Abstract
Objectives
This study aimed to check the status of the contact investigation in congregate settings to eradicate tuberculosis (TB) in the Republic of Korea.
Methods
The “Integrated System for Disease and Public Health Management” is used for care and follow-up for patients and contacts of TB. We downloaded data for contact investigations conducted from January to December 2013.
Results
A total of 1,200 contact investigations in congregate settings were carried out by 25 field investigators in 2013. We performed the status of contact investigation, TB, and LTBI rate by age, accept rate of LTBI treatment, and complete rate of LTBI treatment during 2013. A total of 1,547 index TB patients, 149,166 contacts, and 259 additional TB patients were found through the investigation. Kindergartens showed the highest LTBI rate, 19.8%, among educational facilities. The second highest was in elementary schools and the subtotal LTBI rate of educational facilities was 7.8%. Social welfare/correctional facilities and workplaces showed relatively high LTBI rates of 23.8% and 23.6%, respectively. By age, individuals >35 years showed the highest LTBI rate, followed by those aged 0–4 years, 30–34 years, and 5–9 years, with rates of 18.1%, 16.4%, and 15.4% respectively. When comparing the tuberculin skin test (TST) positive conversion ratio by facility, middle school and high school were relatively high compared to the others. The accept rate of LTBI treatment in the workplace was lowest at 63% and the complete rate in elementary schools was lowest at 76.5%.
Conclusion
TB contact investigation is considered as a meaningful strategy for preventing TB outbreaks in congregate settings and decreasing the prevalence of TB in young people. Results of this study could be used to establish the LTBI management policy.
Keywords: interferon-gamma release tests, latent tuberculosis, tuberculin test, tuberculosis
1. Introduction
1.1. Background
Tuberculosis (TB) remains a serious infectious disease worldwide. The Republic of Korea (ROK) has achieved great progress economically and has managed some infectious diseases, like measles, to the elimination level; however, in the case of TB in the ROK, the incidence and mortality have been highest among the Organization for Economic Cooperation and Development (OECD) countries [1].
In the ROK, many management policies and programs have been promoted to reduce the incidence of TB and eliminate it in the future. The first component for TB control is case detection and management, including activities from diagnosis of TB cases to completion of treatment, as a directly observed treatment and cost support. The second component is contact investigation and outbreak control in households and congregate settings like schools, military units, correctional facilities, and workplaces. Also, testing and treatment of latent TB infection (LTBI) is an important program. To decrease the incidence of TB effectively, not only early detection and treatment of TB patients, but also the management of LTBI, has been known to be implemented [2]. In addition, many activities have strengthened in the field of education and public relations for the prevention of TB and research. These activities have pushed forward and become enhanced since 2011. In 2013, the total number of TB cases decreased by about 4,000 and the number of new TB patients decreased by about 3,500 compared to 2012 as an effect of these programs, efforts, and resources assignment. However, the incidence is still high in 2013 and the incidence of TB patients and new TB patients was 89.6/100,000 population and 71.4/100,000 population, respectively [3].
The TB and LTBI diagnosis and treatment program when the case occurred in congregate settings contributed significantly to the reduction of the incidence in 2013. In particular, expanding contacts to be investigated in a group facility and ensuring expertise of contact investigation by the arrangement of 25 field investigators across the country were essential factors in reducing the number of patients. The total number of contact investigations in congregate settings, performed in 2013, was 1,200.
1.2. Process of TB contact investigation in congregate settings
In the ROK, TB patients are reported through the Korea National Tuberculosis Surveillance and it is checked whether the patient belongs to congregate settings. Congregate settings refer to school, military facilities, correctional facilities, the office or workplace, social welfare facilities, and so on. In patients aged <25 years, even when affiliation information of the report is not collected, extra work collecting the occupation or status information is needed through interviews with the patient, because the patient is very likely to be a military personnel or a student. If the case is confirmed to belong to some congregate settings, the patient is registered as the index case and contact investigators check the presence or absence of infectiousness of the index case and how many TB cases occurred in the same site within the past 6 months. If the index case has infectiousness (sputum acid fast bacilli (AFB) smear positive or culture positive) or more than two patients with extrapulmonary TB occur in the same facility, contact investigation is determined to be implemented (Figure 1). Contacts are persons in the same place as the index patient during the infectious period.
