Abstract
Epithelial ovarian cancer (OC) is a common gynecologic malignancy in women. The standard treatment for OC is maximal cytoreductive surgical debulking followed by platinum-based chemotherapy. Despite the high response rate to primary therapy, approximately 85% of patients will develop recurrent ovarian cancer (ROC). This review identifies the clinical use of trabectedin in the treatment algorithm for ROC, with specific emphasis on platinum-sensitive ROC, for which trabectedin in combination with pegylated liposomal doxorubicin has been approved as a treatment protocol. The main mechanisms of action of trabectedin at the cellular level and in the tumor microenvironment is also discussed as bases for identifying biomarkers for selecting patients who may largely benefit from trabectedin-based therapies.
Keywords: Trabectedin, ovarian cancer, DNA repair, platinum-sensitive ovarian cancer
Epithelial ovarian cancer (OC) is a common gynecologic malignancy and the fifth most frequent cause of death by cancer in women[1]. Approximately 75% of women with OC present advanced stage disease associated with poor outcome. For these women, the standard treatment is maximal cytoreductive surgical debulking followed by platinum-based chemotherapy[2]. In spite of this, while the median survival from the diagnosis of OC has been extended to more than 4 years, the overall survival (OS) has not changed over the last 30 years[3].
Despite the 70%-80% response rates (RRs) to primary therapy, only approximately 15% of women are cured[4]. The remaining patients develop drug-sensitive disease that will ultimately become resistant and have a 5-year OS rate lower than 50%[4],[5]. Therefore, emerging drugs and treatment strategies for recurrent ovarian cancer (ROC) represent a continuous clinical challenge.
The 4th Ovarian Cancer Consensus Conference of the Gynecological Cancer InterGroup (GCIC) established the definition of platinum-free interval (PFI) as the interval from the last date of platinum administration to documented progressive disease[6]. However, the categorization of patients with ROC as platinum-resistant or platinum-sensitive, with a PFI of < 6 months and≥ 6 months, respectively, did not adequately reflect the disease prognosis because PFI constitutes a continuous variable rather than a dichotomized variable at 6 months[7]. Therefore, it was agreed that PFI should be used to subcategorize these patients (Table 1)[6],[8].
Table 1. Definition of platinum resistance according to the platinum-free interval[6],[8].
| Term | Time from last platinum treatment to relapse |
| Platinum-refractory | During platinum treatment or within 4 weeks of last administration |
| Platinum-resistant | < 6 months |
| Partially platinum-sensitive | 6 to 12 months |
| Platinum-sensitive | More than 12 months |
Patients with a fully platinum-sensitive relapse typically receive a salvage second-line therapy based on rechallenge with platinum-containing regimens with RRs ranging from 30% to 75%[9]. Among platinum-sensitive patients, those with partially platinum-sensitive disease after primary platinum-based therapy obtain substantially lower RRs to platinum rechallenge (27%-33%)[10]. Approximately 20%-40% of all OC patients had partially platinum-sensitive disease[11],[12], for whom controversies and uncertainties regarding the best post-progression treatment still exist. It has been proposed that PFI extension through intercalation of a non-platinum therapy prior to subsequent platinum rechallenge may increase the likelihood of response to a later platinum re-treatment[13], as we will review.
ROC treatment continues to evolve while new drugs with diverse mechanisms of action are introduced into the oncologist's armamentarium. This review identifies the clinical use of trabectedin in the treatment algorithm for ROC. In addition, the selection of patients who may largely benefit from trabectedin-based therapies and biomarkers is also reviewed.
Ovarian Cancer Biotypes as Bases of Directed Therapy
OC is a misleading term for a series of genomically and etiologically heterogenic diseases that often do not arise from ovarian tissue and simply share an anatomic location, resulting in different OC histotypes (i.e., mucinous, endometrioid, clear cell, and serous)[3],[14],[15]. Hence, given the complexity of OC, the current approaches of treating OC as a single disease has to move toward patient-tailored therapy based on molecular and histotype-driven treatments (biotypes). Recently, The Cancer Genome Atlas (TCGA) Research Network (http://cancergenome.nih.gov/) described an integrated analysis of the genomic and epigenomic landscapes of almost 500 high-grade serous OC patients with advanced stage disease, with the aim to identify molecular abnormalities that influence pathophysiology and outcomes and could constitute therapeutic targets[16]. This integrated analysis has definitely demonstrated the low mutation rate of high-grade OC, with the exception of the tumor protein 53 (TP53) and breast cancer genes 1 and 2 (BRCA1/2), which are affected in 96% and 22% of OC cases, respectively. In contrast, extensive focal and broad DNA losses and gains were observed through genomic analyses of OC with DNA deletions and amplifications affecting many genes. Interestingly, germline mutations in the BRCA1/2 genes are significantly associated with improved OS and overall response rate (ORR) to platinum-based chemotherapy[16]–[19]. Indeed, deficiencies in the homologous recombination pathway, which is involved in DNA repair, can disrupt the repair of DNA crosslinks introduced by platinum-based chemotherapy and other DNA-damaging agents, such as trabectedin, resulting in higher survival rates due to an improved response in BRCA-deficient patients. Furthermore, these homologous recombination deficiencies sensitize tumors for targeted therapies such as poly(ADP-ribose) polymerase (PARP) inhibitors[20] or trabectedin[21], as we will discuss later.
