Abstract
Purpose:
The purpose was to evaluate and compare the visual and refractive outcomes, topographic keratometry (K) and complications of Intacs and Intacs SK for mild to moderate keratoconus.
Methods:
In this retrospective study, all mild to moderate keratoconus eyes that underwent implantation of Intacs (Intacs group) or Intacs SK (Intacs SK group) with minimum follow-up of 12 months were included. Preoperative and postoperative uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction, manifest cylinder, spherical equivalent (SE), minimum topographic keratometry, maximum topographic keratometry, and average topographic keratometry were compared in both groups.
Results:
There were 16 eyes in the Intacs group and 18 eyes in the Intacs SK group. Preoperatively, both groups were comparable for most parameters except gender and minimum K and average K. At 6 months postoperatively there were statistically significant improvements in UDVA, CDVA, manifest sphere, SE, minimum K, maximum K, and average K (P < 0.05, all comparisons). Manifest cylinder improved at 6 months, but the improvement was not statistically significant (P > 0.05). The outcomes remained stable with no statistically significant differences between the 6 and 12 months visits. There were no complications in both groups.
Conclusion:
Both models of Intacs significantly improved vision and refractive outcomes, and topographic keratometry in cases of mild to moderate keratoconus. Intacs SK provided better (not statistically significant) results.
Keywords: Intacs, Keratoconous, Keratometry, Refractive, Topography
INTRODUCTION
Intracorneal ring segment (ICRS) implantation is becoming widely accepted as a good surgical option for the treatment for keratoconus. However, the lack of a standard nomogram, different ICRS arc lengths, shape, thickness, optical zone, and poor predictability are challenges facing ophthalmologists who treat keratoconus eyes with ICRS.1
Standard Intacs (Addition Technology Inc., Des Plaines, IL, USA) are 150° arc length segments with a hexagonal transverse shape with an external diameter of 8.1 mm, an internal diameter of 6.8 mm and are available in variable thicknesses (0.21-0.45 mm). Standard Intacs (Intacs) were introduced as an option to treat a wide range of keratoconus cases. Studies have shown that Intacs implantation is safe and effective for mild, moderate, and severe keratoconus. The outcomes of Intacs are relatively better in less advanced keratoconus than in advanced cases.2,3,4,5,6,7
Recently, a new design of Intacs was introduced called the Intacs SK. The Intacs SK has a reduced inner diameter of 6 mm, thus allowing enhanced refractive and higher order aberration correction in the central cornea and an oval cross-section to minimize any chances of glare or halos that may arise due to a reduced inner diameter. Originally, Intacs SK segments were available in two thicknesses, 0.40 and 0.45 mm. These two thicknesses have been found to be effective and safe in eyes with moderate to severe keratoconus with a good tolerance profile with respect to glare or halos8 and perhaps better outcomes than the (standard) Intacs in advanced cases because of the smaller optical zone. Intacs SK are now also available in thicknesses of 0.21, 0.25, 0.30, 0.35, 0.40, and 0.45 mm.
The aim of this study was to evaluate and compare the visual and refractive outcomes, topographic keratometry and complications of Intacs SK (thickness range 0.21-045 mm) and (standard) Intacs (thickness range 0.21-045 mm) for mild to moderate keratoconus.
METHODS
This study was a retrospective, nonrandomized comparative case review. The Institutional Research and Ethics Review Board of College of Medicine, King Saud University approved this study and the study adhered to the tenets of the declaration of Helsinki for research involving humans.
Inclusion criteria were all eyes that were categorized as mild to moderate keratoconus corresponding to Grade I and II with Amsler–Krumeich's classification9 and had undergone ICRS implantation with standard Intacs or Intacs SK with a minimum follow-up of 12 months. All eyes had clear central corneas and a corneal thickness of more than 400 µm at the planned site of ICRS implantation.
The eyes were categorized into two groups: An Intacs group composed of mild to moderate keratoconus eyes that underwent standard Intacs implantation and; an Intacs SK group composed of mild to moderate keratoconus eyes that underwent Intacs SK implantation. Intacs implantation in both groups was based on nomograms provided by the manufacturer.
Preoperative, 6 and 12 month postoperative data were collected on uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA), manifest refraction spherical error, manifest refraction cylindrical error, manifest refraction spherical equivalent (SE), and keratometry (K) values from corneal topography (minimum K, maximum K, and average K).
