Abstract
Objectives
1) Determine if distal femoral traction pins result in knee dysfunction in femoral or pelvic fracture patients, and 2) to determine if skeletal traction relieves pain more effectively than splinting for femoral shaft fractures.
Design
Prospective cohort trial.
Setting
Level I urban trauma center.
Patients/Participants
120 adult patients with femoral shaft, acetabular, and unstable pelvic fractures.
Intervention
Patients with femoral shaft fractures were placed into distal femoral skeletal traction or a long-leg splint, based on an attending-specific protocol. Pelvic or acetabular fracture patients with instability or intra-articular bone fragments were placed into skeletal traction.
Main Outcome Measurements
An initial Lysholm knee survey was administered to assess pre-injury knee pain and function; the survey was repeated at 3- and 6-month follow-up visits. Also, a 10-point visual analog scale (VAS) was used to document pain immediately before, during, and immediately after fracture immobilization with traction or splinting.
Results
Thirty-five patients (29%) were immobilized with a long-leg splint, and 85 (71%) were immobilized with a distal femoral traction pin. Eighty-four patients (70%) completed 6-month follow-up. Lysholm scores decreased by a mean 9.3 points from pre-injury baseline to 6 months post-injury in the entire cohort (p<0.01); no significant differences were found between the splint and traction pin groups. During application of the immobilization, VAS pain scores were significantly lower in traction patients as compared to splinted patients (mean 1.9 points less, p<0.01). Traction pins caused no infections, neurovascular injuries, or iatrogenic fractures.
Conclusions
Distal femoral skeletal traction does not result in detectable knee dysfunction at six months post-insertion, and results in less pain during and after immobilization than long-leg splinting.
Keywords: skeletal traction, preoperative fracture stabilization, long-leg splinting, Lysholm score, femoral fracture
Introduction
Distal femoral skeletal traction remains a commonly used method for preoperative fracture stabilization and pain control in patients with femoral shaft, acetabular, and unstable pelvic fractures. Up to 15% of body weight can be applied in this fashion, and the longitudinal vector of pull can improve alignment and stabilize the soft tissues, potentially aiding in resuscitation (1). In contrast to proximal tibial skeletal traction, distal femoral traction has less risk to the peroneal nerve and can be applied even if ligamentous knee instability is present. To date, no studies have evaluated whether distal femoral traction causes knee pain or dysfunction. Potential etiologies of iatrogenic knee pain from traction pin placement include heterotopic ossification within the quadriceps, scarring of the iliotibial band, violation of the articular compartment, neurovascular injury, and periosteal pain (2–4). In our experience, patients frequently perceive that persistent knee pain after skeletal traction placement is due to pin placement.
Femoral fractures are one of the most frequent injuries treated at trauma centers, and yet there is only one prospective study in the literature studying the use of traction for femoral shaft fractures (5). However, no studies have directly compared skeletal traction to long-leg splinting. Moreover, skeletal traction is also useful for acetabular and displaced pelvic fractures, and no studies have reported knee-based outcomes after traction pin use for these injuries either.
We conducted a prospective trial comparing distal femoral skeletal traction to long-leg splinting to investigate two distinct questions, both of which are central to determining if one of these immobilization methods is superior for patients with femoral shaft, acetabular, or unstable pelvic fractures. First, we hypothesized that traction pin placement would cause detectable knee pain and dysfunction, measured using the Lysholm Knee Score, due to passage of the pin through the soft tissues surrounding the knee. Second, we hypothesized that pain during and immediately after application of femoral traction would be significantly less than for long-leg splinting of femoral shaft fractures, based on our belief that more manipulation of an injured lower extremity would be needed to place an effective splint and that splinting would confer less axial fracture stability than traction.
Patients and Methods
One hundred and twenty adult patients presenting to a single level-1 trauma center with femoral shaft, acetabular, and unstable pelvic fractures were enrolled at the time of injury in a prospective cohort study. Participants were enrolled concurrently and consecutively, and informed consent was obtained in each case per institutional review board protocol.
Patients with femoral shaft fractures were placed into distal femoral skeletal traction or were placed into a long-leg splint based on attending preference and clinical circumstances. Two attending surgeons preferred more frequent use of traction pins when on call, and one surgeon preferred application of a splint more commonly, unless time to operative treatment was anticipated to be longer than 24 hours. Similarly, patients with pelvic trauma that met the traction protocol criteria of vertical pelvic ring instability, intra-articular acetabular bone fragments, or hip joint instability had distal femoral skeletal traction applied. Patients with soft-tissue injuries about the knee or peri-articular distal femur fractures were excluded from the study.
