Abstract
Objective
The study aimed at elucidating a potential correlation between specific meteorological variables and the prevalence and intensity of migraine attacks as well as exploring a potential individual predictability of a migraine attack based on meteorological variables and their changes.
Methods
Attack prevalence and intensity of 100 migraineurs were correlated with atmospheric pressure, relative air humidity, and ambient temperature in 4-h intervals over 12 consecutive months. For each correlation, meteorological parameters at the time of the migraine attack as well as their variation within the preceding 24 h were analyzed. For migraineurs showing a positive correlation, logistic regression analysis was used to assess the predictability of a migraine attack based on meteorological information.
Results
In a subgroup of migraineurs, a significant weather sensitivity could be observed. In contrast, pooled analysis of all patients did not reveal a significant association. An individual prediction of a migraine attack based on meteorological data was not possible, mainly as a result of the small prevalence of attacks.
Interpretation
The results suggest that only a subgroup of migraineurs is sensitive to specific weather conditions. Our findings may provide an explanation as to why previous studies, which commonly rely on a pooled analysis, show inconclusive results. The lack of individual attack predictability indicates that the use of preventive measures based on meteorological conditions is not feasible.
Introduction
The influence of the weather on migraine remains one of the most controversially debated aspects of the pathophysiology of migraine. While in clinical practice, migraineurs commonly describe certain weather conditions or their changes over short periods of time as a precipitating factor of their migraine attacks,1,2 scientific evidence supporting this observation is scarce and inconclusive.3 Initial clinical studies were conducted prior to the publication of the IHS criteria,4–7 which define the clinical picture of migraine.8 Furthermore, study design frequently showed methodological shortcomings such as a questionnaire-based design with the associated recall bias4,5,7,9–12 or a lack of dissection of weather as such into its specific meteorological components.12–14 Our findings of a small pilot study with 20 migraineurs suggested that only a subgroup of migraineurs is weather sensitive,15 providing a possible explanation as to why existing studies, which mainly rely on a pooled analysis of all study participants, have shown inconsistent results. However, due to the limited number of participants, definite conclusions could not be drawn.
Based on the promising results of our pilot study,15 it was the aim of this study to elucidate the relationship of specific weather components and migraine in more detail on a large number of migraineurs. We further aimed at investigating whether a potential correlation between a specific meteorological condition and migraine may allow an individual prediction of a migraine attack, as such a predictability could have implications on current treatment strategies.
Methods
Study participants
Clinical data were acquired from the headache diaries of 100 migraineurs who presented for routine consultation at the Headache Outpatient Department at Charité - Universitätsmedizin Berlin, Germany. Included migraineurs were 18–65 years old, had a history of migraine with or without aura based on the criteria established by the International Headache Society (IHS),16 and were residents of Berlin, living within a distance of 50 km of the Headache Center. Headache diaries, which include data about presence of headache, its duration, intensity, location, character, and accompanying symptoms recorded in 4-h intervals, were retrospectively evaluated for the preceding 12 months within the observational period lasting from 1 January 2006 to 31 December 2007. The long duration of the observational period was chosen to exclude a potential change in headache frequency resulting from a seasonal variation. Data provided by migraineurs on preventive treatment were included if patients were on a stable dosage for at least 3 months prior to the observational period and throughout the course of the study. The publication of study results has been approved by the local ethics committee of the Charité – Universitätsmedizin Berlin (EA1/085/14).
Meteorological data
Meteorological data from the meteorological station at Berlin – Alexanderplatz (distance to the Headache Center ∼700 m) were kindly provided by the German Meteorological Service (Deutscher Wetterdienst – DWD, Offenbach, Germany). Data included hourly recordings of atmospheric pressure (in HPa), temperature (in °C), and relative humidity (in %) between 1 January 2006 and 31 December 2007. For statistical analysis, time points (4-h intervals) corresponding to the headache diaries were used.
Statistical analysis
For statistical analysis, we took into account each single entry in the headache diary (migraine events). Outcome measurement was migraine events (single diary entries), coded on a 6-point Likert scale (0 = no headache, 5 = maximum intensity). Migraine events were reported for 1 year, each day and at six standardized time points (equally distributed in 4-h intervals). For the statistical analysis, the dichotomized variable migraine event (yes/no) was chosen. Potential covariates were calendar dates (month, day of the week, clock time) and the meteorological measurements.
