Abstract
Background:
Investigations across the world confirm dramatic increment in the use of complementary and alternative medicine in pregnant women. The most important aspect is lack of awareness of pregnant women about potential effects of using traditional medicine on fetus; some herbal products may be teratogenic in human and animal models. In this area, so far, no research has been conducted in Ethiopia to assess traditional medicine use in pregnant women.
Objectives:
Therefore, the main objective of this study was to investigate the prevalence and use of herbal drugs among pregnant women attending Nekemte Hospital to provide baseline information for future studies.
Patients and Methods:
A cross-sectional descriptive study was conducted by quantitative and qualitative approaches to identify the prevalence of using herbal medicines among pregnant women. About 50.4% of study participants used herbal drugs during their pregnancy. The proportion of herbal drug usage was gradually decreased along with the first, second and third trimesters of pregnancy. The most and least commonly used herbs were ginger (44.36%) and tenaadam (9.15 %), respectively. The common indications of herbal remedies use during pregnancy were nausea (23.90%) and morning sickness (21.05%).
Results:
The result of the present study confirmed wide use of herbal drugs use during pregnancy that need to report the safety concerns of these drugs during pregnancy.
Conclusions:
To achieve the requirements of pregnant women, it is vital for health care workers to be familiar with the effect of herbal medicine in pregnancy.
Keywords: Herbal Medicine, Pregnancy, alternative Medicine
1. Background
Investigations across the world confirm dramatic increment in the use of complementary and alternative medicine in pregnant women. Most pregnant women believe that these medicines are ‘natural’ and ‘safe’ compared to modern drugs. Besides, traditional medicine is believed to treat medical problems and improve health status during pregnancy, birth and postpartum care in many rural areas of the world. There are few researches performed on their safety, purity and adverse consequences during pregnancy (1). Furthermore, herbs are significantly used in developed countries (Europe, USA and Australia). During 1990 to 1997, around 50% of pregnant women in the USA used herbs during pregnancy, and more women were users of alternative medicines than men. However, herbal medicine is not currently subject to the same regulations as conventional drugs. Therefore, many researchers are exploring their adverse effect on human health, especially the safety of herbal drugs in pregnancy (2). In Africa, more pregnant women use herbal remedies to treat pregnancy related problems due to cost-effectiveness of therapy and easy access of these products. In total, 80% of Ethiopian population use traditional medicine and around 90% of all deliveries are managed by traditional birth attendants or relatives. Nevertheless, data available for the use of herbal medicine among pregnant women in Ethiopia is scarce. The most important aspect is lack of awareness of pregnant women about potential effect of traditional medicine use on fetus; some herbal products may be teratogenic in human and animal models (3). Studying traditional medicine use during pregnancy is limited in Sub-Sahara Africa because of limited control of traditional medicine distribution and purchase (4).
2. Objectives
Therefore, the main objective of this study was to investigate the prevalence and use of herbal medicine among pregnant women attending Nekemte Hospital to provide baseline information for future studies.
3. Patients and Methods
3.1. Study Site and Population
The present study was conducted at Nekemte Hospital in Nekemte town, located 331 km far from the Ethiopian capital, Addis Ababa in the west direction, at 9°5'N latitude, 36°33'E longitudes and altitude of 2088 ft to the sea level. The hospital was established by a Swedish mission in 1932 E.C.
3.2. Study Design and Sampling Technique
Semistructured questionnaires were used to study possible sources of information on the prevalence and use of herbal medicine during pregnancy in a cross sectional manner. A total of 250 women were selected based on the expected prevalence rate using minimum sample size for this survey as 50%.
3.3. Study Variables
Age, socioeconomic status, sex, monthly income, ethnicity, educational level, marital status, and access to medical care were independent variables of the study; while, types of used herbal medicine, preference of herbal medicine, preparation of traditional medicine, parts of plant used, type of disease treated by traditional medicine, and method of use were dependent variables of the study. Filled questionnaires were regularly checked to promote consistency and to ensure completion of data.
-
Inclusion criteria were:
- Pregnant women in 2-9 months of pregnancy
- Those with a normal and uncomplicated pregnancy till the date of appointment.
- Able to provide informed consent
- Legally adults (18 years and older)
-
Exclusion criteria were:
- All patients who were unable to hear or communicate and mentally disabled were excluded from the study.
- Those who did not fulfill the inclusion criteria.
3.4. Ethical Considerations
All information from the participants was kept confidential and participants’ name was not recorded on the research documents. The purpose of this study was explained to subjects. Confidentiality of the information was assured and the privacy of respondents was maintained at a safe level.