Figure 1.
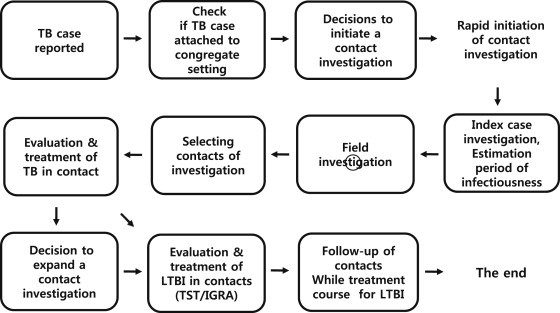
Process of tuberculosis (TB) contact investigation in congregate settings. IGRA = interferon-gamma release assay; LTBI = latent TB infection; TST = tuberculin skin test.
Contact investigation should be initiated rapidly. Within 1 week, much information is collected from the patient, physician, and nurse about whether the patient has multidrug resistant TB or not, whether several examinations required for diagnosis of TB are missing or not, and the treatment status of the patient.
We determine the infectious period on the basis of the information from the index case about TB symptoms, the presence of lung cavities, and sputum AFB smear results [4]. Generally, the period of infection is estimated to be 3 months; contacts within this period are included in the subjects of investigation. The field investigation should be performed within 3 days of the index patient investigation.
A field investigation is carried out by contact investigators. They visit the facility or institution where the index case stayed during infection and check whether TB occurred in other patients or not; they also check spatial structure and environmental characteristics like ventilation and lighting. By reflecting the period of infectiousness and the result of field investigation, a selection of contacts to be investigated is carried out and the list of contacts is offered.
First, contacts receive chest radiograph examinations. If a new TB patient is detected among the contacts, contact investigators decide whether to expand the range of the contacts to be screened. After the TB screening has finished, an LTBI test is performed in the contacts, except patients. The two methods used in the LTBI test are the tuberculin skin test (TST) and the interferon-gamma release assay (IGRA; Figure 2). Contacts who are diagnosed with LTBI are recommended to be treated through consent procedures. In order to monitor the occurrence of new patients among contacts while on a treatment course for LTBI, chest radiograph examination is performed after 3 months and 9 months. The treatment of LTBI is based on the prescription of the doctor and the regimens are isoniazid for 9 months, rifampin for 4 months and both for 3 months. Side effects of the antituberculosis treatment are monitored during the treatment period.
Figure 2.
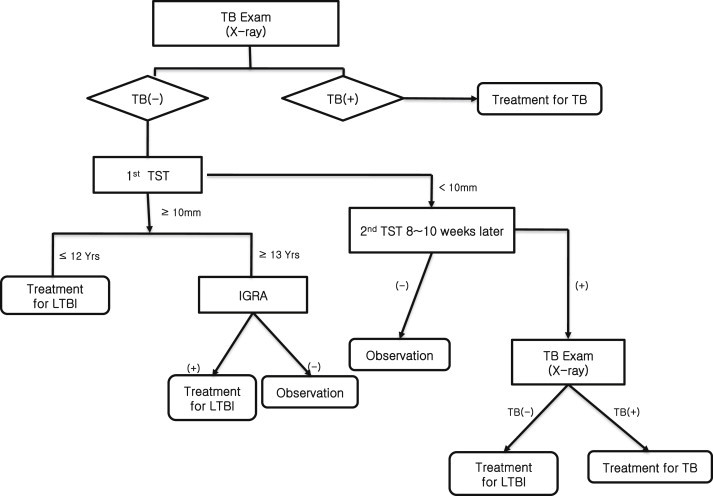
Process of latent tuberculosis infection (LTBI) diagnosis. IGRA = interferon-gamma release assay; TST = tuberculin skin test.