For the three meteorological variables (atmospheric pressure, temperature, and relative humidity), 13 covariates for migraine events were defined for each measurement: measurement at the time of the event, six measurements during the preceding 24 h at six time points, and the six differences of measurements between each of the six time points of the preceding 24 h and the time point of the migraine event. Thus, in total, 39 covariates were investigated.
The association of each of these 39 covariates with migraine events was investigated by an analysis of variance (ANOVA) model with clock time (six levels) and migraine event (yes/no) as fixed factors and the respective meteorological measurement variable as the outcome. In a first step, an overall analysis was done adjusting dependency of data from identical patients using the method of generalized estimating equations (IEE dependency structure, SAS PROC GENMOD). Subsequently, an ANOVA was performed for each patient separately amounting to a total of 3900 calculated ANOVA models. In this analysis, separately for each patient, data of the same patient were analyzed as independent. To adjust for multiple testing, the false discovery rate (FDR) [LIT] was limited to 0.05. Using this method, the P-values were listed in decreasing order. The highest P-value was compared to 0.05, the second highest to 0.05/2 and so on, the smallest P-value was compared to the total number of tests (0.05/3900 = 1.28 × 10−5). If in this sequence for one corrected P-value significance was achieved, all P-values smaller than this index value were considered significant. This procedure assured that the percentage of falsely rejected null hypotheses among all rejected null hypotheses amounts to at most 5%. Using this method, overall P-values were corrected and only P-values below a FDR of 0.05 were reported as significant.
For the construction of classificators (individually for each patient), logistic regression analysis (outcome measurement: migraine event yes/no, covariates: meteorological data, clock time data) was applied. Three different classificators were constructed: one only using weather data, one only using clock time data, and one using the combination of both. Forward variable selection was applied for meteorological data but not for clock time data. This technique avoids overfitting of models, that is, the inclusion of too many covariates. Quality of classification was examined using receiver operating characteristic (ROC) analysis. Results were ten-fold cross-validated, that is, for each patient the sample was divided randomly in 10 subsamples, and for each subsample the model constructed was applied in the remaining nine subsamples, leading to a separate, unbiased estimation of the true classification rate for each patient. The level of significance was 0.05 (two-sided). Statistical analysis was performed using SPSS 19.0 software (SPSS Inc., Chicago, IL). The heat map was computed using R version 2.14.2 (www.r-project.org).
Results
Frequency of migraine events and association with calendar dates
One hundred patients documented their migraine events daily in 4-h intervals over 1 year resulting in 219.000 documented single intervals. Pooled for all patients, migraine events (single headache diary entries) were documented for 15.030 intervals (6.9%). The total number of migraine events per patient recorded over 1 year varied between 16 (0.7% of intervals) and 540 migraine events (24.7% of intervals) (Fig.1A). Migraine events varied to a small extent between months and days of the week, most events being recorded in the months of January, May, and July (7.2–7.4%) and least in the months of November, August, and March (6.4–6.5%). Most migraine events were observed in the middle of the week between Tuesday and Wednesday (7.1%), while the events were recorded on Sunday (6.4%). However, a considerable dependency of migraine events on clock time was observed, with most events at 4 am (9.1%) and 8 am (9.0%) and least events at 8 pm (4.8%) and midnight (3.3%) (Fig.1B). As a consequence of these findings, all analyses were adjusted for clock time.
Figure 1.
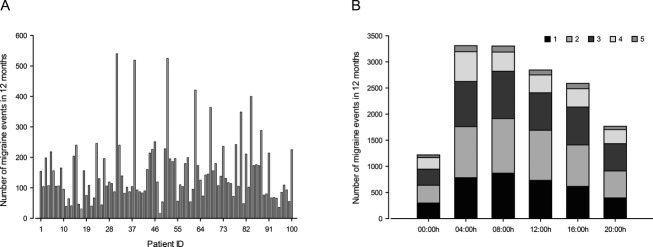
Distribution of migraine events. (A) Number of migraine events for each study participant. (B) Distribution of migraine events over all recorded time points. Stacks indicate migraine intensities with 1 representing the lowest and 5 the highest pain intensity.
