) death for each additional g/d intake of alpha-linolenic acid (ALA) in men and women in the Pooling Project of Cohort Studies on Diet and Coronary Disease. Data are given as hazard ratios (HR) and 95% confidence intervals (CI) by using Cox proportional hazards regression. The multivariate model was adjusted for age at baseline and the calendar year in which the baseline questionnaire was returned, smoking habits, body mass index, physical activity, educational level, history of hypertension, alcohol intake, total energy intake, fibre intake, monounsaturated fatty acid, trans fatty acid, saturated fatty acid, linoleic acid and n-3 LCPUFA intake. Within each study HRs with 95% CI for the incidence of a CHD event and CHD death were calculated by using Cox proportional hazard regression. The squares and horizontal lines represent the study-specific HRs and 95% CI, respectively. The area of the squares reflects the study-specific weight. The “total square” represents the pooled HRs and 95% CI. ARIC, Atherosclerosis risk in Communities Study; ATBC, Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study; FMC, Finnish Mobile Clinic Health Examination Survey; HPFS, Health Professionals Follow-up Study; IWHS, Iowa Women's Health Study; NHSb, Nurses' Health Study; VIP, Västerbotten Intervention Program; WHS, Women's Health Study.
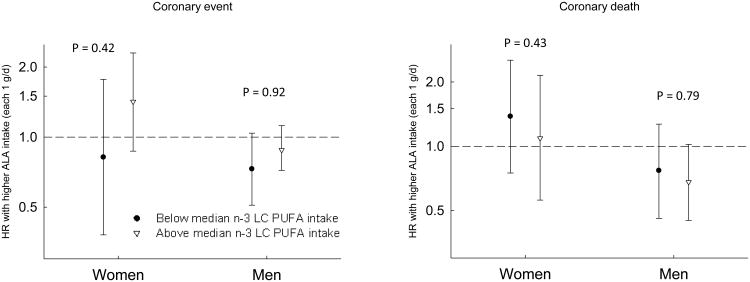
When we assessed if the association between ALA intake and risk of CHD was modified by n-3 LCPUFA, ALA intake was found to be most strongly associated with risk of CHD events among men (Figure 3). However, none of the analyses were significant and no effect modification was observed. Making the same analyses as those used to figure 3, but with the cut off values of n-3 LCPUFA of 0.1 g, suggested by Mozaffarian et al. (14), the analyses were not possible, due to a limited number of cases in the lowest group. In interaction-analysis with a common reference (low ALA intake and low n-3 LCPUFA intake), the lowest risk of CHD event among women was observed when ALA intake was high and n-3 LCPUFA was low (HR: 0.83; 95 % CI: 0.68, 1.02, P for trend = 0.06) compared to women with a low intake of both types of n-3 PUFA (supplementary material, table 2s). Among men, the lowest risk of CHD was observed when both ALA and n-3 LCPUFA intakes were high. In age stratified analyses, the intake of ALA was not significantly associated with risk of CHD, and no effect modification by age was observed (data not shown).
Figure 3.
Risk of coronary (CHD) event associated with each 1 g/d of alpha-linolenic acid (ALA) intake, among men and women with a long-chain n-3 fatty acid (n-3 LCPUFA) intake below (black circle) or above (white triangle) the median intake (women: 0.15 g/d; men: 0.26 g/d). Data are given as hazard ratios (HR) by using Cox proportional hazards regression and error bars indicate 95% confidence intervals (CI). The model was adjusted for age at baseline and the calendar year in which the baseline questionnaire was returned, smoking habits, body mass index, physical activity, educational level, history of hypertension, alcohol intake, total energy intake, fibre intake, monounsaturated fatty acid, trans fatty acid, saturated fatty acid, linoleic acid intake.
