Abstract
Background and Purpose
People with epilepsy (PWE) are more likely to experience suicidality, with suicidal ideation and attempts, than people without epilepsy (PWoE). The aims of the present study were to determine 1) the characteristics of suicidality in Korean PWE, 2) whether PWE with suicidality receive psychiatric intervention, and 3) the risk factors for suicidality.
Methods
Patients who consecutively visited epilepsy clinics at secondary- and tertiary-care hospitals were recruited (n=684), along with age- and sex-matched PWoE (n=229). The presence of current major depressive disorder (MDD), generalized anxiety disorder (GAD), and/or suicidality was established using the Mini International Neuropsychiatric Interview-Plus Version 5.0.0. The Korean version of the Liverpool Adverse Events Profile (K-LAEP) was applied to detect adverse effects of antiepileptic drugs (AEDs).
Results
Suicidality was present in 208 (30.4%) of the 684 PWE. The rate of suicidality was 4.6 times higher among PWE than PWoE, and 108 (15.7%) PWE had suicidal ideation and had attempted suicide. Among those who had attempted suicide, 40.7% had made at least two attempts. The most common method of suicide attempt was drug overdose (34.9%). Unfortunately, of the 208 PWE with suicidality, 136 (65.4%) did not receive psychiatric intervention. The risk factors for suicidality were MDD [odds ratio (OR)=6.448, 95% confidence interval (CI)=3.739-11.120, p<0.001], GAD (OR=3.561, 95% CI=1.966-6.452, p<0.001), item scores of 3 or 4 on the K-LAEP (OR=2.688, 95% CI=1.647-4.387, p<0.001), and a history of febrile convulsion (OR= 2.188, 95% CI=1.318-3.632, p=0.002).
Conclusions
Suicidality is more prevalent in PWE than in PWoE. Clinicians should monitor psychiatric disorders and the adverse effects of AEDs in PWE in an attempt to reduce the incidence of suicidal ideation or suicide attempts in this patient population.
Keywords: suicide, epilepsy, depression, anxiety, adverse effect, risk factor
Introduction
Suicide is the tenth leading cause of death worldwide,1 with approximately 800,000-1,000,000 people succumbing annually and a mortality rate of 11.6 per 100,000 persons per year.2 The Organization for Economic Co-operation and Development (OECD) has reported that suicide is a significant cause of death in many OECD countries, accounting for over 150,000 deaths in 2011.3 Korea has the highest suicide rate of the 34 OECD countries, at 33.3 deaths per 100,000 population.3 Although suicide rates have decreased by more than 20% across OECD countries since 1990,3 the rate has continued to increase in Korea, where suicide has become the fourth leading cause of death.4 Psychiatric disorders, and notably depression, anxiety, psychotic, and personality disorders, are well known as the main risk factors for suicide.1 Therefore, close observation and management of high-risk populations with psychiatric disorders are mandatory for reducing the suicide rate.
People with epilepsy (PWE) have a high risk of developing psychiatric disorders. According to a review of the literature, 9-37% of PWE meet the criteria for depression and 11-25% for anxiety, compared to 6-19% and 7-11%, respectively, of the general population or people without epilepsy (PWoE).5 A Korean hospital-based study found that the risk of developing depression is 3.2-fold higher and the risk of developing anxiety is 4.8-fold higher in PWE than in healthy controls.6 Along with the high prevalence of psychiatric disorders, PWE appear to have a higher risk of developing suicidality, with suicidal ideation and suicide attempts, than do PWoE. A Canadian population-based study exploring numerous aspects of mental health in PWE in the community found that the lifetime prevalence of suicidal ideation is 25%, which is almost two times higher than that for PWoE.7 A Danish population-based study found that the risk of committing suicide is three times higher among PWE than in the general population,8 and a Korean hospital-based survey at two tertiary-care centers found that suicidal ideation is 3.6 times more common in PWE than in healthy controls.6 Although suicidal ideation may be a significant warning sign for suicide attempts, most people who experience suicidal ideation do not actually commit suicide.9 Therefore, investigations of suicide should include the characteristics of suicide attempts, such as the frequency, number, and method of suicide attempts. However, these characteristics were not evaluated in the aforementioned Korean study.
According to studies carried out in the US and Europe, the major risk factors for suicidality are psychiatric disorders or psychiatric symptoms.8,10,11 The following seizure-related parameters have also been proposed as risk factors: daily dose, type, or number of antiepileptic drugs (AEDs), socioeconomic status, and female gender.8,11,12 The use of AEDs has been high-lighted as a potential risk factor.13 In 2008, the US Food and Drug Administration reported a twofold increased risk of suicidal ideation or suicide attempts for 11 AEDs [odds ratio (OR)=1.80 and 95% confidence interval (CI)=1.24-2.66].14 However, the available data are not methodologically strong enough to support or reject the claimed increased risk of suicidality with AEDs.15 Given the controversy regarding the impact of AEDs on suicidality, a study of the adverse effects of AEDs as a risk factor for suicidality may additionally provide evidence to resolve that issue. In Korea, the risk factors for suicide have been investigated in only one hospital-based study in which 257 PWE were recruited, which demonstrated that the strongest predictor for suicidal ideation was depression symptoms, followed by obsessive-compulsive symptoms, hostility, and paranoid ideation; seizure-related factors did not appear to contribute to suicidal ideation.16 The limitations of that study were that the socioeconomic status and adverse effects of AEDs were not considered as variables contributing to suicidal ideation, and the risk factors for suicide attempts were not examined. Therefore, studies are required to determine the risk factors for suicidality, including suicidal ideation and suicide attempts, in which the effects of socioeconomic status and adverse effects of AEDs are also considered.
While many population- or hospital-based studies have been conducted in Western countries to investigate suicidality and its risk factors in PWE,17 such studies involving large numbers of PWE have not been performed in Korea. Furthermore, the proportion of patients with suicidality who actually receive a psychiatric intervention in Korea has not been established. Therefore, the aims of the present multicenter trial were to determine the characteristics of suicidality in a large number of Korean PWE, examine the frequency of psychiatric interventions among PWE with suicidality, and to establish the involved risk factors.
