Abstract
Persisting hemianopia frequently complicates lesions of the posterior cerebral hemispheres, leaving patients impaired on a range of key activities of daily living. Practice-based therapies designed to induce compensatory eye movements can improve hemianopic patients' visual function, but are not readily available. We used a web-based therapy (Eye-Search) that retrains visual search saccades into patients' blind hemifield. A group of 78 suitable hemianopic patients took part. After therapy (800 trials over 11 days), search times into their impaired hemifield improved by an average of 24%. Patients also reported improvements in a subset of visually guided everyday activities, suggesting that Eye-Search therapy affects real-world outcomes.
Introduction
Hemianopia is relatively common, complicating about 15% of strokes.1 Its all-cause prevalence is ∼1% in the over 50s.2 Unfortunately, unlike the majority of motor and cognitive impairments caused by focal brain injury, spontaneous improvement is rare, especially if the hemianopia is complete (17%).3 Hemianopia has a pervasive effect on many activities of daily living (ADL) with >80% of patients reporting problems with driving, shopping, and financial management.4 A variety of treatments are available, the most promising being eye movement-based therapies.5 These induce compensatory eye movements via repetitive practice. Because different types of eye movement are required for different visually guided activities (e.g., reading vs. visual search), these therapies have been shown to be very task specific.6
We previously reported an eye movement-based therapy: “ramp-step” which requires pursuit of a moving target followed by a saccade when the target jumped. This improved visual search after a single session of 300 trials.7 The effect size was large (50%) and came at no cost to visual search into the seeing field. However, the study only included seven patients with hemianopia and had no patient-reported outcome measures. Here, we use a freely available internet-based version of ramp-step therapy on a much larger sample to examine if any therapeutic effects generalize to everyday activities.
With the help of a series of patient-developers, we produced Eye-Search, a browser-based app. It contains four tests which are completed at baseline (T0, prior to therapy) and every time 400 therapy trials are completed. Basic demographic details are also collected.
Subjects and Methods
Participants
This study was approved by the UCL Research Ethics Committee. The patients were self-selected and signed an online consent form. Patient data are stored on a secure university server. Inclusion criteria for the analyses were sequentially applied as follows: (1) Patients with a clear hemianopia who completed assessments at two or more time points (n = 142). (2) No evidence of neglect: 14 had neglect (79% of these with a left-sided hemianopia) and seven had an uninterpretable test: all (n = 21) were excluded. (3) A further 43 of the remaining patients (36%) who had <10% search time deficit into the affected visual field pretherapy, were excluded because the presence of a deficit is necessary in order to assess the effects of rehabilitation. This left 78 patients for data analysis.
Their median age was 60 years (IQR = 47:70). Sixty-four percent were male. Seventy-seven percent reported the cause of their hemianopia as stroke; 8% reported tumor/AVM; 3% TBI while 13% selected “other.” On the visual field test 64% had encroachment into the first degree lateral to fixation (macular-splitting hemianopia), consistent with reported prevalence.8 The time from the onset of their hemianopia to participating in the study (T0), was rightwardly skewed with mean of 34.5 months and a median of 4.3 months (IQR = 1.7:8.9). The median time from T0–T1 (to complete 400 trials) was 5 days (1.8:14.2); and from T0–T2 (completing 800 trials) was 11 days (4.3:23.5).
Eye-Search: cognitive tests and therapy
Visual field test
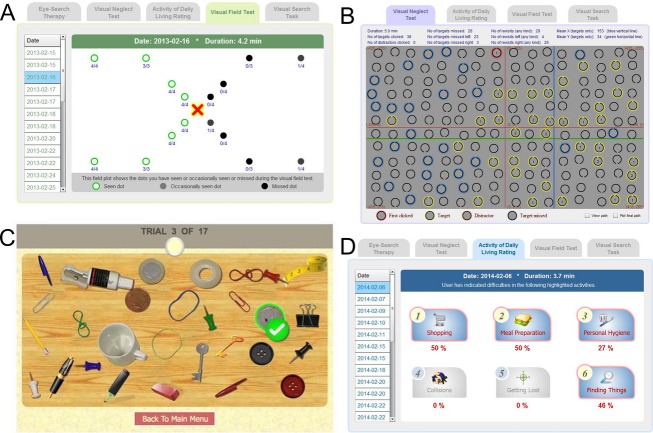
We adapted a validated, online visual field test.9 Testing four points at 1, 2.5, 5, and 10° eccentricity diagonally offset from both the horizontal and vertical meridians (Fig.1A). Each point was tested four times over 36 different stimuli. Hemianopia was diagnosed if two or more points were missed in the same hemifield, at either T0 or T1.