Patients were treated immediately in the emergency department and were immobilized with traction or a splint in the same fashion as if they had not consented for study participation. Those patients unable to consent at the time of stabilization, due to unconsciousness or extreme duress, were asked about their willingness for study participation as soon as they were reasonably able to provide consent.
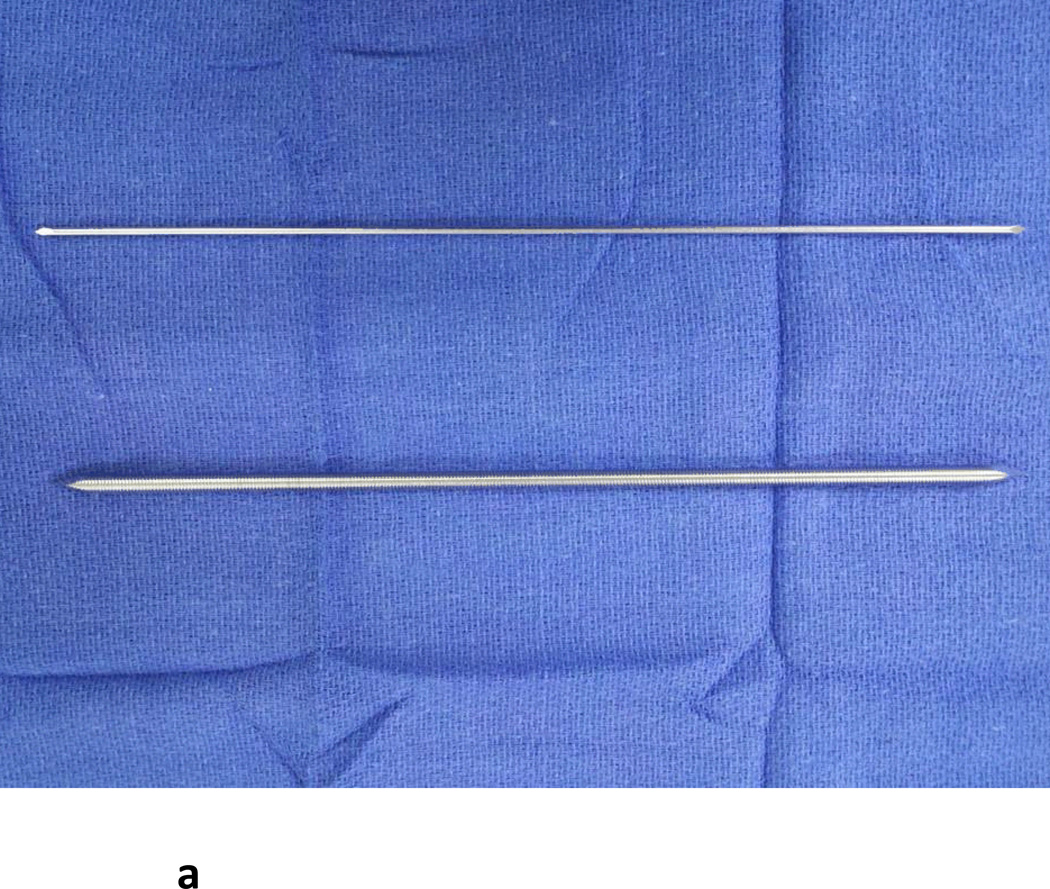
Two attending surgeons preferred use of a tensioned 2mm smooth Kirschner wire for application of traction, and one surgeon preferred use of a 4.5mm threaded Steinmann pin (Figure 1). Pins were placed from medial to lateral just proximal to the femoral condyles in the mid- to anterior femur, immediately superior to the patella. This placement location was extra-articular and avoided disruption of the collateral ligaments. Placement of traction pins was performed using a power drill after the patient had been administered local anesthetic, intravenous narcotic, and/or placed under conscious sedation. The decision for type of analgesia/anesthesia was made based on the patient’s overall condition as well as the willingness of the emergency room attending to administer conscious sedation. Those patients who were placed into long-leg splints were sometimes given conscious sedation during splint application if their level of discomfort was especially severe. Fifteen pounds of traction weight were attached from the end of the bed using a single pulley; in a minority of cases, post-traction radiographs demonstrated continued apposition of femoral fracture fragments and traction was increased to 20 pounds. Splints were applied using 5 inch wide plaster strips, including a U-based component and a posterior component. These were extended as far proximal as possible on the inner thigh and buttock and overwrapped with an ACE wrap.
Figure 1.
A) Demonstrated are a 2mm Kirschner wire (top) and a 4.5mm threaded Steinmann pin (bottom).