Association of migraine events and meteorological variables
Overall analysis pooled for the complete sample of 100 patients did not reveal a significant association of the analyzed meteorological variables and the occurrence of migraine events. However, the overall distribution of P-values is skewed toward smaller values, which demonstrates the presence of some degree of association between weather and migraine (Fig.2A). Therefore, a separate analysis for each patient was conducted. This analysis, adjusted for multiplicity of testing, did reveal significant associations for some of the migraineurs (Fig.2B). Based on the analysis of 3900 tests of significance, 43 tests passed the criterion of a FDR of 0.05. Significant results were limited to a total of 13 patients (13%, 95% CI = 7.1–21.2%) (Fig.2B, Table1). The results therefore indicate that 13% of study participants could be clearly identified as weather sensitive with regard to their migraine events. In this regard, we observed at least one P-value below 0.001 in 31 patients (including the 13 identified weather sensitive migraineurs), compared to four patients with one or more P-values below 0.001 expected by chance when applying 39 independent tests of significance, suggesting that the amount of 13% weather sensitive migraineurs is likely underestimated (Fig.3). However, the results further indicate that significant values or their changes do not follow a constant pattern. While one patient may show a correlation between migraine events and rising atmospheric pressure, another patient's migraine events may correlate to falling atmospheric pressure suggesting that it is the unusual weather condition or a change in a specific parameter as such, that correlates with a migraine event, not its direction (Table1).
Figure 2.

Overall distribution of P-values. The figure shows the distribution of the P-values calculated for all 100 patients. The horizontal line displays the expected number of P-values for a uniform distribution between 0 and 1. Skewing toward smaller P-values indicates a significant association.
Table 1.
Significant predictors for 13 selected weather sensitive migraineurs
| Patient ID |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 9 | 22 | 41 | 51 | 52 | 53 | 62 | 67 | 72 | 80 | 84 | 88 | 91 | Total | |
| pressure | − | − | + | − | 4 | |||||||||
| pressure_4 | + | − | 2 | |||||||||||
| pressure_8 | + | − | 2 | |||||||||||
| pressure_12 | + | − | 2 | |||||||||||
| pressure_16 | + | − | 2 | |||||||||||
| pressure_20 | + | − | 2 | |||||||||||
| pressure_24 | + | − | 2 | |||||||||||
| pressure_d8 | − | 1 | ||||||||||||
| pressure_d12 | − | − | 2 | |||||||||||
| pressure_d16 | − | − | 2 | |||||||||||
| pressure_d20 | − | − | 2 | |||||||||||
| pressure_d24 | − | − | 2 | |||||||||||
| temperature | + | + | 2 | |||||||||||
| temperature_4 | + | 1 | ||||||||||||
| temperature_8 | + | + | 2 | |||||||||||
| temperature_12 | + | 1 | ||||||||||||
| temperature_16 | − | + | 2 | |||||||||||
| temperature_20 | + | 1 | ||||||||||||
| temperature_24 | + | + | 2 | |||||||||||
| temperature_d12 | + | 1 | ||||||||||||
| temperature_d16 | + | 1 | ||||||||||||
| temperature_d24 | − | 1 | ||||||||||||
| humidity | − | 1 | ||||||||||||
| humidity_12 | − | 1 | ||||||||||||
| humidity_16 | − | 1 | ||||||||||||
| humidity_d24 | + | 1 | ||||||||||||
| Total | 1 | 2 | 1 | 2 | 4 | 2 | 7 | 1 | 2 | 7 | 2 | 7 | 5 | 43 |
Pressure is the measurement during the migraine event, pressure_4 is the measurement for hours before the event and pressure_d4 is the difference between pressure_4 and pressure. All other variables are defined analogously. + (−), the respective measurement or the difference was significantly larger (smaller) for time points with migraine. No significant associations between weather data and migraine events were observed for 13 weather variables. These variables are not listed in the table.
Figure 3.
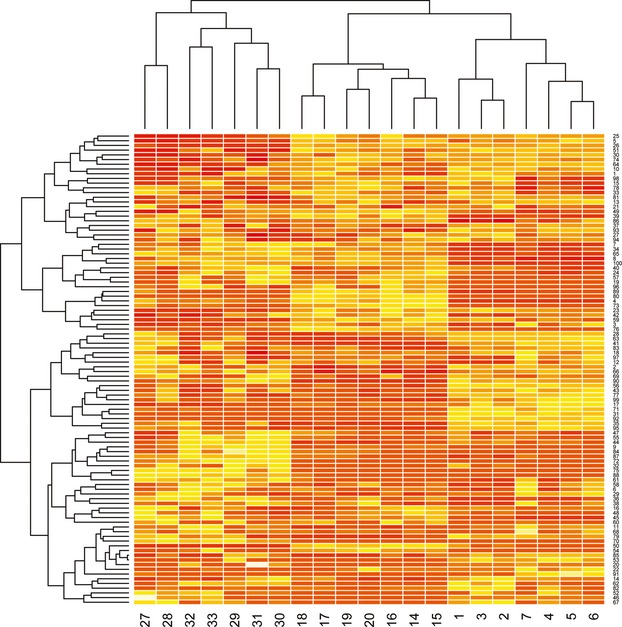
Clustering of patients with similar weather sensitivity. The rows of the illustrated heat map refer to patients, columns to weather variables (k = 21; pressure: 1–7, temperature: 14–20, humidity: 27–33). Dark red color refers to a strong association between weather data and migraine events.
