Abstract
The lack of functional ankle musculature in lower limb amputees contributes to the reduced prosthetic ankle push-off, compensations at other joints and more energetically costly gait commonly observed in comparison to non-amputees. A variety of energy storing and return prosthetic feet have been developed to address these issues but have not been shown to sufficiently improve amputee biomechanics and energetic cost, perhaps because the timing and magnitude of energy return is not controlled. The goal of this study was to examine how a prototype microprocessor-controlled prosthetic foot designed to store some of the energy during loading and return it during push-off affects amputee gait. Unilateral transtibial amputees wore the Controlled Energy Storage and Return prosthetic foot (CESR), a conventional foot (CONV), and their previously prescribed foot (PRES) in random order. Three-dimensional gait analysis and net oxygen consumption were collected as participants walked at constant speed. The CESR foot demonstrated increased energy storage during early stance, increased prosthetic foot peak push-off power and work, increased prosthetic limb center of mass (COM) push-off work and decreased intact limb COM collision work compared to CONV and PRES. The biological contribution of the positive COM work for CESR was reduced compared to CONV and PRES. However, the net metabolic cost for CESR did not change compared to CONV and increased compared to PRES, which may partially reflect the greater weight, lack of individualized size and stiffness and relatively less familiarity for CESR and CONV. Controlled energy storage and return enhanced prosthetic push-off, but requires further design modifications to improve amputee walking economy.
Keywords: Prosthesis, Amputation, Metabolic cost, Biomechanics, Rehabilitation
1. Introduction
One in 190 Americans is currently living with the loss of a limb and the incidence of amputation is on the rise (Ziegler-Graham, MacKenzie, Ephraim, Travison, & Brookmeyer, 2008). Two-thirds of these amputations are of the lower limb, which often leads to limitations in functional mobility, an array of co-morbidities of the intact and residual limb joints (Gailey, Allen, Castles, Kucharik, & Roder, 2008; Struyf, van Heugten, Hitters, & Smeets, 2009) and persistent pain and discomfort (Ehde et al., 2000). The absence of plantar-flexor musculature significantly affects amputee gait by reducing ankle push-off power of the prosthetic limb, likely leading to compensations at other joints and increased loading of the intact limb compared to non-amputees (Gitter, Czerniecki, & de Groot, 1991; Seroussi, Gitter, Czerniecki, & Weaver, 1996; Winter & Sienko, 1988). These alterations in gait may subsequently contribute to the increased metabolic cost of amputee walking compared to non-amputee walking at the same speeds (Genin, Bastien, Franck, Detrembleur, & Willems, 2008; Waters & Mulroy, 1999) as well as contribute to the reduced self-selected walking speed, cadence and stride length (Gitter et al., 1991; Robinson, Smidt, & Arora, 1977; Torburn, Perry, Ayyappa, & Shanfield, 1990; Waters, Perry, Antonelli, & Hislop, 1976; Winter & Sienko, 1988).
Energy storage and return (ESR) prosthetic feet were designed to address reduced prosthetic limb push-off work by returning mechanical energy absorbed from mid to late stance, rather than dissipating it through viscoelastic deformation as with non-ESR prosthetic feet. ESR feet result in amplified peak fore-aft ground reaction forces in the prosthetic limb (Lehmann, Price, Boswell-Bessette, Dralle, & Questad, 1993; Powers, Torburn, Perry, & Ayyappa, 1994), increased prosthetic foot power and work generated (Barr et al., 1992; Gitter et al., 1991) and decreased vertical ground reaction forces in the sound limb during weight acceptance (Lehmann et al., 1993; Perry & Shanfield, 1993; Powers et al., 1994; Snyder, Powers, Fontaine, & Perry, 1995) compared to more traditional prosthetic feet (i.e., SACH foot). Subjectively, many amputees prefer ESR feet (Romo, 1999) and perceive an increase in activity, velocity and stability with less pain and skin problems than with non-ESR feet (Hafner, Sanders, Czerniecki, & Fergason, 2002). However, in several studies the metabolic cost of walking (Hafner et al., 2002; Lehmann et al., 1993; Torburn et al., 1990; Versluys et al., 2009; Waters et al., 1976), preferred walking speed and gait symmetry (from Barth, Schumacher, & Thomas, 1992; Grabowski, Rifkin, & Kram, 2010; Hsu, Nielsen, Lin-chan, & Shurr, 2006; Torburn et al., 1990) have not been shown to change significantly for amputees wearing ESR feet compared to more traditional designs. The general consensus is that despite subjective preference, current ESR feet demonstrate little objective improvement in overall walking performance (Hafner et al., 2002; van der Linde et al., 2004).
Increased prosthetic ankle push-off work may improve amputee gait by minimizing compensations at other joints (Au, Weber, & Herr, 2009; Houdijk, Pollman, Groenewold, Wiggerts, & Polomski, 2009; Seroussi et al., 1996). Simple walking models suggest that much of the mechanical work required for ambulation is determined by the amount of energy dissipated in the transition between steps, as the center of mass (COM) is redirected by the new stance limb (Donelan, Kram, & Kuo, 2002; Kuo, Donelan, & Ruina, 2005). The appropriate magnitude and timing of trailing leg push-off is thought to reduce the collision of the leading leg, which may lead to a decrease in total COM work (Kuo, 2002; Ruina, Bertram, & Srinivasan, 2005). Traditional prosthetic feet cause a disruption in this cycle by reducing the positive work performed by the trailing prosthetic leg at push-off, disproportionately increasing dissipation in the leading intact leg and increasing metabolic energy cost of amputee walking (Houdijk et al., 2009). Therefore, a prosthesis with increased push-off work could potentially reduce this dissipation, reduce metabolic cost and improve amputee gait.
A Controlled Energy Storage and Return (CESR) prototype prosthetic foot (Collins & Kuo, 2010), which can capture and store some of the collision energy normally dissipated at foot contact and then transfer it to the forefoot just prior to toe-off, may increase prosthetic push-off work, reduce energy loss at collision of the intact leg and reduce metabolic cost of gait. In a study of non-amputees wearing a simulator boot, a CESR foot prototype increased both average ankle push-off power and COM pushoff work, decreased intact limb COM collision work, and reduced metabolic cost by 9% compared to a conventional prosthetic foot (Collins & Kuo, 2010), suggesting the potential for similar benefits in amputees.