The LTBI diagnosis process of contact investigation differs slightly depending on the age of contacts (Figure 2). Children aged ≤12 years who have an induration of ≥10 mm on primary TST testing are diagnosed with LTBI. However, in children ≥13 years of age, contacts who have an induration of ≥10 mm on primary TST testing receive a further test – IGRA. If positive, they are diagnosed with LTBI and given treatment. In children aged <5 years, excluding newborns aged <4 weeks, even if the induration size is <10 mm on primary TST testing, treatment of LTBI is recommended in a preventive manner until secondary TST time. If there is no positive conversion on the secondary TST test, preventive treatment is stopped, and if there is a positive conversion, treatment of LTBI is maintained.
In this study, we describe the results of the contact investigation in congregate settings in 2013, discuss the results, and suggest future directions of the investigation.
2. Materials and methods
In the ROK, processes and results of contact investigation in congregate settings are managed with the “Integrated System for Disease and Public Health Management” for care and follow-up for patients and contacts. Demographic, epidemiologic, TB historic, and medical information of index patients, new patients, and patients' associated contacts have been registered in the system since 2013.
For this study, we downloaded data from the system on February 28, 2014, from contact investigations conducted from January 2013 to December 2013. We then carried out analysis on the number of patients, contact investigations and contacts by congregate settings, the LTBI rate by age and congregate settings, and the consent rate of treatment on LTBI and completion rate.
3. Results
A total of 1200 contact investigations were performed in congregate settings in 2013. Most contact investigations, 769, were conducted in educational facilities such as daycare centers/kindergartens and elementary, middle, and high schools, etc. Among these, 300 investigations were conducted in high school. A total of 201 investigations were conducted in social welfare facilities and correctional facilities, 127 investigations were conducted in military or police units, and 46 investigations were conducted in workplaces.
The total number of contacts associated with 1547 index patients was 149,166, and >50% of contacts, 79,369 in high schools were examined. New patients detected through contact investigation totaled 259, and the mean rate of detecting new patients was 0.2, and ranged from 0.0 to 0.5 by congregate settings (Table 1).
Table 1.
Results of contact investigations by congregate settings.
| Congregate settings | Facilities (n) | Index patients (n) | Contacts (n) | New patients detected, n (%) | LTBI, n (%) | |
|---|---|---|---|---|---|---|
| Education facilities | Daycare center/kindergarten | 49 | 50 | 1,993 | 0 (0.0) | 394 (19.8) |
| Elementary school | 33 | 33 | 1,628 | 1 (0.1) | 215 (13.2) | |
| Middle school | 93 | 103 | 12,637 | 4 (0.0) | 910 (7.2) | |
| High school | 300 | 419 | 79,369 | 105 (0.1) | 6,055 (7.6) | |
| University | 290 | 377 | 29,384 | 82 (0.3) | 2,121 (7.2) | |
| Other schools | 10 | 11 | 803 | 2 (0.2) | 82 (10.2) | |
| Subtotal | 769 | 993 | 125,814 | 194 (0.2) | 9,777 (7.8) | |
| Military or police unit | 127 | 145 | 9,335 | 30 (0.3) | 1,085 (11.6) | |
| Social welfare facilities/correctional facilities | 201 | 292 | 10,522 | 26 (0.2) | 2,499 (23.8) | |
| Workplaces | 46 | 60 | 1,552 | 7 (0.5) | 366 (23.6) | |
| Others | 51 | 57 | 1,943 | 2 (0.1) | 559 (28.8) | |
| Total | 1,200 | 1,547 | 149,166 | 259 (0.2) | 14,286 (9.6) | |
For educational facilities, not only students, but also teachers and staff were included in contact investigations. The LTBI rate in daycare centers/kindergartens was 19.8%, which was the highest. In high school, 105 new patients were detected and the total of LTBI during investigation was 6055. These figures were most among education facilities, but the rate of LTBI was 7.6%, which was similar to the LTBI rate of the entire education facilities (7.8%).