Surgical technique
Surgical procedure was similar in both groups. One surgeon (AM) performed all surgeries. Implantation was performed using mechanical dissection in both groups. The procedure was performed under topical anesthesia using combination of oxybuprocaine 0.4% (Benoxinate, Chauvin Pharmaceuticals Ltd., England) and lidocaine hydrochloride 2% jelly (Rialocaine, Riyadh Pharma, Saudi Arabia). The geometrical center was marked with gentian violet using Sinskey hook. A 0.9-mm radial incision was made using a diamond knife set at 75% of the corneal thickness. The incision site was placed at the steepest topographic meridian. A regular Intacs dissector was used for standard Intacs, and modified dissectors were used to fashion tunnels sized appropriately for the smaller diameter of Intacs SK. Segment thickness and use of symmetrical or asymmetrical segment was based on the nomogram provided by the manufacturer in both groups. Two tunnels were created using clockwise and counterclockwise dissectors (Addition Technology, Inc.,) under suction created by a vacuum centering guide. The two Intacs segments were implanted in the clockwise and counterclockwise tunnels. The incision was closed with a single or double interrupted 10–0 nylon suture. A bandage contact lens was placed for 3–4 days postoperatively. Patients were prescribed a topical antibiotic and steroid combination to be instilled 4 times daily for 1-week and frequent use of preservative-free artificial tears. The suture was removed 6–8 weeks postoperatively.
Statistical analysis
Visual acuity was assessed at 20 feet and converted to the logarithm of the minimum angle of resolution (logMAR) for statistical analysis and is reported as logMAR in this study. Statistical analysis performed with SPSS (IBM Corp., New York, NY, USA). Baseline characteristics were analyzed using descriptive statistics. Results are expressed as means ± standard deviation (SD). Change over time, from preoperatively to 6 and 12 months postoperatively, was assessed using analysis of variance for repeated measurements and post-hoc bonferroni corrections, as applicable, within and between the two groups. All statistical analyses were two-sided and were evaluated at the 0.05 significance level.
RESULTS
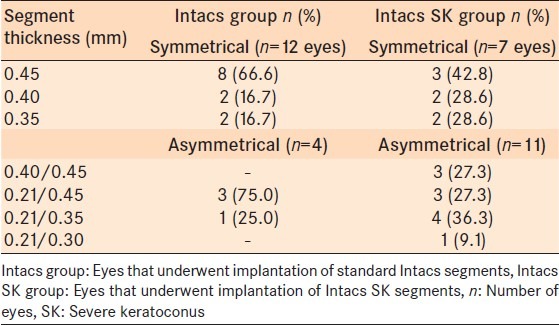
The entire study sample was comprised of 34 eyes of 26 patients. There were 16 eyes of 13 patients (10 [76.9%] males, 3 [23.1%] females) in the Intacs group. The mean age of the Intacs group was 29.6 ± 5.4 years and 12 (75%) eyes were Grade I and 4 (25%) eyes were Grade II keratoconus according to the Amsler-Krumeich classification. There were 18 eyes of 13 patients (4 [30.3%] male, 9 [69.2%] females) in the Intacs SK group. The mean age of the Intacs SK group was 28.1 ± 4.9 years and 10 (55.6%) eyes were Grade I and 8 (44.4%) eyes were Grade II keratoconus according to the Amsler-Krumeich classification. The two groups were comparable in age and keratoconus grading (P = 0.249 and P = 0.236, respectively). The gender distribution was statistically significantly different between groups (P = 0.049) [Table 1]. Segment thickness and use of symmetrical or asymmetrical rings are presented in Table 2.
Table 1.
Preoperative comparison of eyes with mild to moderate keratoconus that underwent implantation of Intacs or Intacs SK
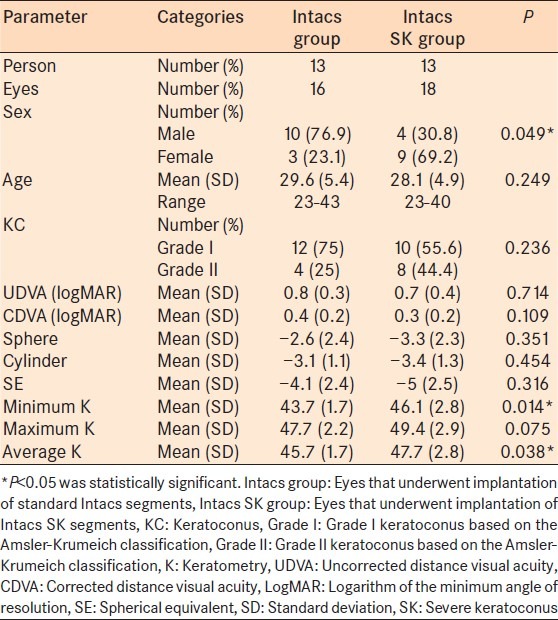
Table 2.
Distribution of Intacs or Intacs SK segments that were implanted for mild to moderate keratoconus
There was no statistically significant difference in preoperative UDVA and CDVA between groups (P = 0.714 and P = 0.109, respectively) [Table 1]. At 6 months, there was a statistically significant improvement in both groups in UDVA (P = 0.002 in the Intacs group and P = 0.001 in the Intacs SK group) and in CDVA (P = 0.023 in the Intacs group and P = 0.011 in the Intacs SK group) [Table 3]. At 6 and 12 months postoperatively, and there was no statistically significant difference between the 2 groups in UDVA (P = 0.254 and P = 0.424 respectively) and in CDVA (P= 0.1 and 0.261 respectively) [Table 3]. The UDVA improved by a mean of 0.3 ± 0.2 logMAR in the Intacs group and 0.3 ± 0.3 logMAR in the Intacs SK group (P = 0.330). The CDVA improved by a mean of 0.2 ± 0.2 logMAR in the Intacs group and 0.2 ± 0.2 logMAR in the Intacs SK group (P = 0.385) [Table 4].