The aim of this study was to test for biomechanical and metabolic effects of the same CESR prototype foot on transtibial amputee gait compared to a common conventional foot and to each subject’s prescribed foot. We tested whether amputees wearing this CESR prototype would exhibit: (1) increased prosthetic foot push-off power and work, (2) increased prosthetic limb COM push-off work, (3) decreased intact limb COM collision work, (4) decreased total COM work, and (5) reduced energetic cost of walking.
2. Methods
2.1. Participants
We examined seven traumatic unilateral transtibial amputees, 52.3 ± 12 years old, 1.85 ± 0.05 m in height, and weighed 80.9 ± 9.9 kg, who gave informed consent to participate in this IRB approved study. Participants were all male between 18 and 80 years old, wore a prosthesis for at least eight hours per day for a minimum of two years, could ambulate without upper-limb aides and had no history of injurious falls within the previous six months. They were considered moderately active community ambulators and were free from neurological deficits and underlying musculoskeletal disorders that may have impacted gait characteristics by self-report.
2.2. Prosthetic components
Three prosthetic feet were fit and optimally aligned for each participant by the same experienced prosthetist in random order: (1) our prototype Controlled Energy Storage and Return prosthetic foot (CESR; 1.4 kg), (2) a conventional prosthetic foot (CONV, Seattle Lightfoot2™, size: 27 cm, Seattle Systems, Poulsbo, WA) in the participant’s own shoe, with weight added to match the CESR foot, and (3) each participant’s previously prescribed prosthetic foot (PRES) in their own shoe. Unlike the CONV and PRES feet, the CESR foot (Fig. 1) contained actively controlled elements, which regulated energy storage and return of a coil compression spring (stiffness: 157 N/mm). During prosthetic load acceptance, the rear-foot keel rotates and compresses the spring, which is locked into place with a continuous one-way clutch. During the ensuing push-off phase, a sufficient load on the fore-foot keel overcomes the spring compression, which triggers the release of a toe clutch and transfers the stored energy to the toe keel, thereby enhancing prosthetic foot push-off. A microcontroller was placed in a backpack (0.80 kg) worn by each participant for all foot conditions and connected to the CESR foot and an analog data acquisition system via cables. A detailed description of the CESR foot design and function is provided in Collins and Kuo (2010).
Fig. 1.
Schematic design of CESR foot showing the locations of the energy-storing and reset springs, clutches and sensors.
The CONV and PRES conditions provided two different comparisons to CESR. As an initial prototype, the CESR device has a number of disadvantages that may confound the test, including a lack of different sizes and stiffness for each participant, greater weight and less familiarity for participants who have far more experience with conventional feet. The CONV condition provided a controlled comparison with a low-profile foot also of a single size and stiffness for all participants, weight-matched the CESR and of less familiarity for participants compared to their prescribed foot. Accordingly, the PRES condition did not attempt to control for these possible confounds. While the PRES feet were all different between subjects (Table 1), this condition represented the expert opinion of the participant’s physician of the most optimal commercially available prosthetic foot, with size and stiffness individualized for each participant. Subjects were also fully acclimated to the PRES condition. Therefore, the PRES condition provided a clinically relevant benchmark for comparison. Additional prosthetic components remained consistent for all foot conditions (Table 1).
Table 1.
Prosthetic components for each participant. All participants wore total contact patellar tendon-bearing carbon laminated sockets.
| Subject | Prescribed foot/pylon | Suspension | Interface (liners) |
|---|---|---|---|
| 1 | FS1000a | Clutch lock | Alpha max medium (6 mm)e |
| 2 | Renegadea/Rotatord | Pin lock | Alpha original uniform (9 mm)e |
| 3 | Ceterusb | Suction | Alpha original uniform (6 mm)e |
| 4 | Seattle Carbon LightFoot 2™c | Pin lock | Alpha taper uniform (6 mm)e |
| 5 | Flex Footb | Pin lock | Comfort Liner (Iceross)b |
| 6 | Luxon Maxd | Pin lock | Alpha Spirite |
| 7 | Vari-flexb | Pin lock | Dermo (Iceross)b |
Freedom Innovation, Inc., Irvine, California.
Ossur, Reykjavik, Iceland.
Seattle Systems, Poulsbo, Washington.
Otto Bock, Duderstadt, Germany.
Ohio Willow Wood, Mt. Sterling, Ohio.
2.3. Data collection
To familiarize participants with the different prosthetic feet and experimental design, a training session was completed two to seven days prior to the data collection, in which participants practiced walking on the treadmill for 5 minutes with each foot condition. On a subsequent day, participants completed a data collection session which entailed walking on the CESR foot for approximately 30 extra minutes using varying spring stiffness. Results of this session are presented in a separate manuscript (Zelik et al., 2011). These two additional sessions helped the amputees get comfortable walking with the novel prosthetic foot and were done on separate days to minimize the effect of fatigue.
Anthropometric measurements were taken for each participant according to the Plug-in-Gait requirements for static and dynamic modeling (Vicon, Centennial, CO). Thirty-five 14 mm reflective markers were placed on each participant at locations consistent with Vicon’s Plug-in-Gait full-body model. Prosthetic heel, toe and lateral ankle marker placements were consistent for all foot conditions and placed on similar locations as the intact foot marker placements. Participants were fit with each foot condition in random order and given time to re-acclimate to each condition (by self-report) prior to data collection. Breath-by-breath oxygen consumption rates were collected using the Oxycon Mobile wireless ergospirometry system (CareFusion, Yorba Linda, CA). An initial baseline measurement was collected while participants stood quietly for six minutes. Participants then walked on a treadmill (belt dimension: 51 × 140 cm) at the target speed of 1.14 m/s, a typical speed for transtibial amputee gait (Robinson et al., 1977; Torburn et al., 1990) for approximately 10 minutes, until they reached steady state (3 min of consistent VO2 readings as determined by visual inspection of a real-time graph telemetered to a laptop computer throughout the data collection). Speed was controlled across conditions to minimize the confounding effects of variable speed gait on biomechanical variables (Lelas, Merriman, Riley, & Kerrigan, 2003). Participants wore a harness system as a precaution against falling, but this was kept slack to reduce interference.