Methods
Subjects
Subjects who visited epilepsy clinics at secondary- and tertiary-care hospitals were recruited consecutively. The participants were adults aged 21-70 years old with a current diagnosis of epilepsy who had been taking one or more AEDs for at least 1 year; all were able to provide informed consent to participate and agreed with the study protocol. The following exclusion criteria were applied: 1) insufficient information in the medical records, 2) mental retardation or serious medical, neurological, or psychiatric disorders that prevent the patient from understanding the questionnaire or cooperating with the study, and 3) refusal to respond to the questionnaires. Age- and sex-matched PWoE were also recruited, including parents, children, or relatives of the patients, medical students, and hospital employees without epilepsy.
Study design
The Multicenter trial of Epilepsy and PSYchiatric diseases (MEPSY) is a multicenter, cross-sectional study assessing depression, anxiety, suicidality, the burden of adverse effects of AEDs, and quality of life in Korean PWE. The subjects were consecutively enrolled beginning in November 2012 at the outpatient epilepsy clinics of four tertiary- and one secondary-care hospitals in Daegu City located in the Southern part of Korea. This study was performed as a part of the MEPSY study. The Institutional Review Board of each center approved the study, and all subjects provided written informed consent to participate before the study began. All of the participants were diagnosed according to the International League Against Epilepsy classification of seizures and epileptic syndromes.18,19 All patients were interviewed by trained epileptologists who also reviewed their medical charts for demographic, social, and clinical information in the computerized database. Socioeconomic factors were classified as follows: having a job vs. not having a job; earning ≥1,000,000 Korean won (KRW)/month (equivalent to US$ 980/month) vs. <1,000,000 KRW/month; having a driving license vs. not having a driving license; and being married vs. being divorced, bereaved, or unmarried. The clinical variables included the age at disease onset, disease duration, seizure type, disease etiology, epilepsy syndrome, seizure control, magnetic resonance imaging (MRI) abnormality, history of febrile convulsion, family history of epilepsy, duration of AED intake, AED therapy regimen, and AED load. Etiology was divided into idiopathic and cryptogenic/symptomatic epilepsy, and epileptic syndromes were divided into the following four groups: temporal lobe epilepsy (TLE), extraTLE, generalized epilepsy, and unknown syndromes. ExtraTLE included epilepsy syndromes in which the epileptic attacks originate from the frontal, parietal, or occipital lobes. Seizure control was divided into the following three groups:20
Well-controlled epilepsy (WCE), defined as freedom from seizures over the preceding year.
Uncontrolled epilepsy (UCE), defined according to the criteria used to determine drug-refractory epilepsy (i.e., the failure of adequate trials of two AEDs, an average of more than one seizure per month for 18 months, and no seizure-free periods longer than 3 months).
Poorly controlled epilepsy, defined as an intermediate degree of seizure control that did not meet the criteria for WCE or UCE.
The seizure control classification for individual PWE was determined based on information about the seizure frequency that was obtained from their medical records. The AED load of each individual patient was estimated as the sum of the prescribed daily dose divided by the daily dose (DDD) ratios for each AED included in the treatment regimen,21 where DDD corresponds to the assumed average maintenance daily dose of a drug used for its main indication.22
Neuropsychologists evaluated eligible subjects for current major depressive disorder (MDD), current generalized anxiety disorder (GAD), and suicidality using the Mini-International Neuropsychiatric Interview-Plus Version 5.0.0 (MINI).23 In PWE, the Korean version of the Liverpool Adverse Events Profile (K-LAEP) was implemented to detect the adverse effects of AEDs.24 The frequency of suicidal ideation and suicide attempts in PWE was established, and if suicide had been attempted, the number of attempts was counted and the method(s) of attempt noted. Also recorded was whether PWE experiencing suicidality were provided with a psychiatric intervention as part of their treatment. The timing of any psychiatric intervention (i.e., current or previous) was noted in order to establish whether the patients were submitting to a psychiatric intervention while enrolled in the study. The variables contributing to suicidality in PWE were determined. After the risk factors were established, the probability of suicidality relative to the combination of risk factors was measured.
Interview and questionnaire
The MINI
The MINI is a brief, structured interview based on the Diagnosis and Statistical Manual of Mental Disorders-IV criteria, and is the gold standard for detecting psychiatric disorders.10 The Korean version of this instrument has been validated.23 Cohen's kappa values for the diagnosis of MDD and GAD using the MINI were found to be 0.71 and 0.57, respectively, demonstrating good agreement between the MINI-based diagnosis and expert diagnosis. Suicidality is assessed with the suicidality module, which was developed by Sheehan et al.25 and consists of the following six, differently weighted questions pertaining to the "wish for death":
In the past month, did you think you would be better off dead or wish you were dead? (weight of 1).
In the past month, did you want to harm yourself? (weight of 2).
In the past month, did you have suicidal thoughts? (weight of 6).
In the past month, did you have a suicide plan? (weight of 10).
In the past month, did you attempt suicide? (weight of 10).
Have you ever attempted suicide? (weight of 4).
Recent suicide-related questions were asked based on the symptoms experienced during the preceding 1 month. If respondents answered "yes" for at least one of the six questions, they were considered to have suicidality. The degree of current suicidality was estimated from the sum of the weighted score of the six questions as follows: no (score=0) or a low (score=1-5), moderate (score=6-9), or high (score ≥10) level of suicide risk.
The K-LAEP
The K-LAEP measures common adverse effects of AEDs during the preceding 4 weeks,24 and consists of a 19-item questionnaire. Each item in the questionnaire is scored on a 4-point Likert scale (from 1 to 4), where scores of 1, 2, 3, and 4 indicate never a problem, rarely a problem, sometimes a problem, and always or often a problem, respectively. Total scores for the K-LAEP can range from 19 to 76, and higher scores are indicative of a greater burden of adverse effects. Cronbach's α coefficient for this instrument is 0.9. The 21-item version was used in the present analysis, with 2 items being added (thinking clearly and slurred speech) in accordance with the quality-of-life study of Baker et al.26 Therefore, in the present study the possible K-LAEP score ranged from 21 to 84. It was considered that items scoring 3 or 4 points were factors related to the adverse effects of AEDs.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS version 19.0) was used for the data analyses. Descriptive statistics are presented in terms of the counts, percentages, means, and standard deviations. The independent t test, Mann-Whitney U test, and chi-square test were used to compare continuous and categorical variables as appropriate. The chi-square test was used to calculate the OR and 95% CI values. Factors associated with suicidality in PWE were measured by univariate and multivariate logistic regression analyses. The threshold for statistical significance was set at p<0.05.
