Abstract
Metachromatic Leukodystrophy is a rare disorder with great clinical variability. We report the first case of triplets with the late infantile form of the disease and their systematic progression of symptoms. We reviewed the literature and identified all human studies that reported new cases since 1921. We analyzed survival by decade to assess the impact of historical changes in management of care. Mean age at death and 5-year survival from onset of symptoms for late infantile, juvenile and adult phenotype were 4.2 years and 24.9%, 17.4 years and 70.3%, and 43.1 years and 88.6% respectively. 5-year survival of cases reported after 1990 was significantly better than cases reported before 1970 in all subtypes of metachromatic leukodystrophy (late infantile: 52% vs. 14%, juvenile: 100% vs. 46%, adult: 95% vs. 67%). Survival in the late infantile subtype was worse than in other subtypes. Survival significantly improved over time in all subtypes.
Keywords: metachromatic leukodystrophy, demyelination
Introduction
Metachromatic Leukodystrophy is an autosomal recessive inherited disease with a deficiency of the lysosomal enzyme arylsulfatase A1. This results in accumulation of sulfated glycolipids in the myelin sheaths of the nervous system and to a lesser extent in visceral organs like liver, gallbladder and kidney1. In the central nervous system this accumulation results in progressive demyelination. metachromatic leukodystrophy is subdivided into three clinical subtypes according to age of onset: late-infantile, juvenile and adult 1,2. The impact of genetic and environmental factors is not well understood.
Clinical, radiological and laboratory findings in these subtypes have previously been reported, however the composite overall survival of these patients remains unknown. To explore this further we reviewed the literature since description of the first metachromatic leukodystrophy patient in 19213. We describe triplets with late infantile onset metachromatic leukodystrophy, two identical and one fraternal, who share a common environment, have the same genetic mutations and demonstrate a remarkable synchronicity in neurological decline.
Case Report
The triplets were born via cesarean section at 29 weeks gestation. Two boys were identical twins and one was fraternal. The mother had suffered from fetal alcohol syndrome and had a history of developmental delay and depression. Aside from bed rest, the pregnancy was unremarkable. Their Apgar scores were 8 and 8 at 1 and 5 minutes respectively. They had a typical neonatal intensive care unit course, which included evaluation for sepsis and possible necrotizing enterocolitis, apnea and bradycardia. Cranial ultrasounds revealed no intracranial hemorrhage. The triplets were in the neonatal intensive care unit for approximately two months and then discharged home on routine oral feedings without a requirement for supplemental oxygen or medications.
Initially, developmental progress was achieved in all domains. The triplets rolled over at 10 months, sat up at 11 months, began crawling at 12 months and walking at 15 months. By 16 months they were speaking in 2 to 3 word sentences, feeding themselves with utensils and adequately navigating through fine motor tasks.
Around 16 months of age, there was a rapid and striking change in development in the three boys. Regression in motor skills was recognized first. The gross motor skills were more affected than the fine motor skills. They lost their ability to walk, crawl, sit up, and roll over. Loss of head control followed. During that time, the family noted left-sided ptosis in all three. Over the next few weeks their speech and language skills declined to the expression of one-syllable words. They also lost fine motor skills and pincer grasp. Deep tendon reflexes were preserved.
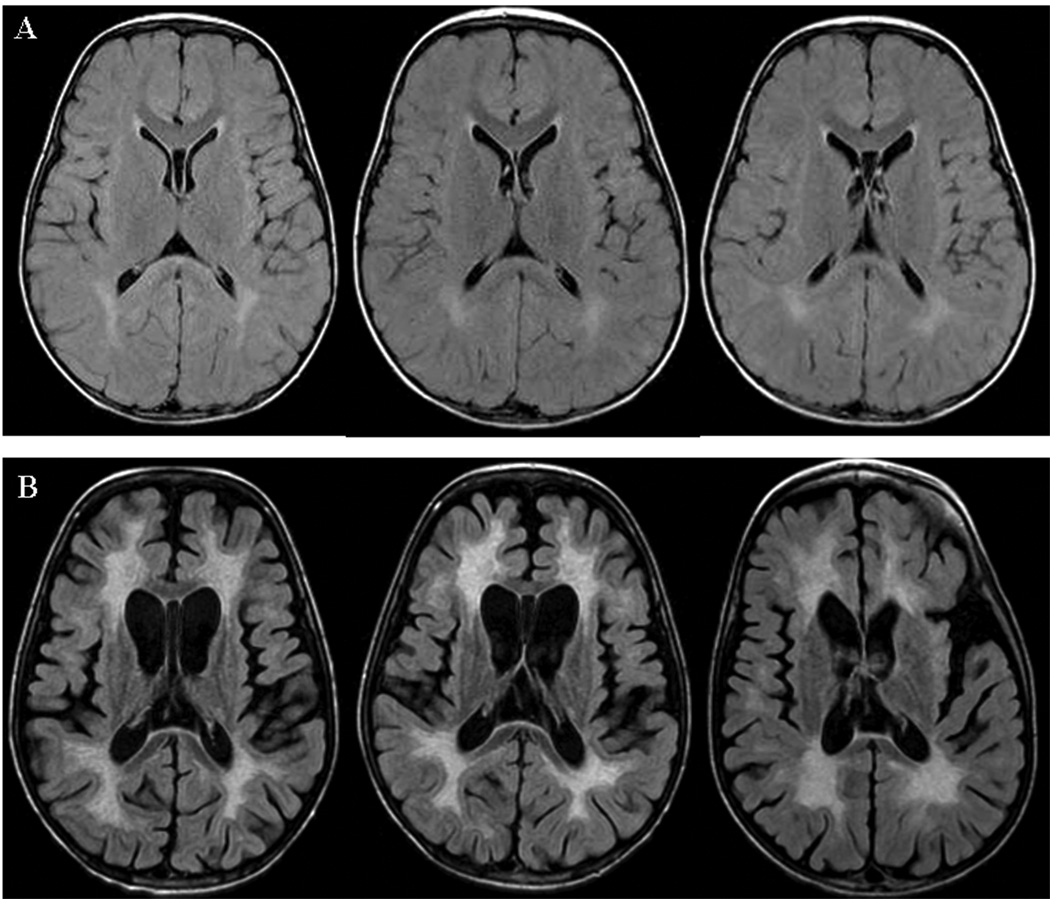
A battery of metabolic and genetic testing was performed, including plasma amino acids, urine organic acids, cerebrospinal fluid neurotransmitters and amino acids. All were within normal range. A brain MRI showed T2 hyperintense periventricular lesions that were difficult to distinguish from normal terminal myelination zones (Figure 1A). Measurement of arylsulfatase A activity in leukocytes showed levels of 4.5, 7.8 and 8.1 nmol/h/mg protein in the triplets versus a normal mean of about 80 nmol/h/mg protein. Urine analysis showed an increase in sulfatides, confirming the diagnosis of metachromatic leukodystrophy. DNA analysis revealed one copy of the common LI mutation (G459+1A) in each child. The other mutation in these children is a deletion starting between intron 6 and exon 8 and extending beyond the end of the gene. These are both severe mutations likely to lead to a late infantile presentation.
Figure 1.
Brain MRI of triplets at 15 months (A) and 4 years (B) of age. Axial fast fluid-attenuated inversion recovery (repetition time = 10,000 milliseconds, echo time = 140 milliseconds, inversion time: 2200 milliseconds) images are shown.
By 24 months of age, they developed progressive truncal hypotonia with peripheral spasticity. All three displayed persistent fisting of the hands, facial weakness, and diffuse hyperreflexia. A nerve conduction study revealed normal conduction velocities in the median, ulnar, tibial and peroneal nerves.