Following each treadmill test, overground biomechanics data were collected for the same foot condition. The participants walked at the same controlled walking speed (1.14 ± 0.11 m/s) along a 10 m walkway, while marker trajectories were collected with a 12-camera Vicon MX System at a sampling frequency of 120 Hz and ground reaction forces were collected with four embedded force plates (2 Bertec, Columbus, OH; 2 AMTI, Watertown, MA; dimensions: 40 × 60 cm) at a sampling frequency of 1200 Hz. Six trials were collected for each condition that were within 10% of the target speed and had at least two sequential foot strikes on two separate force plates. Participants rested for approximately 5 minutes after completing overground walking trials while the prosthetist switched prosthetic feet. This protocol was repeated for each foot condition in random order.
2.4. Data analysis
Marker trajectory data were filtered with Vicon’s Woltring quintic spline algorithm with a mean-square-error value of 20 prior to standard 3D inverse dynamics computations (Winter, 1991). An additional 25 Hz 3rd-order Butterworth filter was applied after calculation of joint moments and powers. All data were normalized to subject body weight.
Inter-segmental power between the foot and shank of the prosthetic and intact limbs was calculated by summing the translational and rotational powers at the distal shank (Prince, Winter, Sjonnesen, & Wheeldon, 1994; Robertson & Winter, 1980) using custom software in MATLAB. Unlike standard inverse dynamics, this analysis technique makes no rigid body assumptions, treating the foot-ankle as a deformable body and has been suggested to be a better estimate of work associated with compliant structures and un-modeled degrees of freedom as found in prosthetic foot keels (e.g., Prince et al., 1994). Translational power was calculated as the dot product of the ground reaction force and translational velocity at the lateral malleolus ankle marker. Rotational power was calculated as the dot product of the joint moment about the lateral malleolus and the angular velocity of the shank. Push-off work at the foot-ankle was defined as the integral of positive foot-ankle power generated during the final positive region of the power curve (Fig. 2). Net work absorbed prior to pushoff was calculated as the integral of all foot-ankle power prior to push-off. In addition, we examined the three distinct regions of prosthetic foot work absorbed and generated prior to push-off as: (1) the integral of the negative power in early stance, (2) the integral of the negative power in mid to late stance, and (3) the integral of the positive power in early stance (Fig. 3). Hip and knee joint power were calculated using standard inverse dynamics techniques (i.e., from moment and angular velocity only) with Nexus software (Vicon).
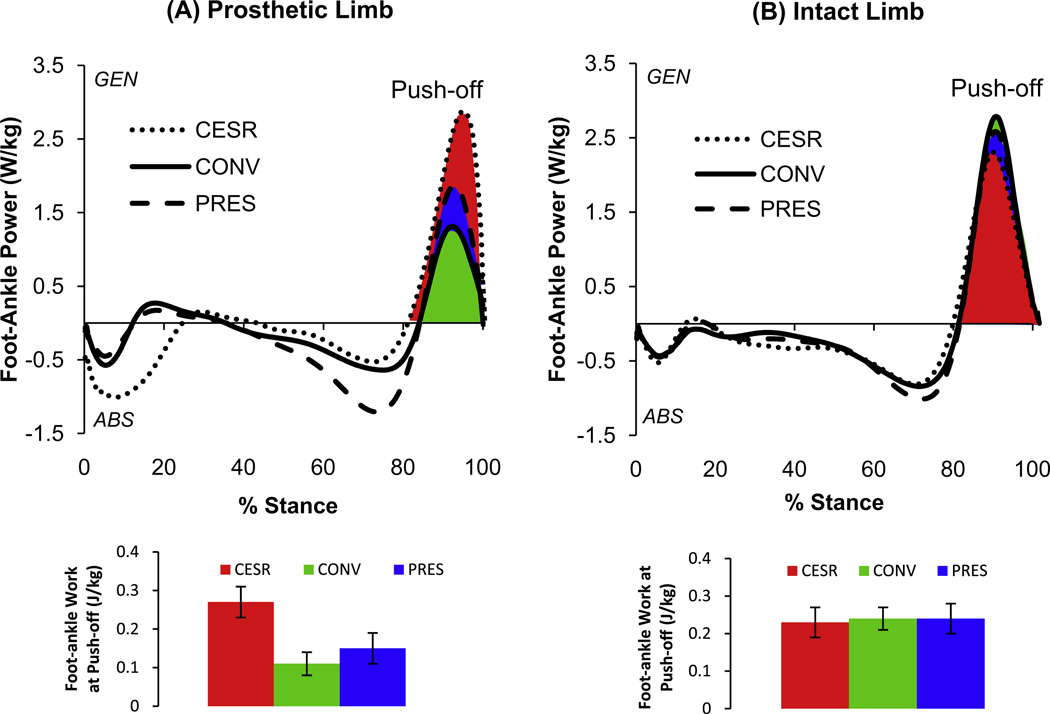
Fig. 2.
Average (n = 7) foot-ankle power (W/kg) and push-off work (J/kg) for the (A) prosthetic limb and (B) intact limb. Shaded regions indicate prosthetic foot work at push-off.
Fig. 3.
Average (n = 7) foot-ankle work for the three phases prior to push-off: (1) work absorbed in early stance, (2) work generated in early stance and (3) work absorbed mid to late stance across foot conditions.
COM work rate was calculated as the three-dimensional dot product of the ground reaction force and COM velocity independently for each limb (Donelan et al., 2002). COM velocity was calculated from ground reaction forces and gravity, assuming steady-state periodic strides. Push-off and collision work were then calculated as the time integrals of COM work rate during the push-off and collision phases of gait, respectively (Fig. 4). We estimated the total positive and negative COM work values as the time integrals of all regions of positive and negative COM work rate, respectively, across both limbs during a single stride for each foot condition. We also estimated “biological COM work rate” values by subtracting the instantaneous prosthetic foot-ankle power from the total COM work rate for each foot condition. We then estimated positive and negative “biological COM work” as the time integrals of all positive and negative regions of “biological COM work rate,” respectively. While these two quantities are computed using discrepant methods (Zelik & Kuo, 2010), their difference does yield a rough estimate of the power output of the biological leg structures, separate from the prosthesis (similar to Sawicki and Ferris (2009)).
Fig. 4.
