Abstract
Purpose:
The purpose was to evaluate subjective quality of vision and patient satisfaction after laser in situ keratomileusis (LASIK) for myopia and myopic astigmatism.
Patients and Methods:
A self-administered patient questionnaire consisting 29 items was prospectively administered to LASIK patients at the Yemen Magrabi Hospital. Seven scales covering specific aspects of the quality of vision were formulated including; global satisfaction; quality of uncorrected and corrected vision; quality of night vision; glare; daytime driving and; night driving. Main outcome measures were responses to individual questions and scale scores and correlations with clinical parameters. The scoring scale ranged from 1 (dissatisfied) to 3 (very satisfied) and was stratified in the following manner: 1-1.65 = dissatisfied; 1.66-2.33 = satisfied and; 2.33-3 = very satisfied. Data at 6 months postoperatively are reported.
Results:
This study sample was comprised of 200 patients (122 females: 78 males) ranging in age from 18 to 46 years old. The preoperative myopic sphere was − 3.50 ± 1.70 D and myopic astigmatism was 0.90 ± 0.82 D. There were 96% of eyes within ± 1.00 D of the targeted correction. Postoperatively, the uncorrected visual acuity was 20/40 or better in 99% of eyes. The mean score for the overall satisfaction was 2.64 ± 0.8. A total of 98.5% of patients was satisfied or very satisfied with their surgery, 98.5% considered their main goal for surgery was achieved. Satisfaction with uncorrected vision was 2.5 ± 0.50. The main score for glare was 1.98 ± 0.7 at night. Night driving was rated more difficult preoperatively by 6.2%, whereas 79% had less difficulty driving at night.
Conclusion:
Patient satisfaction with uncorrected vision after LASIK for myopia and myopic astigmatism appears to be excellent and is related to the residual refractive error postoperatively.
Keywords: Laser In Situ Keratomileusis, Myopia, Patient Satisfaction, Refractive Surgery, Yemen
INTRODUCTION
In recent years, a number of possible surgical procedures in ophthalmology has offered prospective patients an alternative to wear spectacles or contact lenses.1 Several laser and nonlaser refractive surgical procedures have been used to modify the shape of the cornea and correct myopia, hyperopia, astigmatism, and presbyopia. Introduction of the excimer laser to reshape the cornea has resulted in remarkable developments in the correction of these refractive errors. Combined with other advanced ophthalmic instruments, laser refractive eye surgery has resulted in a substantial increase in the safety, efficacy, and predictability of surgical outcomes.1
Laser in situ keratomileusis (LASIK) surgery is one of the most common surgeries performed worldwide.2,3 Refractive surgery has enabled individuals to enter occupations they were previously precluded from due to their vision. It is well-recognized that LASIK surgery can correct refractive errors and reduce dependence on eyeglasses or contact lenses.4 In addition, patient satisfaction following LASIK is commonly reported as high and studies of the visual and refractive outcome of LASIK for the treatment of myopia and astigmatism have reported great success.5,6,7
Laser in situ keratomileusis has become one of the most popular procedures for the reduction or elimination of myopic refractive errors and has emerged as the refractive corneal surgical procedure of choice for the correction of myopia.8
Patient satisfaction is considered as a measure of the quality of treatment, and there is a documented relationship between patient satisfaction and the utilization of a medical service.3 Patient satisfaction after LASIK ranges from 82% to 98%.6,7,8 Therefore, satisfaction studies can provide important feedback about the quality of care and outcomes, which in turn allows the medical provider to improve the services offered.5 Until date, there have been no studies that have specifically evaluated the quality of life and patient satisfaction after LASIK in the Middle East. This study assesses subjective patient satisfaction, self-perceived outcomes, and subjective visual improvement after LASIK for the correction of myopia and myopic astigmatism.
PATIENTS AND METHODS
Study design and setting
The study was approved by the Research and Ethics Committee of the Yemen Magrabi Hospital, Sana’a, Yemen. The study was performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional), and concurred with the Helsinki declaration of 1975, as revised in 2000. The risk of the surgery was fully explained to the patients in accordance with the Helsinki declaration, and verbal informed consent was obtained.