B) AP radiograph of knee demonstrating Kirschner wire placement.
C) AP radiograph of knee demonstrating Steinmann pin placement.
An initial Lysholm knee survey (100-point scale) was administered at the time of injury to assess pre-injury knee pain and function. Patients were specifically instructed to report their pre-injury state. If patients were unconscious or severely intoxicated, the pre-injury Lysholm score was obtained as soon as they were able to provide informed consent and enroll in the study. The Lysholm score integrated 8 components: pain, limping, locking, support, instability, swelling, stair climbing, and squatting (6). Follow-up Lysholm surveys as well as radiographs were also obtained at 3-month and 6-month follow-up visits, and patients who did not return to clinic were called to obtain their 6-month Lysholm score.
Additionally, at the time of fracture stabilization in the emergency department, patients were asked to grade their pain levels before, during, and after traction pin/splint placement using a 10-point visual analog scale (VAS), with a score of 10 being the most severe pain level. If patients were unconscious or severely intoxicated this portion of the study (Hypothesis #2) was not performed. For patients who underwent conscious sedation, VAS scores before and after immobilization were obtained but a score for pain during immobilization was not recorded.
Serial radiographs were taken preoperatively, immediately postoperatively, at 3-month follow-up, and at 6-month follow-up. Each patient’s fracture classification, concomitant injuries, comorbidities, and subsequent complications were also documented.
Table 1 includes demographic, mechanism, and injury data for the study group of 120 patients. The mean age of the cohort was 39.7 years (range 18.1–89.5), with the majority of patients less than 35 years of age (median 34.1). The most common mechanism of injury was motor vehicle collision (n=49, 40.8%). Mean time spent in preoperative traction was 1.6 days (range 0–7 days, SD 1.4). Ten subjects reported a previous injury to the involved lower extremity, and 11 had radiographic signs of osteoarthritis in the involved knee as evidenced by joint space narrowing and osteophyte formation.
Table 1.
Age, gender, injury mechanism, injury type, and previous knee status data for all subjects enrolled.
| n=120 | ||||
|---|---|---|---|---|
| mean | range | SD | ||
| Age | ||||
| 39.7 | 18.1–89.5 | 18.5 | ||
| n | % | |||
| Gender | ||||
| Male | 85 | 70.8 | ||
| Female | 35 | 29.2 | ||
| Mechanism | ||||
| MVC | 49 | 40.8 | ||
| Ground level fall | 21 | 17.5 | ||
| MCC | 11 | 9.2 | ||
| GSW | 12 | 10.0 | ||
| Pedestrian struck | 9 | 7.5 | ||
| Fall from height | 6 | 5.0 | ||
| Other motorized | 5 | 4.2 | ||
| Bicycle | 4 | 3.3 | ||
| Sports | 3 | 2.5 | ||
| Injury | ||||
| Femur shaft | 71 | 59.2 | ||
| Acetabulum | 37 | 30.8 | ||
| Pelvic ring | 7 | 5.8 | ||
| Combination | 5 | 4.2 | ||
| Open Fracture | ||||
| Yes | 3 | 2.5 | ||
| Previous Injury | ||||
| Yes | 10 | 8.3 | ||
| Previous OA | ||||
| Yes | 11 | 9.2 |
The majority of patients sustained a femoral shaft fracture (n=68, 57%). Overall, 35 subjects were immobilized with a plaster splint, 61 were immobilized with a smooth Kirschner wire, and 24 were immobilized with a threaded Steinmann pin (Table 2). The largest proportion of subjects was treated with local anesthetic alone (n=56, 47%), all of whom were placed in skeletal traction with either a smooth wire (n=38) or a threaded pin (n=18) (Table 3).
Table 2.
Summary of immobilization types for all subjects, by injury type.
| Injury | Femoral shaft | Acetabulum | Pelvic ring | Combination | ||
|---|---|---|---|---|---|---|
| Immobilization | ||||||
| Splint | 33 | 0 | 0 | 2 | 35 | |
| Smooth wire | 29 | 24 | 5 | 3 | 61 | |
| Threaded pin | 9 | 13 | 2 | 0 | 24 | |
| 71 | 37 | 7 | 5 | 120 |
Table 3.