4. Results
Of 250 pregnant women participated in the study, most were in the age range of 24-29 years (45.2%), Oromo (75.2%), married (88.8%), protestants (60%) and literate (25.2%) (Table 1).
Table 1. Sociodemographic Variables of Respondentsa.
| Variables | Results |
|---|---|
| Age | |
| 18-23 | 74 (29.6) |
| 24-29 | 113 (45.20) |
| 30-35 | 57 (22.8) |
| > 35 | 6 (2.4) |
| Marital status | |
| Married | 222 (88.8) |
| Single | 0 (0) |
| Divorced | 11 (4.4) |
| Widowed | 6 (2.4) |
| Separated | 11 (4.4) |
| Educational level | |
| Illiterate | 51 (20.4) |
| Primary school (1-8) | 38 (15.2) |
| Secondary school (9-12) | 64 (25.6) |
| College/university | 51 (20.4) |
| Diploma/degree | 46 (18.4) |
| Ethnicity | |
| Oromo | 188 (75.2) |
| Amhara | 51 (20.4) |
| Tigrinia | 11 (4.4) |
| Others | 0 (0) |
| Religion | |
| Orthodox | 87 (35.0) |
| Muslim | 13 (5.0) |
| Protestant | 150 (60.0) |
| Monthly Income | |
| < 500 | 46 (18.4) |
| 500-1.300 | 85 (34.0) |
| > 1.300 | 92 (36.8) |
| Employment | |
| Employed | 115 (46.0) |
| Housewife | 135 (54.0) |
| Smoking status | |
| Smoker/ex-smoker | 17 (6.8) |
| Non-smoker | 233 (93.2) |
aData are presented as No. (%).
4.1. Usage of Herbal Drugs in Pregnancy
As shown in Table 2, more herbs (69.84%) were used during the first trimester and 4.76% of women used herbs in all trimesters. The most and least commonly used herbs were ginger (44.36%) and tenaadam (9.15 %), respectively (Table 3).
Table 2. Use of Herbal Medicines in Different Trimesters in Pregnant Women at Nekemte Hospital From January 28, 2013 to February 8, 2013a.
| Variables | Response (Yes) |
|---|---|
| First trimester | 88 (69.84) |
| Second trimester | 19 (15.08) |
| Third trimester | 13 (10.32) |
| Throughout pregnancy | 6 (4.76) |
a Data are presented as No. (%).
Table 3. Types of Herbal Medicines Used During Pregnancya.
| Plants used | Number of Women |
|---|---|
| Garlic (Allium sativum) | 53 (37.32) |
| Ginger (zingiberofficinale) | 63 (44.36) |
| Eucalyptus | 13 (9.15) |
| Tenaadam (Rutachalenssis) | 13 (9.15) |
a Data are presented as No. (%).
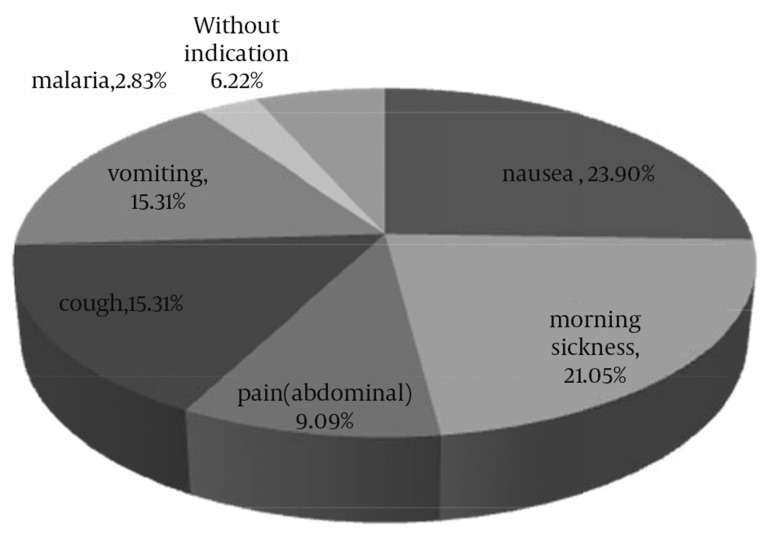
Figure 1 represents frequently reported indications of traditional medicine use in pregnancy. A total 126 indications were reported (the mean of 1.6, range: 1-4 indications). Generally, herbs were used to treat nausea (23.90%), morning sickness (21.05%), vomiting (15.31%), cough (15. 31 %), deficiency in nutrition (6.22%), and malaria (2.83%). Around 41% of pregnant women prepared herbal remedies; while, the rest obtained it from herbalists, traditional healers, neighbors or reverence places (Table 4). As depicted in table 5, most participants received information from neighbor (34.29%) and family (23.81%). Most women took herbal medicines in the form of crude (43.16%), extract (23.16 %), maceration (23.16 %), and decoction (10.53%). Various parts of plants used by the participants were leaves and roots at the same ratio of 42.33%, followed by rhizome at 7.98 %, seed and stem at 3.68 %, respectively.