This prospective hospital-based study was performed to assess the functional outcomes and patient satisfaction after LASIK for the treatment of myopia and myopic astigmatism. The LASIK procedure was performed by two experienced ophthalmic surgeons. Treatments were performed at the Yemen Magrabi Hospital in Sana’a. The study sample was comprised of 200 consecutive patients (122 females and 78 males) enrolled from February 2009 to May 2010. Patients were aged 18-46 years old. Patient follow-up data are reported at 6 months after LASIK. The study protocol allowed planned undercorrections or overcorrections of ± 1.00D.
Patient selection
The inclusion criteria were −1.0-−8.0D of myopia (manifest refraction spherical equivalent [SE]). And −4.25D of myopic astigmatism or less. Soft contact lens wearers were advised to stop wearing lenses 3 days before the examination; rigid contact lenses were advised to stop wearing lenses 2 weeks before the examination. Patient had have a stable refraction, defined as <0.5D of change over at least 1-year. Patients had to provide verbal informed consent to be included in the study. Corneal topography was performed in all cases to rule out the keratoconus, keratoconus suspect, and pellucid marginal degeneration. Patients with a calculated residual stromal depth <300 mm were excluded from surgery.
Examination protocol
A standardized examination protocol was followed in all patients. Patients were examined preoperatively, 1-day, 1-week, 1-month, and at 6 months postoperatively. Preoperative and 6 months postoperative data are reported here. Preoperative and 6 month postoperative examinations included measurement of uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA) (projector chart [feet system], Nidek Co. Ltd., Gamagori, Japan), noncycloplegic and cycloplegic refraction (ARK-700 auto-refracto-keratometer, Nidek Co. Ltd., Gamagori, Japan), and subjective refractions with a trial lens set. Subjective patient satisfaction and evaluation of the visual outcome postoperatively were assessed by patients completing a survey questionnaire at 6 months postoperatively. The NIDEK EC-5000 excimer laser (NIDEK Co. Ltd., Gamagori, Japan) was used for all treatments. The Moria M2 microkeratome (Moria Co., Antony, France) was used to create a superiorly hinged flap with a 90 mm depth plate producing flap thickness of 90-120 mm. The NIDEK US 1000 pachymeter (NIDEK Co. Ltd., Gamagori, Japan) was used to measure flap thickness.
Questionnaire
The patient questionnaire was developed and validated by expert review of three ophthalmologists active in the field and has been used to evaluate subjective patient satisfaction and self-perceived outcomes after LASIK surgery for the correction of myopia and myopic astigmatism. The questionnaire was translated from the original English version to Arabic. The questionnaire was proven to be reliable by a relatively high level of internal consistency with a Cronbach ά coefficient superior or equal to 0.7. For statistical purposes, the 29 items on the questionnaire were grouped into seven distinct scales that were self-reported by the patients. The scoring on the scale increased with increasing satisfaction, ranging from 1 (dissatisfied) to 3 (very satisfied) and was stratified in the following manner: 1-1.65 = dissatisfied; 1.66-2.33 = satisfied and; 2.33-3 = very satisfied. Each of the seven scales covered a specific aspect of the quality of vision including global satisfaction, quality of uncorrected and corrected vision, quality of night vision, glare, daytime driving and night driving.
Data analysis
Statistical analysis was performed using the Statistical Package for Social Sciences version 11.5 (IBM Corp., New York, NY, USA). For statistical purposes, UCVA and BSCVA of the better eye in the decimal system were used for calculation. The t-test was used to compare parameters. Correlation between the patient questionnaire scores and clinical parameters was assessed with the Pearson coefficient of correlation (r). The strength of the correlation between two variables was defined as strong (r ≥ 0.60), moderate (0.30 ≤ r < 0.60), or weak (0.10 ≤ r < 0.30). The mean ± standard deviation are reported in this study. A P < 0.05 was considered as statistically significant.