Summary of types of analgesia used for immobilization of all fracture types.
| ER analgesia | ||
|---|---|---|
| n | % | |
| Local | 56 | 46.7 |
| IV | 22 | 18.3 |
| Local + IV | 9 | 7.5 |
| Sedation | 20 | 16.7 |
| Unknown | 13 | 10.8 |
| 120 |
An a priori power analysis indicated that 25 patients in each arm of the study (Kirschner wire, Steinmann pin, and splint) would be needed to detect a clinically significant difference (1.3 points) in VAS scores to a power of 0.8 (7). Two-tailed independent samples t-tests and one-way ANOVA were used to analyze differences in means of continuous variables between groups. Spearman’s rho was used to analyze correlation between continuous variables with non-parametric characteristics. Mann-Whitney U and Kruskal-Wallis tests were used to analyze differences in ordinal variables between and among groups. Linear regression analysis was used to evaluate independent variable contribution to final Lysholm scores and confounding, but no variables were associated with the outcome and the model predicted less than 24% of the variation in outcome. Statistical analyses were performed using a standard software package (IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY).
Results
Definitive Treatment
All patients with femoral shaft fractures were operatively treated by intramedullary nailing (66 antegrade, 5 retrograde) with distal interlocking screws. Two patients with acetabular fractures were treated non-operatively due to relatively minimal displacement of the fracture fragments on post-traction radiographs and medical comorbidities; all other acetabular fractures were treated with open reduction and internal fixation. Unstable pelvic ring injuries were treated with posterior internal fixation, with or without anterior fixation, which most often included symphyseal plating or a subcutaneous internal fixator (8).
Knee Function Scores
The mean initial Lysholm score for all patients was 91.4 (range 31–100, SD 14.9). Initial Lysholm scores were negatively correlated with age (r = −0.34, r2 = 0.12, p<0.01), with scores declining as age increased. Table 4 demonstrates differences in initial Lysholm score by pre-injury, injury, and immobilization groups (smooth pin, threaded pin, and splint). No significant differences were seen in the baseline Lysholm scores based on injury or immobilization type, but subjects with previous injury (p<0.01) and radiographic osteoarthritis (p<0.01) had significantly lower initial Lysholm scores.
Table 4.
Comparison of initial Lysholm scores across injury type, immobilization type, previous injury, previous osteoarthritis, and age.
| Initial Lysholm | n=119 | |||
|---|---|---|---|---|
| mean | st dev | range | p | |
| Injury | ||||
| Femur shaft | 92.3 | 14.1 | 32–100 | |
| Acetabulum | 88.9 | 16.9 | 31–100 | |
| Pelvic ring | 93.3 | 15.7 | 58–100 | |
| Combination | 96.2 | 8.5 | 81–100 | 0.60 |
| Immobilization | ||||
| Splint | 91.5 | 13.3 | 50–100 | |
| Smooth wire | 91.6 | 16.5 | 31–100 | |
| Threaded pin | 91.0 | 13.2 | 56–100 | 0.99 |
| Splint | 91.5 | 13.3 | 50–100 | |
| Skeletal traction | 91.4 | 15.6 | 31–100 | 0.98 |
| Previous Injury | ||||
| yes | 78.2 | 23.5 | 32–100 | |
| no | 92.7 | 13.4 | 31–100 | <0.01 |
| Previous OA | ||||
| yes | 72.2 | 25.5 | 31–100 | |
| no | 93.4 | 11.9 | 50–100 | <0.01 |
| Spearman's rho | r | r2 | p |
|---|---|---|---|
| Age: initial Lysholm | −0.344 | 0.12 | <0.01 |
Eighty-four subjects (70%) provided six-month follow-up data. The mean Lysholm score 6 months after injury was 82.2 (range=17–100, SD 19.7). There was no difference between the mean initial Lysholm scores of the subjects with 6-month follow up (91.5) compared to those lost to follow up (91.4, p=0.996). For subjects with both initial and 6-month Lysholm scores, the mean change was 9.3 (95% CI: 5.3–13.7, p<0.01). Age remained negatively correlated with initial Lysholm scores in this subgroup (r = −0.28, r2 = 0.08, p = 0.01), but was not correlated with the 6-month Lysholm score (r = −0.05, r2 < 0.00, p = 0.64). Table 5 demonstrates differences in both initial and 6-month Lysholm scores among the same pre-injury, injury, and immobilization subgroups within the cohort of 84 subjects who provided 6-month data. There were no significant differences in 6-month Lysholm scores among the immobilization groups.
Table 5.