Trabectedin as a Therapeutic Option of Recurrent, Platinum-sensitive Ovarian Cancer
Trabectedin
Trabectedin (ecteinascidin-743, ET-743, Yondelis) is a tetrahydroisoquinoline alkaloid that was isolated from the Caribbean tunicate Ecteinaiscidia turbinate in the late 1960s and is currently produced synthetically[22]. Trabectedin consists of three fused tetrahydroisoquinoline rings referred to as subunits A, B, and C. Experimental data strongly suggest that the cytotoxic effects of trabectedin depend on its binding to the minor groove of DNA at the N2 position of guanine with some sequence specificity [23]. Subunits A and B of the drug are responsible for DNA recognition and binding, whereas subunit C protrudes out of the minor groove perpendicular to the helix axis[21]. It was suggested that the C ring interaction with nuclear proteins could account for the cytotoxic effects of trabectedin, although other trabectedin analogs lacking the C ring, such as PM00128, have biological activity superimposable to that of trabectedin[24]. Hence, the interaction between trabectedin and DNA causes an unusual DNA helix distortion, which triggers a cascade of events that interfere with several transcription factors, DNA-binding proteins, and DNA repair pathways, resulting in G2-M cell cycle arrest and ultimately apoptosis[25],[26].
Clinical development
Phase I-II trials
The initial phase I trials with trabectedin reported responses in patients with OC[27],[28]. Its further development in three phase II trials with different schedules as a single-agent treatment for OC yielded ORRs of 7% in platinum-resistant and 37% in platinum-sensitive diseases; the median progression-free survival (PFS) and overall survival (OS) were considerably longer in the platinum-sensitive setting than in the platinum-resistant setting (median PFS, 6 months vs. 2 months; median OS, 20.4 months vs. 11.1 months)[29]–[32]. The effectiveness of trabectedin treatment was highly associated with PFI, and there were no differences in the RRs compared with prior chemotherapy lines[29].
Phase III trial: OVA-301 (ClinicalTrials.gov identifier: NCT00113607).
Patients with platinum-resistant and partially platinum-sensitive disease were randomized to receive either pegylated liposomal doxorubicin (PLD) in combination with trabectedin or PLD alone, which resulted in a median PFS of 7.3 months versus 5.8 months [hazard ratio (HR) = 0.79, 95% confidence interval (CI) = 0.65-0.96, P = 0.019). This difference was maintained in the platinum-sensitive population: PFS of 9.2 months versus 7.5 months (HR = 0.73, 95% CI = 0.56-0.95, P =0.017) [33]. Based on these results, in 2009, the European Commission granted a marketing authorization for the non-platinum combination of trabectedin with PLD for the treatment of platinum-sensitive ROC. Patients recruited for the trial included those unable or unwilling to receive carboplatin due to previous toxicity or contraindications such as platinum hypersensitivity reactions. The final analysis of partially platinum-sensitive OC (214 patients representing 32% of the whole OVA-301 series) discovered a 35% risk reduction of disease progression or death that ultimately translated into a 36% reduction in the risk of death and a 6-month improvement in median OS favoring the trabectedin plus PLD combination[34],[35]. These results have been analyzed to explore post hoc the hypothesis suggesting that PFI can be artificially prolonged using a non-platinum regimen. Among 214 patients with partially platinum-sensitive disease, 121 received platinum-based therapy afterwards. Trabectedin plus PLD induced a 6-month longer median OS, with a significant 36% decrease in the risk of death compared with PLD alone (22.4 months vs. 16.4 months, HR = 0.64, P = 0.0027), most likely as a result of PFI extension (9.8 months vs. 7.9 months, HR = 0.64, P = 0.0167)[36].
Toxicity profile
Hematologic toxicities. Grade 3-4 neutropenia was fre-quent (62.7%), but neutropenic fever occurred in only 8% of treated patients. Other hematologic toxicities included grade 3-4 thrombocytopenia in 2.4% and anemia in 4.8% of patients[33].
Non-hematologic toxicities. Liver toxicity translated into elevated transaminemia [grade 3-4 serum alanine aminotransferase (ALT) elevation occurred in 30.9% of patients treated with trabecetadin plus PLD][33]. Importantly, this toxicity occurred during initial cycles and decreased in frequency afterwards[33]. Pre-medication with dexamethasone was mandatory because it reduced the frequency of this dose-limiting complication and allowed prolonged treatment duration[37]. Cardiac toxicity was low in patients treated with trabecetadin alone (1.4%), liposomal doxorubicin alone (1.8%), or in combination (3.3%)[38]. Other toxicities such as nausea (64.7%), fatigue (58.3%), and vomiting (40.1%) were usually low-grade[39]. From a practical point of view, due to its vesicant properties, trabectedin must be administered through a central venous catheter.
New directions
Based on its mechanism of action[26] and selective benefit, as shown in preclinical studies of the effect of trabectedin on BRCA1/2-deficient cells, the MITO-15 study has explored, in a non-randomized phase II trial, the efficacy of trabectedin on OC with mutated or wild-type BRCA1/2[40]. The preliminary data from this study showed an ORR of 52% for BRCA1/2-mutated OC versus 41% for wild-type BRCA1/2 OC; however, this difference was not significant (P = 0.29). We do not yet have full information on the differences between the platinum-resistant and platinum-sensitive populations.
With the encouraging clinical data showing the effective combination of non-platinum PLD and trabectedin, a new phase III trial has been launched called the INNOVATYON study (NCT01379989), is now recruiting, and will answer whether this combination is beneficial in terms of OS compared with standard carboplatin-PLD in the partially platinum-sensitive setting[35].
The new compound pharmamar (lurbinectedin, formerly PM01183), which has demonstrated its activity in platinum-resistant OC, with 22% RR, will be launched in a phase III trial to assess its efficacy[41].