RESULTS
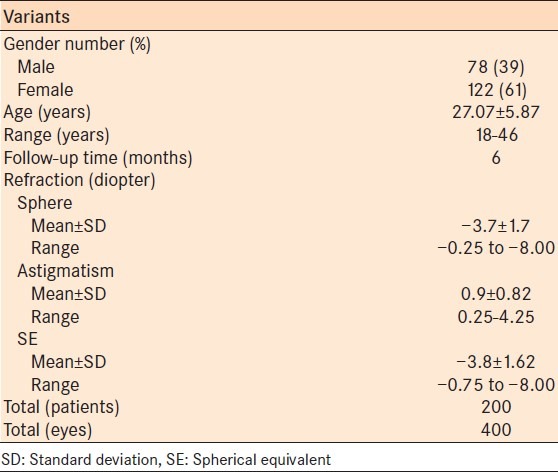
Population demographics and characteristics are listed in Table 1. The mean patient age was 27.07 ± 5.87 (range, 18-46 years).
Table 1.
Demographics and characteristics patients who underwent laser in situ keratomileusis for myopia and myopic astigmatism
Preoperative distribution of myopia
There were 188 (47.0%), patients with myopia ranging from −0.50 to −3.00 D, 184 (46.0%) patients with myopia from −3.25 to −6.00 daccounted and 28 (7.0%) patients with myopia between −6.25 and −8.00 D.
Motivation for laser in situ keratomileusis
The most frequently reported motivation for desiring surgical correction of refractive error was to reduce dependence on glasses (176, 88.0% patients), to improve UCVA (118, 59.0% patients), for job-related issues (31, 15.5% patients) and problems handling contact lenses (28, 14.0% patients).
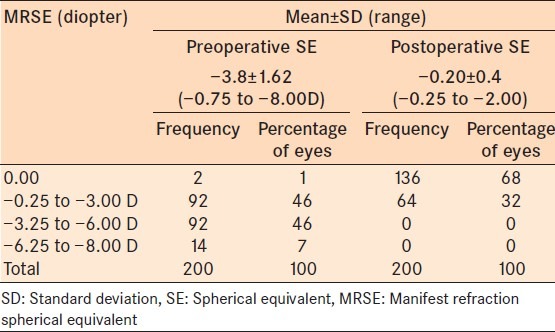
Refraction
The mean postoperative SE was −0.20 ± 0.4D (range −0.25 to -2.00 D). The mean postoperative sphere was −0.12 ± 0.32 D (range −0.75 to -1.75 D) and the mean postoperative astigmatism was 0.1 ± 0.23 D (range 0.25−1.75 D).
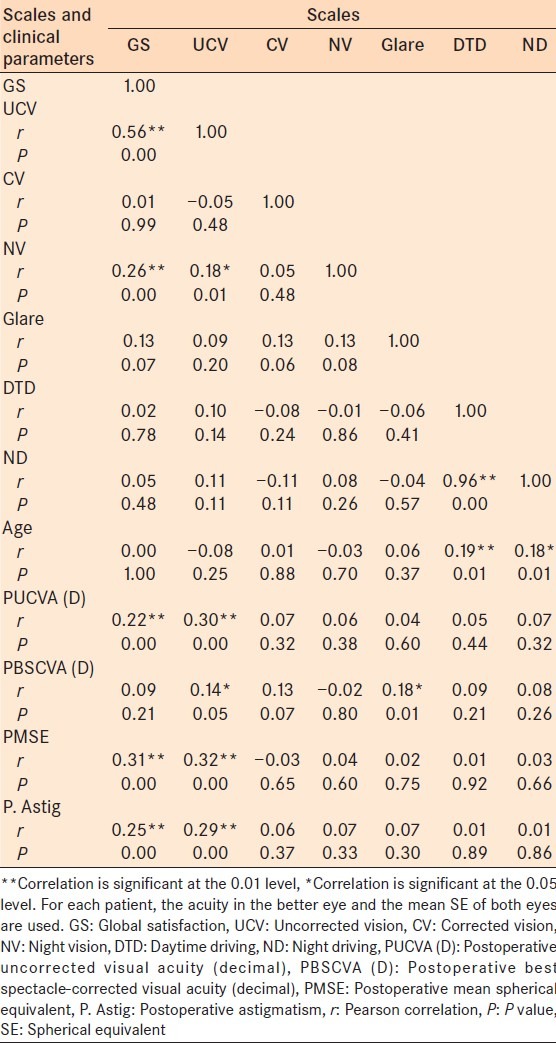
Preoperative mean SE and postoperative UCVA had a significant correlation (r) of 0.340 (P = 0.000). The correlation between preoperative mean astigmatism and postoperative UCVA was significant at 0.273 (P = 0.000). There was a significant correlation between uncorrected vision and the postoperative SE (r = 0.32, P = 0.000), postoperative astigmatism (r = 0.29, P = 0.000), and postoperative UCVA (r = 0.30, P = 0.000). There were 96% of eyes within ± 1.00 D and 87% within ± 0.50 D of the targeted correction.