Discussion
In this study of dietary intake of ALA and risk of CHD, we found a non-significant inverse association between dietary intake of ALA and the risk of an incident CHD event and CHD death among men. The pooling of data from eight large cohorts is a major strength of the present study and allowed studying the association between intake of ALA and risk of CHD among women and men in different populations with different diets and over a wide range of intakes. Variations in intake are essential for the ability to detect potential associations with health. Furthermore, an advantage of using a pooling study design rather than a meta-analysis is that this design greatly reduces risk of publication bias, because results came both from studies that did not previously publish on association between ALA and risk of CHD and studies that did. Indeed, only three of the eight studies included (NHS (26;32) ATBC (28), and HPFS (14;33)) had reported results from such analysis earlier. Another strength of this pooled study is that data on intake of ALA as well as covariates were harmonized and the same statistical approach was used across all studies. Habitual diet was determined by validated FFQs or from dietary history interviews. ALA levels in human tissue may provide a more accurate measure of habitual ALA intake than dietary records or questionnaires. However, ALA status in tissues may be influenced by metabolic differences between subjects with regard to genetic, gender and background diet, and day-to-day variation in tissue levels cannot be excluded either. The fact that our particular pooling study of prospective cohorts required an assumption of no changes in diet over time may also contribute to measurement error over time. To reduce this, repeated measurements are a solution but were only available on a small selected subset. Further, the PUFA composition of foods e.g. butter have changed over time meaning that even though people have used the same type and amount of butter during their lifetime, their fatty acid intakes have changed. This change is partly explained by the change in feeding of ruminants with concentrated cereal-grain-based feed rather than grass which is naturally higher in ALA. At the study inception in 1986 approximately 15-20% of ALA came from beef and dairy sources in the NHS and HPFS, but this percentage waned with follow-up.
The fatty acid compositions vary a lot in ready-made dishes and take away food, as well as in biscuits and cakes (depending on whether the fat used, is of animal or plant origin). Furthermore, ALA (and fat in general) is difficult to recognize and quantify, in questionnaires and interviews, due to its role in food preparation – frying and cooking as well as a component in sauces and dressings. This could lead to random misclassification of ALA intake, which may result in attenuation of associations. In the United States e.g. in NHS and HPFS the primary source of ALA is derived from intakes of mayonnaise or other creamy dressings or oil and vinegar salad dressing, which may be difficult to quantify in FFQs. Because salad dressings are major sources of ALA, ALA may be a proxy for vegetable intake; therefore it could have been interesting to make stratified analyses on intake of vegetables/salad, in an attempt to remove confounding by intake of vegetables/salad. We did not make any adjustment for vegetable/salad intake, because we do not have these data for all the cohorts included in the Pooling Project of Cohort Studies on Diet and Coronary Disease, and one principle of pooling is to treat all cohorts the same (same confounders). However, a previous study using data from only NHS have made further adjustment of vegetable intake without any change in their results (26). However, the association could still have been influenced by a generally healthier lifestyle and diet of those who consumed most vegetables or salad. Another challenge in evaluating associations between ALA and risk of CHD, is that LA and ALA intakes are difficult to separate, as they are often present in the same product e.g. soybean oil, margarine and mayonnaise. However, in the present study the correlation coefficient was only 0.42, thus enabling statistical adjustment of LA intake in the multivariate analyses.