DNA Damage and Predictive Biomarkers for Trabectedin
Nucleotide excision repair (NER) is the primary mechanism known to remove platinum-DNA adducts (including cisplatin-induced intra-strand crosslinks) from DNA[42], thus increasing resistance to the drug. NER is composed of two subpathways for DNA damage detection: 1) global genome NER, which maintains the integrity of the entire genome, and 2) transcription-coupled NER, which accounts for removal of damage in the transcribed strands of active genes. Impaired NER activity is associated with several rare autosomal-recessively photosensitive diseases, including xeroderma pigmentosum (XP), Cokayne syndrome, and trichothiodystrophy [43]. NER factors are also mutated in some human cancers, including ovarian tumors[44], and can therefore contribute to clinical resistance to platinum derivates[42].
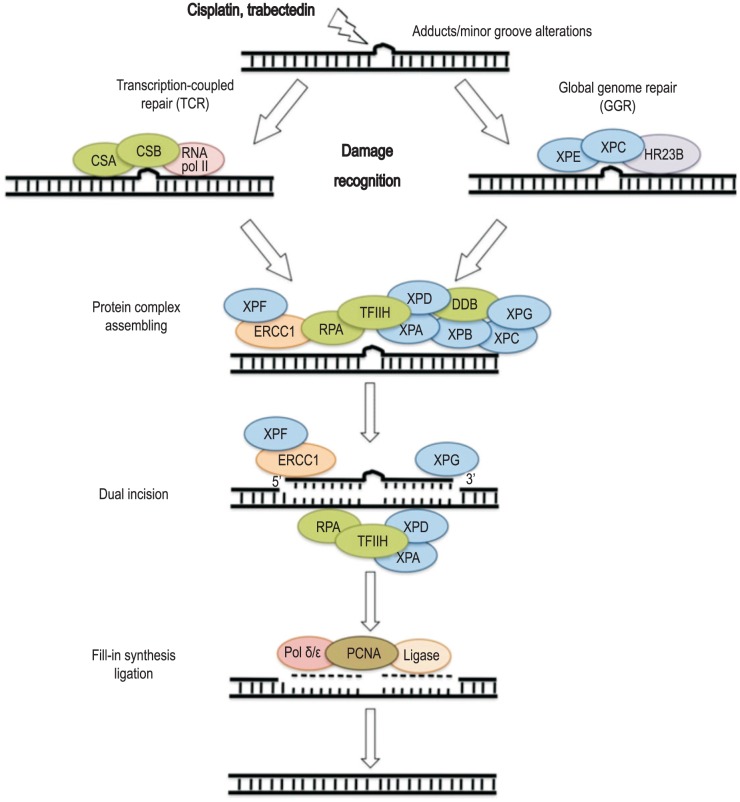
Global genome NER and transcription-coupled NER are comparable in terms of mechanism, except for the initial damage-recognition step[43]. In global genome NER, helix-distorting base lesions are identified by xeroderma pigmentosum group C and RAD23 yeast, homolog of B proteins (XPC-hHR23B). In transcription-coupled NER, elongating RNA polymerase II encounters the lesion and recruits the Cokayne syndrome factors CSA and CSB. Subsequent stages of the two subpathways are the same. Transcription factor II human (TFIIH) is composed of xeroderma pigmentosum complementation group B (XPB) and D (XPD) subunits, which are helicase components that catalyze ATP-dependent unwinding of the DNA strands. XPA and replication protein A stabilize the open complex and position the other factors. Dual incision is then performed by the excision repair cross-complementation group 1 (ERCC1)-XPF and XPG endonucleases, which cleave the damaged strand 5′ and 3′ of the lesion, respectively. Finally, NER is completed by gap-filling DNA synthesis, followed by strand ligation (Figure 1) [45].
Figure 1. Nucleotide excision repair (NER) mechanism.
NER is a particularly important mechanism by which the cell can prevent unwanted mutations by removing the vast majority of DNA damage that is produced by platinum-based therapies such as trabectedin. The recognition of these distortions leads to the removal of a short single-strand DNA segment that includes the lesion, creating a single-strand gap in the DNA that is subsequently filled in by DNA polymerase by using the undamaged strand as a template. NER can be divided into two subpathways (global genomic NER and transcription-coupled NER), which differ only in their recognition of helix-distorting DNA damage (see the text for details). CSA, Cockayne syndrome A; XPE, xeroderma pigmentosum, complementation group E; HR23B, RAD23 yeast, homolog B; ERCC1, excision repair cross-complementation group 1; RPA, human replication protein; TFIIH, transcription factor II human; DDB, damaged DNA-binding protein; PCNA, proliferating cell nuclear antigen.
As for all platinum-based drugs, DNA distortion produced by trabectedin is a substrate for the NER pathway; however, the mechanism by which trabectedin interacts with DNA and exerts its antitumor activity is different from those of cisplatin. Cisplatin binds to the N7 position of guanine in the major groove of DNA[42], whereas trabectedin, as previously mentioned, forms monoadducts at the N2 position of guanine in the minor groove of DNA, forcing the minor groove toward the major groove and allowing possible interactions between the C-ring portion of the drug and NER factors[23],[25]. Initial studies revealed a unique pattern of sensitivity to the drug in cells with defects in the NER machinery[46]–[49]. It has in fact been reported that NER-deficient cells are significantly less sensitive to trabectedin (from 2- to 8-fold) than NER-proficient cells. This is unusual, intriguing, and somewhat paradoxical, as a deficiency in NER is generally associated with increased sensitivity to DNA-interacting agents[50]. The formation of lethal single-strand DNA breaks was reported to be related to a functional transcription-coupled NER pathway [49],[51]. Soares et al.[52] performed an in vitro study and suggested that the action of trabectedin in eukaryotic cells might be the result of NER inactivation through the formation of an inactive XPG/DNA/trabectedin ternary complex, which conveyed the idea that NER components may represent the primary targets of the drug. In this regard, using a reverse-phase lysate microarray platform, Stevens et al.[53] demonstrated, in a series of tumor cell lines, that XPF and XPG showed the highest negative correlations with drug activity across all three tissue-of-origin groups (colon cancer, OC, and XP cell lines). Furthermore, the increased XPF and XPG protein levels were directly correlated with trabectedin sensitivity and cisplatin resistance, as previously reported[48],[54]. Despite this finding, the authors concluded that it is difficult to identify a single NER biomarker to predict drug sensitivity and that the heterogeneity of tumors and the influence of NER-independent pathways probably contribute to this complexity.