Looking at the LTBI rate by age, it was the highest (26.2%) at ≥35 years of age. LTBI rates at 0–4 years of age, 30–34 years of age, and 5–9 years of age were 18.1%, 16.4%, and 15.4%, respectively (Table 2). In adolescents aged 15–19 years of age, 4849 were diagnosed with LTBI, which was the highest number, but the LTBI rate was lower at 5.7%.
Table 2.
Latent tuberculosis infection (LTBI) by age.
| Age (y) | No. of LTBI (%) | LTBI rate |
|---|---|---|
| 0∼4 | 197 (1.4) | 18.1 |
| 5∼9 | 175 (1.2) | 15.4 |
| 10∼14 | 547 (3.8) | 6.5 |
| 15∼19 | 4,849 (33.9) | 5.7 |
| 20∼24 | 1,892 (13.2) | 7.7 |
| 25∼29 | 562 (3.9) | 8.6 |
| 30∼34 | 581 (4.1) | 16.4 |
| ≥35 | 5,483 (38.4) | 26.2 |
| Total | 14,286 (100) | 9.6 |
By congregate settings, the proportion of LTBI people who have been diagnosed with TST positive conversion was higher in middle and high school (Figure 3).
Figure 3.
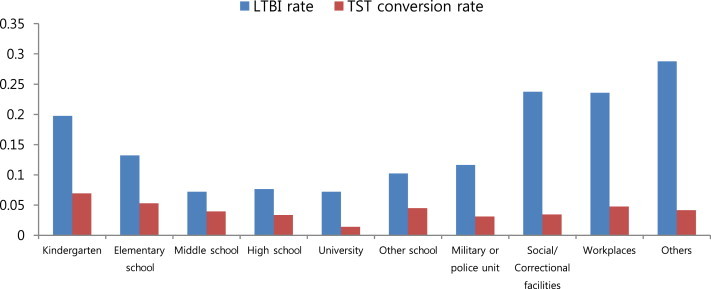
Latent tuberculosis infection rate (LTBI) and tuberculin skin test (TST) conversion rate by congregate setting.
By age, the proportion of LTBI people who have been diagnosed with TST positive conversion was higher in those aged 10–14 years than in those aged 15–19 years (Figure 4).
Figure 4.
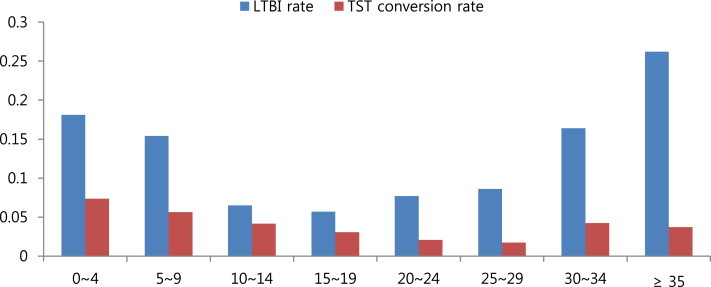
Latent tuberculosis infection (LTBI) rate and tuberculin skin test (TST) conversion rate by age.
For treatment of LTBI, the consent procedure should be gone through prior to treatment (Table 3). The proportion of LTBI individuals who agreed to the treatment was 79.7%, and the proportion of those who completed treatment among people supposed to finish treatment up to December 31, 2013 was 90.3%. The highest treatment consent rate by congregate settings was 93.2% in correctional facilities and social welfare facilities, and the lowest rate was 63.0% in the workplace. The highest treatment completion rate, 100%, was in workplaces, and there was a 91.2% treatment completion rate in educational facilities, but the rate in elementary schools was relatively low (76.5%).
Table 3.