Results
In total, 825 PWE were initially enrolled in the study, of which 141 were excluded due to refusal to participate in the study (n=32), inability to complete the interviews or questionnaire because of mental retardation (n=47) or serious medical or neurological diseases (n=43), and old age (n=19). Therefore, 684 PWE (mean age, 41.5 years; 57.6% male) were ultimately included. In addition, 229 PWoE (mean age, 41.4 years; 57.2% male) were also invited to participate in the study. The demographic and clinical characteristics of all of the study subjects are listed in Table 1. The levels of education, employment, household income, driving license ownership, and marriage were lower for PWE than for PWoE. Concurrent medical diseases were present in 146 PWE (21.3%), and included diabetes and other endocrinologic disorders (n=41), hypertension and other cardiovascular disorders (n=37), cerebrovascular disease and other neurological disorders (n=24), hepatic and gastrointestinal disorders (n=20), renal disorders (n=8), and other diseases (n=47). Concurrent medical diseases were present in 46 PWoE (20.1%), and included diabetes and other endocrinologic disorders (n=11), hypertension and other cardiovascular disorders (n=8), cerebrovascular disease and other neurological disorders (n=7), hepatic and gastrointestinal disorders (n=6), renal disorders (n=3), and other diseases (n=11). Partial onset of seizures and cryptogenic/symptomatic etiologies were more prevalent among PWE than generalized seizures and idiopathic etiology. Of the PWE, 61% had experienced 1 year of seizure freedom. MRI abnormalities were found in 276 (40.4%) PWE, and the etiologies of these abnormalities were hippocampal sclerosis (n=78), vascular lesions (n=54), traumatic injury (n=47), congenital anomalies (n=44), infection (n=36), tumor (n=8), and others (n=32). The duration of AED intake was 14.0±12.1 years (mean±SD; range, 1-54 years), and almost 50% of the patients received AED monotherapy. The AED load was 1.5±1.2 (range 0.1-7.7). With respect to adverse effects, 61.5% of the patients scored K-LAEP items with 3 or 4 points.
Table 1.
Demographic and clinical characteristics of PWE and PWoE
The data are presented as mean±SD (range) or number (%).
*Number of patients with an item scoring at least 3 points on the K-LAEP.
AEDs: antiepileptic drugs, K-LAEP: Korean version of the Liverpool Adverse Events Profile, KRW: Korean won, MRI: magnetic resonance imaging, PCE: poorly controlled epilepsy, PWE: people with epilepsy, PWoE: people without epilepsy, UCE: uncontrolled epilepsy, WCE: well-controlled epilepsy.
The probabilities of current MDD and GAD and suicidality for PWE and PWoE are given in Table 2. The frequencies of current MDD and GAD were 21.9% and 18.6% in PWE, respectively, and were 4.7 times and 6.3 times higher than for PWoE. The frequency of suicidality was 30.4% in PWE, which was 4.6 times higher than that in PWoE. The degree of suicidality did not differ between PWE and PWoE. Suicidal ideation without a suicide attempt was reported by 100 PWE (14.6%), and combined issues manifested in 108 PWE (15.8%). Among the 108 PWE who attempted suicide, 64 (59.3%) had made a single attempt, 17 (15.7%) had made two attempts, 8 (7.4%) had made 3 attempts, and 19 (17.6%) had attempted suicide more than 3 times. In total, 40.7% of patients who attempted suicide had done so more than once.
Table 2.
Comparison of Mini International Neuropsychiatric Interview between PWE and PWoE
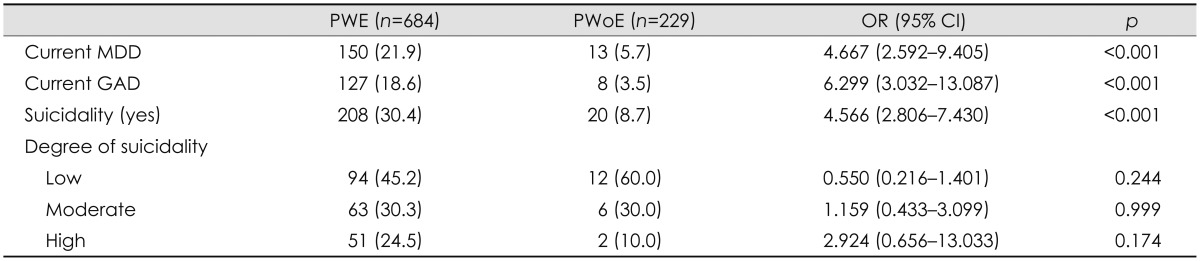
The data are presented as number (%).
CI: confidence interval, GAD: generalized anxiety disorder, MDD: major depressive disorder, OR: odds ratio, PWE: people with epilepsy, PWoE: people without epilepsy.