Table 2 presents the frequency and percentage distributions of the change in BSCVA.
Table 2.
Frequency and percentages distributions of change in BSCVA of the better eye
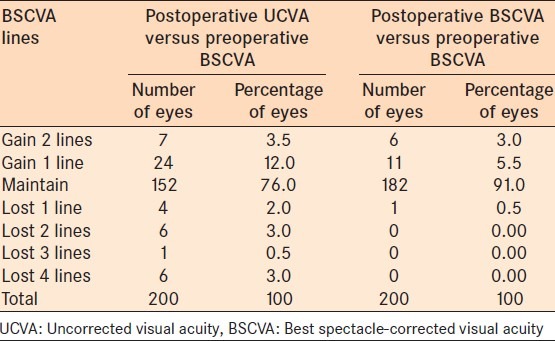
Table 3 presents the frequency and percentage distributions of preoperative versus postoperative mean manifest refraction spherical equivalent.
Table 3.
Frequency and percentages distributions of preoperative versus postoperative mean manifest refractive SE of the better eye
Patient satisfaction and self-perceived outcomes
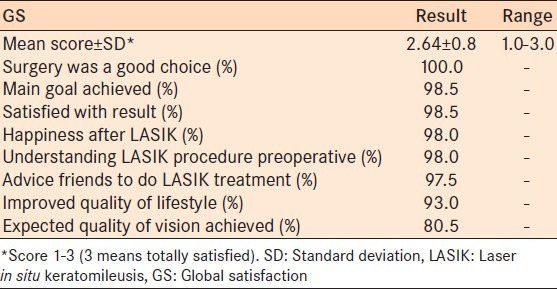
Global satisfaction
The mean score for the overall satisfaction was 2.64 ± 0.8 (3 means totally satisfied). The majority of patients (98.5%) reported that their main goal had been achieved, and they would be willing to have the surgery again if they could do it all again. An improved quality-of-life was reported by 93.0% of patients, and 97.5% would advise friends to do the LASIK treatment. Table 4 presents the global satisfaction scale score.
Table 4.
GS scale score
Quality of daytime vision without correction
The mean score for all patients was 2.5 ± 0.5; UCVA was characterized as slightly or much better than preoperative corrected vision by 33.5% of patients. Satisfaction with uncorrected vision was 2.5 ± 0.50. Postoperative UCVA was 20/40 or better in 99.0% of eyes. Uncorrected near vision was characterized as slightly or much better than the preoperative corrected near vision by 77% of patients.
Quality of daytime vision with correction
The mean score for patient's spectacle wear for quality of daytime vision was 1.81 ± 0.4. Wearing spectacles or contact lenses for distance vision on a regular basis was reported by 1.5% of patients. Near vision correction was used by 3% of patients.
Quality of night vision
The mean score for night vision was 2.75 ± 0.55. Night vision was considered the same or better than before surgery by 96.5% of patients and was considered worse than before surgery by 3.5% of patients [Table 5].
Table 5.
NV, glare and driving scale scores
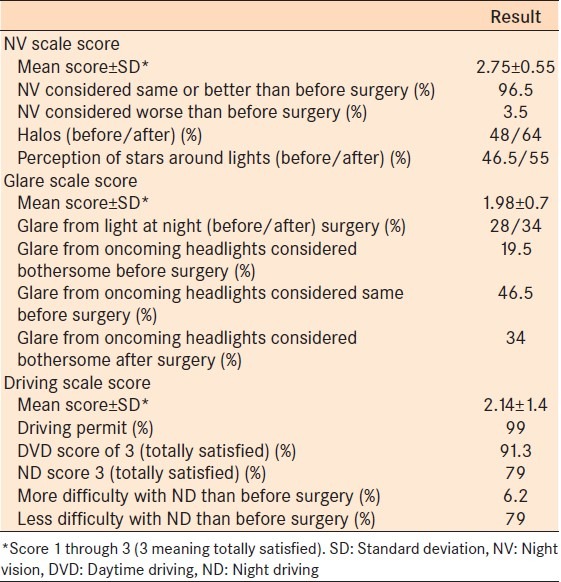
Glare
The mean glare score was 1.98 ± 0.7. Postoperatively, glare from oncoming headlights was considered that same as preoperatively by 46.5% of patients and considered more bothersome by 34% of patients [Table 5]. There was no correlation between the glare or night vision scores and the degree of correction.