Individual classification
For the 13 patients showing an association between their migraine events and specific meteorologic parameters, ROC analysis was applied to inspect classification rates for migraine events based on clock time and meteorological data. The classification rates were obtained using the predicted probability from the logistic regression analysis for migraine events as classificator. Areas under the curve (AUC) were compared for three approaches: using only clock time data, only weather data or the combination of both. Exclusive analysis of weather data was superior to that of clock time data. The combination of both improved the classification considerably as compared to the exclusive analysis of clock time. However, AUC ranged between 0.58 and 0.70 for the selected 13 migraineurs. These results clearly demonstrate that even in weather sensitive migraineurs, an individual prediction of their attacks based on the investigated meteorological parameters is not feasible.
Discussion
This study aimed at investigating a potential relationship between specific meteorological parameters and the occurrence of migraine attacks and furthermore at elucidating the feasibility of weather data based prediction of migraine attacks. The results show a significant correlation, but only in a subgroup of migraineurs confirming the preliminary results of our pilot study.15 Within this subgroup, the association remains significant even after adjusting data for multiplicity of testing and for clock time. In contrast to the observations made in our previous study, the findings of this study reveal that the changes as such of the investigated meteorologic parameters, not a specific change into a certain direction, correlate with a higher incidence of migraine events. However, the study results further revealed that a prognosis of migraine attacks in susceptible individuals based exclusively on the investigated weather parameters is not possible.
Migraineurs commonly describe the weather as a reliable trigger of their attacks1,2 but clinical studies aimed at confirming this observation deliver inconclusive results. This discrepancy reflects the pathophysiological complexity of migraine and the lack of adequate study design rather than of a common misperception of a substantial number of migraineurs.
Migraine is a complex disorder of the brain which can be triggered by a multitude of conditions.1,14,17,18 Interestingly, not all patients respond to the same trigger factors. It may therefore be assumed that different trigger factors may elicit the relatively homogeneous and well-defined clinical syndrome of migraine8 through distinct mechanisms. It may be postulated that trigger factors that have been identified by migraineurs are much less common than generally assumed and may simply reflect premonitory symptoms during the early phase of an already ongoing migraine attack. This hypothesis is supported by recent evidence indicating that many external stimuli commonly identified as trigger factors may not trigger migraine attacks when systematically studied in a prospective setting.19,20 However, the design of this study consists of an objective and retrospective correlation between the presence of migraine and specific meteorological conditions so that the possibility of a misinterpretation of a premonitory symptom is excluded.
Clinical studies analyzing the influence of specific weather components on migraine have focused mainly on atmospheric pressure, ambient temperature, and relative humidity.15,21,22 In this context, many, but not all migraineurs indicate these weather components as being a trigger factor for their migraine attacks.15 However, most clinical studies were based on the hypothesis that migraineurs are weather sensitive without analyzing further if this relationship may only exist in a subgroup of patients. Our data indicate that only 13% of the studied migraineurs are weather sensitive. If data from these patients are pooled with data obtained from the remaining 87 patients, significance is lost. In this context, in the 3900 tests of significance we observed 664 (17%) significant results compared to 195 (5%) that would be expected by chance. Moreover, 50 of 100 migraineurs showed uncorrected P-values below 0.05. However, as an individual distinction of a significance by chance or as a result of a true correlation is not possible without an adjustment for the multiplicity of testing, we applied a FDR with the respective loss of significances inherent to the statistical technique. With this method, we could clearly identify single weather sensitive migraineurs but their total amount (13%) may be underestimated. This is underlined by the fact that in an additional 15 patients, we found results which strongly indicated an existing weather sensitivity based on the observed P-values for the 39 tests of significance calculated for each patient. In addition, for patients with a low attack frequency a correlation may be missed as for these individuals the power of the study may not have been large enough to demonstrate a relationship between their migraine events and the analyzed meteorological variables.
Taken together, the results indicate that at least 13% of study participants are weather sensitive but due to the strict statistical adjusting methods applied, the actual number of weather sensitive migraineurs could be substantially higher. Even so, the relatively small number of weather sensitive migraineurs and the extent of the correlation in affected patients may explain why many studies, which studied an entire population without performing an individual analysis for each patient, have failed to consistently show a correlation that would reflect the perception of many migraineurs.