Average (n = 7) COM Work Rate (W/kg) for the (A) prosthetic limb and (B) intact limb. The shaded regions indicate total push-off work (positive integral) and collision work (negative integral) for the prosthetic and intact limbs, respectively for each foot condition. These phases of gait associated with positive and negative fluctuations of COM work rate have been previously defined in Donelan et al. (2002) and Kuo et al. (2005).
Metabolic energy expenditure was estimated using breath-by-breath oxygen consumption rate measurements during steady-state gait (defined as the final 3 minutes of each treadmill trial). Standard indirect calorimetry equations were used to calculate metabolic rate (Brockway, 1987). Net metabolic rate was calculated by subtracting resting metabolic rate from the metabolic rate for each foot condition.
Differences across condition were determined using linear mixed effects models with foot condition (CESR, CONV, and PRES) as the fixed effect and subject as the random effect. The inclusion of random effects accounts for repeated measures within subject by enabling the estimation of both within-subject error and between-subject error. Summary statistics are presented as mean ± one standard deviation (SD). All statistical analyses were carried out using R 2.9.0 software (R Development Core Team, 2009) and overall statistical significance was set at p < .05. Post-hoc pair-wise comparisons were completed when an overall association across conditions was present. A Bonferroni correction was applied to those multiple comparisons which resulted in significance set at p < .017. Percent differences were calculated to aide with interpretation of the results using the following equation:
| (1) |
3. Results
The CESR foot demonstrated 58% and 41% increases in prosthetic foot peak mechanical power output during push-off as compared to CONV (p < .001) and PRES (p = .001), respectively. CESR also demonstrated increased total work generation in push-off (61% more than CONV; 44% more than PRES; p < .001; Table 2B, Fig. 2A). The PRES foot also produced significantly greater push-off than the CONV foot (26% increase in power, p = .016; 27% increase in work, p = .004). Intact ankle peak power was 17% lower with CESR compared to CONV (p = .013) and PRES (p = .002) conditions (Table 2B, Fig. 2B). However, intact ankle push-off work was not significantly different across conditions (p = .4). The CESR and PRES foot stored 33% (p = .013) and 42% (p = .027) more energy, respectively, prior to push-off than CONV. Although the average percent increase was larger for PRES vs. CONV, this comparison was only borderline significant with the Bonferroni correction due to a larger standard error. The timing of energy storage differed across feet. For the CESR foot, the increase in energy storage primarily occurred from 0 to 20% of stance (CESR: −0.14 ± 0.02; CONV: −0.035 ± 0.02; PRES: −0.028 ± 0.01 J/kg). Whereas the PRES condition demonstrated increased energy storage from 50 to 80% of stance (PRES: −0.25 ± 0.08; CESR: −0.086 ± 0.03; CONV: −0.14 ± 0.07), reflecting the CESR mechanism to capture and recycle heel-strike work specifically (Fig. 3; Collins & Kuo, 2010).
Table 2.
Mean [±one standard deviation] for biomechanical variables separated by limb (prosthetic and intact) and metabolic cost across foot condition (CESR, CONV and PRES). Overall statistical significance was tested first (p < .05), followed by individual pair-wise comparisons with significance set at p < .017 after a Bonferroni correction.
| CESR | CONV | PRES | Overall p-value | |
|---|---|---|---|---|
| A: Temporal parameters | ||||
| Stride length (m) | 1.42 [0.06] | 1.41 [0.06] | 1.41 [0.05] | .4 |
| Stride time (s) | 1.30 [0.06] | 1.26 [0.05] | 1.25 [0.07] | <.001a,b |
| Velocity (m/s) | 1.10 [0.05] | 1.12 [0.04] | 1.13 [0.05] | .037b |
| B: Foot- ankle | ||||
| Peak power (generated) (W/kg) | ||||
| Prosthetic | 3.2 [0.7] | 1.4 [0.3] | 1.9 [0.5] | <.001a,b,c |
| Intact | 2.4 [0.4] | 2.9 [0.6] | 2.8 [0.5] | .005a,b |
| Work at push-off (generated) (J/kg) | ||||
| Prosthetic | 0.27 [0.04] | 0.11 [0.03] | 0.15 [0.04] | <.001a,b,c |
| Intact | 0.23 [0.04] | 0.24 [0.05] | 0.24 [0.03] | .4 |
| Net work (absorbed) (J/kg) | ||||
| Prosthetic | −0.21 [0.05] | −0.14 [0.06] | −0.24 [0.08] | .04a |
| Intact | −0.26 [0.07] | −0.23 [0.05] | −0.26 [0.05] | .1 |
| C: Center of mass (COM) | ||||
| COM push-off work (J/kg) | ||||
| Prosthetic | 0.20 [0.03] | 0.09 [0.02] | 0.12 [0.02] | <.001a,b,c |
| Intact | 0.18 [0.05] | 0.20 [0.04] | 0.18 [0.03] | .3 |
| COM collision work (J/kg) | ||||
| Prosthetic | −0.13 [0.04] | −0.11 [0.06] | −0.11 [0.05] | .3 |
| Intact | −0.065 [0.03] | −0.16 [0.09] | −0.12 [0.04] | .003a,b |
| Biological COM work across stance (J/kg) | ||||
| Positive | 0.45 [0.11] | 0.58 [0.13] | 0.54 [0.12] | .002a |
| Negative | −0.60 [0.17] | −0.63 [0.19] | −0.53 [0.14] | .014c |
| Total COM work across stance (J/kg) | ||||
| Positive | 0.66 [0.15] | 0.67 [0.18] | 0.64 [0.13] | .4 |
| Negative | −0.76 [0.18] | −0.75 [0.21] | −0.72 [0.16] | .4 |
| D: Metabolic cos | ||||
| Net metabolic rate (W/kg) | 3.45 [0.59] | 3.13 [0.33] | 2.97 [0.15] | .023b |
Significant difference between CESR and CONV (p < .017).
Significant difference between CESR and PRES (p < .017).
Significant difference between CONV and PRES (p < .017).