Figure 1.
Screen shots from the four Eye-Search cognitive tests. (A) Visual field test, showing a patient with a right-sided, homonymous hemianopia with macular splitting. (B) Neglect test from a different patient showing leftward neglect. Targets are circles with a gap at the top. Those that were correctly selected are outlined in yellow; missed targets are outlined in blue. Numbers within targets are revisits (abnormal). The average target position (always in the center of the field) is shown in red crosshairs, while the average position of targets selected is in blue and green crosshairs; this shows the patient's average spatial bias (to the right in this case). (C) Crowded desk scene for the main outcome measure (visual search). In this case the subject has correctly located the 20 pence coin to the right of fixation. (D) Output from a different patient's T0 activities of daily living (ADL) ratings.
Neglect test
We adapted a sensitive test of visual neglect.10 Neglect was diagnosed if patients missed twice as many targets to one side compared with the other, or if they had a similar ratio of revisits (Fig.1B).
Visual search test (primary outcome measure)
We adapted a validated, reaction time-based, visual search test where subjects had to search for an everyday object in a crowded desk scene7 (see: http://www.eyesearch.ucl.ac.uk/es/es_sc_vst.php and Fig.1C). After a practice trial, 16 trials were pseudorandomly split 50:50 into target left:target right trials. Reaction time was taken as time from the cluttered desk to appear to a correct click on the item. Incorrect trials were excluded. A mean RT was calculated for left and right-sided trials which were re-labeled as affected/unaffected field means.
Patient-reported outcome measures (secondary outcome measure)
A vertically orientated visual analogue scale was used by patients to rate their abilities for the following six ADLs: shopping; meal preparation; personal hygiene; collisions; getting lost, and finding things.4 The scale was calibrated 0 (no problem) to 100 (impossible): http://www.eyesearch.ucl.ac.uk/es/es_sc_adl.php (Fig.1D). T0 scores were hidden from subjects when re-rating their ADLs at T1 and T2.
Therapy: ramp-step paradigm
Subjects were instructed to pursue a smoothly moving stimulus (ramp phase) from one side of the display toward the midline, and then quickly shift gaze to its new location when it unpredictably “jumped” into the opposite hemifield (step phase).7 The stimulus was a white circle with a black “C” that appeared to roll as it moved. Subjects had to report the orientation of the C (up or down) in the final target. To encourage subjects to follow the target during the ramp phase, the endpoint after the jump was partly predictable based on this initial trajectory. To ensure subjects generated a saccade to the endpoint, the “C” was small enough that it could only be discriminated with foveal vision. There were 400 trials per level with the start position on the left or right (50:50 ratio). There were 16 levels which varied in difficulty (varying numbers of distractors, less predictable trajectory, more complex background, lower contrast targets). Subjects could do as many trials as they liked in any one session. After 400 trials they had to retest themselves on all four cognitive tests before they could access the therapy again.
Statistical methods
Primary and secondary outcome measures were entered into repeated-measures analysis of variance (ANOVA)s using SPSS v22 software Armonk, NY: IBM Corp. with time as the within-group factor. An additional within-group factor: field (affected/unaffected), was entered for the visual search analysis. Where sphericity assumptions were violated, Greenhouse-Geisser measures are reported. Significance was set at the conventional P < 0.05 level. We also calculated effect sizes for the main outcome measure using both unstandardized ((T0 − T2)/T0 × 100 = % improvement in RT) and standardized (Cohen's d) methods.
Results
Visual search
Two analyses were carried out for both T0–T1 (78 subjects) and T0–T1–T2 time points (56 subjects). There was a significant time × hemifield interaction for both the T0–T1 F(1, 77) = 3.98, P = 0.05, and T0–T1–T2 F(2, 54) = 8.58, P = 0.001, analyses (Fig.2).
Figure 2.