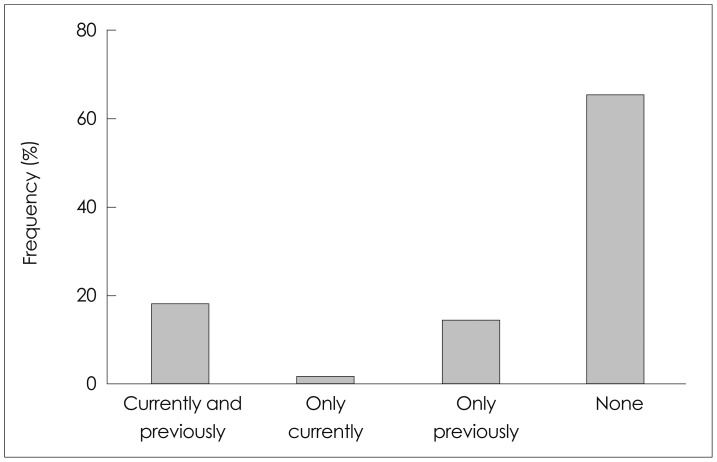
The methods of suicide attempt are illustrated in Fig. 1. The most common method of suicide attempt was drug overdose (n=46, 34.9%), followed by cutting or stabbing (n=25, 18.9%), hanging (n=17, 12.9%), jumping (n=14, 10.6%), poisoning (n=10, 7.6%), drowning (n=9, 6.8%), vehicular impact (n=6, 4.5%), and others (n=5, 3.8%). The drugs used in drug overdoses were psychiatric drugs (n=24, 18.2%), medical drugs (n=15, 11.4%), and AEDs (n=7, 5.3%).
Fig. 1.
Method of suicidal attempt in eligible patients (n=108).
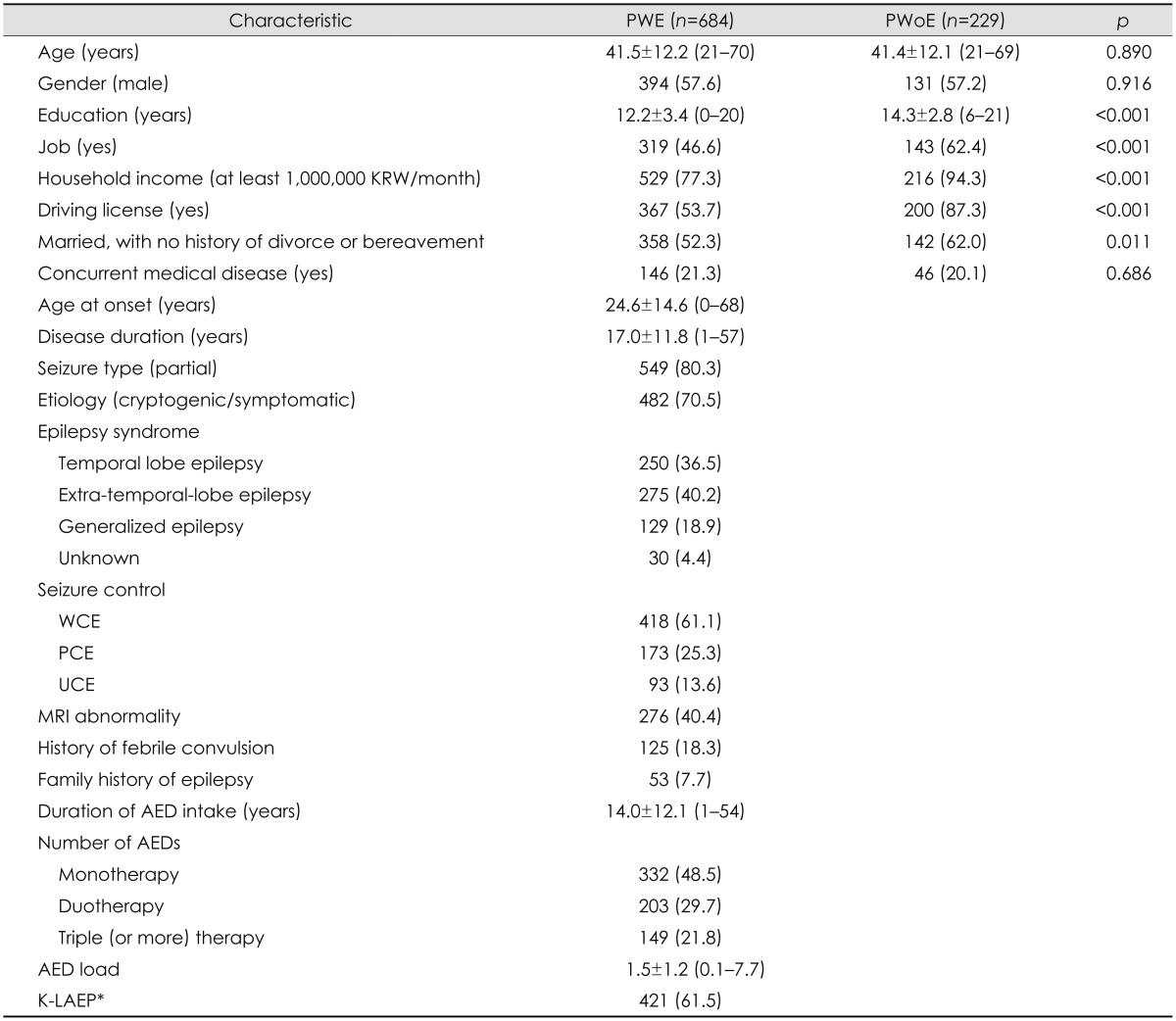
The frequency of psychiatric interventions among PWE with suicidality is shown in Fig. 2. Among 208 PWE who were suicidal, 38 patients (18.3%) had previously undergone or were currently undergoing a psychiatric intervention. However, 4 patients (1.9%) were only currently receiving an intervention and 30 (14.4%) had only received an intervention previously. Unfortunately, 136 patients (65.4%) had never received any psychiatric intervention.
Fig. 2.
The frequency of psychiatric intervention in patients with suicidality (n=208). The time of psychiatric intervention (currently or previously) was determined as whether patients were receiving psychiatric intervention at the enrollment of the study.
The factors associated with suicidality in PWE according to univariate analysis are summarized in Table 3. Suicidality was significantly associated with female gender, unemployment, low household income, no driver's license, being unmarried, divorced, or bereaved, early age of onset, large number of AEDs (monotherapy vs. triple therapy), cryptogenic/symptomatic etiology, poor seizure control (WCE vs. UCE), history of febrile convulsion, high AED load, MDD, GAD, and item(s) scoring 3 or 4 on the K-LAEP.
Table 3.