Summary of initial and 6-month Lysholm scores compared across injury types, immobilization types, previous knee injury, previous knee osteoarthritis, and age in subjects completing 6-month follow up.
| Initial Lysholm | n=83 | 6 Months Lysholm |
n=84 | |||||
|---|---|---|---|---|---|---|---|---|
| mean | st dev | range | p | mean | st dev | range | p | |
| Injury | ||||||||
| Femur shaft | 92.7 | 11.1 | 55–100 | 84.4 | 19.2 | 24–100 | ||
| Acetabulum | 89.5 | 17.1 | 31–100 | 78.9 | 21.2 | 17–100 | ||
| Pelvic ring | 90.6 | 18.4 | 58–100 | 79.4 | 18.9 | 50–100 | ||
| Combination | 93.7 | 11.0 | 81–100 | 0.79 | 86.0 | 14.0 | 72–100 | 0.66 |
| Immobilization | ||||||||
| Splint | 89.6 | 13.0 | 55–100 | 81.1 | 22.0 | 24–100 | ||
| Smooth wire | 93.2 | 14.4 | 31–100 | 83.4 | 19.3 | 17–100 | ||
| Threaded pin | 89.3 | 13.6 | 56–100 | 0.48 | 80.4 | 18.2 | 50–100 | 0.83 |
| Splint | 89.6 | 13.0 | 55–100 | 81.1 | 22.0 | 24–100 | ||
| Skeletal traction | 92.1 | 14.1 | 31–100 | 0.47 | 82.6 | 18.9 | 17–100 | 0.77 |
| Previous Injury | ||||||||
| yes | 84.7 | 16.3 | 51–100 | 84.1 | 20.2 | 41–99 | ||
| no | 92.1 | 13.5 | 31–100 | 0.18 | 82.0 | 19.7 | 17–100 | 0.78 |
| Previous OA | ||||||||
| yes | 77.1 | 24.1 | 31–100 | 73.3 | 18.8 | 17–100 | ||
| no | 93.2 | 11.1 | 51–100 | <0.01 | 83.2 | 25.2 | 24–100 | 0.15 |
| Spearman's rho | r | r2 | p |
|---|---|---|---|
| Age: initial Lysholm | −0.28 | 0.08 | 0.01 |
| Age: 6 mos Lysholm | −0.05 | 0.00 | 0.64 |
Subgroup analysis of the 71 subjects with femur fractures in isolation is summarized in Tables 6 and 7. For the 46 subjects in this subgroup who provided 6-month follow up data, there were no differences in initial Lysholm scores based on type of immobilization. Mean initial Lysholm score (92.7), and mean 6-month Lysholm score (84.0) were significantly different (8.7, 95% CI: 2.3–15.1, p<0.01). There were no significant differences in 6-month Lysholm scores among immobilization types in the subgroup of isolated femur fractures.
Table 6.
Age, gender, injury mechanism, previous knee status, time to surgery, type of immobilization, and immobilization analgesia data for subjects with isolated femoral shaft fractures.
| Isolated Femur fxs | n=71 | |||
|---|---|---|---|---|
| mean | range | SD | ||
| Age | ||||
| 40.2 | 18.4–89.5 | 19.7 | ||
| n | % | |||
| Gender | ||||
| Male | 52 | 73.2 | ||
| Female | 19 | 26.8 | ||
| Mechanism | ||||
| MVC | 22 | 31.0 | ||
| Ground level fall | 19 | 26.7 | ||
| MCC | 6 | 8.5 | ||
| GSW | 11 | 15.5 | ||
| Pedestrian struck | 6 | 8.5 | ||
| Fall from height | 3 | 4.2 | ||
| Other motorized | 1 | 1.4 | ||
| Bicycle | 2 | 2.8 | ||
| Sports | 1 | 1.4 | ||
| Previous Injury | ||||
| Yes | 8 | 11.3 | ||
| Previous OA | ||||
| Yes | 8 | 11.3 | ||
| Time to surgery | ||||
| <24 hours | 59 | 83.1 | ||
| Immobilization | ||||
| Splint | 33 | 46.5 | ||
| Smooth wire | 29 | 40.8 | ||
| Threaded pin | 9 | 12.7 | ||
| Analgesia | ||||
| Local | 29 | 40.8 | ||
| IV | 20 | 28.2 | ||
| Local +IV | 5 | 7.0 | ||
| Sedation | 8 | 11.3 | ||
| Unknown | 9 | 12.7 |
Table 7.
