Abstract
Background
Lack of insurance is associated with suboptimal receipt of diabetes preventive care. One known reason for this is an access barrier to obtaining healthcare visits; however, little is known about whether insurance status is associated with differential rates of receipt of diabetes care during visits.
Purpose
To examine the association between health insurance and receipt of diabetes preventive care during an office visit.
Methods
This retrospective cohort study used electronic health record and Medicaid data from 38 Oregon community health centers. Logistic regression was used to test the association between insurance and receipt of four diabetes services during an office visit among patients who were continuously uninsured (n=1,117), continuously insured (n=1,466), and discontinuously insured (n=336) in 2006–2007. Generalized estimating equations were used to account for within-patient correlation. Data were analyzed in 2013.
Results
Overall, continuously uninsured patients had lower odds of receiving services at visits when due, compared to those who were continuously insured (AOR=0.73, 95% CI=0.66, 0.80). Among the discontinuously insured, being uninsured at a visit was associated with lower odds of receipt of services due at that visit (AOR=0.77, 95% CI=0.64, 0.92) than being insured at a visit.
Conclusions
Lack of insurance is associated with a lower probability of receiving recommended services that are due during a clinic visit. Thus, the association between being uninsured and receiving fewer preventive services may not be completely mediated by access to clinic visits.
Introduction
Preventive diabetes care decreases the risk of complications.1–4 Yet, despite the effectiveness of preventive care, many patients delay or forgo recommended services.5,6 One factor contributing to this phenomenon is lack of health insurance; uninsured people are less likely to receive healthcare services than insured,7–17 even at community health centers (CHCs) providing services at low or no cost to many uninsured patients.10,12,15
Lack of insurance is associated with fewer office visits.18–24 It is unclear, however, whether access to primary care visits is sufficient to ensure that uninsured patients receive needed services, or whether insurance status is related to differential receipt of care even when patients have visits. It is hypothesized that there is a significant association between insurance status and receipt of recommended diabetes services at visits when services are due.
Methods
This study used electronic health record (EHR) data from 38 Oregon clinics in the OCHIN network (originally called the Oregon Community Health Information Network, but shortened to OCHIN when membership expanded beyond Oregon) with fully operational EHRs by 2005. Each patient has a single medical record shared across all OCHIN network clinics.13 Adults (aged ≥18 years) with diabetes were identified who had ≥two primary care visits associated with an ICD-9 code for diabetes (type 1 or 2) at a study clinic before December 31, 2005, and ≥one visit for any reason in 2006 and in 2007 (to ensure a minimum of care continuity). The combined EHR and Medicaid data sets used for this study provided detailed information about each patient’s precise duration of coverage. Health insurance coverage start and stop dates from the EHR data were confirmed and supplemented for patients with Medicaid by creating linkages to Oregon’s Medicaid enrollment data; these were assessed over a 2-year study period (January 1, 2006–December 31, 2007). Patients with a Medicare start date in the EHR data were assumed to have continuous coverage after that date. Patients with any private insurance were excluded because coverage intervals could not be verified (n=521). Patients in the final study population (N=2,919) were categorized as: continuously insured (n=1,466), continuously uninsured (n=1,117), or discontinuously insured (insured for part of the period; n=336). For discontinuously insured patients, the 2-year study period was segmented into insured and uninsured intervals. The appropriate IRBs approved the study protocol.
Standard procedure codes from the EHR were used to measure hemoglobin (HbA1c) monitoring, low-density lipoprotein (LDL) screening, influenza vaccination, and nephropathy screening (urine microalbumin). Patients were classified as due for HbA1c monitoring if last receipt was >180 days prior (recommended ≥two times annually25) or >365 days prior (LDL and microalbumin; recommended annually). Patients were considered due for an influenza vaccination if a visit occurred in October–April, with no influenza vaccination recorded for that season. The dependent variable was dichotomous, indicating receipt of service due at each visit such that if all four services were needed at a visit, then that visit contributed four times in the analysis.
Statistical Analyses
Data were analyzed in 2013 using SAS Enterprise, version 5.1 (SAS Institute Inc., Cary NC). Differences in demographic characteristics between the insurance groups were tested using Kruskal-Wallis and chi-square tests. Using the approach of Song and colleagues,27 aggregate and individual measures of the odds of receiving services due at visit between insurance groups were estimated using a single covariate–adjusted generalized estimating equation (GEE) logistic model. The model included the type of service due (e.g., HbA1c, vaccination), interaction of service type, partial versus continuous insurance status, and insurance status at visit, allowing for estimation of aggregate and specific service ORs through contrast statements. Comparisons of continuously insured and uninsured were between groups. For the discontinuously insured group, comparisons were within group (i.e., uninsured versus insured periods). The specified within-patient correlation structure was compound symmetry and clinics were included as a fixed effect.26 Only services due at any given visit were included in the analysis. The following potentially confounding characteristics were controlled for: age, gender, race, ethnicity, and income below the Federal Poverty Level (FPL).