Factors associated with suicidality in PWE (univariate analysis)
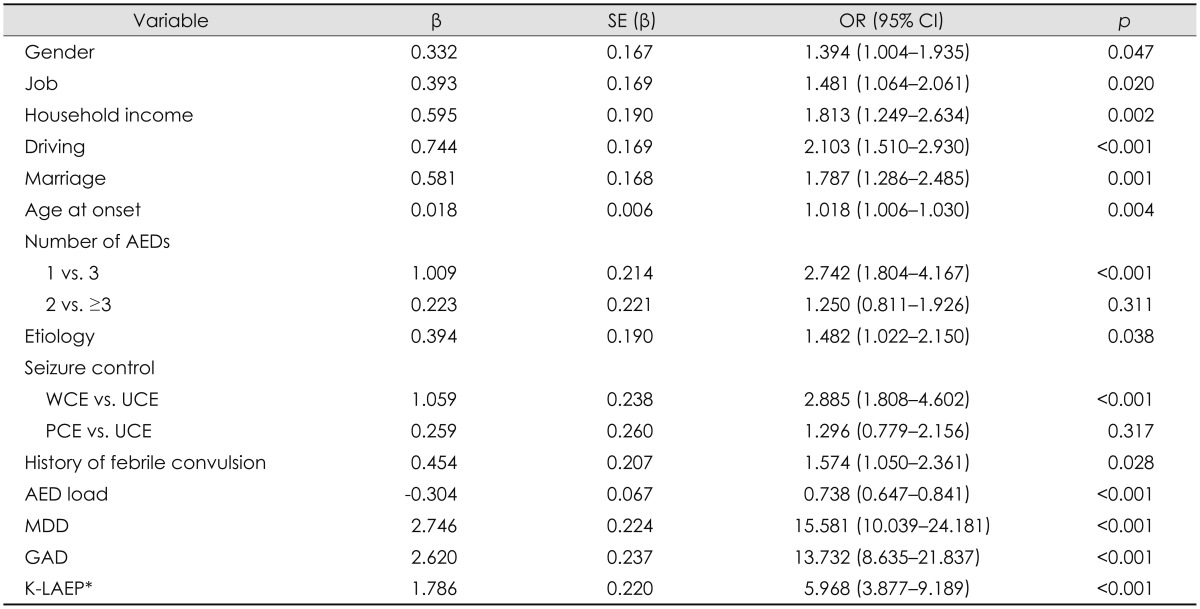
*Item(s) scoring 3 or 4 on the K-LAEP.
AEDs: antiepileptic drugs, CI: confidence interval, GAD: generalized anxiety disorder, K-LAEP: Korean version of the Liverpool Adverse Events Profile, MDD: major depressive disorder, OR: odds ratio, PCE: poorly controlled epilepsy, PWE: people with epilepsy, SE: standard error, UCE: uncontrolled epilepsy, WCE: well-controlled epilepsy.
The risk factors for suicidality revealed multivariate logistic regression analysis are listed in Table 4. The most powerful risk factor for suicidality was MDD (OR=6.448, 95% CI=3.739-11.120, p<0.001), followed by GAD (OR=3.561, 95% CI=1.966-6.452, p<0.001), item(s) scoring 3 or 4 on the K-LAEP (OR=2.688, 95% CI=1.647-4.387, p<0.001), and a history of febrile convulsion (OR=2.188, CI=1.318-3.632, p=0.002). The probability of suicidality with respect to the combination of three main risk factors of MDD, GAD, and item(s) scoring 3 or 4 on the K-LAEP is given in Table 5. If the patient had MDD, GAD, and item(s) scoring 3 or 4 on the K-LAEP, the probability of suicidality was 45.5-fold higher compared to patients with none of these risk factors (p<0.001). The probability of suicidality was also 22.6-fold higher when the patient had two risk factors, such as MDD/GAD, MDD/item(s) scoring 3 or 4 on the K-LAEP, or GAD/item(s) scoring 3 or 4 on the K-LAEP (p<0.001). However, it increased only 2.9-fold when the patient had only one of these risk factors (p<0.001). Although patients who had three risk factors appeared more likely to have increased suicidality than those patients who had only two risk factors, the difference was not statistically significant.
Table 4.
Risk factors associated with suicidality in PWE (multivariate analysis)
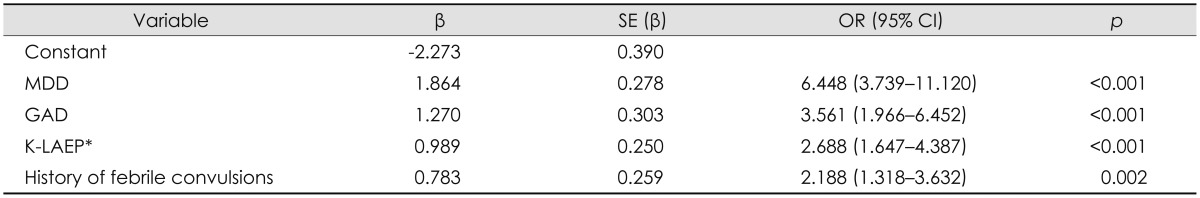
*Item(s) scoring 3 or 4 on the K-LAEP.
CI: confidence interval, GAD: generalized anxiety disorder, K-LAEP: Korean version of the Liverpool Adverse Events Profile, MDD: major depressive disorder, OR: odds ratio, PWE: people with epilepsy, SE: standard error.
Table 5.
Odds ratio of suicidality with respect to the combination of the three main risk factors
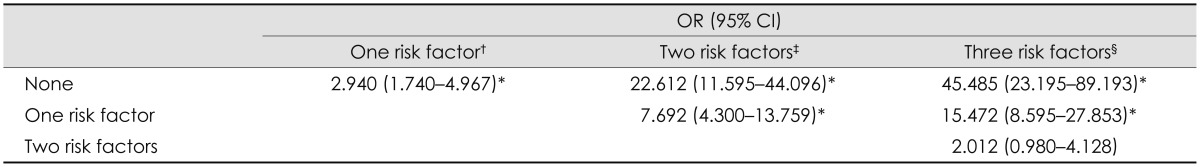
*p<0.001, †One of MDD, GAD, and item(s) scoring 3 or 4 on the K-LAEP, ‡MDD/GAD, MDD/item(s) scoring 3 or 4 on the K-LAEP score, or GAD/item(s) scoring 3 or 4 on the K-LAEP, §MDD+GAD+item(s) scoring 3 or 4 on the K-LAEP.