In addition to the difficulties and contradicting results in demonstrating a relationship between meteorological components and migraine,9,15,21–23 clinical studies have furthermore shown inconclusive results with regard to the specific meteorological parameter responsible for the association or its specific change over time. While some studies, for example, observed an influence of atmospheric pressure on migraine21 others did not observe a significant correlation15 despite very similar study designs. Some studies showed a correlation between migraine and cold temperatures15,24 other studies found opposing results.9–11 The results of this study suggest that the meteorological change as such may be associated with migraine, regardless of its direction. This finding adds to the explanation as to why previous studies had substantial difficulties in demonstrating a specific meteorological condition serving as a trigger factor of migraine attacks, especially in studies that analyzed a complete population without performing individual analyses for all study participants. In this context, it has to be considered that in susceptible individuals migraine-associated weather changes probably only increase the risk of suffering a migraine attack, but other factors may be required to trigger the attack.
With the identification of weather sensitive individuals the question about a clinical implication is a logical consequence. As weather is a nonavoidable trigger factor, one may speculate if a short-term preventive treatment would be a feasible option if a specific meteorological condition known to be associated with migraine would be forecasted. We therefore conducted logistic regression analysis to calculate the individual classification rates for the prediction of migraine events in the 13 identified weather sensitive migraineurs. The results indicate that an individual prognosis of migraine events solely based on the analyzed weather parameters is not possible, even if this question is restricted to confirmed weather sensitive migraineurs. Moreover, the selection of the 13 most weather sensitive migraineurs may have produced a bias toward better classification rates. Equating sensitivity and specificity for the moment to 70%, which was the result for the best classified patient, for an event prevalence of 10% during the 2190 time intervals reported, the positive predictive value would only be 19%. Therefore, we concluded that due to the relatively small event prevalence, even among frequent migraineurs and the extent of the correlation, positive predictive values would be too small to justify an intervention, such as a short-term preventive treatment, based on weather data. The fact that a weather-based prediction of migraine attacks is not feasible highlights the complexity of the pathophysiology of migraine and supports the assumption that migraine attacks may be the result from a combination of multiple factors, none of which alone may be significant enough to trigger an attack.
Acknowledgments
The authors would like to thank Lisa Wang, MSc at the Institute for Clinical Epidemiology and Applied Biometry in Tübingen (Germany) for providing the heat map.
Author Contributions
Jan Hoffmann involved in conception and design of the study, acquisition of data, analysis and interpretation of data, drafting and revising of the manuscript, study coordination and supervision. Tonio Schirra contributed to acquisition of data, revision of the manuscript. Hendra Lo involved in acquisition of data, revision of the manuscript. Lars Neeb contributed to acquisition of data, revision of the manuscript. Uwe Reuter involved in conception and design of the study, acquisition of data, revision of the manuscript. Peter Martus contributed to conception and design of the study, statistical analysis, analysis and interpretation of data, drafting and revising of the manuscript.
Conflict of Interest
Jan Hoffmann received travel reimbursement from Pharm-Allergan, the International Headache Society and the American Headache Society as well as a research fellowship from the Deutsche Forschungsgemeinschaft – DFG (HO4369/1-1). Tonio Schirra reports no disclosures. Hendra Lo reports no disclosures. Lars Neeb received honoraria for speaking and funding for travel expenses from Pharm-Allergan and St. Jude Medical. Uwe Reuter has recently received honoraria from Co-Lucid, Amgen, Pharm-Allergan, Autonomic Technologies for participation in advisory boards or other company related activities (scientific presentations). He also received honoraria from St. Jude Medical, Berlin Chemie, Almirall, MSD, Janssen-Cilag and Glaxo Smith Kline. Peter Martus received honoraria from Parexel for serving on a Safety Board.