Results
Demographic characteristics of the study population and visit characteristics by insurance status are shown in Table 1.
Table 1.
Demographic characteristics of study patients and visit characteristics: overall and by public insurance coverage, 2006–2007
| DEMOGRAPHIC CHARACTERISTICS | |||||
|---|---|---|---|---|---|
| Patient Characteristics | Total | Continuously Insured | Discontinuously Insured | Continuously Uninsured | P-value between groups* |
| Total N | 2,919 | 1,466 | 336 | 1,117 | |
| Median Age, years (25th%, 75th%) | 54.9 (45.1–63.5) | 58.8 (50.2–67.5) | 54.9 (44.0–61.9) | 49.6 (40.2–57.7) | <0.0001a |
| Female, N (column %) | 1780 (61.0%) | 918 (62.6%) | 191 (58.9%) | 671 (60.0%) | 0.1077b |
| Hispanic, N (column %) | 964 (33.0%) | 166 (11.3%) | 98 (29.2%) | 700 (62.7%) | <0.0001b |
| Minority Racec, N (column %) | 430 (14.7%) | 298 (20.3%) | 50 (14.9%) | 82 (7.3%) | <0.0001b |
| <100% FPLd, N (column %) | 2285 (78.3%) | 1228 (83.8%) | 262 (78.0%) | 795 (71.2%) | <0.0001b |
| VISIT CHARACTERISTICS | |||||
|---|---|---|---|---|---|
| Visit Characteristics | Total | Continuously Insured | Discontinuously Insured | Continuously Uninsured | |
| Insured Periods | Uninsured Periods | ||||
| Visits where any service was due, N | 47,965 | 26,421 | 3,358 | 2,179 | 16,007 |
| Visits where HbA1c was due, N (% of these visits in which service was received) | 28,265 (18.5%) | 10,792 (18.6%) | 1,256 (20.7%) | 918 (15.4%) | 7,754 (18.5%) |
| Visits where LDL was due, N (% of these visits in which service was received) | 19,785 (8.2%) | 9,558 (9.0%) | 1,345 (8.0%) | 1,050 (6.5%) | 7,832 (7.6%) |
| Visits where Microalbumin was due, N (% of these visits in which service was received) | 32,847 (5.1%) | 17,976 (5.2%) | 2,382 (5.1%) | 1,593 (3.5%) | 10,896 (5.1%) |
| Visits where Flu immunization was due, N (% of these visits in which service was received) | 2,399 (9.8%) | 1,398 (11.0%) | 1,710 (8.9%) | 1,180 (7.0%) | 8,801 (8.7%) |
Source. Authors’ analysis of 2006–2007 data from 38 Oregon clinics in the OCHIN network that had fully operational electronic health records by 2005. Medicaid insurance status verified and supplemented by 2006–2007 Medicaid enrollment data.
Boldface indicates statistical significance (p<0.05).
Kruskal-Wallis test.
Chi-square test.
Minority race included patients with a designation of Black, Asian, Native American, Pacific Islander, Non-Caucasian, and “Other race.”