Mechanical work on the COM during prosthetic limb push-off was 55% and 40% greater (p < .001) for CESR compared to CONV and PRES conditions, respectively. PRES was also 25% greater (p < .001) than CONV (Table 2C, Fig. 4A). The corresponding contra-lateral intact limb COM collision work was reduced for CESR compared to both CONV (59% reduction, p = .004) and PRES (46% reduction, p = .001) (Table 2C, Fig. 4B). The biological contribution of the positive COM work for CESR was reduced compared to CONV (17% reduction, p < .002). A similar trend was apparent for CESR compared to PRES, but this comparison did not reach statistical significance (15% reduction, p = .023). For the biological contribution of the total negative COM work, CONV demonstrated significantly more work absorbed compared to PRES (16% increase, p = .014). A similar trend was found for CESR compared to PRES, but this comparison did not reach statistical significance (12% increase, p = .021). However, total positive and total negative COM work across a complete gait cycle was the same across foot conditions (Table 2C).
Hip and knee joint powers were examined qualitatively to assess whether large compensations were present at more proximal joints for the CESR foot. Average hip power for both the prosthetic (Fig. 5A) and intact (Fig. 5B) limbs appeared similar across conditions, except for a slight decrease in H2 and additional burst of power (H3) for the CESR prosthetic limb in early swing phase (Fig. 5A). Larger differences seemed to occur at the knee. Prosthetic limb peak negative and positive knee power appeared to increase for CESR at approximately 35% and 45% of the gait cycle, respectively, as well as an increase in K3 in early swing phase compared to CONV and PRES. (Fig. 6A). Finally, a decrease in both K1 and K2 power bursts was apparent for the CESR foot intact limb compared to CONV and PRES conditions (Fig. 6B), similar to the differences in intact limb COM work rate (Fig. 4).
Fig. 5.
Average (n = 7) sagittal plane hip power (W/kg) for the (A) prosthetic limb and (B) intact limb. H1–3 refer to specific peaks defined in Winter (1983) and Winter and Sienko (1988).
Fig. 6.
Average (n = 7) sagittal plane knee power (W/kg) for the (A) prosthetic limb and (B) intact limb. K1–4 refer to specific peaks defined in Winter (1983) and Winter and Sienko (1988).
The net metabolic energy cost (Table 2D) of CESR was 8.3% greater than CONV, but this difference did not reach statistical significance (p = .078). However, CESR was greater than PRES, with an average net increase in metabolic expenditure of 12.1% (p = .007). The average percent increase of CONV over PRES was 4.6%, though this difference was not significantly different (p = .3).
Participants walked at equivalent stride lengths across all foot conditions, with a slightly longer stride time (3% increase) and slightly slower speed (1.8% reduction) when walking overground with the CESR foot (Table 2A).
4. Discussion
We compared transtibial amputees walking at a constant speed with each of three different prosthetic feet: a controlled energy storage and return (CESR) foot, a standard weight-matched conventional (CONV) foot and the participants’ own prescribed (PRES) foot using a within-subject, randomized study design. Our results revealed increased prosthetic limb push-off power and push-off work as well as increased prosthetic limb COM push-off work and reduced intact limb COM collision work with the CESR foot compared to CONV and PRES conditions. Despite the fact that the biological contribution of the positive COM work over the full gait cycle with the CESR foot was significantly reduced compared to CONV, the metabolic cost was not significantly improved for the CESR foot compared with CONV and was higher than the PRES condition. These results suggest that prosthetic push-off can be increased with a controlled energy storage and return prosthetic foot, reducing the biological contributions to the positive COM work. However, other factors appear to interfere with the amputee’s ability to use this energy, a common challenge when integrating a mechanical device with the human body (Gitter et al., 1991; Sawicki & Ferris, 2008).
Our results demonstrate how amputee foot-ankle mechanics can be altered as a result of changes in mechanical foot design. A more than two-fold increase in amputee prosthetic foot peak push-off power and push-off work was evident for the CESR foot compared to CONV, with power and work magnitudes similar to the contra-lateral intact ankle (Fig. 2). This was consistent with the results of non-amputees wearing the CESR foot with a simulator boot (Collins & Kuo, 2010). The increase in push-off was the result of increased energy storage during the loading phase combined with the unique release features of the CESR foot in later stance, just prior to push-off. A smaller but still statistically significant increase in peak push-off power and push-off work also occurred for CESR compared to PRES.
Unlike other energy storing prosthetic feet, the CESR foot is intended to primarily capture energy from the collision of the prosthetic limb with the ground. Indeed, net prosthetic foot work absorbed in early stance was more than three times greater for CESR compared to CONV and PRES (Fig. 3). In contrast, the CESR foot demonstrated 65% and 40% less energy absorption in later stance (across 40–80% of stance) compared with PRES and CONV, respectively. Alterations in the timing of energy absorption are the result of differences in the design of the CESR compared with PRES feet. The PRES feet have more compliant keel designs, resulting in greater energy storage from mid- to late-mid stance. Despite the difference in timing of foot-ankle absorption, there was no apparent compensation for the prosthetic limb hip and knee powers across foot conditions during the same phase of the gait cycle (early stance, Figs. 5A and 6A). Despite the lack of evidence that adaptation occurred related to the proximal positive work performed, we suspect that undetected compensations such as isometric and co-contractions of the quadriceps may have been employed to stabilize the knee during this large energy absorption. One possible solution to address these compensations may be to reduce the energy storage in early stance with a different heel spring in the CESR foot and increase it later in stance with a more compliant forefoot keel, thereby better mimicking intact ankle mechanics. This may lead to an improved balance of early and mid-stance energy absorption throughout stance, less compensation and more optimal energy return and rate of return of push-off.
The CESR foot increased COM push-off work of the prosthetic limb and reduced COM collision work of the intact limb as compared to CONV, which were consistent with both dynamic walking model-based predictions (Kuo, 2002; Ruina et al., 2005) and with the results of non-amputees wearing the CESR foot (Collins & Kuo, 2010). This finding adds to the empirical evidence that supports a correlation between increased COM push-off work and decreased contralateral limb collision in humans (Collins & Kuo, 2010; Houdijk et al., 2009; van Engelen et al., 2010). The decrease in positive biological COM work across a full gait cycle for CESR provides further evidence in support of the models that predict that balanced step-to-step transition work will reduce overall mechanical work requirements (Kuo, 2002; Kuo et al., 2005; Ruina et al., 2005). Despite increased energy absorption by the CESR foot in early prosthetic stance, there was no change to the prosthetic limb COM collision work for CESR (Fig. 4A). However, there was an apparent increase in the duration of COM collision for CESR. Therefore, adjustments in the spring properties to tune the timing and magnitude of the prosthetic foot work absorbed in early stance may minimize costly compensations and potentially lead to overall improvements in amputee gait.