Treatment agreement rate and completion rate by congregate settings.
| Congregate settings | Treatment agreement rate (%) | Treatment completion ratea (%) | |
|---|---|---|---|
| Education facilities | Daycare center/kindergarten | 83.8 | 94.1 |
| Elementary school | 88.1 | 76.5 | |
| Middle school | 81.0 | 90.0 | |
| High school | 80.8 | 92.2 | |
| University | 66.2 | 90.4 | |
| Other schools | 72.5 | 100.0 | |
| Subtotal | 78.0 | 91.2 | |
| Military or police unit | 83.9 | 88.6 | |
| Social welfare facilities/correctional facilities | 93.2 | 91.1 | |
| Workplaces | 63.0 | 100.0 | |
| Others | 64.6 | 42.9 | |
| Total | 79.7 | 90.3 | |
Treatment completion rate of latent tuberculosis infection (LTBI) is the proportion of people who completed treatment among those supposed to finish treatment up to December 31, 2013.
4. Discussion
The most important purpose of the TB contact investigation is to find and prevent additional patients. We found and cured 259 additional TB patients through targeted contact investigation in congregate settings. The detection rate of TB patients was about 0.2%. TB patient detection rate of family contacts was 1.9% in 2011–2012 in the ROK [5]. It is known that the detection rate of the United States was about 1–2% [6–9], thus our detection rate was lower than others. The reason for the low detection rate could be the setup of a wide range of contacts. For example, if two infectious TB patients occur within 6 months in a school, we set up the contacts as all students in the same grade, and if there was one additional patient, we set up the contacts as all students in the school. There is a very large difference between our investigation's average number of contact persons per one index patient and the number of the United States. Our average number was about 100 but in the United States, the number was about six [1]. If the range of contacts is set widely, the efficiency of the investigation may be low because of non-recent infected persons included for the LTBI treatment target. If the range of contacts is set narrowly, although the efficiency of investigation can be high, there is a concern about loss of the real recently infected person. In the case of the ROK, to prevent the additional patient is more important than the efficiency of the investigation, because the TB incidence is high. In addition, there is a risk of revealing the index patient's identification when the range of contacts is set up narrowly. This side effect may be the barrier of the contact investigation. However, we need to compare the incidences of close contact and casual contact. It is important that there are efforts to eliminate prejudice about the index patient.
The total LTBI rate of contact investigation in congregate settings was 9.6% in 2013 and there was a large variation according to facility or age. Typically, it is known that one third of the world's population is LTBI [1]. In several studies conducted in the ROK, the TSTs positive rate, >10 mm, was 21.4% at high school screening tests [10], 28% at military unit screening tests, and 31.1% at military unit contact investigation [11]. In addition, the LTBI rate was 28.8% at family contact investigation in the ROK in 2001–2012 [5]. The LTBI rates in our investigation were much lower than those of other studies because we use the dual diagnosis strategy which classifies as LTBI when both TST and IGRA test positive at >13 years old or a TST positive conversion. Another reason may be that contact strength is bigger at family than congregate settings. The temporal interval between the studies might also be considered.
It is known that the strongest evidence of recently infected LTBI is a TST positive conversion. Therefore, a high proportion of positive conversion individuals among the whole LTBI means many recent infected LTBI are included for treatment. This proportion was relatively high at elementary schools, middle schools, and high schools, but a relatively low proportion was seen in those aged >20 years. Thus, bacterial transmission happened more actively at school than university or other social places, and therefore the efficiency of the investigation was higher at school than other settings.
Accept rates and complete rates of LTBI differed among the facilities. Elementary schools showed a relatively high accept rate, but a low complete rate, whereas the accept rates of workplaces and other social facilities were relatively low. These results could be used to establish the LTBI management strategy or policy. Even though we diagnosed LTBI persons through the contact investigation, if the accept rate and complete rate were low, we could not achieve the purpose of the contact investigation. Thus, some way to improve the accept rate and complete rate to prevent additional TB patients is required. According to the literature, a short duration of the LTBI treatment drug regimen may be helpful to complete rate of treatment [12]. Therefore, it is necessary to introduce a short term drug regimen and find a way to intensive medication management.