It has been shown that trabectedin-induced DNA damage requires double-strand base (DSB) repair, suggesting a pivotal role of this pathway in drug-induced cytotoxicity[52]. Hence, the homologous recombination repair of DSBs is also critical for modulating the cellular response to trabectedin in homologous recombination-deficient cells displaying hypersensitivity to the drug[21],[52]. In the proposed model, the trabectedin adducts in the minor groove are recognized by the NER system, particularly by the XPG protein. The catalytic endonuclease activity of XPG was found to be dispensable, but its C-terminal region was essential for the formation of “cytotoxic complexes” that, during the S phase, gave rise to DSB lesions that had to be repaired by homologous recombination. Cells lacking the homologous recombination pathway are indeed extremely sensitive to the drug, with a decrease in the 50% inhibition concentration (IC50) by approximately 100 folds[21]. In addition, complementation of the defects almost completely reverts the sensitivity to the normal control level, strongly suggesting that homologous recombination is a key determinant for repairing trabectedin-induced lesions[21].
Trabectedin treatment induces the formation of both phosphorylated histone H2AX (g-H2AX) and Rad51 foci in NER-proficient cells, suggesting that the DSBs in DNA are tentatively repaired by the induction of Rad51 foci. Both events are much less evident in a NER-deficient background, suggesting that, in the presence of trabectedin, the NER pathway is responsible for the incision/excision of the DNA lesion, leading to the formation of DSBs[21]. In addition, the induction of g-H2AX phosphorylation is much more evident in the S phase of the cell cycle, corroborating the hypothesis of a strict requirement for DNA synthesis in the formation of trabectedin-induced DSBs[52]. The fact that a clear-cut induction of g-H2AX phosphorylation and Rad51 focus formation is observed only in NER-proficient cells can be explained in light of the experiments performed by Tavecchio et al. [21] in S. pombe, where the formation and stabilization of a ternary complex among DNA-bound trabectedin and the Rad13 carboxy-terminal region was responsible for the toxicity of the drug. This suggests that the NER proficiency leads to the accumulation of unprocessed single-strand bases (SSBs) that can be converted to DSBs in the S phase. In contrast, the inability of NER-deficient cells to efficiently induce Rad51 foci appears to have a protective role when cells are treated with trabectedin[21].
The accumulating evidence of the existence of a subset of tu-mors with specific defects in the homologous recombination DNA repair pathway, the so-called BRCAness phenotype[55],[56], clearly suggest that patients whose tumors harbor those specific defects should benefit more from a trabectedin-based therapy.
In an attempt to clarify these observations, Monk et al. [57] evaluated the role of 13 proteins, which are involved in cell proliferation (Ki67), cell cycle checkpoint signaling [P53, ataxia telangiectasia mutated (ATM), checkpoint kinase 1 (CHK1), and CHK2], and DNA repair [BRCA1, BRCA2, DNA-PK, excision-repair complementing defective in Chinese hamster 1 (ERCC1), Fanconi anemia complementation group D2 (FANCD2), Nibrin, Rad50, and XPA], as potential predictive biomarkers in patients with advanced OC using the OVA-301 phase III trial series as the study population. The authors found that low protein expression of Nibrin was statistically associated with better clinical outcome (higher ORR in univariate analysis as well as longer PFS and OS in both univariate and multivariate analyses). Nibrin also showed a high predictive value for treatment outcome in patients with platinum-sensitive disease and in those who were treated with trabectedin plus PDL, but not in those treated with PDL alone.
Nibrin is a 754-amino acid polypeptide involved in the recognition and repair of DSBs[58]. This protein interacts with meiotic recombination 11 (MRE11) and RAD50 homolog (RAD50) to form the Mre11-Rad50-Nibrin (MRN) complex and is required for translocating this complex to the sites of DSBs[58]. The MRN complex plays a crucial role as a sensor of DSBs, in activating the signal transduction cascades that lead to cell cycle checkpoints and in regulating the DNA repair pathway selection.
Other Action Modes of Trabectedin
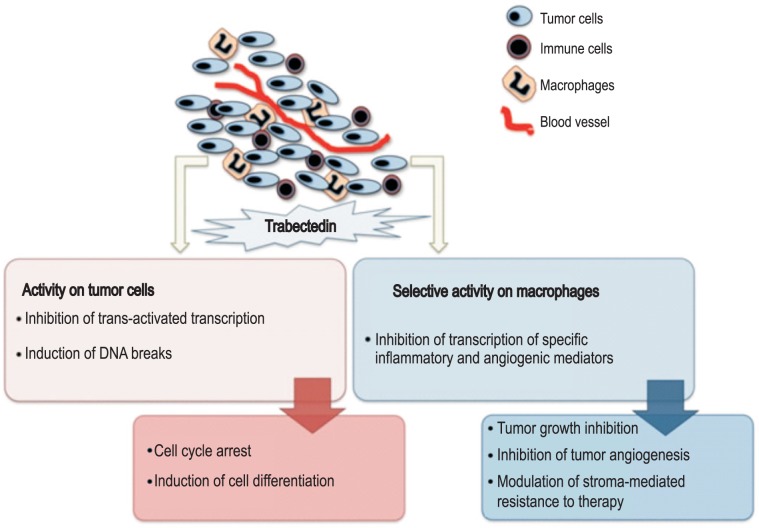
From the beginning of its development, trabectedin has shown some peculiar properties that clearly distinguish it from other anticancer drugs. Trabectedin not only induces DNA damage, as already discussed, but also directly inhibits growth, induces cell death and differentiation of malignant cells, and affects the tumor microenvironment by reducing the production of key inflammatory mediators[26],[59]–[61] (Figure 2).