The lack of reduction in metabolic cost for CESR despite increased prosthetic foot-ankle and COM push-off work and reduced biological COM work may be the result of additional muscular work not captured by measurements of mechanical work (Cavanagh & Kram, 1985; Eng & Winter, 1995; Gitter et al., 1991; Williams, 1985). Factors other than COM work or joint work have been shown to contribute to metabolic energy expenditure (Adamczyk, Collins, & Kuo, 2006; Houdijk et al., 2009; van Engelen et al., 2010; Vanderpool, Collins, & Kuo, 2008). Based on qualitative observation, we suspect that metabolically costly muscular co-contraction across the knee joint was present to enhance stability during loading. Increased absorption at the knee in late stance (Fig. 6A: K3) may have also diminished the energy transfer from the prosthesis to the COM. This increase in negative knee work may have led to compensations at the hip (Fig. 5A: H3 power burst) for CESR versus CONV, which may be an indicator of excessive push-off. Furthermore, the reduced foot-ankle work absorbed from mid to late stance for CESR (Fig. 3) as compared to the intact limb ankle mechanics (Fig. 2B), may suggest that the prosthetic keel was too stiff, leading to non-optimal deformation of the prosthetic foot across stance and reduced foot function (Hansen, Childress, & Knox, 2000). These altered foot mechanics may have contributed to the apparent increase in knee power for CESR (Fig. 6A) as compared to the other foot conditions, which occurred at a similar time in the gait cycle (mid-stance). Amputees might also have had more difficulty adapting to the more complex dynamics of the CESR foot, despite two training sessions. It has been shown to take as many as 21 days of acclimation to a novel prosthesis for measurable changes in metabolic cost to occur (Grabowski et al., 2010). Therefore, longer acclimation time may be necessary to elicit reduced metabolic cost while walking with a novel prosthesis.
Our metabolic results are not in complete agreement with the results from non-amputees reported previously (Collins & Kuo, 2010). The non-amputee participants in this study demonstrated reduced metabolic cost while walking on the CESR prototype compared to the CONV condition. This disparity may be due to the inherent differences between populations (Zelik et al., 2011) and protocols. For example, the residual limb-socket interface is likely less stiff than the rigid prosthesis simulator boot and therefore, may have been less capable of effectively transferring energy. The non-amputees were also younger in age and walked faster. Finally, since amputees are more accustomed to their prescribed feet, they may have been relatively more adapted to walking on the similar CONV foot than the CESR foot compared with the non-amputees, who had equal acclimation time for both prosthetic feet using the simulator. Therefore, the amputee’s added experience with a CONV style foot may have caused a bias in favor of this condition, which was not apparent with the non-amputee population. The combination of these factors may have resulted in the non-amputees being better suited to adapt and benefit from the increased push-off of the CESR foot.
The following limitations should be noted when interpreting the results of this study. Though the prosthetic foot work calculations used in this study capture the behavior of non-rigid segments better than standard inverse dynamics, they are still sensitive to some forms of measurement error that may affect the absolute calculated magnitudes of each variable. Such metrics should be used in conjunction with other, corroborating measures when possible. Also, the estimate of biological COM work should not be considered absolute, since there is a known discrepancy between COM work and joint work computations, especially for negative work (Kuo et al., 2005; Zelik & Kuo, 2010). However, all conditions should suffer similarly from this problem, so relative comparisons are expected to be valid. Furthermore, the number of participants included in the protocol was relatively small, due in part to the demands of a study design that requires multiple laboratory visits and recruitment of a population of only active traumatic amputees with at least two years of experience walking with a prosthesis. Due to the high inter-subject variability associated with metabolic data, a larger sample population may have been necessary for the metabolic assessment. Further analysis with a larger population may serve to identify whether certain subjects can benefit more from this type of novel prosthesis. Finally, comparison of CONV and CESR conditions with PRES may indicate how practical, experimental limitations can affect results. It is typical for amputees to be prescribed a relatively lightweight prosthesis with size and stiffness selected for their body weight, stature and activity level. In testing a relatively heavy initial prototype, it was not practical to individualize the CESR condition for each subject, nor feasible to provide longer acclimation periods at this time. We attempted to subject the CONV condition to similar constraints to serve as a controlled comparison, although the passive CONV foot was more similar to the PRES feet and also less optimal. It is therefore not unexpected that average energy expenditure was lower on the PRES foot. The PRES condition is a clinically relevant comparison that serves as an indicator of the possible gains through individualized prescription and seems to be within reach for improvement in future prosthetic feet.
5. Conclusions
In conclusion, transtibial amputees wearing the CESR foot demonstrated the ability to restore pushoff energy on their prosthetic limb and reduce collision on their contra-lateral intact limb during constant speed ambulation; however, there was not a corresponding reduction in metabolic rate. The rate of release of the energy and its associated need for greater muscle work to control the energy release, or possibly inadequate adaptation time may have interfered with the amputees’ ability to use this energy. Future generations of this technology should focus on optimizing the foot characteristics to minimize compensatory strategies involving ineffective contractions, which may ultimately lead to overall systemic improvements during daily ambulation.
Acknowledgments
This research was supported by the Department of Veterans Affairs, Rehabilitation Research and Development Service (A4372R). Other funding sources included the National Institutes of Health (HD055706), the Department of Defense (DR081177) and the National Science Foundation (Grant 0450646 and Graduate Student Research Fellowship). Statistical analyses were performed by Jane B. Shofer, MS. Prosthetic adjustments were performed by Wayne Biggs, CPO.
Footnotes
Conflict of interest
Drs. Adamczyk and Collins are part-owners of Intelligent Prosthetic Systems, LLC, which was incorporated to perform research and development related to the CESR foot. None of the data presented here are proprietary. Foot prostheses based on this technology are under development, but none are commercially available.