FPL = Federal Poverty Level
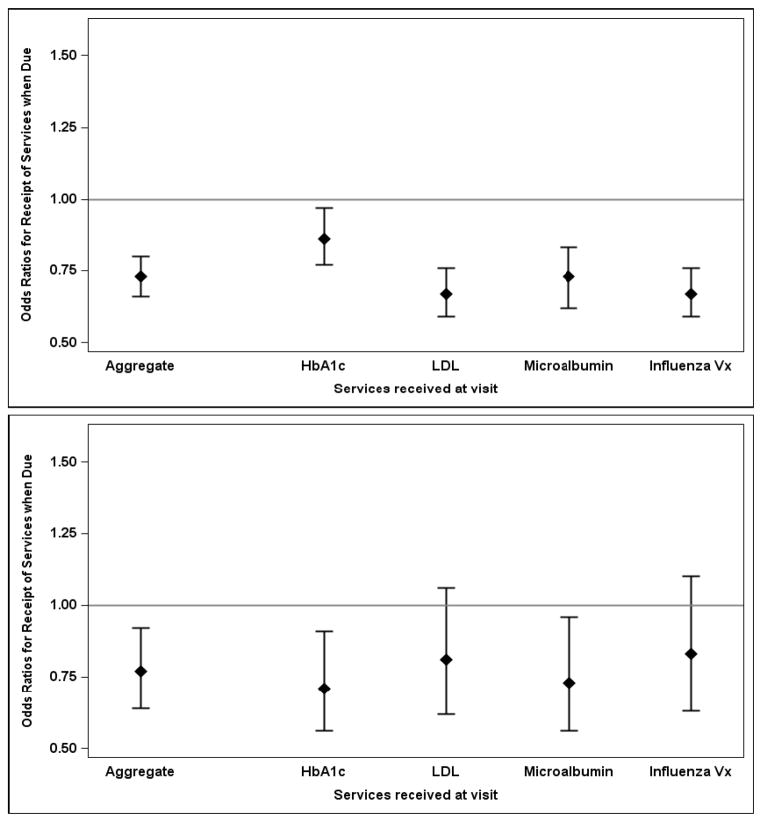
When considered in aggregate, continuously uninsured patients had lower odds of receiving services at visits when due, compared to the continuously insured (AOR=0.73, 95% CI=0.66, 0.80) (Figure 1A). When examining individual services, odds were significantly lower for all four services (HbA1c: AOR=0.86, 95% CI=0.77, 0.97; LDL: AOR=0.67, 95% CI=0.59, 0.76; microalbumin: AOR=0.73, 95% CI=0.62, 0.83; influenza vaccination: AOR=0.67, 95% CI=0.59, 0.76).
Figure 1.
Figure 1A. Odds of a patient receiving services due at the time of visit: Continuously uninsured patients vs. continuously insured patients (reference group);
Figure 1B. Odds of a discontinuously insured patient receiving services due at the time of visit: uninsured visits vs. visits when insured (reference group).
Source. 2006–2007 data from 38 Oregon clinics in the OCHIN network that had fully operational electronic health records by 2005. Medicaid insurance status verified and supplemented by 2006–2007 Oregon Medicaid enrollment data.
Notes. Diamonds represent estimated odds ratios; vertical lines represent corresponding 95% CIs. Odds ratios are estimated using a single generalized estimating equation (GEE) logistic regression of receipt of services at visits in which a service was due adjusted for fixed effects of the type of service due, clinic, gender, Hispanic ethnicity, race, age, and income below 100% of the Federal Poverty Level (FPL) ratios. Odds ratios of specific services and an aggregate measure of any service received when due are reported. HbA1c= hemoglobin A1c; LDL=low-density lipoprotein; Microalbumin=urine microalbumin; Influenza vx=influenza vaccination.
Discontinuously insured patients had lower aggregate odds of receiving services due at a visit when uninsured, compared to an insured visit (AOR=0.77, 95% CI=0.64, 0.92) (Figure 1B). Patients had lower odds of receiving HbA1c monitoring (AOR=0.71, 95% CI=0.56, 0.91) and microalbumin testing (AOR=0.73, 95% CI=0.56, 0.96) during uninsured versus insured visits. There were no statistically significant differences in receipt of LDL screening (AOR=0.81, 95% CI=0.62, 1.06) or influenza vaccination (AOR=0.83, 95% CI=0.63, 1.10) by insurance status at visit.
Discussion
Lack of health insurance is associated with poorer diabetes control.23 Previous studies suggest that this could be due to uninsured patients utilizing fewer healthcare services than insured patients.10,15,23,28 This study adds new information to help explain this disparity: even when uninsured patients use healthcare services, they are still less likely to receive recommended diabetes preventive care at a visit compared to insured patients.
There are plausible reasons for why uninsured patients receive fewer services at visits when due. Out-of-pocket costs differ for insured versus uninsured patients; previous studies found that patients who lose their insurance often postpone services until they regain coverage.6,18,29,30 There may have also been differences in the nature of the visit (i.e., acute versus preventive) or in the number of competing demands for insured patients versus uninsured patients. Future research is warranted.
Given the health complications of uncontrolled diabetes, systems similar to those implemented for childhood immunizations31 might help ensure the delivery of diabetes services during office visits. EHR-based technologies could support such system-level interventions by generating reminders about services due,32 and by alerting patients to insurance renewal dates or coverage opportunities, especially with the expanded coverage options via the Affordable Care Act.33 It is important for clinicians to know patient’s insurance status at visits, and how it might affect decisions to decline or delay services that are due.34
Limitations
These results might not generalize to privately insured patients. Services received outside of the OCHIN member clinics might have been missed; however, a previous study validated capture of diabetes preventive services in OCHIN’s EHR data.35 Patients were identified as having diabetes if they had ≥two visits associated with a diabetes code; this excluded patients who had only one diabetes-related visit. Finally, the observational design of this study prevents the ability to draw causal inferences; however, the differential pattern of service receipt observed in the discontinuously insured subgroup suggests that insurance plays a key role, as patients served as their own controls, limiting changes in other characteristics that might confound the insurance effect.