CI: confidence interval, GAD: generalized anxiety disorder, K-LAEP: Korean version of the Liverpool Adverse Events Profile, MDD: major depressive disorder, OR: odds ratio.
Discussion
This is the first study to investigate the characteristics of suicidality among PWE living in Korea. Over 30% of the included PWE had suicidality, and this rate was 4.6 times higher than that of PWoE. Almost 16% of patients had attempted suicide, and GAD was closely related to the number of suicide attempts. Drug overdose was the most common method of suicide attempt. Almost two-thirds of patients had not received psychiatric interventions at the time of enrollment. The main risk factors contributing to suicidality were MDD, GAD, and item(s) scoring 3 or 4 on the K-LAEP score. Clinicians should thus always pay attention to possible psychiatric problems and the adverse effects of AEDs in PWE, and manage them appropriately in an attempt to reduce the risk of suicidal ideation or suicide attempts.
Population-based, case-control studies have revealed that the frequency of psychiatric diseases is increased in PWE.7,8 In a Korean hospital-based study, PWE had 3.2- and 4.8-fold higher risks of developing depression and anxiety symptoms, respectively, than healthy controls.6 In the present study, the frequencies of current MDD and GAD were 21.9% and 18.6%, respectively, in PWE, and they were 4.7 and 6.3 times higher than those in PWoE. The differences in these frequencies of MDD and GAD can be explained by differences in their methods of assessment. The MINI interview was conducted herein to identify depression and anxiety, rather than a self-reported questionnaire.
In this study, 30.4% of PWE had suicidality, which is higher than the lifetime prevalence of suicidal ideation in Canadian PWE,7 probably because suicidality in this study included both suicidal ideation and suicide attempts. A suicide attempt is a significant risk factor for completed suicide, and completed suicide is an important contributor to increased mortality.10 This means that it is necessary to investigate both suicide attempts and suicidal ideation. A retrospective cohort study in the UK found that 51% of PWE attempted suicide more than once during the 15-year observation period, with this frequency being 1.6 times higher than that in PWoE.27 In the present study, 40.7% of patients who attempted suicide tried to do so more than once. Although this was a cross-sectional study, we presumed that many PWE were likely to repeatedly attempt suicide. The number of suicide attempts was not counted for PWoE, and so it was not possible to identify whether the number of repeated suicide attempts was higher in PWE than in PWoE.
The methods of suicide in PWE were determined in this study. A previous study involving a general population found that the most common methods of suicide were hanging, poisoning, and self-immolation.28 In Singapore, jumping is the most frequent method.29 In countries with larger rural populations, such as India and the Republic of Korea, poisoning (usually by pesticides) is common.30,31 In a recent brief report on suicide by the Korean Ministry of Health and Welfare, the most frequent method of suicide attempt in people who visited an emergency room was drug ingestion (55.9%), followed by stabbing with a knife or sharpener (14%) and poisoning by agricultural chemicals (12.2%).32 A UK study on PWE found that 94% of self-harmed PWE had poisoned themselves, whereas only 33% of self-harming PWE had injured themselves.27 The present study revealed the same tendency as the UK study, with the frequency of drug overdose and poisoning being higher than for self-injury (42.5% vs. 18.9%).
While comorbid psychiatric disorders and suicidality in PWE have been found in many studies, a significant proportion of patients has not been appropriately diagnosed or treated by clinicians. In a hospital-based study assessing the impact of sertraline on the severity and frequency of seizures in PWE, 50% of patients diagnosed with MDD at enrollment did not have a previous history thereof.33 In a multicenter trial evaluating psychiatric morbidity in chronic epilepsy, only 43.3% of patients diagnosed with a current MDD were taking an antidepressant medication.34 A hospital-based study investigating psychiatric disorders in patients with complex partial seizure revealed that 42.9% of patients with a current MDD had never received treatment.35 Furthermore, in a survey of the approach used by clinicians to suicidality and depression in PWE, almost 62% did not use a scale to routinely screen for depression in PWE.36 Among the respondents, only 17% asked their visiting patients about suicidality, and 47% queried about suicidality only among patients with depression. Approximately 42% of the patients did not feel comfortable receiving treatment for depression. A recent retrospective cohort study in the UK found that 30% of PWE reported harming themselves, as defined by intentional self-poisoning, self-injury, or both, and they did not undergo psychiatric treatment.27 The present study found that 65.4% of PWE with suicidality did not receive any psychiatric intervention. This means that suicidality is much more likely to be underrecognized in Korean PWE than among PWE in at least some Western countries. There is a high suicide rate among the Korean population, and so clinicians should address PWE as a population at a high risk of attempting suicide. We therefore strongly recommend that clinicians screen for suicidality in PWE. The suicidality module of the MINI is a short, efficient diagnostic interview designed to detect suicidal ideation, suicidal plans, and suicide attempts,25 and it can be applied to PWE.10 If there is insufficient time to perform such an interview, then we recommend that physicians use the suicide item of the Neurological Disorders Depression Inventory for Epilepsy (NDDI-E; i.e., item 4 of the NDDI-E: "I'd be better off dead").37 The findings of the present study may help to alert clinicians to PWE who are at risk of suicide, and may thus promote further assessment or appropriate referrals.