Summary of mean initial and 6-month Lysholm scores by gender, previous injury, previous osteoarthritis, time to surgery, and type of immobilization.
| Isolated Femur fxs | n=71 | ||||||
|---|---|---|---|---|---|---|---|
| Initial Lysholm | 6 Months Lysholm |
||||||
| mean | st dev | p | mean | st dev | p | ||
| Gender | |||||||
| Male | 96.0 | 8.3 | 84.0 | 20.7 | |||
| Female | 82.2 | 20.6 | <0.01 | 85.8 | 13.0 | 0.79 | |
| Previous injury | |||||||
| Yes | 81.3 | 24.3 | 92.4 | 7.6 | |||
| No | 93.7 | 11.8 | 0.02 | 83.4 | 20.0 | 0.33 | |
| Previous OA | |||||||
| Yes | 76.3 | 23.8 | 78.5 | 16.7 | |||
| No | 94.3 | 11.0 | <0.01 | 85.3 | 19.6 | 0.43 | |
| Time to surgery | |||||||
| <24 hours | 94.3 | 11.0 | 82.4 | 20.5 | |||
| >24 hours | 82.7 | 22.3 | 0.01 | 92.3 | 9.3 | 0.17 | |
| Immobilization | |||||||
| Splint | 91.0 | 13.5 | 80.2 | 22.2 | |||
| Smooth wire | 94.2 | 14.9 | 88.3 | 17.2 | |||
| Threaded pin | 90.8 | 14.5 | 0.64 | 86.2 | 10.4 | 0.40 | |
| Splint | 91.0 | 13.5 | 80.2 | 22.2 | |||
| Skeletal traction | 93.4 | 14.7 | 0.48 | 87.9 | 15.9 | 0.18 |
Pain Scores
VAS scores for subjects with isolated femur fractures in the pre-immobilization, application, and post-immobilization phases were analyzed by type of immobilization. Table 8 summarizes a subanalysis of only subjects with isolated femur fractures. Again, statistically significant differences in application pain scores were seen, with the skeletal traction group as a whole (1.7 points less than splint group, p = 0.002) and the smooth wire group specifically (1.1 and 2.0 points less than threaded and splint groups, respectively, p<0.01) reporting lower scores. In this subanalysis of only subjects with femur fractures, no significant differences were seen in post-immobilization pain scores.
Table 8.
Visual analog scores compared across immobilization types for subjects with isolated femur shaft fractures.
| Pain scores, femur | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-immobilzation | Application | Post-immobilization | |||||||
| mean | st dev | p | mean | st dev | p | mean | st dev | p | |
| Kwire | 6.8 | 2.9 | 6.5 | 2.4 | 4.3 | 2.8 | |||
| Threaded | 7.7 | 2.1 | 7.6 | 2.9 | 5.4 | 1.6 | |||
| Splints | 7.7 | 2.5 | 0.40 | 8.5 | 2.6 | <0.01 | 5.6 | 2.7 | 0.19 |
| All Pins | 7.0 | 2.7 | 6.8 | 2.5 | 4.5 | 2.6 | |||
| Splints | 7.7 | 2.5 | 0.26 | 8.5 | 2.6 | <0.01 | 5.6 | 2.7 | 0.12 |
Complications
No traction pin site infections, septic arthritis, post-operative osteomyelitis about the knee, neurovascular injuries from traction pins, or iatrogenic fractures at the pin site were observed over the 6-month follow-up period.
Discussion
Our study represents the first prospective study to determine the effect of distal femoral skeletal traction on knee pain and function, both in the setting of acute fracture stabilization as well as at 6 months follow-up. In addition, this is the first study to compare skeletal traction to long-leg splinting for femoral shaft fractures in adult patients. We found that no detectable knee dysfunction existed at 6 months post-injury, rejecting our first hypothesis. We also found that traction pin placement led to significantly less patient discomfort during application compared to splint placement.
Placement of distal femoral traction pins is common in trauma centers, and while this is a technique that has been used for many decades there has been no systematic study of its relative benefits and risks. Advantages of skeletal traction include the ability to control axial femoral fracture reduction, which is not possible using long-leg splinting. Theoretically, axial traction of pelvic and lower extremity fractures improves the ease with which reduction can then be achieved during surgery, although this concept is anecdotal and has not been clearly demonstrated in the literature. Moreover, the risk of pressure sores from improper splint padding is minimized, and soft tissue injuries to the affected extremity can be more easily managed in the preoperative phase with skeletal traction than with splinting. Disadvantages of skeletal traction are that pin placement can be disconcerting for patients, traverses large soft tissue envelopes and bone, and is a theoretical risk for infection. There is also a risk of neurovascular injury to the femoral/popliteal artery, saphenous nerve, and peroneal nerve with traction pin placement about the knee (4). Finally, placing a pin across the femur creates a stress riser due to disruption of the cortices, a potential risk for iatrogenic fracture. While this has not been reported for distal femoral traction pins, it has been reported after proximal tibial pin placement (9).