Several prospective cohort studies have evaluated the association between ALA intake and risk of CHD and found inconsistent results (14;26;28;32-34). Indeed, our findings are in line with a recent meta-analysis from 2012 of 13 prospective studies showing that higher ALA intakes (each 1 g/d increment) were associated with a 10% lower risk of incident CVD (HR: 0.90, 95% CI: 0.81,0.99) (11). However, in the evaluation of ALA intake and risk of CVD subtypes, CHD events and CHD death, only three studies were included in the meta-analysis of CHD event and six studies in the analysis of CHD death and the association was only significant for ALA intake and CHD death (HR: 0.80, 95% CI: 0.65, 0.98) (ALA and CHD event: HR: 0.84, 95% CI; 0.61, 1.15). Four of these nine studies used cohorts that were also included in the present study (NHS, HPFS and ATBC). Only two of the nine studies considered women (data from NHS) (26;32), six were conducted solely in men (28;33;35-38), whereas the last study had a mix of the two gender with 27% women and 73% men (39). In the present study, we found different results for women and men. Whether the different results for women and men, reflect true biological differences, or are due to power, or are caused by some kind of bias, remains to be seen. On the other hand, an inverse association between ALA and risk of CHD is theoretically more likely among the women than among the men, as several studies have shown that the conversion of ALA to n-3 LCPUFA is stimulated by estrogen and is greater in women (12;13). Two prior studies in women that evaluated the associations between ALA and risk of CHD, both with data from NHS have been made (26;32) and both were included in the recent meta-analysis by Pan et al. (11). In one of these studies(26), Hu et al. found that ALA intake was associated with a lower risk of CHD death (after 10 years of follow-up). In the other study, by Albert et al. (32), analysis were performed for both sudden death and overall CHD death and this showed no association between ALA intake and risk of total CHD death (after 18 years of follow-up). Albert et al. (32) concluded that the benefit of ALA on CHD death found by Hu et al. (26), was likely to be due to a benefit on sudden death, which account for a higher proportion of CHD death in the younger women. Both of these studies using NHS, used a simple updated analysis that used the most recent ALA value available, which may explain the deviation of the results from NHS in the present study. Furthermore, the age distribution in the present study, was similar for both men and women, but the number of female cases was lower (death =560, event = 1,156) than that of men (death = 1,191, event = 3,337), because women in general are older when they experience CHD. Therefore the estimate of an association between ALA and risk of CHD among women may be statistically uncertain, which may also, explain the different results.
Mozaffarian et al. (14) showed that each additional 1 g/d intake of ALA was associated with a 58 % lower risk of CHD event (HR: 0.42, 95% CI: 0.23,0.75) among men with low n−3 LCPUFA intakes (<0.1g/d), whereas ALA intake was not associated with risk of CHD events among men with a higher n-3 LCPUFA intakes (≥0.1g/d), P for interaction = 0.0006. In the present study, among men intakes of n-3 LCPUFA below the median (<0.26 g/d), each 1 g/d of ALA intake was associated with a 27% lower risk of CHD events (HR: 0.73; 95% CI: 0.51, 1.04) but among men with intakes of n-3 LCPUFA above the median there was no significant association (HR: 0.90; 95 % CI: 0.72,1.12), P for interaction = 0.92. Further, we found no effect modification by n-3 LCPUFA among the women. Albert et al. (32) have showed an additive effect of ALA and n−3 LCPUFA, indicating that the lowest risk of sudden cardiac death occurred among those with the highest intakes of both ALA and n-3 LCPUFA. In the present study, the lowest risk of CHD event and death among men was observed at high intake of both ALA and n-3 LCPUFA, although not significant. However, among women, the lowest risk of CHD event among women was observed when ALA intake was low and n-3 LCPUFA was high (HR: 0.83; 95 % CI: 0.68, 1.02, P for trend = 0.06) compared to women with a low intake of both types of n-3 PUFA. Although CHD death and CHD event are both atherosclerotic disorders and have common risk factors, we found signs of differential effect modification by n-3 LCPUFA on the association between ALA intake and risk depending on whether the outcome was CHD event or CHD death. However, ALA may be more important in individuals with low n-3 LCPUFA because these individuals need ALA, whereas individuals with high n-3 LCPUFA do not need it to achieve optimal levels of n-3 LCPUFA – so it may not be so much the feedback inhibition, but the deficiency in n-3 LCPUFA itself that matters. In our previous study on Danish men and women (40), we found no effect modification by n-3 LCPUFA on the association between ALA intake and risk of CHD.
Conclusion
In this large pooled study of dietary intake of ALA and risk of CHD, there was an tendency of an inverse association between dietary ALA and risk of CHD among men, however not significant. No consistent associations were observed among women. This study is the largest and most powerful study evaluating the association of ALA and risk of CHD to date. Given that a higher ALA intake was found to reduce the risk of CHD, although only among men, from a public health point of view, it may be feasible to increase ALA intake. Canola oil (which is high in ALA) is the cheapest oil in many countries, and thus can be used in household cooking by a majority of populations. However, canola oil is best for raw use (i.e. salad dressing) and not for heating due to its degree of unsaturation. Other sources of ALA are for instance walnuts and flaxseeds, although they are not as common in all populations. To have 1 g of ALA one have to consume 2 teaspoons of canola oil or 15 gram of walnuts or 6 g of flaxseed. Gender differences in prospective cohort studies have received little attention and deserve further investigation.