Figure 1. Most Commonly Reported Indications for the Use of Herbal Medicine in Pregnancy in This Study Population.
Table 4. Sources to Obtain Herbal Medicines by Pregnant Women at Nekemte Hospital From January 28, 2013 to February 8, 2013a.
| Places | Results |
|---|---|
| Traditional healers | 6 (4.32) |
| Self-preparation | 57 (41.01) |
| Herbalist | 32 (23.02) |
| Worship place | 6 (4.32) |
| Market places | 32 (23.02) |
| Neighbor | 6 (4.32) |
a Data are presented as No. (%)
Table 5. Sources of Information on Herbal Medicine for Pregnant Women at Nekemte Hospital From January 28, 2013 to February 8, 2013 a.
| Source of information | Results |
|---|---|
| Health professionals | 30 (14.29) |
| Traditional healers | 20 (9.52) |
| Religious leaders | 6 (2.86) |
| Family | 50 (23.81) |
| Neighbor | 72 (34.29) |
| Herbalist | 32 (15.24) |
a Data are presented as No. (%).
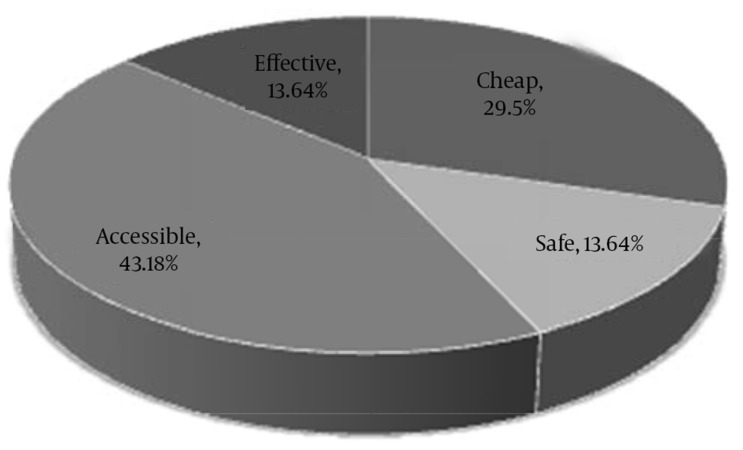
Figure 2. Reasons for Preference of Herbal Medicines Over Conventional Medicine Among Pregnant Women in This Study.
5. Discussion
The result of the present study showed that most pregnant women (50.4%) used herbs compared to other studies performed in developed countries. The possible explanation is probably easy accessibility (43.18%) and less affordability of conventional medicines. Most women rely on advices from their family and friends, and many did not disclose of care providers (5). Herbal medicine use during pregnancy in a group of Australian women was reported as 36% (6). Age and education significantly affected the use of herbal medicine. As they became older and more educated, the rate of herbal drug usage was increased. Among herbal supplements, raspberry leaf (14%), ginger (12%) and chamomile (11%) were the most widely used; while the most commonly used herbs in our study area were garlic, tenaadam, and ginger (6). A study by Nordeng and Havnen indicated wide use of echinacea, iron-rich herbs, ginger, chamomile and cranberry as herbal supplement during pregnancy (2). However, herbs used in our study were studied to be safe in most cases. Studies suggest ginger effectiveness against nausea and inflammation. there is insufficient studies regarding adverse effects of traditional plants during pregnancy (7). Leaves and roots (42.33%) were the most widely used plant parts in the present study. Nevertheless, different plant parts may be used due to differences in the types of plants available in different regions.