Many studies have found that the frequency of psychiatric diseases is elevated among PWE,5,6,7 and that psychiatric problems are the strongest risk factors for suicide.8,10,11,16 We also found that MDD is the strongest predictor of suicidality in PWE, followed by GAD. Brief screening tools, such as the NDDI-E and the seven-item GAD questionnaire, are adequate for identifying depression and anxiety in a busy clinical setting.38,39
A unique finding of the present study is that the adverse effect of AEDs is a major risk factor for suicidality. However, there is no definite proof for increased suicidality in PWE taking AEDs;15 instead, depression and anxiety exacerbate the adverse effects of AEDs,40 and hence psychiatric problems may play a role in these findings. Further investigation into the relationship between suicidality and AEDs after adjusting for psychiatric disorders is needed. We recommend the use of the K-LAEP for identifying the adverse effects of AEDs in a busy clinical setting.24 A history of febrile convulsion was also found in this study to be a risk factor for suicidality. Prolonged febrile seizures are reportedly associated with acute hippocampal injury, an increased risk of epilepsy, and medial temporal sclerosis.41 Since hippocampal injury is associated with depression and suicide,42 a history of febrile convulsions might be likely to produce suicidality.
A limitation of this study was the inclusion of a relatively small sample. However, this is the first study to investigate the characteristics of suicidality in PWE living in Korea, and we have demonstrated that suicidality is more prevalent in PWE than in PWoE. Despite suicide being an important contributor to the increased mortality in PWE,8 we have shown here that Korean clinicians tend to overlook suicidality in this patient group. We recommend that clinicians should routinely ask PWE about suicidal ideation and their history (if any) of suicide attempts and, if suicidal ideation and suicide attempts are suspected, they should apply appropriate psychiatric interventions. Since Korean psychiatrists do not generally treat PWE, the neurologists caring for such patients should consult with psychiatrists and/or address the underlying psychiatric issues. Thus, communication and cooperation between neurologists and psychiatrists is crucial to the success of timely recognition and treatment of this potential mental health issue among PWE.
Acknowledgements
The authors thank Ju-Hui Lee, a neuropsychologist, for conducting the MINI-Plus 5.0.0 and helping in the completion of self-report questionnaires and Won-Kee Lee, a professor of Center of Biostatics, School of Medicine, Kyungpook National University for helping the statistical analyses.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 2.Värnik P. Suicide in the world. Int J Environ Res Public Health. 2012;9:760–771. doi: 10.3390/ijerph9030760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organisation for Economic Co-operation and Development (OECD) Health at a Glance 2013: OECD indicators [Internet] [place unknown]: OECD Publishing; 2013. [cited 2013 Nov 21]. Available from: http://dx.doi.org/10.1787/health_glance-2013-en. [Google Scholar]
- 4.Jeon HJ. Depression and suicide. J Korean Med Assoc. 2011;54:370–375. [Google Scholar]
- 5.Kwon OY, Park SP. Depression and anxiety in people with epilepsy. J Clin Neurol. 2014;10:175–188. doi: 10.3988/jcn.2014.10.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon OY, Park SP. Frequency of affective symptoms and their psychosocial impact in Korean people with epilepsy: a survey at two tertiary care hospitals. Epilepsy Behav. 2013;26:51–56. doi: 10.1016/j.yebeh.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Tellez-Zenteno JF, Patten SB, Jetté N, Williams J, Wiebe S. Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia. 2007;48:2336–2344. doi: 10.1111/j.1528-1167.2007.01222.x. [DOI] [PubMed] [Google Scholar]
- 8.Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6:693–698. doi: 10.1016/S1474-4422(07)70175-8. [DOI] [PubMed] [Google Scholar]
- 9.Mościcki EK. Epidemiologic surveys as tools for studying suicidal behavior: a review. Suicide Life Threat Behav. 1989;19:131–146. doi: 10.1111/j.1943-278x.1989.tb00372.x. [DOI] [PubMed] [Google Scholar]
- 10.Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003;4(Suppl 3):S31–S38. doi: 10.1016/j.yebeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 11.Nilsson L, Ahlbom A, Farahmand BY, Asberg M, Tomson T. Risk factors for suicide in epilepsy: a case control study. Epilepsia. 2002;43:644–651. doi: 10.1046/j.1528-1157.2002.40001.x. [DOI] [PubMed] [Google Scholar]
- 12.Kalinin VV, Polyanskiy DA. Gender differences in risk factors of suicidal behavior in epilepsy. Epilepsy Behav. 2005;6:424–429. doi: 10.1016/j.yebeh.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Brent DA, Crumrine PK, Varma RR, Allan M, Allman C. Phenobarbital treatment and major depressive disorder in children with epilepsy. Pediatrics. 1987;80:909–917. [PubMed] [Google Scholar]
- 14.Levenson M, Rochester CG, Mentari E, Hughes A, Feeney J, 3rd, Stone M, et al. Statistical review and evaluation: antiepileptic drugs and suicidality [Internet] Silver Spring (MD): U.S. Food and Drug Administration; 2008. [cited 2014 May 23]. Available from: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm100190.htm. [Google Scholar]
- 15.Mula M, Sander JW. Suicide risk in people with epilepsy taking antiepileptic drugs. Bipolar Disord. 2013;15:622–627. doi: 10.1111/bdi.12091. [DOI] [PubMed] [Google Scholar]