At 36 months of age they began to complain of pain with minimal passive movement of the limbs, particularly the legs. This was aggravated during activities such as dressing and physical activity but did not occur at rest or when unprovoked. Pain episodes led to increased dystonia and worsened spasticity. Progressive lower extremity spasticity, especially in the gastrocnemius, led to plantar flexion of the feet at rest. Baclofen was initiated to alleviate the worsening spasticity. Hip radiographs did not reveal uncovering of subluxation of the femoral heads. Regarding development, they continued to use single words, identify body parts through pointing, smile and have meaningful interactions with their parents and caregivers.
In the subsequent months they developed oromotor dysfunction and difficulty with weight gain. A swallow study documented aspiration of thin liquids. All three children underwent surgery for gastric tube placement. For the next several months, no aspiration problems or airway obstruction occurred. None of the triplets had seizures, either clinically or electrographically. Gastric motility slowed and continuous feeds with frequent breaks and venting were required to maintain comfort. Gabapentin was initiated to help with neuropathic-enteral pain. Over time, the boys’ nutritional status declined secondary to the feeding intolerance. They developed iron deficiency. A follow-up MRI was performed at 4 years of age and confirmed radiographic progression of white matter disease in all three (see Figure 1B). The boys became less interactive and required increased levels of voice and tactile stimulation to respond.
Literature Review Methods
We undertook a systematic review to identify human studies of metachromatic leukodystrophy that reported new cases. We searched PubMed from 1920 through June 30th, 2006 using the terms: “Metachromatic”, “Leukodystrophy”, “MLD” (metachromatic leukodystrophy), and combinations of these terms. Additionally, we manually reviewed the reference lists of all the other publications for other potential data sources. This search was repeated four times by two reviewers (AM and HWM) independently. Data abstraction was done by one reviewer (AM or HWM or FE) and verified independently by one of the other two reviewers. We only included studies that reported new cases with definite diagnosis of metachromatic leukodystrophy. We used the subtypes as assigned by the original publication. In the absence of definitive subtype, we assigned the subtype considering manifestations, its rate of progression and age at the onset of symptoms (late infantile: 0.5–4 years, juvenile 4 – 16 years, adult > 16 years). Studies were excluded if they did not provide either: a) age at the onset of symptoms, or b) age at death or last follow-up. We also excluded studies limited exclusively to patients receiving transplants. Sufficient information on ethnicity of the patients was not available and thus it was not included in the analysis.
Survival analyses, as function of years since onset of symptoms, were performed using the Kaplan-Meier and Cox proportional hazard method and log-rank test using the statistical software package STATA 8 (College station, Texas). When the date of death was not known, the record was censored in the analysis as of the date of last follow-up. To assess the impact of historical changes in management of care we analyzed survival by decade in the three phenotypes.
Results
We identified 142 eligible studies and information about 303 cases was extracted. The first included case occurred in 1921,reported by Witte et al3. Ninety-eight patients of the late infantile subtype from 50 studies4–53, 78 patients of the juvenile subtype from 42 studies22, 24, 26, 27, 30, 49, 50, 54–88, and 127 patients of the adult onset subtype from 69 studies3, 7, 14, 22, 27, 30, 81–144 were identified and are summarized in Table 1.
Table 1.
Characteristics of three subtypes of Metachromatic Leukodystrophy.
| Phenotype | N | Sex | Age of onset in Years |
Follow-up Period in Years |
Survival Probability** | ||||
|---|---|---|---|---|---|---|---|---|---|
| # of Male(%)* |
Mean (SD) |
Median (IQR) |
Mean (SD) |
Median (IQR) |
Median | 5-Year | 10-Year | ||
| Late Infantile |
98 | 36 (45%) | 1.49 (0.5) |
1.5 (0.69) |
2.6 (1.8) | 2.1 (2.3) | 2.7 | 25.1% | 0% |
| Juvenile | 78 | 36 (49%) | 10 (4.3) | 10 (7) | 6.3 (5.3) | 5 (5) | 9 | 70.3% | 44.3% |
| Adult | 127 | 67 (52.7%) |
27.2 (10.1) |
25 (14) | 8.8 (8.4) | 6 (8) | 25 | 87.1% | 69.6% |
SD: Standard Deviation, IQR: Interquartile range
Sex of 23 patients was not reported in the study.
Survival as a function of years since onset of symptoms
Symptoms in the late infantile group were poorly reported in general but well illustrated in our case report. Out of 38 late infantile cases for which detailed clinical features were provided, 61% patients presented with motor or gait abnormalities and 39% patients presented with seizures. In the juvenile group, 66% presented with inattention and difficulties at school, 26% with gait difficulties, 18% with tremor or ataxia, 13% with neuropathy and 5% with seizures. In the adult group, 72% presented with dementia and behavioral difficulties, 16% with psychosis and schizophrenia, 28% with neuropathy, and 12% with seizures.
Survival
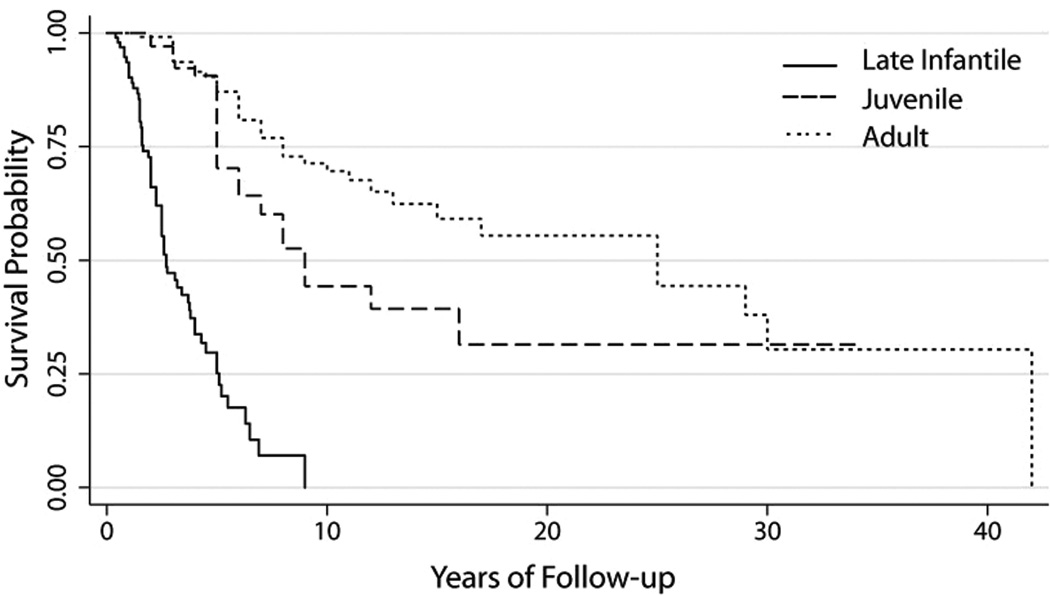
In all three subtypes, both sexes were equally affected, and there was no gender difference in survival (late infantile p=0.115, juvenile p=0.955, adult p=0.688). In the late infantile subgroup, 62/98 (63.3%) of patients were reported to have died at a mean age of 4.2 years. In the juvenile subgroup, 30/75 (38.5%) patients died at a mean age of 17.4 years. In the adult subtype, 35/127 (28%) died at a mean age of 43.1 years. 5-year and 10-year survival in these types are depicted in table 1 and figure 2.
Figure 2.
Comparison of survival probability from onset of symptoms in the three subtypes of metachromatic leukodystrophy.
When comparing survival in patients whose manifestation started before two years of age (n=79) with patients who manifested at and after two years (n=19), we did not find any significant difference (p=0.765). Similarly in the juvenile subtype, a cut-off of six years of age at initial manifestation did not affect the survival [4–6 group (n=13) versus 6–16 group (n=61), p=0.365]. However, the 19 patients whose age at onset of disease was between two and four years (classified as late infantile) performed significantly worse than those 13 patients whose disease started between four and six years (classified as juvenile) (p<0.001). Overall survival was better in patients with the adult subtype than the late infantile or juvenile subtype (p<0.001 and p=0.005 respectively).