Figure 2. Mechanisms of action and biological effects of trabectedin on cancer cells and the tumor microenvironment.
It has been reported that trabectedin affects gene transcription through different mechanisms. First, trabectedin prevents the binding of transcription factors to DNA[62]. Second, the DNA adducts formed by trabectedin functionally mimic an inter-strand crosslinking lesion, which blocks transcription by stabilizing double-strand DNA[63]. Finally, trabectedin directly interacts with the elongating Pol II, regardless of the strands in which they are located[63].
In addition to its transcriptional action, trabectedin has selective anti-inflammatory and immunomodulatory properties on monocytes and tumor-associated macrophages (TAMs), and it inhibits the production of factors potentially relevant for tumor growth, tumor progression, and the inhibition of tumor-promoted angiogenesis. Indeed, trabectedin also targets inflammatory cells in the tumor microenvironment to reduce the angiogenic and pro-inflammatory effects mediated by cytokines, thus leading to a delayed response with prolonged stabilization (i.e., tumor dormancy). For example, trabectedin treatment down-regulates the expression of interleukine-6 (IL-6), chemokine (C-C motif) ligand 2 (CCL2), chemokine (C-X-C motif) ligand 8 (CXCL8), angiopoietin-2, and vascular endothelial growth factor (VEGF), but not other biological mediators such as the tumor necrosis factor alpha (TNFα)[61],[64]. The anti-inflammatory effects of trabectedin were confirmed in different tumor xenograft models and in human soft-tissue sarcoma samples from patients receiving trabectedin as neoadjuvant therapy[60].
Hence and overall, trabectedin is probably more than a cytotoxic drug, given that its antitumor activity arises from different combinations that act through more than one mechanism, and provides a consolidated therapeutic approach as a multitarget drug with far more multifaceted activity than initially formulated. Through these mechanisms, trabectedin is likely to impact relevant biological pathways involved in cancer, which may influence disease outcome.
Conclusions
Treatment of ROC currently constitutes a continuous clinical challenge. Considering the histological heterogeneity, distinct genetic abnormalities, and treatment responses of OC, individualized drug selection is essential for the successful targeted treatment of specific groups of patients. Furthermore, effective consolidation or maintenance treatment with new drugs with acceptable non-cumulative toxicity to reduce the risk of recurrence after a clinical response and improve survival probably will have a great impact in ROC treatment. In this sense, the OVA-301 study has demonstrated the superiority of trabectedin plus PLD over PLD alone in the overall population of patients, with striking differences in outcomes in patients with platinum-sensitive disease and in the subset of patients with a PFI of 6–12 months and a median OS prolonged by 6 months. The clinical activity of this combination has been documented to exhibit comparable activity to platinum combinations among platinum-sensitive patients; hence, the combination of trabectedin plus PLD may now represent an acceptable, non-platinum/non-taxane alternative for treating patients with platinum-sensitive relapse, particularly for patients with partially platinum-sensitive disease who can benefit from a delay in platinum re-treatment, patients with platinum-sensitive relapse suffering from platinum-induced toxicities or hypersensitivity, and patients who have received more than one platinum-based chemotherapy.
Trabectedin causes distortions in DNA, promoting DNA damage that is recognized by the NER and homologous recombination DNA repair machineries. Some evidence has suggested the existence of tumors with defects in elements from these DNA repair complexes, which clearly suggests that patients whose tumors harbor these specific defects should benefit more from a trabectedin-based therapy. Several efforts have been performed to define the biomarkers able to identify this population. In this sense and although a larger series of studies must be completed for validation, the Nibrin protein constitutes a promising candidate biomarker. Low expression levels of Nibrin seem to be an independent prognostic or predictive factor of outcome in patients with OC, particularly in those with platinum-sensitive disease and in those treated with trabectedin plus PLD.
Finally, trabectedin has other mechanisms of action, including direct effects on cancer cells as well as host-modulating properties (including inflammation and immune response) that appear to be of great importance for its therapeutic effect. A deeper understanding of these mechanisms will allow for the design of more effective drug combinations.