Conclusions
Lack of insurance is associated with lower probability of receiving recommended services that are due during a clinic visit. Thus, the association between being uninsured and receiving fewer preventive services may not be completely mediated by access to clinic visits.
Acknowledgments
We are grateful to OCHIN, Inc. and the participating clinics for making this research possible. We would like to acknowledge Carrie Tillotson, MPH, for her assistance with the production of Figure 1.
This study was supported by grant No. R01HL107647 from the National Heart, Lung, and Blood Institute, and grant No. K08HS021522 from the Agency for Healthcare Research and Quality. The study sponsor had no role in study design; collection, analysis, or interpretation of data; writing the report; or in the decision to submit the report for publication.
Footnotes
The authors have no potential conflicts of interest to declare.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vijan S, Stevens DL, Herman WH, Funnell MM, Standiford CJ. Screening, prevention, counseling, and treatment for the complications of type II diabetes mellitus. Putting evidence into practice. J of Gen Intern Med. 1997;12(9):567–80. doi: 10.1046/j.1525-1497.1997.07111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383–93. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 3.Harris R, Donahue K, Rathore SS, Frame P, Woolf SH, Lohr KN. Screening adults for type 2 diabetes: a review of the evidence for the U.S. Preventive Services Task Force. Ann Internal Med. 2003;138(3):215–29. doi: 10.7326/0003-4819-138-3-200302040-00015. [DOI] [PubMed] [Google Scholar]
- 4.Meier M, Hummel M. Cardiovascular disease and intensive glucose control in type 2 diabetes mellitus: moving practice toward evidence-based strategies. Vasc Health Risk Manag. 2009;5:859–71. doi: 10.2147/vhrm.s4808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Health & Human Services. AHRQ Publication No 12-0005. Rockville, MD: Agency for Healthcare Research and Quality; 2012. National Healthcare Quality Report, 2011. [Google Scholar]
- 6.Ng JH, Kaftarian SJ, Tilson WM, et al. Self-reported delays in receipt of health care among women with diabetes and cardiovascular conditions. Womens Health Issues. 2010;20(5):316–22. doi: 10.1016/j.whi.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 7.DeVoe J, Graham A, Angier H, Baez A, Krois L. Obtaining healthcare services for low-income children: a hierachy of needs. J Health Care Poor Underserved. 2008;19(4):1192–211. doi: 10.1353/hpu.0.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson JM, Shavers V. The role of health insurance coverage in cancer screening utilization. J Health Care Poor Underserved. 2008;19(3):842–56. doi: 10.1353/hpu.0.0048. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health & Human Services. AHRQ Publication No 12-0006. Rockville, MD: Agency for Healthcare Research and Quality; 2012. National Healthcare Disparities Report, 2011. [Google Scholar]
- 10.Gold R, DeVoe J, Shah A, Chauvie S. Insurance continuity and receipt of diabetes preventive care in a network of federally qualified health centers. Med Care. 2009;47(4):431–9. doi: 10.1097/mlr.0b013e318190ccac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nelson KM, Chapko MK, Reiber G, Boyko EJ. The association between health insurance coverage and diabetes care; data from the 2000 Behavioral Risk Factor Surveillance System. Health Serv Res. 2005;40(2):361–72. doi: 10.1111/j.1475-6773.2005.00361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang JX, Huang ES, Drum ML, et al. Insurance status and quality of diabetes care in community health centers. Am J Public Health. 2009;99(4):742–7. doi: 10.2105/AJPH.2007.125534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devoe JE, Gold R, Spofford M, et al. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-based Research Network (SNW-PBRN) J Am Board Fam Med. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oladele CR, Barnett E. Racial/Ethnic and social class differences in preventive care practices among persons with diabetes. BMC Public Health. 2006;6:259. doi: 10.1186/1471-2458-6-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gold R, DeVoe JE, McIntire PJ, Puro JE, Chauvie SL, Shah AR. Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage. J Am Board Fam Med. 2012;25(1):42–9. doi: 10.3122/jabfm.2012.01.110142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jerant A, Fiscella K, Tancredi DJ, Franks P. Health insurance is associated with preventive care but not personal health behaviors. J Am Board Fam Med. 2013;26(6):759–67. doi: 10.3122/jabfm.2013.06.130054. [DOI] [PubMed] [Google Scholar]