Alternative methods for placing lower extremity traction include percutaneous extramedullary clamps and skin traction, although each method has potential drawbacks. Extramedullary skeletal clamps have been shown to have inferior pullout strength to a tensioned trans-femoral Kirschner wire and do not eliminate the risk of pin infection (10). Four prospective studies have compared skeletal and skin traction for femur fractures, although three of these included only hip fractures (5, 11–13). Even et al. recently compared skin and distal femoral skeletal traction for diaphyseal femoral fractures in a prospective randomized trial (5). They found no significant differences in post-traction pain relief, pain medication requirements, or intra-operative fracture reduction time between the two methods. However, time for application of skin traction was significantly faster than for skeletal traction. This study did not report incidence of cutaneous breakdown from the skin traction or pain levels during traction placement, a known potential complication of this technique (12). Also, the mean length of time patients in this study spent in traction was less than 1 day. Thus, the risk of skin compromise was low but may be higher in patients who require traction for several days due to other more serious injuries.
In our study, patients demonstrated small but significant decreases in mean Lysholm scores at 6-month follow-up compared to pre-injury condition, regardless of immobilization method used. When all traction pin patients were pooled and compared to splinted patients, there was still no significant difference in Lysholm score change. Thus we have concluded that pelvic and femoral trauma patients do have some decrease in knee function 6 months after injury, but that this is not caused by placement of a traction pin.
Lysholm scores between 95–100 are deemed excellent, 84–94 are good, 65–83 are fair, and <65 poor (14). Briggs et al. 2009 concluded that the mean Lysholm score in a large group of adult patients with no known knee pathology was 94 points, and did not correlate with either age or gender (15). Thus, our 6-month post-injury scores in the 3 immobilization groups represent fair to good knee function; compared to pre-injury scores, all patients lost approximately one functional grade, including those who were splinted. The reduced knee scores can be explained by mechanism of injury (such as dashboard injury causing hip dislocation), surgical treatment (placement of distal interlock screws for femoral intramedullary nails), referred pain from an injury about the hip or femur, or incomplete quadriceps and hamstring rehabilitation causing impaired knee strength and stability. Numerous previous studies have demonstrated persistent knee dysfunction after the types of injuries sustained by the patients in this study (16–19). Our analysis did not demonstrate that a particular injury type was predictive of greater knee dysfunction.
VAS pain scores during immobilization of isolated femur fractures were a mean 2.0 points lower in patients who were placed in skeletal traction using 2mm Kirschner wires than in those who were splinted, with strong significance. These same patients reported a mean 1.3-point improvement in post-immobilization pain control than splinted patients, although this did not reach statistical significance. These differences exceed the minimum clinically-significant change in VAS scores of 1.3 points (7), suggesting that these traction pins have a true benefit for patient comfort over splinting.
There are several limitations to this study. First, the pre-injury Lysholm scores are based on patient recollection; since these scores were obtained when the patient was initially brought into the emergency department the results are subject to recall bias. Patients possibly underestimated their pre-injury knee function since they were often in significant pain during initial stabilization. However, this is a problem faced in most prospective orthopaedic trauma studies. Also, our study design was not randomized, as we assigned patients to treatment groups based on clinical circumstances and attending preferences; therefore, selection bias was possible. However, there is no conceivable reason to think that this affected pain during pin placement or post-injury knee function. Lastly, knee function was assessed at the six-month time point, which is relatively short-term. However, the fact that traction pin patients had similar Lysholm knee scores compared to splinted patients at this time point suggests that the effects of traction pin placement on knee function have plateaued by this point. Additionally, there is no physiologic basis for potential knee function deterioration from six months onwards. Regarding the use of phone interviews to obtain some final Lysholm scores, we do not believe that the accuracy of the survey was compromised by the lack of a face-to-face interview; however, results not included in this study, such as knee range of motion, could clearly not be assessed in this fashion. Despite these weaknesses, we feel that this study adds important prospective information to the literature regarding initial management and stabilization of common orthopaedic trauma injuries.
Conclusions
We found that insertion of femoral traction pins were without complication and provided patients acute pain relief and no identifiable morbidity at 6 months. Further, we found that pain during traction pin placement was less than during application of a long-leg splint for femoral shaft fractures. A 2mm tensioned Kirschner wire produced the least pain during placement. Distal femoral traction is a safe and effective technique for preoperative pelvic, acetabular, and femoral fracture stabilization.
Acknowledgments
Ricci – Consultancy: Smith & Nephew, Biomet, Stryker Royalties: Smith & Nephew, Biomet, Stryker, Wright Medical, Lippincott Research Support: Smith & Nephew
Gardner – Consultancy: Synthes, Stryker, DGIMed, BoneSupport AB Royalties: Lippincott Research Support: Synthes
Sources of Funding:
An institutional grant from the National Institutes of Health (NIH NCATS UL1TR000448) supported the completion of this study.