References
- 1.Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.Heintz AP, Odicino F, Maisonneuve P, et al. Carcinoma of the ovary. FIGO 26th annual report on the results of treatment in gynecological cancer. Int J Gynaecol Obstet. 2006;95(Suppl 1):S161–S192. doi: 10.1016/S0020-7292(06)60033-7. [DOI] [PubMed] [Google Scholar]
- 3.Vaughan S, Coward JI, Bast RC, Jr, et al. Rethinking ovarian cancer: recommendations for improving outcomes. Nat Rev Cancer. 2011;11:719–725. doi: 10.1038/nrc3144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colombo N, Van Gorp T, Parma G, et al. Ovarian cancer. Crit Rev Oncol Hematol. 2006;60:159–179. doi: 10.1016/j.critrevonc.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong DK. Relapsed ovarian cancer: challenges and management strategies for a chronic disease. Oncologist. 2002;7(Suppl 5):20–28. doi: 10.1634/theoncologist.7-suppl_5-20. [DOI] [PubMed] [Google Scholar]
- 6.Stuart GC, Kitchener H, Bacon M, et al. 2010 Gynecologic Cancer InterGroup (GCIG) consensus statement on clinical trials in ovarian cancer: report from the Fourth Ovarian Cancer Consensus Conference. Int J Gynecol Cancer. 2011;21:750–755. doi: 10.1097/IGC.0b013e31821b2568. [DOI] [PubMed] [Google Scholar]
- 7.Friedlander M, Trimble E, Tinker A, et al. Clinical trials in recurrent ovarian cancer. Int J Gynecol Cancer. 2011;21:771–775. doi: 10.1097/IGC.0b013e31821bb8aa. [DOI] [PubMed] [Google Scholar]
- 8.Pujade-Lauraine E. How to approach patients in relapse. Ann Oncol. 2012;23(Suppl 10):x128–x131. doi: 10.1093/annonc/mds358. [DOI] [PubMed] [Google Scholar]
- 9.Hall M, Rustin G. Recurrent ovarian cancer: when and how to treat. Curr Oncol Rep. 2011;13:459–471. doi: 10.1007/s11912-011-0199-3. [DOI] [PubMed] [Google Scholar]
- 10.Colombo N, Gore M. Treatment of recurrent ovarian cancer relapsing 6-12 months post platinum-based chemotherapy. Crit Rev Oncol Hematol. 2007;64:129–138. doi: 10.1016/j.critrevonc.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Parmar MK, Ledermann JA, Colombo N, et al. Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: The ICON4/AGO-OVAR-2.2 trial. Lancet. 2003;361:2099–2106. doi: 10.1016/s0140-6736(03)13718-x. [DOI] [PubMed] [Google Scholar]
- 12.Pujade-Lauraine E, Wagner U, Aavall-Lundqvist E, et al. Pegylated liposomal doxorubicin and carboplatin compared with paclitaxel and carboplatin for patients with platinum-sensitive ovarian cancer in late relapse. J Clin Oncol. 2010;28:3323–3329. doi: 10.1200/JCO.2009.25.7519. [DOI] [PubMed] [Google Scholar]
- 13.Monk BJ, Coleman RL. Changing the paradigm in the treatment of platinum-sensitive recurrent ovarian cancer: from platinum doublets to nonplatinum doublets and adding antiangiogenesis compounds. Int J Gynecol Cancer. 2009;19(Suppl 2):S63–S67. doi: 10.1111/IGC.0b013e3181c104fa. [DOI] [PubMed] [Google Scholar]
- 14.Bast RC, Jr, Hennessy B, Mills GB. The biology of ovarian cancer: new opportunities for translation. Nat Rev Cancer. 2009;9:415–428. doi: 10.1038/nrc2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romero I, Sun CC, Wong KK, et al. Low-grade serous carcinoma: new concepts and emerging therapies. Gynecol Oncol. 2013;130:660–666. doi: 10.1016/j.ygyno.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 16.Cancer Genome Atlas Research Network Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang D, Khan S, Sun Y, et al. Association of BRCA1 and BRCA2 mutations with survival, chemotherapy sensitivity, and gene mutator phenotype in patients with ovarian cancer. JAMA. 2011;306:1557–1565. doi: 10.1001/jama.2011.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Majdak EJ, Debniak J, Milczek T, et al. Prognostic impact of BRCA1 pathogenic and BRCA1/BRCA2 unclassified variant mutations in patients with ovarian carcinoma. Cancer. 2005;104:1004–1012. doi: 10.1002/cncr.21276. [DOI] [PubMed] [Google Scholar]
- 19.Bolton KL, Chenevix-Trench G, Goh C, et al. Association between BRCA1 and BRCA2 mutations and survival in women with invasive epithelial ovarian cancer. JAMA. 2012;307:382–390. doi: 10.1001/jama.2012.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varga D, Deniz M, Schwentner L, et al. Ovarian cancer: in search of better marker systems based on DNA repair defects. Int J Mol Sci. 2013;14:640–673. doi: 10.3390/ijms14010640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tavecchio M, Simone M, Erba E, et al. Role of homologous recombination in trabectedin-induced DNA damage. Eur J Cancer. 2008;44:609–618. doi: 10.1016/j.ejca.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Cuevas C, Francesch A. Development of Yondelis (trabectedin, ET-743). A semisynthetic process solves the supply problem. Nat Prod Rep. 2009;26:322–337. doi: 10.1039/b808331m. [DOI] [PubMed] [Google Scholar]
- 23.Pommier Y, Kohlhagen G, Bailly C, et al. DNA sequence- and structure-selective alkylation of guanine N2 in the DNA minor groove by ecteinascidin 743, a potent antitumor compound from the Caribbean tunicate Ecteinascidia turbinata. Biochemistry. 1996;35:13303–13309. doi: 10.1021/bi960306b. [DOI] [PubMed] [Google Scholar]