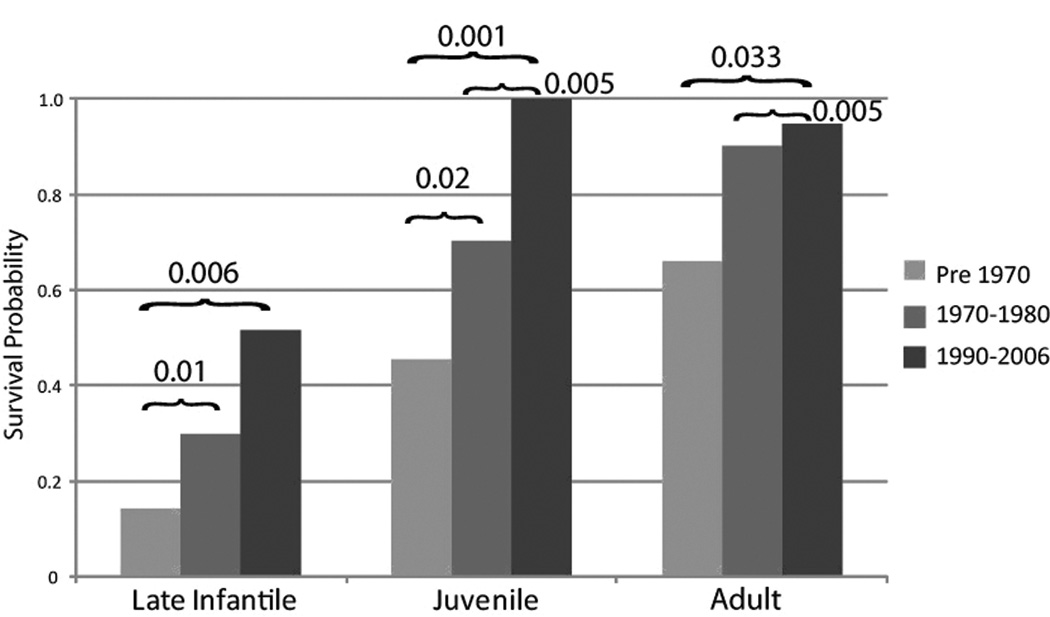
The analysis by decades (1921–2006) showed that survival significantly improved over time in all subtypes as depicted in figure 3. 5-year survival of cases reported after 1990 was significantly better than the cases reported before 1970 in all subtypes of metachromatic leukodystrophy.
Figure 3.
Comparison of 5-year survival probability in three subtypes over time.
Discussion
In this study we described the first case of triplets with the late infantile form of the disease and their systematic and synchronous progression of symptoms. We performed a pooled survival analysis of 303 metachromatic leukodystrophy cases published as single case reports and small series over a nearly 80-year period in order to shed more light on the natural history of metachromatic leukodystrophy than was previously available. Survival in the late infantile subtype was worse than the other two subtypes. Adult patients had the most favorable disease course, with a median survival from the time of diagnosis of 25 years. Interestingly, we found an increase in survival in all age groups over time, and in absence of disease modifying or curative therapies this likely reflects improvement in supportive care alone. Survival was similar in patients within the same subtype and did not change with age at symptom onset within subtype.
As our case report of triplets with progressive spastic body paresis demonstrates, disease progression in the late infantile form of metachromatic leukodystrophy is remarkably systematic. As in 61% of reported cases, the triplets’ first symptom was motor regression. They lost their ability to walk within a few days of each other due to rapid progression in lower extremity muscle tone. Left-sided ptosis was noted in all three at 32 months of age. Significant gastric dysmotility led to major feeding discomfort and malnutrition. The late infantile form of this disease is a devastating diagnosis of limited life expectancy.
Our review of historical data found that only 50% of infants with metachromatic leukodystrophy survive beyond 2.7 years after their 1st symptoms. The 5-year survival was 25%. Of note, however, milder cases may have been under-reported. Caution must be exercised in extrapolating the rate of progression from the age of death. In our experience, a rapid clinical decline does not necessitate short survival. With measures of gastric tube placement, hygiene precautions and adequate antibiotic coverage, patients can survive in a vegetative state for months and years. We note that 5-year survival has improved since 1970. Despite the fact that no changes in treatment occurred, survival improved, probably due to improved supportive care.
The initial symptoms in the juvenile and adult metachromatic leukodystrophy patients are predominated by behavioral difficulties. The insidious nature of cognitive symptoms poses problems in early recognition and challenge clinicians across disciplines. Some metachromatic leukodystrophy patients with juvenile disease can benefit from hematopoietic stem cell transplantation if performed early in the course 66, 145. Recently, adult patients with metachromatic leukodystrophy have also been transplanted. Better techniques for early diagnose are urgently needed.
While the present therapeutic options for metachromatic leukodystrophy are very limited, recent progress in the technology of enzyme replacement and gene therapy has been made146. Animal models of metachromatic leukodystrophy have been partially cured by both interventions146, 147. It remains to be seen whether enzyme replacement therapy will have long-term benefit for the central nervous system; one may envisage that it could be used in combination with other approaches. The impact of novel therapies will have to be measured against the defined clinical variability presented in our study. The survival patterns we derive from a review of the literature cannot replace a carefully conducted natural history study in order to establish the rate of progression of metachromatic leukodystrophy.
Acknowledgments
The systematic review was initiated by Dr. Hugo W. Moser who sadly passed away in January 2007. We dedicate this article to him. The authors wish to thank Ms. Anne Snitcher, and Ms Jacqueline Pittman for their assistance. Support for F.E. by NIH grant 1K08NS52550-01A1, and partial support for D.A.W. was from NIH grant DK08795.
Footnotes
The authors have no conflicts of interest.