References
- Adamczyk PG, Collins SH, Kuo AD. The advantages of a rolling foot in human walking. Journal of Experimental Biology. 2006;209:3953–3963. doi: 10.1242/jeb.02455. [DOI] [PubMed] [Google Scholar]
- Au SK, Weber J, Herr H. Powered ankle-foot prosthesis improves amputee walking metabolic economy. IEEE Transactions on Robotics. 2009;25:51–57. [Google Scholar]
- Barr AE, Siegel KL, Danoff JV, McGarvey CL, Tomasko A, Sable I, et al. Biomechanical comparison of the energy-storing capabilities of SACH and Carbon Copy II prosthetic feet during the stance phase of gait in a person with below-knee amputation. Physical Therapy. 1992;72:344–354. doi: 10.1093/ptj/72.5.344. [DOI] [PubMed] [Google Scholar]
- Barth DG, Schumacher L, Thomas SS. Gait analysis and energy cost of below-knee amputees wearing six different prosthetic feet. Journal of Prosthetics and Orthotics. 1992;4:63–75. [Google Scholar]
- Brockway JM. Derivation of formulae used to calculate energy expenditure in man. Human Nutrition: Clinical Nutrition. 1987;41C:463–471. [PubMed] [Google Scholar]
- Cavanagh PR, Kram R. Mechanical and muscular factors affecting the efficiency of human movement. Medicine and Science in Sports and Exercise. 1985;17:326–331. [PubMed] [Google Scholar]
- Collins SH, Kuo AD. Recycling energy to restore impaired ankle function during human walking. PLoS One. 2010;5:e9307. doi: 10.1371/journal.pone.0009307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donelan JM, Kram R, Kuo AD. Mechanical work for step-to-step transitions is a major determinant of the metabolic cost of human walking. Journal of Experimental Biology. 2002;205:3717–3727. doi: 10.1242/jeb.205.23.3717. [DOI] [PubMed] [Google Scholar]
- Ehde DM, Czerniecki JM, Smith DG, Campbell KM, Edwards WT, Jensen MP, et al. Chronic phantom sensations, phantom pain, residual limb pain and other regional pain after lower limb amputation. Archives of Physical Medicine and Rehabilitation. 2000;81:1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- Eng JJ, Winter DA. Kinetic analysis of the lower limbs during walking: What information can be gained from a three-dimensional model? Journal of Biomechanics. 1995;28:753–758. doi: 10.1016/0021-9290(94)00124-m. [DOI] [PubMed] [Google Scholar]
- Gailey R, Allen K, Castles J, Kucharik J, Roder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. Journal of Rehabilitation Research and Development. 2008;45:15–29. doi: 10.1682/jrrd.2006.11.0147. [DOI] [PubMed] [Google Scholar]
- Genin JJ, Bastien GJ, Franck B, Detrembleur C, Willems PA. Effect of speed on the energy cost of walking in unilateral traumatic lower limb amputees. European Journal of Applied Physiology. 2008;103:655–663. doi: 10.1007/s00421-008-0764-0. [DOI] [PubMed] [Google Scholar]
- Gitter A, Czerniecki JM, de Groot DM. Biomechanical analysis of the influence of prosthetic feet on below-knee amputee walking. American Journal of Physical Medicine and Rehabilitation. 1991;70:142–148. doi: 10.1097/00002060-199106000-00006. [DOI] [PubMed] [Google Scholar]
- Grabowski AM, Rifkin J, Kram R. K3 Promoter™ prosthetic foot reduces the metabolic cost of walking for unilateral transtibial amputees. Journal of Prosthetics and Orthotics. 2010;22:113–120. [Google Scholar]
- Hafner BJ, Sanders JE, Czerniecki J, Fergason J. Energy storage and return prostheses: Does patient perception correlate with biomechanical analysis? Clinical Biomechanics. 2002;17:325–344. doi: 10.1016/s0268-0033(02)00020-7. [DOI] [PubMed] [Google Scholar]
- Hansen AH, Childress DS, Knox EH. Prosthetic foot roll-over shapes with implications for alignment of transtibial prostheses. Prosthetics and Orthotics International. 2000;24:205–215. doi: 10.1080/03093640008726549. [DOI] [PubMed] [Google Scholar]
- Houdijk H, Pollman E, Groenewold M, Wiggerts H, Polomski W. The energy cost for the step-to-step transition in amputee walking. Gait and Posture. 2009;30:35–40. doi: 10.1016/j.gaitpost.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Hsu MJ, Nielsen DH, Lin-chan ST, Shurr D. The effects of prosthetic foot design on physiologic measurements, self-selected walking velocity and physical activity in people with transtibial amputations. Archives of Physical Medicine and Rehabilitation. 2006;87:123–129. doi: 10.1016/j.apmr.2005.07.310. [DOI] [PubMed] [Google Scholar]
- Kuo AD. Energetics of actively powered locomotion using the simplest walking model. Journal of Biomechanical Engineering. 2002;124:113–120. doi: 10.1115/1.1427703. [DOI] [PubMed] [Google Scholar]
- Kuo AD, Donelan JM, Ruina A. Energetic consequences of walking like an inverted pendulum: Step-to-step transitions. Exercise and Sport Science Reviews. 2005;33:88–97. doi: 10.1097/00003677-200504000-00006. [DOI] [PubMed] [Google Scholar]
- Lehmann JF, Price R, Boswell-Bessette S, Dralle A, Questad K. Comprehensive analysis of dynamic elastic response feet: Seattle Ankle/Lite Foot versus SACH foot. Archives of Physical Medicine and Rehabilitation. 1993;74:853–861. doi: 10.1016/0003-9993(93)90013-z. [DOI] [PubMed] [Google Scholar]
- Lelas JL, Merriman GJ, Riley PO, Kerrigan DC. Predicting peak kinematic and kinetic parameters from gait speed. Gait and Posture. 2003;17:106–112. doi: 10.1016/s0966-6362(02)00060-7. [DOI] [PubMed] [Google Scholar]
- Perry J, Shanfield S. Efficiency of dynamic elastic response prosthetic feet. Journal of Rehabilitation Research and Development. 1993;30:137–143. [PubMed] [Google Scholar]
- Powers CM, Torburn L, Perry J, Ayyappa E. Influence of prosthetic foot design on sound limb loading in adults with unilateral below-knee amputations. Archives of Physical Medicine and Rehabilitation. 1994;75:825–829. [PubMed] [Google Scholar]