- 24.Erba E, Cavallaro E, Damia G, et al. The unique biological features of the marine product Yondelis (ET-743, trabectedin) are shared by its analog ET-637, which lacks the C ring. Oncol Res. 2004;14:579–587. doi: 10.3727/0965040042707925. [DOI] [PubMed] [Google Scholar]
- 25.Zewail-Foote M, Hurley LH. Ecteinascidin 743: a minor groove alkylator that bends DNA toward the major groove. J Med Chem. 1999;42:2493–2497. doi: 10.1021/jm990241l. [DOI] [PubMed] [Google Scholar]
- 26.D'Incalci M, Galmarini CM. A review of trabectedin (ET-743): a unique mechanism of action. Mol Cancer Ther. 2010;9:2157–2163. doi: 10.1158/1535-7163.MCT-10-0263. [DOI] [PubMed] [Google Scholar]
- 27.Pardo B, Salazar R, Ciruelos E, et al. Phase I and pharmacokinetic study of trabectedin 3-hour infusion every three weeks in patients with advanced cancer and alteration of hepatic function. Med Oncol. 2012;29:2240–2250. doi: 10.1007/s12032-011-9979-8. [DOI] [PubMed] [Google Scholar]
- 28.Vidal L, Magem M, Barlow C, et al. Phase I clinical and pharmacokinetic study of trabectedin and carboplatin in patients with advanced solid tumors. Invest New Drugs. 2012;30:616–628. doi: 10.1007/s10637-010-9559-3. [DOI] [PubMed] [Google Scholar]
- 29.del Campo JM, Sessa C, Krasner CN, et al. Trabectedin as single agent in relapsed advanced ovarian cancer: results from a retrospective pooled analysis of three phase II trials. Med Oncol. 2013;30:435. doi: 10.1007/s12032-012-0435-1. [DOI] [PubMed] [Google Scholar]
- 30.Sessa C, De Braud F, Perotti A, et al. Trabectedin for women with ovarian carcinoma after treatment with platinum and taxanes fails. J Clin Oncol. 2005;23:1867–1874. doi: 10.1200/JCO.2005.09.032. [DOI] [PubMed] [Google Scholar]
- 31.Krasner CN, McMeekin DS, Chan S, et al. A phase II study of trabectedin single agent in patients with recurrent ovarian cancer previously treated with platinum-based regimens. Br J Cancer. 2007;97:1618–1624. doi: 10.1038/sj.bjc.6604088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Del Campo JM, Roszak A, Bidzinski M, et al. Phase II randomized study of trabectedin given as two different every 3 weeks dose schedules (1.5 mg/m2 24 h or 1.3 mg/m2 3 h) to patients with relapsed, platinum-sensitive, advanced ovarian cancer. Ann Oncol. 2009;20:1794–1802. doi: 10.1093/annonc/mdp198. [DOI] [PubMed] [Google Scholar]
- 33.Monk BJ, Herzog TJ, Kaye SB, et al. Trabectedin plus pegylated liposomal doxorubicin in recurrent ovarian cancer. J Clin Oncol. 2010;28:3107–3114. doi: 10.1200/JCO.2009.25.4037. [DOI] [PubMed] [Google Scholar]
- 34.Monk BJ, Herzog TJ, Kaye SB, et al. Trabectedin plus pegylated liposomal doxorubicin (PLD) versus PLD in recurrent ovarian cancer: overall survival analysis. Eur J Cancer. 2012;48:2361–2368. doi: 10.1016/j.ejca.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Poveda A, Ray-Coquard I, Romero I, et al. Emerging treatment strategies in recurrent platinum-sensitive ovarian cancer: focus on trabectedin. Cancer Treat Rev. 2014;40:366–375. doi: 10.1016/j.ctrv.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Poveda A, Vergote I, Tjulandin S, et al. Trabectedin plus pegylated liposomal doxorubicin in relapsed ovarian cancer: outcomes in the partially platinum-sensitive (platinum-free interval 6-12 months) subpopulation of OVA-301 phase III randomized trial. Ann Oncol. 2011;22:39–48. doi: 10.1093/annonc/mdq352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donald S, Verschoyle RD, Greaves P, et al. Complete protection by high-dose dexamethasone against the hepatotoxicity of the novel antitumor drug Yondelis (ET-743) in the rat. Cancer Res. 2003;63:5902–5908. [PubMed] [Google Scholar]
- 38.Lebedinsky C, Gomez J, Park YC, et al. Trabectedin has a low cardiac risk profile: a comprehensive cardiac safety analysis. Cancer Chemother Pharmacol. 2011;68:1223–1231. doi: 10.1007/s00280-011-1614-z. [DOI] [PubMed] [Google Scholar]
- 39.Le Cesne A, Yovine A, Blay JY, et al. A retrospective pooled analysis of trabectedin safety in 1,132 patients with solid tumors treated in phase II clinical trials. Invest New Drugs. 2012;30:1193–1202. doi: 10.1007/s10637-011-9662-0. [DOI] [PubMed] [Google Scholar]
- 40.Lorusso D, Ferrandina G, Pignata S, et al. Trabectedin in patients with BRCA mutated and BRCAness phenotype advanced ovarian cancer (AOC): phase II prospective MITO-15 study. Ann Oncol. 2014;25:iv309. doi: 10.1093/annonc/mdv608. [DOI] [PubMed] [Google Scholar]
- 41.Poveda A, Berton-Rigaud D, Laure Ray-Coquard I, et al. Lurbinectedin (PM01183), an active compound in platinum-resistant/refractory ovarian cancer (PRROC) patients: results of a two-stage, controlled phase II study. J Clin Oncol. 2014;32:abstr 5505. [Google Scholar]
- 42.Kelland L. The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer. 2007;7:573–584. doi: 10.1038/nrc2167. [DOI] [PubMed] [Google Scholar]
- 43.Hoeijmakers JH. Genome maintenance mechanisms for preventing cancer. Nature. 2001;411:366–374. doi: 10.1038/35077232. [DOI] [PubMed] [Google Scholar]