References
- Wöber C, Holzhammer J, Zeitlhofer J, et al. Trigger factors of migraine and tension-type headache: experience and knowledge of the patients. J Headache Pain. 2006;7:188–195. doi: 10.1007/s10194-006-0305-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Mackensen S, Hoeppe P, Maarouf A, et al. Prevalence of weather sensitivity in Germany and Canada. Int J Biometeorol. 2005;49:156–166. doi: 10.1007/s00484-004-0226-2. [DOI] [PubMed] [Google Scholar]
- Becker WJ. Weather and migraine: can so many patients be wrong? Cephalalgia. 2011;31:387–390. doi: 10.1177/0333102410385583. [DOI] [PubMed] [Google Scholar]
- Gomersall JD, Stuart A. Variations in migraine attacks with changes in weather conditions. Int J Biometeorol. 1973;17:285–299. doi: 10.1007/BF01804622. [DOI] [PubMed] [Google Scholar]
- Cull RE. Barometric pressure and other factors in migraine. Headache. 1981;21:102–103. doi: 10.1111/j.1526-4610.1981.hed2103102.x. [DOI] [PubMed] [Google Scholar]
- Wilkinson M, Woodrow J. Migraine and weather. Headache. 1979;19:375–378. doi: 10.1111/j.1526-4610.1979.hed1907375.x. [DOI] [PubMed] [Google Scholar]
- Osterman PO, Lövstrand KG, Lundberg PO, et al. Weekly headache periodicity and the effect of weather changes on headache. Int J Biometeorol. 1981;25:39–45. doi: 10.1007/BF02184436. [DOI] [PubMed] [Google Scholar]
- Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- Prince PB, Rapoport AM, Sheftell FD, et al. The effect of weather on headache. Headache. 2004;44:596–602. doi: 10.1111/j.1526-4610.2004.446008.x. [DOI] [PubMed] [Google Scholar]
- Cooke LJ, Rose MS, Becker WJ. Chinook winds and migraine headache. Neurology. 2000;54:302–307. doi: 10.1212/wnl.54.2.302. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Wellenius GA, Suh HH, et al. Weather and air pollution as triggers of severe headaches. Neurology. 2009;72:922–927. doi: 10.1212/01.wnl.0000344152.56020.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spierings EL, Ranke AH, Honkoop PC. Precipitating and aggravating factors of migraine versus tension-type headache. Headache. 2001;41:554–558. doi: 10.1046/j.1526-4610.2001.041006554.x. [DOI] [PubMed] [Google Scholar]
- Robbins L. Precipitating factors in migraine: a retrospective review of 494 patients. Headache. 1994;34:214–216. doi: 10.1111/j.1526-4610.1994.hed3404214.x. [DOI] [PubMed] [Google Scholar]
- Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394–402. doi: 10.1111/j.1468-2982.2007.01303.x. [DOI] [PubMed] [Google Scholar]
- Hoffmann J, Lo H, Neeb L, et al. Weather sensitivity in migraineurs. J Neurol. 2011;258:596–602. doi: 10.1007/s00415-010-5798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- Wober C, Brannath W, Schmidt K, et al. Prospective analysis of factors related to migraine attacks: the PAMINA study. Cephalalgia. 2007;27:304–314. doi: 10.1111/j.1468-2982.2007.01279.x. [DOI] [PubMed] [Google Scholar]
- Wöber C, Wöber-Bingöl Ç. Chapter 12 – triggers of migraine and tension-type headache. In: Michael J, Aminoff FB, Dick FS, editors. Handb Clin Neurol. Vol. 97. 2010. pp. 161–172. [DOI] [PubMed] [Google Scholar]
- Hougaard A, Amin FM, Hauge AW, et al. Provocation of migraine with aura using natural trigger factors. Neurology. 2013;80:428–431. doi: 10.1212/WNL.0b013e31827f0f10. [DOI] [PubMed] [Google Scholar]
- Hoffmann J, Recober A. Migraine and triggers: post hoc ergo propter hoc? Curr Pain Headache Rep. 2013;17:370. doi: 10.1007/s11916-013-0370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimoto K, Aiba S, Takashima R, et al. Influence of barometric pressure in patients with migraine headache. Intern Med. 2011;50:1923–1928. doi: 10.2169/internalmedicine.50.5640. [DOI] [PubMed] [Google Scholar]
- Zebenholzer K, Rudel E, Frantal S, et al. Migraine and weather: a prospective diary-based analysis. Cephalalgia. 2011;31:391–400. doi: 10.1177/0333102410385580. [DOI] [PubMed] [Google Scholar]
- Larmande P, Hubert B, Sorabella A, et al. Influence of changes in climate and the calendar on the onset of a migraine crisis. Rev Neurol (Paris) 1996;152:38–43. [PubMed] [Google Scholar]
- Scheidt J, Koppe C, Rill S, et al. Influence of temperature changes on migraine occurrence in Germany. Int J Biometeorol. 2012;57:649–654. doi: 10.1007/s00484-012-0582-2. [DOI] [PubMed] [Google Scholar]