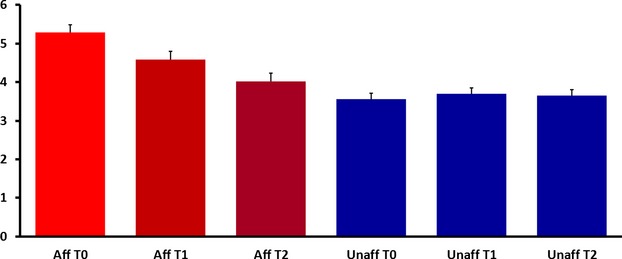
Average reaction times (y-axis in seconds) to items in the affected (Aff: red) and unaffected (Unaff: blue) at the three timepoints: pretherapy (T0), after 400 trials (T1) and after 800 trials (T2). Error bars show within subject, standard error of the mean.
The unstandardized effect size between T0–T2 was 24% reduction in search time into the affected field, with a Cohen's d of 0.48 (at the border between a “medium” and “large” effect).
ADLs
Of the six ADL ratings, only three significantly improved over time (T0–T1–T2): “shopping” F(1.8, 54) = 5.36, P = 0.008; “collisions” F(2, 54) = 8.12, P < 0.001; and, “finding things” F(2, 54) = 3.12, P = 0.048. The other three: “meal preparation”, “hygiene”, and “getting lost” did not: Ps all >0.45 (Fig.3).
Figure 3.
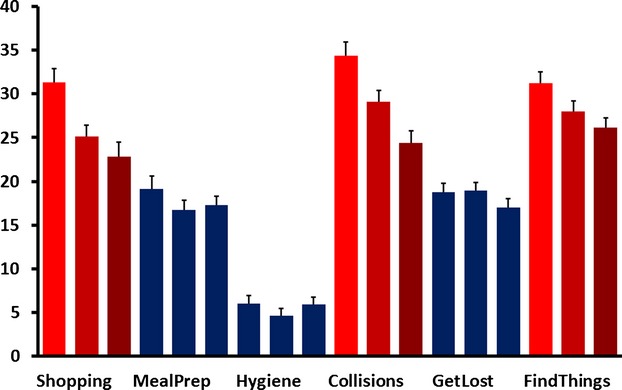
Average, self-reported difficulty ratings (y-axis in %) for the six activities of daily living (ADL) categories. For each category three scores are shown, one for each time point left-to-right (T0–T1–T2). Categories that significantly declined over time are shown in red, those with no significant change are in blue. Error bars show within subject, standard error of the mean.
Discussion
Use of a web-based therapy for hemianopia led to objective improvements in visual search times, and also benefited ADLs dependent on visual guidance, according to the patients' own ratings. Given that hemianopic patients don't always interact with standard care pathways,11 Eye-Search provides a high impact therapy that, given the reach of the internet, is scalable to very large numbers of patients throughout the world.
Patients improved on three of the six self-reported outcome measures. This suggests that therapy effects are not limited to the task but can translate to improve “real-world” outcomes. While there could be an expectation of improvement in “finding things”, given that the training and assessment tasks are of this nature, the other two activities (“collisions” and “shopping”) do not relate to components of the task. However, all three of these activities involve identifying objects that appear in the visual angle treated by Eye-Search (∼15° either side of fixation).
No control group was included (e.g.,: hemianopic patients with no visual search impairment) for two reasons: firstly, it does not make sense to expose patients to a rehabilitation intervention when they stand no chance of gaining from it; secondly, search times into the undamaged hemifield act as the critical within-subject control. It is very unlikely that the improvement in search times into the damaged field are due to practice effects on the outcome test, as this would also have been true for search times into the undamaged hemifield and we would have seen no significant time × hemifield interaction. We selected patients who had a clear disparity (>10%) in their visual search times to targets in their affected versus unaffected visual fields prior to therapy, so there is a concern that this could introduce a selection bias, in which case improvements at the second time point (T1) could be due to regression to the mean.12 However, the fact that patients continued to improve between T1 and the third time point (T2) makes this explanation unlikely: patients were not selected based on performance at T1 so regression to the mean cannot account for subsequent improvements.
The effect size was less than in the original face-to-face study (24% vs. 50%). This could be explained by the online visual search test being easier (fewer distractors). As in the original pilot, there was no “cost” of therapy in terms of increased search times into the unaffected hemifield. This is important because some visual therapies (e.g.,: for patients with prosopagnosia) have been shown to come with a perceptual cost.13
These findings show that a web-based eye movement therapy for patients with hemianopia can be effective. The effect size is moderate to large and appears to have an impact on self-reported, visually guided ADLs. This is the first web-based therapy for visual search disorders and is available for suitable patients to use for free anywhere with internet access: https://www.eyesearch.ucl.ac.uk/.