- 16.Lim HW, Song HS, Hwang YH, Lee HW, Suh CK, Park SP, et al. Predictors of suicidal ideation in people with epilepsy living in Korea. J Clin Neurol. 2010;6:81–88. doi: 10.3988/jcn.2010.6.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verrotti A, Cicconetti A, Scorrano B, De Berardis D, Cotellessa C, Chiarelli F, et al. Epilepsy and suicide: pathogenesis, risk factors, and prevention. Neuropsychiatr Dis Treat. 2008;4:365–370. doi: 10.2147/ndt.s2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1981;22:489–501. doi: 10.1111/j.1528-1157.1981.tb06159.x. [DOI] [PubMed] [Google Scholar]
- 19.Proposal for classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1985;26:268–278. [PubMed] [Google Scholar]
- 20.Berg AT, Shinnar S, Levy SR, Testa FM, Smith-Rapaport S, Beckerman B. Early development of intractable epilepsy in children: a prospective study. Neurology. 2001;56:1445–1452. doi: 10.1212/wnl.56.11.1445. [DOI] [PubMed] [Google Scholar]
- 21.Deckers CL, Hekster YA, Keyser A, Meinardi H, Renier WO. Reappraisal of polytherapy in epilepsy: a critical review of drug load and adverse effects. Epilepsia. 1997;38:570–575. doi: 10.1111/j.1528-1157.1997.tb01142.x. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization Collaborating Centre for Drug Statistics Methodology (NO) ATC/DDD Index 2014 [Internet] Oslo: World Health Organization Collaborating Centre for Drug Statistics Methodology; 2013. [cited 2013 Nov 1]. Available from: http://www.whocc.no/atc_ddd_index/ [Google Scholar]
- 23.Yoo SW, Kim YS, Noh JS, Oh KS, Kim CH, Namkoong K, et al. Validity of Korean version of the Mini-International Neuropsychiatric Interview. Anxiety Mood. 2006;2:50–55. [Google Scholar]
- 24.Park JM, Seo JG, Park SP. Validity and reliability of the Korean version of the Liverpool Adverse Events Profile (K-LAEP) in people with epilepsy. J Korean Epilepsy Soc. 2012;16:43–48. [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34-57. [PubMed] [Google Scholar]
- 26.Baker GA, Jacoby A, Buck D, Stalgis C, Monnet D. Quality of life of people with epilepsy: a European study. Epilepsia. 1997;38:353–362. doi: 10.1111/j.1528-1157.1997.tb01128.x. [DOI] [PubMed] [Google Scholar]
- 27.Meyer N, Voysey M, Holmes J, Casey D, Hawton K. Self-harm in people with epilepsy: a retrospective cohort study. Epilepsia. 2014;55:1355–1365. doi: 10.1111/epi.12723. [DOI] [PubMed] [Google Scholar]
- 28.Morovatdar N, Moradi-Lakeh M, Malakouti SK, Nojomi M. Most common methods of suicide in Eastern Mediterranean Region of WHO: a systematic review and meta-analysis. Arch Suicide Res. 2013;17:335–344. doi: 10.1080/13811118.2013.801811. [DOI] [PubMed] [Google Scholar]
- 29.Ung EK. Youth suicide and parasuicide in Singapore. Ann Acad Med Singapore. 2003;32:12–18. [PubMed] [Google Scholar]
- 30.Bose A, Konradsen F, John J, Suganthy P, Muliyil J, Abraham S. Mortality rate and years of life lost from unintentional injury and suicide in South India. Trop Med Int Health. 2006;11:1553–1556. doi: 10.1111/j.1365-3156.2006.01707.x. [DOI] [PubMed] [Google Scholar]
- 31.Shin SD, Suh GJ, Rhee JE, Sung J, Kim J. Epidemiologic characteristics of death by poisoning in 1991-2001 in Korea. J Korean Med Sci. 2004;19:186–194. doi: 10.3346/jkms.2004.19.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ministry of Health and Welfare (KR) Brief report of national survey on suicide 2013. Available from: http://download.mw.go.kr/front_new/modules/download.jsp?BOARD_ID=140&CONT_SEQ=299571&FILE_SEQ=148548.
- 33.Kanner AM, Kozak AM, Frey M. The Use of Sertraline in Patients with Epilepsy: Is It Safe? Epilepsy Behav. 2000;1:100–105. doi: 10.1006/ebeh.2000.0050. [DOI] [PubMed] [Google Scholar]
- 34.Jones JE, Hermann BP, Barry JJ, Gilliam F, Kanner AM, Meador KJ. Clinical assessment of Axis I psychiatric morbidity in chronic epilepsy: a multicenter investigation. J Neuropsychiatry Clin Neurosci. 2005;17:172–179. doi: 10.1176/jnp.17.2.172. [DOI] [PubMed] [Google Scholar]
- 35.Wiegartz P, Seidenberg M, Woodard A, Gidal B, Hermann B. Co-morbid psychiatric disorder in chronic epilepsy: recognition and etiology of depression. Neurology. 1999;53(5 Suppl 2):S3–S8. [PubMed] [Google Scholar]
- 36.Shneker BF, Cios JS, Elliott JO. Suicidality, depression screening, and antiepileptic drugs: reaction to the FDA alert. Neurology. 2009;72:987–991. doi: 10.1212/01.wnl.0000344403.13815.8d. [DOI] [PubMed] [Google Scholar]
- 37.Gilliam FG, Barry JJ, Hermann BP, Meador KJ, Vahle V, Kanner AM. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol. 2006;5:399–405. doi: 10.1016/S1474-4422(06)70415-X. [DOI] [PubMed] [Google Scholar]
- 38.Ko PW, Hwang J, Lim HW, Park SP. Reliability and validity of the Korean version of the Neurological Disorders Depression Inventory for Epilepsy (K-NDDI-E) Epilepsy Behav. 2012;25:539–542. doi: 10.1016/j.yebeh.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 39.Seo JG, Cho YW, Lee SJ, Lee JJ, Kim JE, Moon HJ, et al. Validation of the generalized anxiety disorder-7 in people with epilepsy: a MEPSY study. Epilepsy Behav. 2014;35:59–63. doi: 10.1016/j.yebeh.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 40.Kanner AM, Barry JJ, Gilliam F, Hermann B, Meador KJ. Depressive and anxiety disorders in epilepsy: do they differ in their potential to worsen common antiepileptic drug-related adverse events? Epilepsia. 2012;53:1104–1108. doi: 10.1111/j.1528-1167.2012.03488.x. [DOI] [PubMed] [Google Scholar]
- 41.Finegersh A, Avedissian C, Shamim S, Dustin I, Thompson PM, Theodore WH. Bilateral hippocampal atrophy in temporal lobe epilepsy: effect of depressive symptoms and febrile seizures. Epilepsia. 2011;52:689–697. doi: 10.1111/j.1528-1167.2010.02928.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.López JF, Chalmers DT, Little KY, Watson SJ. A.E. Bennett Research Award. Regulation of serotonin1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: implications for the neurobiology of depression. Biol Psychiatry. 1998;43:547–573. doi: 10.1016/s0006-3223(97)00484-8. [DOI] [PubMed] [Google Scholar]