References
- 1.von-Figura KGV, Jaeken J. Metachromatic Leukodystrophy. In: Scriver C, Beaudet A, Sly W, Valle D, editors. The Metabolic & Molecular Bases of Inherited Disease. 8 ed. McGraw-Hill: 2001. pp. 3695–3724. [Google Scholar]
- 2.Percy AMG. The Biochemistry of Myelin and Leukodystrophies. In: Vinken PBG, editor. Handbook of Clinical Neurology. Amsterdam: North Holland Publishing Co; 1970. pp. 3695–3724. [Google Scholar]
- 3.Witte F. Ueber pathologische Abbauvorgange im Zentralnervensystem. Munch. Med. Wochenschr. 1921;68:69. [Google Scholar]
- 4.Austin JH. Metachromatic form of diffuse cerebral sclerosis. I. Diagnosis during life by urine sediment examination. Neurology. 1957;7(6):415–426. doi: 10.1212/wnl.7.6.415. [DOI] [PubMed] [Google Scholar]
- 5.Austin J. Recent Studies in the Metachromatic and Globoid Body Forms of diffuse Sclerosis. In: Folch-Pi JAB H, editor. Brain Lipids and Lipoproteins and Leucodystrophies. 1st ed. New York: Elsevier Publishing Company; 1963. [Google Scholar]
- 6.Greenfield J. A form of progressive cerebral sclerosis in infants associated with primary degeneration of the interfascicular glia. J. Neurol. Psychopath. 1933:13. doi: 10.1136/jnnp.s1-13.52.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 81–1962. N Engl J Med. 1962;267(23):1198–1204. doi: 10.1056/NEJM195612202552508. [DOI] [PubMed] [Google Scholar]
- 8.Brandberg O, Sjovall E. Z Neurol. 1940;170:131. [Google Scholar]
- 9.Frank J. Arch Psychiatr Nervenkr. 1947;179(46) [Google Scholar]
- 10.Jacobi M. Arch Pathol Anat U Physiol, Virchow's. 1947;314 [PubMed] [Google Scholar]
- 11.Brain WR, Greenfield JG. Late infantile metachromatic leuco-encephalopathy, with primary degeneration of the interfascicular oligodendroglia. Brain. 1950;73(3):291–317. doi: 10.1093/brain/73.3.291. [DOI] [PubMed] [Google Scholar]
- 12.Leslie DA. Diffuse progressive metachromatic leucoencephalopathy. J Pathol Bacteriol. 1952;64(4):841–855. doi: 10.1002/path.1700640416. [DOI] [PubMed] [Google Scholar]
- 13.Bertrand I, Thieffry S, Bargeton E. [Familial leukodystrophy and spleno-hepatic determination characterizing a general metabolic disorder.] Rev Neurol (Paris) 1954;91(3):161–174. [PubMed] [Google Scholar]
- 14.Peiffer J. [On metachromatic leukodystrophy (Scholz type).] Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr. 1959;199:386–416. doi: 10.1007/BF00342847. [DOI] [PubMed] [Google Scholar]
- 15.Wohlwill FJ, Bernstein J, Yakovlev PI. Dysmyelinogenic leukodystrophy; report of a case of a new, presumably familial type of leukodystrophy with megalobarencephaly. J Neuropathol Exp Neurol. 1959;18(3):359–383. doi: 10.1097/00005072-195907000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Jervis GA. Infantile metachromatic leukodystrophy. (Greenfield's disease) J Neuropathol Exp Neurol. 1960;19:323–341. doi: 10.1097/00005072-196007000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Norman RM, Urich H, Tingey AH. Metachromatic leucoencephalopathy: a form of lipidosis. Brain. 1960;83:369–380. doi: 10.1093/brain/83.3.369. [DOI] [PubMed] [Google Scholar]
- 18.Ogawa K. Late infantile metachromatic leukodystrophy. The nature of the chromotrope. Arch Neurol. 1961;4:418–429. doi: 10.1001/archneur.1961.00450100066009. [DOI] [PubMed] [Google Scholar]
- 19.Hagberg B. Brain lipids and lipoproteins and the leukodystrophies. Amesterdam: Elsevier; 1963. Clinical Symptoms, Signs and Tests in Metachromatic Leucodystrophy; pp. 134–146. J F-P, H B, editors. [Google Scholar]
- 20.Schutta HS, Pratt RT, Metz H, et al. A family study of the late infantile and juvenile forms of metachromatic leucodystrophy. J Med Genet. 1966;3(2):86–91. doi: 10.1136/jmg.3.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dalinka MK, Rosen RA, Kurth RJ, et al. Metachromatic leukodystrophy. A cause of cholelithiasis in childhood. Am J Dig Dis. 1969;14(8):603–606. doi: 10.1007/BF02232933. [DOI] [PubMed] [Google Scholar]
- 22.Stumpf D, Austin J. Metachromatic leukodystrophy (MLD). IX. Qualitative and quantitative differences in urinary arylsulfatase A in different forms of MLD. Arch Neurol. 1971;24(2):117–124. doi: 10.1001/archneur.1971.00480320045004. [DOI] [PubMed] [Google Scholar]
- 23.Duckett S, Cracco J, Graziani L, et al. Inclusions in the sural nerve in metachromatic leukodystrophy. Acta Neurol Latinoam. 1975;21(1–4):184–193. [PubMed] [Google Scholar]
- 24.Thomas PK, King RH, Kocen RS, Brett EM. Comparative ultrastructural observations on peripheral nerve abnormalities in the late infantile, juvenile and late onset forms of metachromatic leukodystrophy. Acta Neuropathol (Berl) 1977;39(3):237–245. doi: 10.1007/BF00691703. [DOI] [PubMed] [Google Scholar]
- 25.Buonanno FS, Ball MR, Laster DW, et al. Computed tomography in late-infantile metachromatic leukodystrophy. Ann Neurol. 1978;4(1):43–46. doi: 10.1002/ana.410040108. [DOI] [PubMed] [Google Scholar]
- 26.Libert J, Van Hoof F, Toussaint D, et al. Ocular findings in metachromatic leukodystrophy. An electron microscopic and enzyme study in different clinical and genetic variants. Arch Ophthalmol. 1979;97(8):1495–1504. doi: 10.1001/archopht.1979.01020020157015. [DOI] [PubMed] [Google Scholar]
- 27.Luijten JA, Staal GE, Willemse J. Metachromatic leukodystrophy and age: a comparative study of clinical, enzymological and ultrastructural findings. Clin Neurol Neurosurg. 1979;81(4):221–233. doi: 10.1016/0303-8467(79)90026-x. [DOI] [PubMed] [Google Scholar]
- 28.Harben AM, Krawiecki N, Marcus R, Hommes FA. A Km mutant of arylsulfatase A. Clin Chim Acta. 1982;125(3):351–354. doi: 10.1016/0009-8981(82)90266-2. [DOI] [PubMed] [Google Scholar]
- 29.Kihara H, Fluharty AL, Ng WG, Leider W. Presymptomatic diagnosis: metachromatic leukodystrophy or pseudo arylsulphatase A deficiency? J Inherit Metab Dis. 1982;5(4):215–217. doi: 10.1007/BF02179145. [DOI] [PubMed] [Google Scholar]
- 30.Martin JJ, Ceuterick C, Mercelis R, Joris C. Pathology of peripheral nerves in metachromatic leucodystrophy. A comparative study of ten cases. J Neurol Sci. 1982;53(1):95–112. doi: 10.1016/0022-510x(82)90084-3. [DOI] [PubMed] [Google Scholar]
- 31.Poduslo SE, Miller K, Jang Y. Biochemical studies of the late infantile form of metachromatic leukodystrophy. Acta Neuropathol (Berl) 1982;57(1):13–22. doi: 10.1007/BF00688873. [DOI] [PubMed] [Google Scholar]
- 32.Tonnesen T, Bro PV, Brondum Nielsen K, Lykkelund C. Metachromatic leukodystrophy and pseudoarylsulfatase A deficiency in a Danish family. Acta Paediatr Scand. 1983;72(2):175–178. doi: 10.1111/j.1651-2227.1983.tb09692.x. [DOI] [PubMed] [Google Scholar]