Supplementary Material
Acknowledgments
We are grateful to Alberto Ascherio and Aaron Folsom, for their comments on the manuscript and involvement in the Pooling Project of Cohort Studies on Diet and Coronary Disease. We are also thankful to Gearóid O'Reilly for statistical assistance. The authors thank the staff and participants of the Atherosclerosis Risk In Communities Study, the Alpha-Tocopherol and Beta-Carotene Cancer Prevention Study, the Finnish Mobile Clinic Health Study, the Health Professionals Follow-up Study, the Iowa Women's Health Study, the Nurses' Health Study, the Västerbotten Intervention Program, and the Women's Health Study for their important contributions.
Financial support: This work is carried out as a part of the research program of the Danish Obesity Research Centre (DanORC). DanORC is supported by the Danish Council for Strategic Research (Grant 2101-06-0005). National Institute of Health grants: P01 CA87969 (NHS), UM1 CA167552 (HPFS) and R01 HL58904.
Footnotes
Conflict of interest: None
Authorship: The authors' responsibilities were as follows; MSV, MUJ, LL and BLH: study concept and design; MSV, MUJ, LL, BLH, GH, GC, JB, PK, JV, LMS, KB, EBR, EJO: interpretation of data and critical revision of the manuscript; MSV: draft of the manuscript; and MSV and EJO: statistical analysis.
References
- 1.WHO, World Heart Federation, World Stroke Organization. Global atlas on cardiovascular disease prevention and control. 2011 [Google Scholar]
- 2.Bang HO, Dyerberg J, Hjoorne N. The composition of food consumed by Greenland Eskimos. Acta Med Scand. 1976;200(1-2):69–73. doi: 10.1111/j.0954-6820.1976.tb08198.x. [DOI] [PubMed] [Google Scholar]
- 3.Hansen SN, Harris WS. New evidence for the cardiovascular benefits of long chain omega-3 fatty acids. Curr Atheroscler Rep. 2007 Dec;9(6):434–40. doi: 10.1007/s11883-007-0058-8. [DOI] [PubMed] [Google Scholar]
- 4.Harris WS, Miller M, Tighe AP, Davidson MH, Schaefer EJ. Omega-3 fatty acids and coronary heart disease risk: clinical and mechanistic perspectives. Atherosclerosis. 2008 Mar;197(1):12–24. doi: 10.1016/j.atherosclerosis.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Harris WS, Kris-Etherton PM, Harris KA. Intakes of long-chain omega-3 fatty acid associated with reduced risk for death from coronary heart disease in healthy adults. Curr Atheroscler Rep. 2008 Dec;10(6):503–9. doi: 10.1007/s11883-008-0078-z. [DOI] [PubMed] [Google Scholar]
- 6.Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol. 2011 Nov 8;58(20):2047–67. doi: 10.1016/j.jacc.2011.06.063. [DOI] [PubMed] [Google Scholar]
- 7.Delgado-Lista J, Perez-Martinez P, Lopez-Miranda J, Perez-Jimenez F. Long chain omega-3 fatty acids and cardiovascular disease: a systematic review. Br J Nutr. 2012 Jun;107(Suppl 2):S201–S213. doi: 10.1017/S0007114512001596. [DOI] [PubMed] [Google Scholar]
- 8.Brouwer IA, Katan MB, Zock PL. Dietary alpha-linolenic acid is associated with reduced risk of fatal coronary heart disease, but increased prostate cancer risk: a meta-analysis. J Nutr. 2004 Apr;134(4):919–22. doi: 10.1093/jn/134.4.919. [DOI] [PubMed] [Google Scholar]
- 9.Wang C, Harris WS, Chung M, Lichtenstein AH, Balk EM, Kupelnick B, et al. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr. 2006 Jul;84(1):5–17. doi: 10.1093/ajcn/84.1.5. [DOI] [PubMed] [Google Scholar]