- 44.Takebayashi Y, Nakayama K, Kanzaki A, et al. Loss of heterozy-gosity of nucleotide excision repair factors in sporadic ovarian, colon and lung carcinomas: implication for their roles of carcinogenesis in human solid tumors. Cancer Lett. 2001;174:115–125. doi: 10.1016/s0304-3835(01)00690-5. [DOI] [PubMed] [Google Scholar]
- 45.Fu D, Calvo JA, Samson LD. Balancing repair and tolerance of DNA damage caused by alkylating agents. Nat Rev Cancer. 2012;12:104–120. doi: 10.1038/nrc3185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Damia G, Silvestri S, Carrassa L, et al. Unique pattern of ET-743 activity in different cellular systems with defined deficiencies in DNA-repair pathways. Int J Cancer. 2001;92:583–588. doi: 10.1002/ijc.1221. [DOI] [PubMed] [Google Scholar]
- 47.Erba E, Bergamaschi D, Bassano L, et al. Ecteinascidin-743 (ET-743), a natural marine compound, with a unique mechanism of action. Eur J Cancer. 2001;37:97–105. doi: 10.1016/s0959-8049(00)00357-9. [DOI] [PubMed] [Google Scholar]
- 48.Takebayashi Y, Pourquier P, Zimonjic DB, et al. Antiproliferative activity of ecteinascidin 743 is dependent upon transcription-coupled nucleotide-excision repair. Nat Med. 2001;7:961–966. doi: 10.1038/91008. [DOI] [PubMed] [Google Scholar]
- 49.Soares DG, Poletto NP, Bonatto D, et al. Low cytotoxicity of ecteinascidin 743 in yeast lacking the major endonucleolytic enzymes of base and nucleotide excision repair pathways. Biochem Pharmacol. 2005;70:59–69. doi: 10.1016/j.bcp.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 50.Damia G, Imperatori L, Stefanini M, et al. Sensitivity of cho mutant cell lines with specific defects in nucleotide excision repair to different anti-cancer agents. Int J Cancer. 1996;66:779–783. doi: 10.1002/(SICI)1097-0215(19960611)66:6<779::AID-IJC12>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 51.Herrero AB, Martin-Castellanos C, Marco E, et al. Cross-talk between nucleotide excision and homologous recombination DNA repair pathways in the mechanism of action of antitumor trabectedin. Cancer Res. 2006;66:8155–8162. doi: 10.1158/0008-5472.CAN-06-0179. [DOI] [PubMed] [Google Scholar]
- 52.Soares DG, Escargueil AE, Poindessous V, et al. Replication and homologous recombination repair regulate DNA double-strand break formation by the antitumor alkylator ecteinascidin 743. Proc Natl Acad Sci U S A. 2007;104:13062–13067. doi: 10.1073/pnas.0609877104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stevens EV, Nishizuka S, Antony S, et al. Predicting cisplatin and trabectedin drug sensitivity in ovarian and colon cancers. Mol Cancer Ther. 2008;7:10–18. doi: 10.1158/1535-7163.MCT-07-0192. [DOI] [PubMed] [Google Scholar]
- 54.Furuta T, Ueda T, Aune G, et al. Transcription-coupled nucleotide excision repair as a determinant of cisplatin sensitivity of human cells. Cancer Res. 2002;62:4899–4902. [PubMed] [Google Scholar]
- 55.Turner N, Tutt A, Ashworth A. Hallmarks of ‘BRCAness’ in sporadic cancers. Nat Rev Cancer. 2004;4:814–819. doi: 10.1038/nrc1457. [DOI] [PubMed] [Google Scholar]
- 56.Lord CJ, Garrett MD, Ashworth A. Targeting the double-strand DNA break repair pathway as a therapeutic strategy. Clin Cancer Res. 2006;12:4463–4468. doi: 10.1158/1078-0432.CCR-06-1269. [DOI] [PubMed] [Google Scholar]
- 57.Monk BJ, Kaye SB, Poveda A, et al. Nibrin is a marker of clinical outcome in patients with advanced serous ovarian cancer treated in the phase III OVA-301 trial. Gynecol Oncol. 2014;132:176–180. doi: 10.1016/j.ygyno.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 58.Stracker TH, Petrini JH. The MRE11 complex: starting from the ends. Nat Rev Mol Cell Biol. 2011;12:90–103. doi: 10.1038/nrm3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.D'Incalci M, Badri N, Galmarini CM, et al. Trabectedin, a drug acting on both cancer cells and the tumour microenvironment. Br J Cancer. 2014;111:646–650. doi: 10.1038/bjc.2014.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Germano G, Frapolli R, Belgiovine C, et al. Role of macrophage targeting in the antitumor activity of trabectedin. Cancer Cell. 2013;23:249–262. doi: 10.1016/j.ccr.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 61.Allavena P, Signorelli M, Chieppa M, et al. Anti-inflammatory properties of the novel antitumor agent Yondelis (trabectedin): inhibition of macrophage differentiation and cytokine production. Cancer Res. 2005;65:2964–2971. doi: 10.1158/0008-5472.CAN-04-4037. [DOI] [PubMed] [Google Scholar]
- 62.Di Giandomenico S, Frapolli R, Bello E, et al. Mode of action of trabectedin in myxoid liposarcomas. Oncogene. 2014;33:5201–5210. doi: 10.1038/onc.2013.462. [DOI] [PubMed] [Google Scholar]
- 63.Feuerhahn S, Giraudon C, Martinez-Diez M, et al. XPF-dependent DNA breaks and RNA polymerase II arrest induced by antitumor DNA interstrand crosslinking-mimetic alkaloids. Chem Biol. 2011;18:988–999. doi: 10.1016/j.chembiol.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 64.Germano G, Frapolli R, Simone M, et al. Antitumor and anti-inflammatory effects of trabectedin on human myxoid liposarcoma cells. Cancer Res. 2010;70:2235–2244. doi: 10.1158/0008-5472.CAN-09-2335. [DOI] [PubMed] [Google Scholar]