- 33.Burgess JH, Kalfayan B, Slungaard RK, Gilbert E. Papillomatosis of the gallbladder associated with metachromatic leukodystrophy. Arch Pathol Lab Med. 1985;109(1):79–81. [PubMed] [Google Scholar]
- 34.Krivit W, Shapiro E, Kennedy W, et al. Treatment of late infantile metachromatic leukodystrophy by bone marrow transplantation. N Engl J Med. 1990;322(1):28–32. doi: 10.1056/NEJM199001043220106. [DOI] [PubMed] [Google Scholar]
- 35.Harvey JS, Nelson PV, Carey WF, et al. An arylsulfatase A (ARSA) missense mutation (T274M) causing late-infantile metachromatic leukodystrophy. Hum Mutat. 1993;2(4):261–267. doi: 10.1002/humu.1380020405. [DOI] [PubMed] [Google Scholar]
- 36.Koul RL, Gururaj A, Chacko AP, et al. Late infantile metachromatic leucodystrophy in two siblings. Indian Pediatr. 1994;31(6):694–698. [PubMed] [Google Scholar]
- 37.Luyten JA, Wenink PW, Steenbergen-Spanjers GC, et al. Metachromatic leukodystrophy: a 12-bp deletion in exon 2 of the arylsulfatase A gene in a late infantile variant. Hum Genet. 1995;96(3):357–360. doi: 10.1007/BF00210424. [DOI] [PubMed] [Google Scholar]
- 38.Lissens W, Vervoort R, Van Regemorter N, et al. A D255H substitution in the arylsulphatase A gene of two unrelated Belgian patients with late-infantile metachromatic leukodystrophy. J Inherit Metab Dis. 1996;19(6):782–786. doi: 10.1007/BF01799173. [DOI] [PubMed] [Google Scholar]
- 39.Tsuda T, Hasegawa Y, Eto Y. Two novel mutations in a Japanese patient with the late-infantile form of metachromatic leukodystrophy. Brain Dev. 1996;18(5):400–403. doi: 10.1016/0387-7604(96)00041-1. [DOI] [PubMed] [Google Scholar]
- 40.Kim TS, Kim IO, Kim WS, et al. MR of childhood metachromatic leukodystrophy. AJNR Am J Neuroradiol. 1997;18(4):733–738. [PMC free article] [PubMed] [Google Scholar]
- 41.Regis S, Filocamo M, Stroppiano M, et al. A T > C transition causing a Leu > Pro substitution in a conserved region of the arylsulfatase A gene in a late infantile metachromatic leukodystrophy patient. Clin Genet. 1997;52(1):65–67. doi: 10.1111/j.1399-0004.1997.tb02518.x. [DOI] [PubMed] [Google Scholar]
- 42.Regis S, Filocamo M, Stroppiano M, et al. A 9-bp deletion (2320del9) on the background of the arylsulfatase A pseudodeficiency allele in a metachromatic leukodystrophy patient and in a patient with nonprogressive neurological symptoms. Hum Genet. 1998;102(1):50–53. doi: 10.1007/s004390050652. [DOI] [PubMed] [Google Scholar]
- 43.Berger J, Gmach M, Mayr U, et al. Coincidence of two novel arylsulfatase A alleles and mutation 459+1G>A within a family with metachromatic leukodystrophy: molecular basis of phenotypic heterogeneity. Hum Mutat. 1999;13(1):61–68. doi: 10.1002/(SICI)1098-1004(1999)13:1<61::AID-HUMU7>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 44.Hayashi M. Nine-year-old girl presenting familial occurrence of progressive developmental abnormalities with the white matter lesions. Neuropathology. 2002;22(4):350–352. doi: 10.1046/j.1440-1789.2002.00464.x. [DOI] [PubMed] [Google Scholar]
- 45.Eng B, Heshka T, Tarnopolsky MA, et al. Infantile metachromatic leukodystrophy (MLD) in a compound heterozygote for the c.459 + 1G > A mutation and a complete deletion of the ARSA gene. Am J Med Genet A. 2004;128(1):95–97. doi: 10.1002/ajmg.a.30085. [DOI] [PubMed] [Google Scholar]
- 46.Lugowska A, Szymanska K, Kmiec T, et al. Homozygote for mutation c.1204 + 1G > A of the ARSA gene presents with a late-infantile form of metachromatic leukodystrophy and a rare MRI white matter lesion type. J Appl Genet. 2005;46(3):337–339. [PubMed] [Google Scholar]
- 47.Toldo I, Carollo C, Battistella PA, Laverda AM. Spinal cord and cauda equina MRI findings in metachromatic leukodystrophy: case report. Neuroradiology. 2005;47(8):572–575. doi: 10.1007/s00234-005-1369-5. [DOI] [PubMed] [Google Scholar]
- 48.Regis S, Lualdi S, Biffi A, et al. Somatic intragenic recombination of the arylsulfatase A gene in a metachromatic leukodystrophy patient. Mol Genet Metab. 2006;89(1–2):150–155. doi: 10.1016/j.ymgme.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 49.Suzuki Y, Mizuno Y. Juvenile metachromatic leukodystrophy: deficiency of an arylsufatase A component. J Pediatr. 1974;85(6):823–825. doi: 10.1016/s0022-3476(74)80352-5. [DOI] [PubMed] [Google Scholar]
- 50.Jordan TW, Casey B, Weston HJ. Enzymic detection of metachromatic leukodystrophy patients and heterozygotes. N Z Med J. 1977;85(587):369–372. [PubMed] [Google Scholar]
- 51.Rattazzi MC, Davidson RG. Prenatal diagnosis of metachromatic leukodystrophy by electrophoretic and immunologic techniques. Pediatr Res. 1977;11(10 Pt 1):1072–1077. doi: 10.1203/00006450-197710000-00009. [DOI] [PubMed] [Google Scholar]
- 52.Rodriguez-Soriano J, Rivera JM, Vallo A, et al. Proximal renal tubular acidosis in metachromatic leukodystrophy. Helv Paediatr Acta. 1978;33(1):45–52. [PubMed] [Google Scholar]
- 53.Whitelaw AG, Brett EM. Metachromatic leukodystrophy and limb hypertrophy. Proc R Soc Med. 1975;68(5):301. doi: 10.1177/003591577506800516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baumann N, Turpin JC, Lefevre M, Colsch B. Motor and psycho-cognitive clinical types in adult metachromatic leukodystrophy: genotype/phenotype relationships? J Physiol Paris. 2002;96(3–4):301–306. doi: 10.1016/s0928-4257(02)00019-0. [DOI] [PubMed] [Google Scholar]
- 55.Arbour LT, Silver K, Hechtman P, et al. Variable onset of metachromatic leukodystrophy in a Vietnamese family. Pediatr Neurol. 2000;23(2):173–176. doi: 10.1016/s0887-8994(00)00164-8. [DOI] [PubMed] [Google Scholar]
- 56.Oguz KK, Anlar B, Senbil N, Cila A. Diffusion-weighted imaging findings in juvenile metachromatic leukodystrophy. Neuropediatrics. 2004;35(5):279–282. doi: 10.1055/s-2004-821301. [DOI] [PubMed] [Google Scholar]
- 57.Gordon N. The insidious presentation of the juvenile form of metachromatic leucodystrophy. Postgrad Med J. 1978;54(631):335–337. doi: 10.1136/pgmj.54.631.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.MacFaul R, Cavanagh N, Lake BD, Stephens R, Whitfield AE. Metachromatic leucodystrophy: review of 38 cases. Arch Dis Child. 1982;57(3):168–175. doi: 10.1136/adc.57.3.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carlin L, Roach ES, Riela A, Spudis E, McLean WT., Jr Juvenile metachromatic leukodystrophy: evoked potentials and computed tomography. Ann Neurol. 1983;13(1):105–106. doi: 10.1002/ana.410130124. [DOI] [PubMed] [Google Scholar]
- 60.Clark JR, Miller RG, Vidgoff JM. Juvenile-onset metachromatic leukodystrophy: biochemical and electrophysiologic studies. Neurology. 1979;29(3):346–353. doi: 10.1212/wnl.29.3.346. [DOI] [PubMed] [Google Scholar]