- 10.Geleijnse JM, de GJ, Brouwer IA. Alpha-linolenic acid: is it essential to cardiovascular health? Curr Atheroscler Rep. 2010 Nov;12(6):359–67. doi: 10.1007/s11883-010-0137-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pan A, Chen M, Chowdhury R, Wu JH, Sun Q, Campos H, et al. alpha-Linolenic acid and risk of cardiovascular disease: a systematic review and meta-analysis. Am J Clin Nutr. 2012 Oct 17; doi: 10.3945/ajcn.112.044040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burdge G. Alpha-linolenic acid metabolism in men and women: nutritional and biological implications. Curr Opin Clin Nutr Metab Care. 2004 Mar;7(2):137–44. doi: 10.1097/00075197-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Decsi T, Kennedy K. Sex-specific differences in essential fatty acid metabolism. Am J Clin Nutr. 2011 Dec;94(6 Suppl):1914S–9S. doi: 10.3945/ajcn.110.000893. [DOI] [PubMed] [Google Scholar]
- 14.Mozaffarian D, Ascherio A, Hu FB, Stampfer MJ, Willett WC, Siscovick DS, et al. Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation. 2005 Jan 18;111(2):157–64. doi: 10.1161/01.CIR.0000152099.87287.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fraser GE, Strahan TM, Sabate J, Beeson WL, Kissinger D. Effects of traditional coronary risk factors on rates of incident coronary events in a low-risk population. The Adventist Health Study. Circulation. 1992 Aug;86(2):406–13. doi: 10.1161/01.cir.86.2.406. [DOI] [PubMed] [Google Scholar]
- 16.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989 Apr;129(4):687–702. [PubMed] [Google Scholar]
- 17.The alpha-tocopherol, beta-carotene lung cancer prevention study: design, design, methods, participant characteristics, and compliance. The ATBC Cancer Prevention Study Group. Ann Epidemiol. 1994 Jan;4(1):1–10. doi: 10.1016/1047-2797(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 18.Knekt P, Reunanen A, Jarvinen R, Seppanen R, Heliovaara M, Aromaa A. Antioxidant vitamin intake and coronary mortality in a longitudinal population study. Am J Epidemiol. 1994 Jun 15;139(12):1180–9. doi: 10.1093/oxfordjournals.aje.a116964. [DOI] [PubMed] [Google Scholar]
- 19.Schroll M, Jorgensen T, Ingerslev J. The Glostrup Population Studies, 1964-1992. Dan Med Bull. 1992 Jun;39(3):204–7. [PubMed] [Google Scholar]
- 20.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992 May 15;135(10):1114–26. doi: 10.1093/oxfordjournals.aje.a116211. [DOI] [PubMed] [Google Scholar]
- 21.Goldbourt U, Yaari S. Cholesterol and coronary heart disease mortality. A 23-year follow-up study of 9902 men in Israel. Arteriosclerosis. 1990 Jul;10(4):512–9. doi: 10.1161/01.atv.10.4.512. [DOI] [PubMed] [Google Scholar]
- 22.Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong CP, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med. 2000 Jul 24;160(14):2117–28. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 23.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985 Jul;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 24.Winkvist A, Hornell A, Hallmans G, Lindahl B, Weinehall L, Johansson I. More distinct food intake patterns among women than men in northern Sweden: a population-based survey. Nutr J. 2009;8:12. doi: 10.1186/1475-2891-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women's Health Study: a randomized controlled trial. JAMA. 2005 Jul 6;294(1):56–65. doi: 10.1001/jama.294.1.56. [DOI] [PubMed] [Google Scholar]
- 26.Hu FB, Stampfer MJ, Manson JE, Rimm EB, Wolk A, Colditz GA, et al. Dietary intake of {alpha}-linolenic acid and risk of fatal ischemic heart disease among women. Am J Clin Nutr. 1999 May 1;69(5):890–7. doi: 10.1093/ajcn/69.5.890. [DOI] [PubMed] [Google Scholar]
- 27.Pietinen P, Hartman AM, Haapa E, Rasanen L, Haapakoski J, Palmgren J, et al. Reproducibility and validity of dietary assessment instruments. I. A self-administered food use questionnaire with a portion size picture booklet. Am J Epidemiol. 1988 Sep;128(3):655–66. doi: 10.1093/oxfordjournals.aje.a115013. [DOI] [PubMed] [Google Scholar]