Driving
The mean score for driving was 2.14 ± 1.4. There were 91.3% of patients who were completely satisfied with daytime driving and 79% were completely satisfied with night driving. Night driving difficulties were reported 6.2% had more difficulty with night driving than before surgery [Table 5]. There was no correlation between the satisfaction scores and the degree of preoperative SE. A significant correlation was found between the SE at the last follow-up and the uncorrected vision score and the driving scores.
Table 6 presents the correlation coefficients between all scales and clinical parameters.
Table 6.
Correlation coefficient between scales and clinical parameters
DISCUSSION
The concept of patient satisfaction and its study have appeared in the medical and nursing literature since 1965. In 1994 alone, over 1000 such publications were reported. As refractive surgeons, we generally assumed that patient satisfaction following excimer laser correction of refractive errors with LASIK was high. However, anecdotal impressions are often flawed. Many LASIK patients are excessively enthusiastic about their treatment this leads equal enthusiasm from the ophthalmic personnel. Conversely, a small number of unhappy patients can create a disproportionally negative attitude, both to ophthalmic personnel and to other patients. To maintain a balanced impression, it is important to review visual outcomes and patient satisfaction.6,7,8
The lack of subjective feedback reveals a need to present the patient's clinical outcomes (to evaluate the safety and efficacy) together with a more sensitive, multi-dimensional, patient-oriented questionnaire which targets the specific quality of vision in order to expose and evaluate reasons for any subtle dissatisfaction. There is also a need to differentiate between patients who may use visual acuity as a criterion of satisfaction with the surgery and those who use other criteria to make this judgment. This in turn may identify the preexisting factors which may exacerbate the impression of LASIK postoperatively, and those which may contribute to patient satisfaction.
This study showed an excellent refractive outcome with a good predictability with 87% of eyes within ± 0.5 D and 96% within ± 1.0 D from emmetropia. The mean score for the overall satisfaction was 2.64 ± 0.8 on a scale of 0-3 (a score of 3 meaning that the patient was totally satisfied). More than 98.5% of patients reported that their main goal of surgery had been achieved and would make the same decision if they could do it again. Despite excellent refractive outcome results and high patient satisfaction, quality of vision problems such as night vision complaints, glare, and halos remain a problem. These problems have been reported in many clinical studies after refractive surgery, occurring in 12-57% of patients.6 In general, patients were more satisfied with a postoperative SE close to emmetropia. Similar findings have been shown in other studies.8
A meta-analysis of the US Food and Drug Administration approved LASIK devices found that 97% of patients achieved UCVA of 20/40, and 62% of patients achieved UCVA of 20/20.9 Current estimates of patient satisfaction with LASIK range from 82% to 98%.6,8 We believe that self-administered tests, rather than physician-administered tests enable a more objective view of patient satisfaction and quality of vision. When the test is administered by a physician, results may be biased, and patients might feel compelled to always answer in the affirmative.9
This study had a uniform postoperative interval for administering the questionnaire. All patients were asked to fill the questionnaire at the 6 months follow-up visit. Patient perception changes over time due to psychological factors and corneal healing. A longer follow-up makes it more difficult for the patient to accurately compare his or her preoperative and current quality of vision. One limitation of the study is that better analysis may have been possible if it the questionnaire was administered preoperatively and again at a uniform postoperative interval.
In this study, the main reason that patients underwent LASIK was the desire to get rid of their glasses . Despite popular misconceptions about the real disability of myopia and the perception that LASIK treatment is cosmetic surgery, only 4.10% of patients cited improved cosmesis as a motivating factor in seeking surgery.
Satisfaction has often been assessed as a single global response but, as noted,7,8,10 satisfaction has several components, and this study analyzed a number of these components. Attempts to relate satisfaction to preoperative parameters or postoperative outcomes have provided mixed results.