- 61.Clarke JT, Skomorowski MA, Chang PL. Marked clinical difference between two sibs affected with juvenile metachromatic leukodystrophy. Am J Med Genet. 1989;33(1):10–13. doi: 10.1002/ajmg.1320330104. [DOI] [PubMed] [Google Scholar]
- 62.Guffon N, Souillet G, Maire I, et al. Juvenile metachromatic leukodystrophy: neurological outcome two years after bone marrow transplantation. J Inherit Metab Dis. 1995;18(2):159–161. doi: 10.1007/BF00711755. [DOI] [PubMed] [Google Scholar]
- 63.Haberland C, Brunngraber E, Witting L, Daniels A. Juvenile metachromatic leucodystrophy. Case report with clinical, histopathological, ultrastructural and biochemical observations. Acta Neuropathol (Berl) 1973;26(2):93–106. doi: 10.1007/BF00697745. [DOI] [PubMed] [Google Scholar]
- 64.Haltia T, Palo J, Haltia M, Icen A. Juvenile metachromatic leukodystrophy. Clinical, biochemical, and neuropathologic studies in nine new cases. Arch Neurol. 1980;37(1):42–46. doi: 10.1001/archneur.1980.00500500072011. [DOI] [PubMed] [Google Scholar]
- 65.Kapaun P, Dittmann RW, Granitzny B, et al. Slow progression of juvenile metachromatic leukodystrophy 6 years after bone marrow transplantation. J Child Neurol. 1999;14(4):222–228. doi: 10.1177/088307389901400402. [DOI] [PubMed] [Google Scholar]
- 66.Kidd D, Nelson J, Jones F, et al. Long-term stabilization after bone marrow transplantation in juvenile metachromatic leukodystrophy. Arch Neurol. 1998;55(1):98–99. doi: 10.1001/archneur.55.1.98. [DOI] [PubMed] [Google Scholar]
- 67.Lyon G, Arthuis M, Thieffry S. [Familial infantile metachromatic leukodystrophy. Study of 2 cases, including one with anatomical and chemical examination.] Rev Neurol (Paris) 1961;104:508–532. [PubMed] [Google Scholar]
- 68.Mizuno Y, Nakamura Y, Sugaya A, Komiya K. A case of juvenile metachromatic leukodystrophy--the third case in Japan. Brain Dev. 1988;10(1):50–53. doi: 10.1016/s0387-7604(88)80047-0. [DOI] [PubMed] [Google Scholar]
- 69.Navarro C, Fernandez JM, Dominguez C, et al. Late juvenile metachromatic leukodystrophy treated with bone marrow transplantation; a 4-year follow-up study. Neurology. 1996;46(1):254–256. doi: 10.1212/wnl.46.1.254. [DOI] [PubMed] [Google Scholar]
- 70.Recke AS, Harzer K, Recke SH. [Observations on the course of juvenile metachromatic leukodystrophy] Nervenarzt. 1976;47(2):103–107. [PubMed] [Google Scholar]
- 71.Reider-Grosswasser I, Bornstein N. CT and MRI in late-onset metachromatic leukodystrophy. Acta Neurol Scand. 1987;75(1):64–69. doi: 10.1111/j.1600-0404.1987.tb07891.x. [DOI] [PubMed] [Google Scholar]
- 72.Satoh T, Suzuki H, Monma N, et al. Metachromatic leukodystrophy. Report of siblings with the juvenile type of metachromatic leukodystrophy. Acta Pathol Jpn. 1988;38(8):1041–1051. doi: 10.1111/j.1440-1827.1988.tb02376.x. [DOI] [PubMed] [Google Scholar]
- 73.Scholz W. Klinische, pathologisch-anatomische und erbbiologische Untersuchungen bei familiarer, diffuser Hirnsklerose im Kindesalter. Zeitschrift fur die gesammelte Neurologie Psychiatrie. 1925:651–717. [Google Scholar]
- 74.Schranz D, Dieterich E, Gehler J. [Early symptoms and diagnosis of metachromatic leukodystrophy in childhood] Monatsschr Kinderheilkd. 1980;128(5):387–388. [PubMed] [Google Scholar]
- 75.Warner JO. Juvenile onset metachromatic leucodystrophy. Failure of response on a low vitamin A diet. Arch Dis Child. 1975;50(9):735–737. doi: 10.1136/adc.50.9.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Arbour LT, Silver K, Hechtman P, et al. Variable onset of metachromatic leukodystrophy in a Vietnamese family. Pediatr Neurol. 2000;23(2):173–176. doi: 10.1016/s0887-8994(00)00164-8. [DOI] [PubMed] [Google Scholar]
- 77.Schipper HI, Seidel D. Computed tomography in late-onset metachromatic leucodystrophy. Neuroradiology. 1984;26(1):39–44. doi: 10.1007/BF00328202. [DOI] [PubMed] [Google Scholar]
- 78.Sourander P, Svennerholm L. Sulphatide lipidosis in the adult with the clinical picture of progressive organic dementia with epileptic seizures. Acta Neuropathologica. 1962;1(4):384–396. [Google Scholar]
- 79.Anlar B, Waye JS, Eng B, Oguz KK. Atypical clinical course in juvenile metachromatic leukodystrophy involving novel arylsulfatase A gene mutations. Dev Med Child Neurol. 2006;48(5):383–387. doi: 10.1017/S001216220600082X. [DOI] [PubMed] [Google Scholar]
- 80.Fluharty AL, Fluharty CB, Bohne W, et al. Two new arylsulfatase A (ARSA) mutations in a juvenile metachromatic leukodystrophy (MLD) patient. Am J Hum Genet. 1991;49(6):1340–1350. [PMC free article] [PubMed] [Google Scholar]
- 81.Gomez-Lira M, Perusi C, Mottes M, et al. Molecular genetic characterization of two metachromatic leukodystrophy patients who carry the T799G mutation and show different phenotypes; description of a novel null-type mutation. Hum Genet. 1998;102(4):459–463. doi: 10.1007/s004390050721. [DOI] [PubMed] [Google Scholar]
- 82.Rauschka H, Colsch B, Baumann N, et al. Late-onset metachromatic leukodystrophy: genotype strongly influences phenotype. Neurology. 2006;67(5):859–863. doi: 10.1212/01.wnl.0000234129.97727.4d. [DOI] [PubMed] [Google Scholar]
- 83.Takahashi J, Takahashi S, Utsugizawa K, et al. [Two siblings with metachromatic leukodystrophy of adult and juvenile onset] Rinsho Shinkeigaku. 1993;33(3):312–316. [PubMed] [Google Scholar]
- 84.Quigley HA, Green WR. Clinical and ultrastructural ocular histopathologic studies of adult-onset metachromatic leukodystrophy. Am J Ophthalmol. 1976;82(3):472–479. doi: 10.1016/0002-9394(76)90497-9. [DOI] [PubMed] [Google Scholar]
- 85.Beratis NG, Aaron AM, Hirschhorn K. Metachromatic leukodystrophy: detection in serum. J Pediatr. 1973;83(5):824–827. doi: 10.1016/s0022-3476(73)80377-4. [DOI] [PubMed] [Google Scholar]
- 86.Hirose G, Bass NH. Metachromatic leukodystrophy in the adult. A biochemical study. Neurology. 1972;22(3):312–320. doi: 10.1212/wnl.22.3.312. [DOI] [PubMed] [Google Scholar]
- 87.Percy AK, Kaback MM, Herndon RM. Metachromatic leukodystrophy: comparison of early-and late-onset forms. Neurology. 1977;27(10):933–941. doi: 10.1212/wnl.27.10.933. [DOI] [PubMed] [Google Scholar]
- 88.Tagliavini F, Pietrini V, Pilleri G, et al. Adult metachromatic leucodystrophy: clinicopathological report of two familial cases with slow course. Neuropathol Appl Neurobiol. 1979;5(3):233–243. doi: 10.1111/j.1365-2990.1979.tb00622.x. [DOI] [PubMed] [Google Scholar]