Most participants used herbal remedies to treat pregnancy related problems such as nausea (23.90%), morning sickness (21.05%), deficient nutrition (6.22%), vomiting and cough (15.31% and 15.31%, respectively) and malaria (2.83%). This indicates that pregnant women preferred herbal medicines because of accessibility (43.18%). This may also be due to less affordability of conventional medicines. We found that use of herbs decreased as the trimester increases, which is different from a research performed on Norwegian women where herbal drugs increased throughout pregnancy. This could be beneficial, as it may not increase pregnancy related problems (2). In contrast to other studies, the association between age, educational level, marital status, income, ethnicity and source of information with herbal drug use was not significant. Neighbors and families were major information sources in this study. Most of them preferred herbs to modern medicine, because they believed that these herbs are safe, cost-effective and easily accessible. This result is somewhat similar to the research performed on Norwegian women in 2004, as use of herbal drugs in pregnancy was mostly recommended by family or friends (2). The use of traditional medicine in Ethiopia is not integrated in the health system. Therefore, information provided by family and neighbors may not be enough to advise pregnant women about the use of herbal drugs. Increased self-medication practice, poor patients’ knowledge about drugs and accessibility of herbal medicines may contribute to the use of herbal medicines (41.01%) at the present study area. Self-administration of herbal drugs could result in harmful adverse effects not easily treated by conventional drugs. In this study, only 14.29% of the women reported to have received health advices from healthcare workers. This study was relatively similar to the study performed on the use of herbal drugs in pregnancy: a survey among 400 Norwegian women in which only 11.8% of women reported to have received advice from healthcare workers. This may indicate ineffectiveness of healthcare workers consultation about alternative therapies in Nekemte town, or Nekemte Hospital Health Care personnel may be reluctant to give advice in such matters, or both (2).
Low information was given to women about herbal drugs during pregnancy and this greatly causes misuse and/or potentially harmful use. When healthcare workers were consulted, information was not delivered in 85.71% of the cases, much lower than family/friends, herbal store, neighbors, religious person, traditional healers and alternative practitioner. This indicates that healthcare workers play a small role regarding information provision about herbal drugs to patients/customers. The result of the present study clearly depicted that around 50.4% of the women used herbal drugs during pregnancy in Nekemte Hospital, Nekemte region, Ethiopia. Frequently used herbal drugs were ginger, garlic, and tenaadam. Family and friends recommended the use of herbal drugs in pregnancy.
5.1. Recommendations
It is suggested to perform further studies on adverse effects of herbal medicines used by pregnant women. Wide use of herbal drugs during pregnancy should be assessed carefully. Besides, health education should be provided on the impact of herbal medicines. The Ministry of Health of Ethiopia should assess integrated use of herbal medicine with conventional medicines. In addition, hospitals should encourage traditional practitioners to work together with modern practitioners, and safety and effectiveness of herbal medicines used during pregnancy should be approved and announced to the community.
Acknowledgments
The authors would like to acknowledge Jimma University.
Footnotes
Authors’ Contributions:Study concept and design: Eshetu Mulisa and Bodena Bayisa; acquisition of data: Bodena Bayisa; analysis and interpretation of data: Eshetu Mulisa and Bodena Bayisa; drafting of the manuscript: Ramanjireddy Tatiparthi; critical revision of the manuscript for important intellectual content: Ramanjireddy Tatiparthi and Eshetu Mulisa; statistical analysis: Eshetu Mulisa and Bodena Bayisa; administrative, technical, and material supports: Jimma University; study supervision: Eshetu Mulisa.
References
- 1.Khadivzadeh T, Ghabel M. Complementary and alternative medicine use in pregnancy in Mashhad, Iran, 2007-8. Iran J Nurs Midwifery Res. 2012;17(4):263–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Nordeng H, Havnen GC. Use of herbal drugs in pregnancy: a survey among 400 Norwegian women. Pharmacoepidemiol Drug Saf. 2004;13(6):371–80. doi: 10.1002/pds.945. [DOI] [PubMed] [Google Scholar]
- 3.Kassaye KD, Amberbir A, Getachew B, Mussema Y. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiop J Health Dev. 2006;20(2):127–34. [Google Scholar]
- 4.Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009;9:53. doi: 10.1186/1472-6882-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pallivalappila AR, Stewart D, Shetty A, Pande B, McLay JS. Complementary and Alternative Medicines Use during Pregnancy: A Systematic Review of Pregnant Women and Healthcare Professional Views and Experiences. Evid Based Complement Alternat Med. 2013;2013:205639. doi: 10.1155/2013/205639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forster DA, Denning A, Wills G, Bolger M, McCarthy E. Herbal medicine use during pregnancy in a group of Australian women. BMC Pregnancy Childbirth. 2006;6:21. doi: 10.1186/1471-2393-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dog TL. The use of botanicals during pregnancy and lactation. Altern Ther Health Med. 2009;15(1):54–8. [PubMed] [Google Scholar]