- 17.Pande AH, Ross-Degnan D, Zaslavsky AM, Salomon JA. Effects of healthcare reforms on coverage, access, and disparities: quasi-experimental analysis of evidence from Massachusetts. Am J Prev Med. 2011;41(1):1–8. doi: 10.1016/j.amepre.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Long SK, Stockley K, Grimm E, Coyer C. Medicaid and CHIP Payment and Access Commission (MACPAC Contractor Report No. 2) Washington D.C: Urban Institute; 2012. National findings on access to health care and service use for non-elderly adults enrolled in Medicaid. [Google Scholar]
- 19.Carlson MJ, Devoe J, Wrigbt BJ. Short-term impacts of coverage loss in a Medicaid population: Early results from a prospective cohort study of the Oregon Health Plan. Ann Fam Med. 2006;4(5):391–8. doi: 10.1370/afm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(1 Pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]
- 21.Kasper JD, Giovannini TA, Hoffman C. Gaining and losing health insurance: strengthening the evidence for effects on access to care and health outcomes. Med Care Res Rev. 2000;57(3):298–318. doi: 10.1177/107755870005700302. discussion 319–25. [DOI] [PubMed] [Google Scholar]
- 22.Berk ML, Schur CL. Access to care: how much difference does Medicaid make? Health Aff (Millwood) 1998;17(3):169–80. doi: 10.1377/hlthaff.17.3.169. [DOI] [PubMed] [Google Scholar]
- 23.Zhang X, Bullard KM, Gregg EW, et al. Access to health care and control of ABCs of diabetes. Diabetes Care. 2012;35(7):1566–71. doi: 10.2337/dc12-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright BJ, Carlson MJ, Edlund T, DeVoe J, Gallia C, Smith J. The impact of increased cost sharing on Medicaid enrollees. Health Aff (Millwood) 2005;24(4):1106–16. doi: 10.1377/hlthaff.24.4.1106. [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes Assocation. Standards of Medical Care-2013. Diabetes Care. 2013;36(Suppl 1):S11–66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu FB, Goldberg J, Hedeker D, Flay BR, Pentz MA. Comparison of population-averaged and subject-specific approaches for analyzing repeated binary outcomes. Am J Epidemiol. 1998;147(7):694–703. doi: 10.1093/oxfordjournals.aje.a009511. [DOI] [PubMed] [Google Scholar]
- 27.Song Z, Safran DG, Landon BE, et al. The ‘Alternative Quality Contract,’ based on a global budget, lowered medical spending and improved quality. Health Aff (Milwood) 2012;31(8):1885–94. doi: 10.1377/hlthaff.2012.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X, Geiss LS, Cheng YJ, Beckles GL, Gregg EW, Kahn HS. The missed patient with diabetes: how access to health care affects the detection of diabetes. Diabetes Care. 2008;31(9):1748–53. doi: 10.2337/dc08-0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Voorhees K, Fernald DH, Emsermann C, et al. Underinsurance in primary care: a report from the State Networks of Colorado Ambulatory Practices and Partners (SNOCAP) J Am Board Fam Med. 2008;21(4):309–16. doi: 10.3122/jabfm.2008.04.080001. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Vital signs: health insurance coverage and health care utilization --- United States, 2006–2009 and January–March 2010. MMWR Morb Mortal Wkly Rep. 2010;59(44):1448–54. [PubMed] [Google Scholar]
- 31.Hinman AR, Orenstein WA, Rodewald L. Financing immunizations in the United States. Clin Infect Dis. 2004;38(10):1440–6. doi: 10.1086/420748. [DOI] [PubMed] [Google Scholar]
- 32.Ahmad FS, Tsang T. Diabetes prevention, health information technology, and meaningful use: challenges and opportunities. Am J Prev Med. 2013;44(4 Suppl 4):S357–63. doi: 10.1016/j.amepre.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 33.DeVoe JE. Being uninsured is bad for your health: Can medical homes play a role in treating the uninsurance ailment? Ann Fam Med. 2013;11(5):473–6. doi: 10.1370/afm.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meyers DS, Mishori R, McCann J, Delgado J, O’Malley AS, Fryer E. Primary care physicians’ perceptions of the effect of insurance status on clinical decision making. Ann Fam Med. 2006;4(5):399–402. doi: 10.1370/afm.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Devoe JE, Gold R, McIntire P, Puro J, Chauvie S, Gallia CA. Electronic health records vs Medicaid claims: completeness of diabetes preventive care data in community health centers. Ann Fam Med. 2011;9(4):351–8. doi: 10.1370/afm.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]