- 89.Sadeh M, Kuritzky A, Ben-David E, Goldhammer Y. Adult metachromatic leukodystrophy with an unusual relapsing-remitting course. Postgrad Med J. 1992;68(797):192–195. doi: 10.1136/pgmj.68.797.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Felice KJ, Gomez Lira M, Natowicz M, et al. Adult-onset MLD: a gene mutation with isolated polyneuropathy. Neurology. 2000;55(7):1036–1039. doi: 10.1212/wnl.55.7.1036. [DOI] [PubMed] [Google Scholar]
- 91.Cerizza M, Nemni R, Tamma F. Adult metachromatic leucodystrophy: an underdiagnosed disease? J Neurol Neurosurg Psychiatry. 1987;50(12):1710–1712. doi: 10.1136/jnnp.50.12.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bostantjopoulou S, Katsarou Z, Michelakaki H, Kazis A. Seizures as a presenting feature of late onset metachromatic leukodystrophy. Acta Neurol Scand. 2000;102(3):192–195. doi: 10.1034/j.1600-0404.2000.102003192.x. [DOI] [PubMed] [Google Scholar]
- 93.Cengiz N, Ozbenli T, Onar M, et al. Adult metachromatic leukodystrophy: three cases with normal nerve conduction velocities in a family. Acta Neurol Scand. 2002;105(6):454–457. doi: 10.1034/j.1600-0404.2002.01257.x. [DOI] [PubMed] [Google Scholar]
- 94.Betts TA, Smith WT, Kelly RE. Adult metachromatic leukodystrophy (sulphatide lipidosis) simulating acute schizophrenia. Report of a case. Neurology. 1968;18(11):1140–1142. doi: 10.1212/wnl.18.11.1140. [DOI] [PubMed] [Google Scholar]
- 95.Bosch EP, Hart MN. Late adult-onset metachromatic leukodystrophy. Dementia and polyneuropathy in a 63-year-old man. Arch Neurol. 1978;35(7):475–477. doi: 10.1001/archneur.1978.00500310077017. [DOI] [PubMed] [Google Scholar]
- 96.Brault JL, Gielselmann V, Carpentier A, et al. [2 familial cases of metachromatic leukodystrophy of late onset] Rev Neurol (Paris) 1997;153(3):193–196. [PubMed] [Google Scholar]
- 97.Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 7-1984. A 34-year old man with progressive quadriparesis and mental deterioration. N Engl J Med. 1984;310(7):445–455. doi: 10.1056/NEJM198402163100708. [DOI] [PubMed] [Google Scholar]
- 98.Czmok E, Regli F, Bischoff A, et al. [Clinical and histological diagnosis of a case of familial adult metachromatic leucodystrophy (author's transl)] J Neurol. 1974;207(3):189–204. doi: 10.1007/BF00312560. [DOI] [PubMed] [Google Scholar]
- 99.Comabella M, Waye JS, Raguer N, et al. Late-onset metachromatic leukodystrophy clinically presenting as isolated peripheral neuropathy: compound heterozygosity for the IVS2+1G > A mutation and a newly identified missense mutation (Thr408Ile) in a Spanish family. Ann Neurol. 2001;50(1):108–112. [PubMed] [Google Scholar]
- 100.De Mulder C, Martin JJ. [Adult metachromatic leucodystrophy (author's transl)] Acta Neurol Belg. 1978;78(3):162–166. [PubMed] [Google Scholar]
- 101.Ettinger A. Adults Form of Leucodystrophy of Type Scholz-Bielschowsky-Henneberg, with Metachromatic Breakdown Products, in a 55-year Old Male. Psychiat. Neurol. (Basel) 1965;149:225–239. [Google Scholar]
- 102.Finelli PF. Metachromatic leukodystrophy manifesting as a schizophrenic disorder: computed tomographic correlation. Ann Neurol. 1985;18(1):94–95. doi: 10.1002/ana.410180117. [DOI] [PubMed] [Google Scholar]
- 103.Fressinaud C, Vallat JM, Masson M, et al. Adult-onset metachromatic leukodystrophy presenting as isolated peripheral neuropathy. Neurology. 1992;42(7):1396–1398. doi: 10.1212/wnl.42.7.1396. [DOI] [PubMed] [Google Scholar]
- 104.Fukutani Y, Noriki Y, Sasaki K, et al. Adult-type metachromatic leukodystrophy with a compound heterozygote mutation showing character change and dementia. Psychiatry Clin Neurosci. 1999;53(3):425–428. doi: 10.1046/j.1440-1819.1999.00569.x. [DOI] [PubMed] [Google Scholar]
- 105.Gallo S, Randi D, Bertelli M. et al. Late onset MLD with normal nerve conduction associated with two novel missense mutations in the ASA gene. J Neurol Neurosurg Psychiatry. 2004;75(4):655–657. doi: 10.1136/jnnp.2003.017400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Guseo A, Deak G, Szirmai I. An adult case of metachromatic leukodystrophy. Light, polarization and electron microscopic study. Acta Neuropathol (Berl) 1975;32(4):333–339. doi: 10.1007/BF00696795. [DOI] [PubMed] [Google Scholar]
- 107.Duyff RF, Weinstein HC. Late-presenting metachromatic leukodystrophy. Lancet. 1996;348(9038):1382–1383. doi: 10.1016/S0140-6736(05)65446-3. [DOI] [PubMed] [Google Scholar]
- 108.Haag C, Laakmann G, Voderholzer U, et al. [Adult form of metachromatic leukodystrophy with predominantly psychotic manifestations] Nervenarzt. 1992;63(7):444–446. [PubMed] [Google Scholar]
- 109.Hollander H, Pilz H. [on Metachromatic Leukodystrophy. I. Case Report.] Arch Psychiatr Nervenkr. 1964;205:293–299. doi: 10.1007/BF00395716. [DOI] [PubMed] [Google Scholar]
- 110.Johannsen P, Ehlers L, Hansen HJ. Dementia with impaired temporal glucose metabolism in late-onset metachromatic leukodystrophy. Dement Geriatr Cogn Disord. 2001;12(2):85–88. doi: 10.1159/000051240. [DOI] [PubMed] [Google Scholar]
- 111.Kappler J, von Figura K, Gieselmann V. Late-onset metachromatic leukodystrophy: molecular pathology in two siblings. Ann Neurol. 1992;31(3):256–261. doi: 10.1002/ana.410310305. [DOI] [PubMed] [Google Scholar]
- 112.Klemm E, Conzelmann E. Adult-onset metachromatic leucodystrophy presenting without psychiatric symptoms. J Neurol. 1989;236(7):427–429. doi: 10.1007/BF00314905. [DOI] [PubMed] [Google Scholar]
- 113.Kondo R, Wakamatsu N, Yoshino H, et al. Identification of a mutation in the arylsulfatase A gene of a patient with adult-type metachromatic leukodystrophy. Am J Hum Genet. 1991;48(5):971–978. [PMC free article] [PubMed] [Google Scholar]
- 114.Kumperscak HG, Paschke E, Gradisnik P, et al. Adult metachromatic leukodystrophy: disorganized schizophrenia-like symptoms and postpartum depression in 2 sisters. J Psychiatry Neurosci. 2005;30(1):33–36. [PMC free article] [PubMed] [Google Scholar]
- 115.Manowitz P, Kling A, Kohn H. Clinical course of adult metachromatic leukodystrophy presenting as schizophrenia. A report of two living cases in siblings. J Nerv Ment Dis. 1978;166(7):500–506. doi: 10.1097/00005053-197807000-00005. [DOI] [PubMed] [Google Scholar]
- 116.Marcao AM, Wiest R, Schindler K, et al. Adult onset metachromatic leukodystrophy without electroclinical peripheral nervous system involvement: a new mutation in the ARSA gene. Arch Neurol. 2005;62(2):309–313. doi: 10.1001/archneur.62.2.309. [DOI] [PubMed] [Google Scholar]
- 117.Muller D, Pilz H, ter Meulen V. Studies on adult metachromatic leukodystrophy. 1. Clinical, morphological and histochemical observations in two cases. J Neurol Sci. 1969;9(3):567–584. doi: 10.1016/0022-510x(69)90095-1. [DOI] [PubMed] [Google Scholar]