- 28.Pietinen P, Ascherio A, Korhonen P, Hartman AM, Willett WC, Albanes D, et al. Intake of Fatty Acids and Risk of Coronary Heart Disease in a Cohort of Finnish Men: The Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Am J Epidemiol. 1997 May 15;145(10):876–87. doi: 10.1093/oxfordjournals.aje.a009047. [DOI] [PubMed] [Google Scholar]
- 29.Mizrahi A, Knekt P, Montonen J, Laaksonen MA, Heliovaara M, Jarvinen R. Plant foods and the risk of cerebrovascular diseases: a potential protection of fruit consumption. Br J Nutr. 2009 Oct;102(7):1075–83. doi: 10.1017/S0007114509359097. [DOI] [PubMed] [Google Scholar]
- 30.Pereira MA, O'Reilly E, Augustsson K, Fraser GE, Goldbourt U, Heitmann BL, et al. Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch Intern Med. 2004 Feb 23;164(4):370–6. doi: 10.1001/archinte.164.4.370. [DOI] [PubMed] [Google Scholar]
- 31.Jakobsen MU, O'Reilly EJ, Heitmann BL, Pereira MA, Balter K, Fraser GE, et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009 May;89(5):1425–32. doi: 10.3945/ajcn.2008.27124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Albert CM, Oh K, Whang W, Manson JE, Chae CU, Stampfer MJ, et al. Dietary alpha-linolenic acid intake and risk of sudden cardiac death and coronary heart disease. Circulation. 2005 Nov 22;112(21):3232–8. doi: 10.1161/CIRCULATIONAHA.105.572008. [DOI] [PubMed] [Google Scholar]
- 33.Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ. 1996 Jul 13;313(7049):84–90. doi: 10.1136/bmj.313.7049.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de GJ, Verschuren WM, Boer JM, Kromhout D, Geleijnse JM. Alpha-linolenic acid intake and 10-year incidence of coronary heart disease and stroke in 20,000 middle-aged men and women in the Netherlands. PLoS One. 2011;6(3):e17967. doi: 10.1371/journal.pone.0017967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dolecek TA, Granditis G. Dietary polyunsaturated fatty acids and mortality in the Multiple Risk Factor Intervention Trial (MRFIT) World Rev Nutr Diet. 1991;66:205–16. doi: 10.1159/000419291. [DOI] [PubMed] [Google Scholar]
- 36.Oomen CM, Ocke MC, Feskens EJ, Kok FJ, Kromhout D. alpha-Linolenic acid intake is not beneficially associated with 10-y risk of coronary artery disease incidence: the Zutphen Elderly Study. Am J Clin Nutr. 2001 Oct;74(4):457–63. doi: 10.1093/ajcn/74.4.457. [DOI] [PubMed] [Google Scholar]
- 37.Laaksonen DE, Nyyssonen K, Niskanen L, Rissanen TH, Salonen JT. Prediction of Cardiovascular Mortality in Middle-aged Men by Dietary and Serum Linoleic and Polyunsaturated Fatty Acids. Arch Intern Med. 2005 Jan 24;165(2):193–9. doi: 10.1001/archinte.165.2.193. [DOI] [PubMed] [Google Scholar]
- 38.Lopes C, Aro A, Azevedo A, Ramos E, Barros H. Intake and adipose tissue composition of fatty acids and risk of myocardial infarction in a male Portuguese community sample. J Am Diet Assoc. 2007 Feb;107(2):276–86. doi: 10.1016/j.jada.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 39.Campos H, Baylin A, Willett WC. Alpha-linolenic acid and risk of nonfatal acute myocardial infarction. Circulation. 2008 Jul 22;118(4):339–45. doi: 10.1161/CIRCULATIONAHA.107.762419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vedtofte MS, Jakobsen MU, Lauritzen L, Heitmann BL. Dietary alpha-linolenic acid, linoleic acid, and n-3 long-chain PUFA and risk of ischemic heart disease. Am J Clin Nutr. 2011 Oct;94(4):1097–103. doi: 10.3945/ajcn.111.018762. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.