- Prince F, Winter DA, Sjonnesen G, Wheeldon RK. A new technique for the calculation of the energy stored, dissipated and recovered in different ankle-foot prostheses. IEEE Transactions on Rehabilitation Engineering. 1994;2:247–255. [Google Scholar]
- R Development Core Team. R Foundation for Statistical Computing. Vienna, Austria: 2009. R: A language and environment for statistical computing. ISBN 3-900051-07-0, URL: http://www.R-project.org. [Google Scholar]
- Robertson DGE, Winter DA. Mechanical energy generation absorption and transfer amongst segments during walking. Journal of Biomechanics. 1980;13:845–854. doi: 10.1016/0021-9290(80)90172-4. [DOI] [PubMed] [Google Scholar]
- Robinson JL, Smidt GL, Arora JS. Accelerographic, temporal, and distance gait factors in below-knee amputees. Physical Therapy. 1977;57:898–904. doi: 10.1093/ptj/57.8.898. [DOI] [PubMed] [Google Scholar]
- Romo HD. Specialized prostheses for activities: An update. Clinical Orthopedics. 1999;361:63–70. doi: 10.1097/00003086-199904000-00009. [DOI] [PubMed] [Google Scholar]
- Ruina A, Bertram JEA, Srinivasan M. A collisional model of the energetic cost of support work qualitatively explains leg sequencing in walking and galloping, pseudo-elastic leg behavior in running and the walk-to-run transition. Journal of Theoretical Biology. 2005;237:170–192. doi: 10.1016/j.jtbi.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Sawicki GS, Ferris DP. Mechanics and energetic of level walking with powered ankle exoskeletons. Journal of Experimental Biology. 2008;211:1402–1413. doi: 10.1242/jeb.009241. [DOI] [PubMed] [Google Scholar]
- Sawicki GS, Ferris DP. Powered ankle exoskeletons reveal the metabolic cost of plantar flexor mechanical work during walking with longer steps at constant step frequency. Journal of Experimental Biology. 2009;212:21–31. doi: 10.1242/jeb.017269. [DOI] [PubMed] [Google Scholar]
- Seroussi RE, Gitter A, Czerniecki JM, Weaver K. Mechanical work adaptations of above-knee amputee ambulation. Archives of Physical Medicine and Rehabilitation. 1996;77:1209–1214. doi: 10.1016/s0003-9993(96)90151-3. [DOI] [PubMed] [Google Scholar]
- Snyder RD, Powers CM, Fontaine C, Perry J. The effect of five prosthetic feet on the gait and loading of the sound limb in dysvascular below-knee amputees. Journal of Rehabilitation Research and Development. 1995;32:309–315. [PubMed] [Google Scholar]
- Struyf PA, van Heugten CM, Hitters MW, Smeets RJ. The prevalence of osteoarthritis of the intact hip and knee among traumatic leg amputees. Archives of Physical Medicine and Rehabilitation. 2009;90:440–446. doi: 10.1016/j.apmr.2008.08.220. [DOI] [PubMed] [Google Scholar]
- Torburn L, Perry J, Ayyappa E, Shanfield SL. Below-knee amputee gait with dynamic elastic response prosthetic feet: A pilot study. Journal of Rehabilitation Research and Development. 1990;27:369–384. doi: 10.1682/jrrd.1990.10.0369. [DOI] [PubMed] [Google Scholar]
- van der Linde H, Hofstad CJ, Guerts ACH, Postema K, Geertzen JHB, van Limbeek J. A systematic literature review of the effect of different prosthetic components on human functioning with a lower limb prosthesis. Journal of Rehabilitation Research and Development. 2004;41:555–570. doi: 10.1682/jrrd.2003.06.0102. [DOI] [PubMed] [Google Scholar]
- van Engelen SJ, Wajer QE, van der Platt LW, Doets HC, van Dijk CN, Houdijk H. Metabolic cost and mechanical work during walking after tibiotalar arthrodesis and the influence of footwear. Clinical Biomechanics. 2010;25:809–815. doi: 10.1016/j.clinbiomech.2010.05.008. [DOI] [PubMed] [Google Scholar]
- Vanderpool MT, Collins SH, Kuo AD. Ankle fixation need not increase the energetic cost of human walking. Gait and Posture. 2008;28:427–433. doi: 10.1016/j.gaitpost.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Versluys R, Beyl P, van Damme M, Desomer A, van Ham R, Lefeber D. Prosthetic feet: State-of-the-art review and the importance of mimicking human ankle-foot biomechanics. Disability and Rehabilitation: Assistive Technology. 2009;4:65–75. doi: 10.1080/17483100802715092. [DOI] [PubMed] [Google Scholar]
- Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait and Posture. 1999;9:207–231. doi: 10.1016/s0966-6362(99)00009-0. [DOI] [PubMed] [Google Scholar]
- Waters RL, Perry J, Antonelli D, Hislop H. Energy cost of amputees: The influence of level of amputation. Journal of Bone and Joint Surgery America. 1976;58:42–46. [PubMed] [Google Scholar]
- Williams KR. The relationship between mechanical and physiological energy estimates. Medicine and Science in Sports and Exercise. 1985;17:317–325. [PubMed] [Google Scholar]
- Winter DA. Energy generation and absorption at the ankle and knee during fast, natural and slow cadences. Clinical Orthopaedics and Related Research. 1983;175:147–154. [PubMed] [Google Scholar]
- Winter DA. The biomechanics and motor control of human gait: Normal, elderly and pathological. Waterloo: University of Waterloo Press; 1991. [Google Scholar]
- Winter DA, Sienko SE. Biomechanics of below-knee amputee gait. Journal of Biomechanics. 1988;21:361–367. doi: 10.1016/0021-9290(88)90142-x. [DOI] [PubMed] [Google Scholar]
- Zelik KE, Collins SH, Adamczyk PG, Segal AD, Klute GK, Morgenroth DC, Hahn ME, Orendurff MS, Czerniecki JM, Kuo AD. Systematic variation of prosthetic foot spring affects center-of-mass mechanics and metabolic cost during walking. IEEE TNSRE. 2011 doi: 10.1109/TNSRE.2011.2159018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelik KE, Kuo AD. Human walking isn’t all hard work: Evidence of soft tissue contribution to energy dissipation and return. Journal of Experimental Biology. 2010;213:4257–4264. doi: 10.1242/jeb.044297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation. 2008;89:422–429. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]