Footnotes
Conflict of Interest
For the remaining authors none were declared.
Presentations:
Presented as a poster at the Annual Meeting of the Orthopaedic Trauma Association, Phoenix, Arizona, October 2013.
References
- 1.Mandrella B. The conservative treatment of femur fractures by Perkins traction. Management in adverse situations. Unfallchirurg. 2002;105:923–931. doi: 10.1007/s00113-002-0467-7. [DOI] [PubMed] [Google Scholar]
- 2.Specht LM, Gupta S, Egol KA, et al. Heterotopic ossification of the quadriceps following distal femoral traction: a report of three cases and a review of the literature. J Orthop Trauma. 2004;18:241–246. doi: 10.1097/00005131-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Althausen PL, Hak DJ. Lower extremity traction pins: indications, technique, and complications. American journal of orthopedics. 2002;31:43–47. [PubMed] [Google Scholar]
- 4.Kwon JY, Johnson CE, Appleton P, et al. Lateral femoral traction pin entry: risk to the femoral artery and other medial neurovascular structures. Journal of orthopaedic surgery and research. 2010;5:4. doi: 10.1186/1749-799X-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Even JL, Richards JE, Crosby CG, et al. Preoperative skeletal versus cutaneous traction for femoral shaft fractures treated within 24 hours. Journal of orthopaedic trauma. 2012;26:e177–e182. doi: 10.1097/BOT.0b013e31823a8dae. [DOI] [PubMed] [Google Scholar]
- 6.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985:43–49. [PubMed] [Google Scholar]
- 7.Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390–392. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 8.Gardner MJ, Mehta S, Mirza A, et al. Anterior pelvic reduction and fixation using a subcutaneous internal fixator. Journal of orthopaedic trauma. 2012;26:314–321. doi: 10.1097/BOT.0b013e318220bb22. [DOI] [PubMed] [Google Scholar]
- 9.Evans PE, Thomas WG. Tibial fracture through a traction-pin site. A report of two cases. The Journal of bone and joint surgery American volume. 1984;66:1475–1476. [PubMed] [Google Scholar]
- 10.Simonian PT, Routt ML, Harrington RM, et al. Extramedullary skeletal traction for intramedullary femoral nailing. J Orthop Trauma. 1994;8:409–413. doi: 10.1097/00005131-199410000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Resch S, Thorngren KG. Preoperative traction for hip fracture: a randomized comparison between skin and skeletal traction in 78 patients. Acta Orthop Scand. 1998;69:277–279. doi: 10.3109/17453679809000929. [DOI] [PubMed] [Google Scholar]
- 12.Saygi B, Ozkan K, Eceviz E, et al. Skin traction and placebo effect in the preoperative pain control of patients with collum and intertrochanteric femur fractures. Bulletin of the NYU hospital for joint diseases. 2010;68:15–17. [PubMed] [Google Scholar]
- 13.Finsen V, Borset M, Buvik GE, et al. Preoperative traction in patients with hip fractures. Injury. 1992;23:242–244. doi: 10.1016/s0020-1383(05)80007-5. [DOI] [PubMed] [Google Scholar]
- 14.Kocher MS, Steadman JR, Briggs KK, et al. Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am. 2004;86-A:1139–1145. doi: 10.2106/00004623-200406000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Briggs KK, Steadman JR, Hay CJ, et al. Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med. 2009;37:898–901. doi: 10.1177/0363546508330149. [DOI] [PubMed] [Google Scholar]
- 16.el Moumni M, Voogd EH, ten Duis HJ, et al. Long-term functional outcome following intramedullary nailing of femoral shaft fractures. Injury. 2012;43:1154–1158. doi: 10.1016/j.injury.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Daglar B, Gungor E, Delialioglu OM, et al. Comparison of knee function after antegrade and retrograde intramedullary nailing for diaphyseal femoral fractures: results of isokinetic evaluation. J Orthop Trauma. 2009;23:640–644. doi: 10.1097/BOT.0b013e3181a5ad33. [DOI] [PubMed] [Google Scholar]
- 18.Ricci WM, Bellabarba C, Evanoff B, et al. Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma. 2001;15:161–169. doi: 10.1097/00005131-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Kapp W, Lindsey RW, Noble PC, et al. Long-term residual musculoskeletal deficits after femoral shaft fractures treated with intramedullary nailing. The Journal of trauma. 2000;49:446–449. doi: 10.1097/00005373-200009000-00010. [DOI] [PubMed] [Google Scholar]