- 118.Pilz H, Duensing I, Heipertz R, et al. Adult metachromatic leukodystrophy. I. Clinical manifestation in a female aged 44 years, previously diagnosed in the preclinical state. Eur Neurol. 1977;15(6):301–307. doi: 10.1159/000114818. [DOI] [PubMed] [Google Scholar]
- 119.Pilz H, Muller D. Studies on adult metachromatic leukodystrophy. 2. Biochemical aspects of adult cases of metachromatic leukodystrophy. J Neurol Sci. 1969;9(3):585–595. doi: 10.1016/0022-510x(69)90096-3. [DOI] [PubMed] [Google Scholar]
- 120.Kothbauer P, Jellinger K, Gross H, et al. [Adult metachromatic leukodystrophy manifested as schizophrenic psychosis (author's transl)] Arch Psychiatr Nervenkr. 1977;224(4):379–387. doi: 10.1007/BF00341619. [DOI] [PubMed] [Google Scholar]
- 121.Sadovnick AD, Tuokko H, Applegarth DA, et al. The differential diagnosis of adult onset metachromatic leukodystrophy and early onset familial Alzheimer disease in an Alzheimer clinic population. Can J Neurol Sci. 1993;20(4):312–318. doi: 10.1017/s031716710004823x. [DOI] [PubMed] [Google Scholar]
- 122.Schaffer S, Oepen G, Ott D. [The adult form of metachromatic leukodystrophy with a predominantly psychotic manifestation] Nervenarzt. 1988;59(12):731–733. [PubMed] [Google Scholar]
- 123.Seidel D, Goebel HH, Scholz W. Late-onset metachromatic leukodystrophy: diagnostic problems elucidated by a case report. J Neurol. 1981;226(2):119–124. doi: 10.1007/BF00313439. [DOI] [PubMed] [Google Scholar]
- 124.Seidel D, Heipertz R, Goebel HH, et al. Adult metachromatic leukodystrophy. III. Clinical course, final stages and first biochemical results. Eur Neurol. 1980;19(5):288–293. doi: 10.1159/000115164. [DOI] [PubMed] [Google Scholar]
- 125.Perez Sempere A, Martinez Menendez B, Villaverde Amundarain FJ, et al. [Metachromatic leukodystrophy: an exceptional cause of dementia in the adult] Neurologia. 1992;7(5):114–116. [PubMed] [Google Scholar]
- 126.Skomer C, Stears J, Austin J. Metachromatic leukodystrophy (MLD). XV. Adult MLD with focal lesions by computed tomography. Arch Neurol. 1983;40(6):354–355. doi: 10.1001/archneur.1983.04050060054009. [DOI] [PubMed] [Google Scholar]
- 127.Goebel HH, Shimokawa K, Argyrakis A, Pilz H. The ultrastructure of the retina in adult metachromatic leukodystrophy. Am J Ophthalmol. 1978;85(6):841–849. doi: 10.1016/s0002-9394(14)78115-2. [DOI] [PubMed] [Google Scholar]
- 128.Waltz G, Harik SI, Kaufman B. Adult metachromatic leukodystrophy. Value of computed tomographic scanning and magnetic resonance imaging of the brain. Arch Neurol. 1987;44(2):225–227. doi: 10.1001/archneur.1987.00520140083022. [DOI] [PubMed] [Google Scholar]
- 129.Wang LN, Huang KW, Wang DG, Liu ZY. Adult metachromatic leukodystrophy without deficiency of arylsulphatase. Chin Med J (Engl) 1990;103(10):846–850. [PubMed] [Google Scholar]
- 130.Wildbolz A. [Clinical and genealogical report on a new family with three cases of adult metachromatic leukodystrophy] Schweiz Arch Neurol Neurochir Psychiatr. 1971;109(2):313–321. [PubMed] [Google Scholar]
- 131.Wulff CH, Trojaborg W. Adult metachromatic leukodystrophy: neurophysiologic findings. Neurology. 1985;35(12):1776–1778. doi: 10.1212/wnl.35.12.1776. [DOI] [PubMed] [Google Scholar]
- 132.Zhao JX. [Later onset metachromatic leukodystrophy diagnosed by nerve biopsy] Zhonghua Shen Jing Jing Shen Ke Za Zhi. 1992;25(5):271–272. 316. [PubMed] [Google Scholar]
- 133.Wright GD, Patel MK, Mikel J. An adult onset metachromatic leukodystrophy with dominant inheritance and normal arylsulphatase A levels. J Neurol Sci. 1988;87(2–3):153–166. doi: 10.1016/0022-510x(88)90241-9. [DOI] [PubMed] [Google Scholar]
- 134.Kraus-Ruppert R, Wildbolz A, Matthieu JM, Herschkowitz N. The late form of metachromatic leukodystrophy. I. A histochemical and neurochemical study. J Neurol Sci. 1972;17(4):373–381. doi: 10.1016/0022-510x(72)90149-9. [DOI] [PubMed] [Google Scholar]
- 135.Hoes MJ, Lamers KJ, Hommes OR, ter Haar B. Adult metachromatic leukodystrophy. Arylsulphatase-A values in four generations of one family and some reflections about the genetics. Clin Neurol Neurosurg. 1978;80(3):174–188. doi: 10.1016/s0303-8467(78)80039-0. [DOI] [PubMed] [Google Scholar]
- 136.Cole G, Proctor NS. Adult metachromatic leucodystrophy. S Afr Med J. 1974;48(32):1371–1374. [PubMed] [Google Scholar]
- 137.Roizin L, Scheinesson G, Eros G. Comparative histological and histochemical studies of infantile and adult metachromatic leucodystrophy. Pathol Eur. 1968;3(2):286–293. [PubMed] [Google Scholar]
- 138.Kaltenbach H. Uber einen eigenartigen Markprocess mit metachromatischen Abbauprodukten bei einem paralyseahnlechen Krankheitsbild. Z. Ges. Neurol. Psychiatr. 1922;75 [Google Scholar]
- 139.Helmstaedt ER. [On a case of metachromatic leukodystrophy. A contribution to the development of teaching on leukodystrophy.] Dtsch Z Nervenheilkd. 1963;184:213–234. [PubMed] [Google Scholar]
- 140.Stam F. New histochemical and colloidchemical aspects of leucodystrophy. Psychiat. Neurol. Neurochir. 1960;63:237–245. [Google Scholar]
- 141.Alves D, Pires MM, Guimaraes A, Miranda MC. Four cases of late onset metachromatic leucodystrophy in a family: clinical, biochemical and neuropathological studies. J Neurol Neurosurg Psychiatry. 1986;49(12):1417–1422. doi: 10.1136/jnnp.49.12.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Austin J, Armstrong D, Fouch S, et al. Metachromatic leukodystrophy (MLD). 8. MLD in adults; diagnosis and pathogenesis. Arch Neurol. 1968;18(3):225–240. doi: 10.1001/archneur.1968.00470330015001. [DOI] [PubMed] [Google Scholar]
- 143.Baquis GD, Kelly JJ, Jr, Lieberman A, Wolpert SM. Adult metachromatic leukodystrophy and pes cavus foot deformity. Muscle Nerve. 1991;14(8):784–785. [PubMed] [Google Scholar]
- 144.Besson JA. A diagnostic pointer to adult metachromatic leucodystrophy. Br J Psychiatry. 1980;137:186–187. doi: 10.1192/bjp.137.2.186. [DOI] [PubMed] [Google Scholar]
- 145.Görg M, Wilck W, Granitzny B, et al. Stabilization of juvenile metachromatic leukodystrophy after bone marrow transplantation: a 13-year follow-up. J Child Neurol. 2007;22(9):1139–1142. doi: 10.1177/0883073807306256. [DOI] [PubMed] [Google Scholar]
- 146.Sevin C, Aubourg P, Cartier N. Enzyme, cell and gene-based therapies for metachromatic leukodystrophy. J Inherit Metab Dis. 2007;30(2):175–183. doi: 10.1007/s10545-007-0540-z. [DOI] [PubMed] [Google Scholar]
- 147.Matzner U, Gieselmann V. Gene therapy of metachromatic leukodystrophy. Expert Opin Biol Ther. 2005;5(1):55–65. doi: 10.1517/14712598.5.1.55. [DOI] [PubMed] [Google Scholar]