Acknowledgments
This work was funded by The Stroke Association. P. M. B. and M. H. were supported by the Wellcome Trust. We would like to thank Stephanie Wolff (occupational therapist) who provided ideas on how to capture patient-reported outcome measures in hemianopic patients.
Author Contribution
Y.-H. O. developed and tested all aspects of Eye-Search and she supported users with online help. She also contributed to the writing of the manuscript. S. J.-C. contributed to the development of the ramp-step therapy that was adapted for Eye-Search. She contributed to the writing of the manuscript. N. G. developed the neglect test that was adapted for Eye-Search. He contributed to the writing of the manuscript. P. M. B. contributed to the development of the ramp-step therapy and developed the main outcome measure (visual search task) that was adapted for Eye-Search. He contributed to the analysis of the data and the writing of the manuscript. M. H. contributed to the development of the ramp-step therapy and helped develop the visual tests and contributed to the writing of the manuscript. A. P. L. conceived and managed the project, secured the funding, carried out the statistical analyses, and contributed to the writing of the manuscript.
Conflict of Interest
None declared.
References
- Rathore SS, Hinn AR, Cooper LS, et al. Characterization of incident stroke signs and symptoms: findings from the Atherosclerosis Risk in Communities study. Stroke. 2002;33:2718–2721. doi: 10.1161/01.str.0000035286.87503.31. [DOI] [PubMed] [Google Scholar]
- Gilhotra JS, Mitchell P, Healey PR, et al. Homonymous visual field defects and stroke in an older population. Stroke. 2002;33:2417–2420. doi: 10.1161/01.str.0000037647.10414.d2. [DOI] [PubMed] [Google Scholar]
- Gray CS, French JM, Bates D, et al. Recovery of visual fields in acute stroke: homonymous hemianopia associated with adverse prognosis. Age Ageing. 1989;18:419–421. doi: 10.1093/ageing/18.6.419. [DOI] [PubMed] [Google Scholar]
- Warren M. Pilot study on activities of daily living limitations in adults with hemianopsia. Am J Occup Ther. 2009;63:626–633. doi: 10.5014/ajot.63.5.626. [DOI] [PubMed] [Google Scholar]
- Schofield TM, Leff AP. Rehabilitation of hemianopia. Curr Opin Neurol. 2009;22:36–40. doi: 10.1097/WCO.0b013e32831f1b2c. [DOI] [PubMed] [Google Scholar]
- Schuett S, Heywood CA, Kentridge RW, et al. Rehabilitation of reading and visual exploration in visual field disorders: transfer or specificity? Brain. 2012;135(Pt 3):912–921. doi: 10.1093/brain/awr356. [DOI] [PubMed] [Google Scholar]
- Jacquin-Courtois S, Bays PM, Salemme R, Leff AP, Husain M. Rapid compensation of visual search strategy in patients with chronic visual field defects. Cortex. 2013;49(4):994–1000. doi: 10.1016/j.cortex.2012.03.025. Apr; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X, Kedar S, Lynn MJ, et al. Homonymous hemianopias: clinical-anatomic correlations in 904 cases. Neurology. 2006;66:906–910. doi: 10.1212/01.wnl.0000203913.12088.93. [DOI] [PubMed] [Google Scholar]
- Koiava N, Ong YH, Brown MM, et al. A ‘web app’ for diagnosing hemianopia. J Neurol Neurosurg Psychiatry. 2012;83:1222–1224. doi: 10.1136/jnnp-2012-302270. [DOI] [PubMed] [Google Scholar]
- Parton A, Malhotra P, Nachev P, et al. Space re-exploration in hemispatial neglect. Neuroreport. 2006;17:833–836. doi: 10.1097/01.wnr.0000220130.86349.a7. [DOI] [PubMed] [Google Scholar]
- Rowe F. Care provision and unmet need for post stroke visual impairment. London: Stroke Association and Thomas Pocklington Trust; 2014. [Google Scholar]
- Furby L. Interpreting regression toward mean in developmental research. Dev Psychol. 1973;8:172–179. [Google Scholar]
- Behrmann M, Marotta J, Gauthier I, et al. Behavioral change and its neural correlates in visual agnosia after expertise training. J Cogn Neurosci. 2005;17:554–568. doi: 10.1162/0898929053467613. [DOI] [PubMed] [Google Scholar]