No relation was found between the glare or night vision scores and the degree of correction. Night vision complaints and problems from glare often diminish after 6 months postoperatively.10 Objective quantification of night vision complaints also needs further evaluation, which remains difficult and presents challenges and limitations concerning the precise analysis for documentation. Previous investigators have questioned whether the risk for night vision complaints is really attributable to LASIK or whether the general population has the same prevalence of night vision complaints. Questions have also arisen as to the possible roles of changes in the transition zone and of central neural adaptation in the slow decrease of night vision complaints.
However, 6.2% noted increased difficulty with nighttime driving in this study. This highlights the point that in assessing postsurgical outcome, the proportion of highly myopic individuals are known to experience night time driving difficulties prior to treatment. Therefore, to obtain the most accurate picture of the effect of LASIK or PRK on subjective visual function, questionnaires should be applied before and after intervention to identify genuine change in function, rather than simply the empirical presence or absence of a symptom.
In a study by Brown et al., responses from 13,655 consecutive patients who completed their 1-month postoperative examination were analyzed.11 They11 observed a very high level of satisfaction both for the quality of postoperative care provided (98.6%) and for the visual results obtained (95.0%). Most patients (94.2%) indicated that the surgery improved their life, and most would recommend both laser vision correction (96.5%) and the corporate provider (97.5%) to friends and family. These results are similar to our study. After LASIK, 95% of 200 patients wore no distance optical correction; 99% would have the procedure again; and light sensitivity and night vision problems did not occur in a significant number of patients. The near vision scores were quite high likely reflective of the prepresbyopic population that was enrolled in this study.
There are numerous studies that discussed reasons for patient's dissatisfaction after LASIK. A retrospective study by Jabbur et al., assessed consecutive dissatisfied patients who sought a refractive consultation after refractive surgery was performed elsewhere.12 The most common subjective complaints were blurred distance vision (59.0%), glare and night-vision disturbances (43.5%) and dry eyes (21.1%).12 The most common complications were overcorrection (30.4%) and irregular astigmatism (29.8%).12 A study by Levinson et al. reviewed charts of patients who had LASIK performed elsewhere.13 One hundred fifty-seven eyes of 109 patients were reviewed.13 The most common chief complaints were poor distance vision (63%), dry eyes (19%), and glare and halos (5%). This is the first study in a Middle Eastern country to enroll a majority of females undergoing LASIK. This is notable as females in the region prefer not to wear spectacles and undergo refractive surgery yet many are fearful of surgical complications.
Solomon et al. performed a literature search for article from 1988 to 2008 that included pertinent LASIK surgery data from a review of 2,915 citations.4 A level I rating was assigned to properly conducted, well-designed, randomized clinical trials; a level II rating to well-designed cohort and case-control studies; and a level III rating to case series, case reports, and poorly designed prospective and retrospective studies. Level I and II rated, peer-reviewed articles were entered into a database, and level III articles were eliminated. A total of 309 articles was incorporated into this database, representing well-controlled level I and level II studies of primary LASIK surgery. Nineteen of the 309 database articles (6.1%) reported both patient quality-of-life and satisfaction and reported on a total of 2198 subjects. The overall patient satisfaction after primary LASIK surgery was 95.4% (2,097 of 2,198 subjects; range of patient satisfaction for the 19 articles was 87.2-100%). The patient satisfaction rate after myopic LASIK was 95.3% (1,811 of 1,901 patients). Based on this review, worldwide, an average 95.4% of patients were satisfied with their outcome after LASIK surgery. With 16.3 million procedures performed worldwide and more than a decade of clinical studies and technological innovation, LASIK surgery is considered among the most successful elective procedures.4
CONCLUSION
This study reports a very high level of functional improvement, improved quality-of-life, and consistently high levels of satisfaction post-LASIK across a range of visual function parameters. Proper patient counseling to ensure appropriate patient expectations after refractive surgery are fundamental for patient success. Despite counseling, very quickly many patients forget the details of surgery and the need to set realistic goals. Postoperative symptoms may affect the patient's perception of satisfaction and outcome, but few studies have applied questionnaires before and after surgery.