The limitation of this study is that we did not know when the additional patient became infected, even if he was diagnosed later than the index patient. In addition, we could not be sure that all LTBI persons were infected recently from the index patient. Thus, it is necessary to collect sputum specimens as much as possible and to perform DNA finger print analysis for the propagation path between the patients.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgments
The authors would like to thank Seongchul Lee, GiYeol Heo, Gwang Rae Lim, Inyoung Cho, Eun Jung Lee, Ga Young Lee, Eun young Kim, Soo Yeun Kim and Young Sun Choi for administrative and technical support. This study is funded by Korea Centers for Diseases Control and Prevention (091-4800-4844-303).
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
- 1.World Health Organization . 2013. Global Tuberculosis Report. http://www.who.int/tb/publications/global_report/en/ [accessed 03.12.14] [Google Scholar]
- 2.Dye C., Glaziou P., Floyd K., Raviglione M. Prospects for tuberculosis elimination. Annu Rev Public Health. 2013;34:271–286. doi: 10.1146/annurev-publhealth-031912-114431. [DOI] [PubMed] [Google Scholar]
- 3.Korea Centers for Disease Control and Prevention . 2013. Annual report on the notified tuberculosis in Korea. http://tbfree.cdc.go.kr/tbfree/cmm/BoardView.do?boardType=REPORT&no=402&id=4500 [accessed 03.12.14] [Google Scholar]
- 4.Centers for Disease Control and Prevention Guidelines for using the investigation of contacts of persons with infectious tuberculosis: recommendations from the National Tuberculosis Controllers Association and CDC. MMWR. 2005;54(RR–15) [PubMed] [Google Scholar]
- 5.Seo S.Y., Han J., Kang H. Korean Society for Preventive Medicine; Seoul: 2013. Study of Close Contact Investigation of Patients with Pulmonary Tuberculosis in Korea; p. 291. [Google Scholar]
- 6.Marks S.M., Taylor Z., Qualls N.L. Outcomes of contact investigations of infectious tuberculosis patients. Am J Respir Crit Care Med. 2000 Dec;162(6):2033–2038. doi: 10.1164/ajrccm.162.6.2004022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reichler M.R., Reves R., Bur S. Evaluation of investigations conducted to detect and prevent transmission of tuberculosis. JAMA. 2002 Feb;287(8):991–995. doi: 10.1001/jama.287.8.991. [DOI] [PubMed] [Google Scholar]
- 8.Jereb J., Etkind S.C., Joglar O.T. Tuberculosis contact investigations: outcomes in selected areas of the United States, 1999. Int J Tuberc Lung Dis. 2003 Dec;7(12 Suppl. 3):S384–90. [PubMed] [Google Scholar]
- 9.Anger H.A., Proops D., Harris T.G. Active case finding and prevention of tuberculosis among a cohort of contacts exposed to infectious tuberculosis cases in New York City. Clin Infect Dis. 2012 May;54(9):1287–1295. doi: 10.1093/cid/cis029. [DOI] [PubMed] [Google Scholar]
- 10.Lee J.Y., Choi H.J., Park I.N. Comparison of two commercial interferon-gamma assays for diagnosing Mycobacterium tuberculosis. Eur Respir J. 2006 Jul;28(1):24–30. doi: 10.1183/09031936.06.00016906. [DOI] [PubMed] [Google Scholar]
- 11.Choi C.M., Kang C.I., Kim D.H. The role of TST in the diagnosis of latent tuberculosis infection among military personnel in South Korea. Int J Tuberc Lung Dis. 2006 Dec;10(12):1342–1346. [PubMed] [Google Scholar]
- 12.Horsburgh C.R., Goldberg S., Bethel J. Latent TB infection treatment acceptance and completion in the United States and Canada. Chest. 2010 Feb;137(2):401–409. doi: 10.1378/chest.09-0394. [DOI] [PubMed] [Google Scholar]