Many myopic patients may have night time driving difficulties or glare prior to surgery; thus, such symptoms postoperatively may have less effect on satisfaction than surgeons might presume. However, difficulties with nighttime driving can be a significant problem for a minority of patients and should not be understated during the informed consent procedure. The variation in subjective assessment of functional and satisfaction parameters, ophthalmologists, should look for other variables in addition to the UCVA and residual refractive error, as the benchmarks for assessing the outcome of refractive surgery.
ACKNOWLEDGMENTS
We thank administrators and staff of Yemen Magrabi Hospital for permitting us to conduct this study. They assisted and contributed in the patient's care in our study. Finally, we appreciate the efforts and cooperation of all patients they extended to us in this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.D’Arcy FM, Kirwan C, O’keefe M. Ten year follow up of laser in situ keratomileusis for all levels of myopia. Acta Ophthalmol. 2012;90:e335–6. doi: 10.1111/j.1755-3768.2011.02222.x. [DOI] [PubMed] [Google Scholar]
- 2.Alió JL, Muftuoglu O, Ortiz D, Pérez-Santonja JJ, Artola A, Ayala MJ, et al. Ten-year follow-up of laser in situ keratomileusis for myopia of up to -10 diopters. Am J Ophthalmol. 2008;145:46–54. doi: 10.1016/j.ajo.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 3.O’Doherty M, O’Keeffe M, Kelleher C. Five year follow up of laser in situ keratomileusis for all levels of myopia. Br J Ophthalmol. 2006;90:20–3. doi: 10.1136/bjo.2005.075127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon KD, Fernández de Castro LE, Sandoval HP, Biber JM, Groat B, Neff KD, et al. LASIK world literature review: Quality of life and patient satisfaction. Ophthalmology. 2009;116:691–701. doi: 10.1016/j.ophtha.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 5.Hill JC. An informal satisfaction survey of 200 patients after laser in situ keratomileusis. J Refract Surg. 2002;18:454–9. doi: 10.3928/1081-597X-20020701-07. [DOI] [PubMed] [Google Scholar]
- 6.Tahzib NG, Bootsma SJ, Eggink FA, Nabar VA, Nuijts RM. Functional outcomes and patient satisfaction after laser in situ keratomileusis for correction of myopia. J Cataract Refract Surg. 2005;31:1943–51. doi: 10.1016/j.jcrs.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Bailey MD, Mitchell GL, Dhaliwal DK, Boxer Wachler BS, Zadnik K. Patient satisfaction and visual symptoms after laser in situ keratomileusis. Ophthalmology. 2003;110:1371–8. doi: 10.1016/S0161-6420(03)00455-X. [DOI] [PubMed] [Google Scholar]
- 8.Lazon de la Jara P, Erickson D, Erickson P, Stapleton F. Visual and nonvisual factors associated with patient satisfaction and quality of life in LASIK. Eye (Lond) 2011;25:1194–201. doi: 10.1038/eye.2011.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey MD, Zadnik K. Outcomes of LASIK for myopia with FDA-approved lasers. Cornea. 2007;26:246–54. doi: 10.1097/ICO.0b013e318033dbf0. [DOI] [PubMed] [Google Scholar]
- 10.Pop M, Payette Y. Risk factors for night vision complaints after LASIK for myopia. Ophthalmology. 2004;111:3–10. doi: 10.1016/j.ophtha.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 11.Brown MC, Schallhorn SC, Hettinger KA, Malady SE. Satisfaction of 13,655 patients with laser vision correction at 1 month after surgery. J Refract Surg. 2009;25:S642–6. doi: 10.3928/1081597X-20090611-03. [DOI] [PubMed] [Google Scholar]
- 12.Jabbur NS, Sakatani K, O’Brien TP. Survey of complications and recommendations for management in dissatisfied patients seeking a consultation after refractive surgery. J Cataract Refract Surg. 2004;30:1867–74. doi: 10.1016/j.jcrs.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Levinson BA, Rapuano CJ, Cohen EJ, Hammersmith KM, Ayres BD, Laibson PR. Referrals to the Wills Eye Institute Cornea Service after laser in situ keratomileusis: Reasons for patient dissatisfaction. J Cataract Refract Surg. 2008;34:32–9. doi: 10.1016/j.jcrs.2007.08.028. [DOI] [PubMed] [Google Scholar]