Table 3.
Within group comparison between preoperative and postoperative data of eyes with mild to moderate keratoconus that underwent implantation of Intacs or Intacs SK
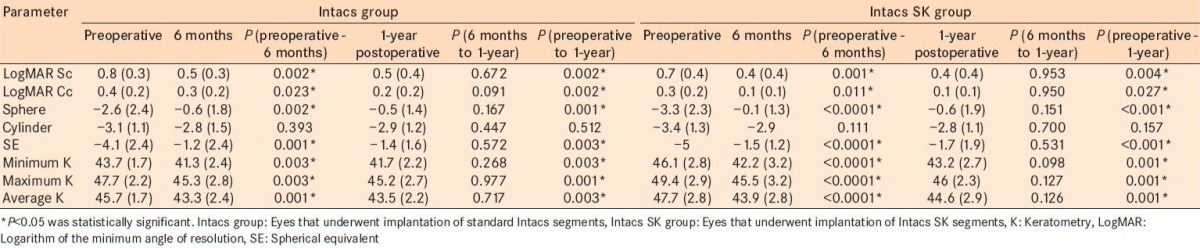
Table 4.
Between groups postoperative data
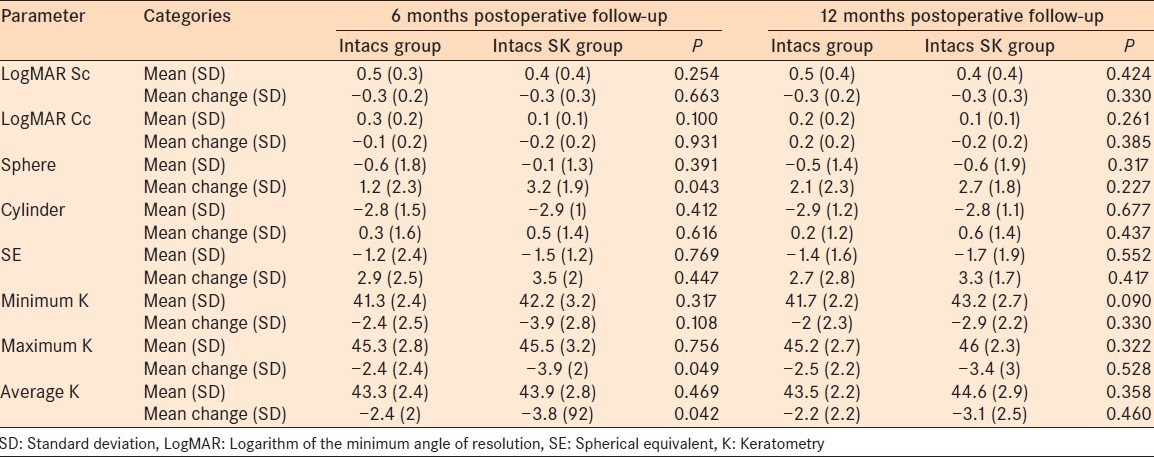
At 6 months, there was a statistically significant improvement in both groups in manifest sphere (P = 0.002 for the Intacs group and P < 0.0001 for the Intacs SK group) and in SE (P = 0.001 in the Intacs group and P < 0.0001 in the Intacs SK group) [Table 3]. For manifest cylinder, there was an improvement at 6 months but not statistically significant (P = 0.393 in the Intacs group and P = 0.111 in the Intacs SK group). The mean change in the manifest sphere, manifest cylinder, and SE was better in the Intacs SK group, but it was not statistically significant [Table 4].
There was a statistically significant difference in preoperative minimum K and average K between groups (P < 0.05 both comparisons) [Table 1]. At 6 months, there were statistically significant improvements in both groups in minimum K (P = 0.003 in the Intacs group and P 0≤ 0.0001 in the Intacs SK group), maximum K (P = 0.003 in the Intacs group and P < 0.0001 in the Intacs SK group), and average K (P = 0.001 in the Intacs group and P ≤ 0.0001 in the Intacs SK group) [Table 4]. The mean change in minimum K, maximum K, and average K was higher in the Intacs SK group, but it was not statistically significant [Table 4].
Our study findings suggest that the mean (SD) differences in improvement in both groups at 6 and 12 months postoperatively do not vary much between groups. At 6 months postoperatively, there were statistically significant differences in terms of sphere (P = 0.043) and average K (P = 0.042), these difference disappeared by 1-year postoperatively [Figures 1 and 2]. In the Intacs group and Intacs SK group, CDVA was maintained at preoperative levels in 4 (25%) and 7 (38.9%) eyes, respectively. 12 (75%) eyes in the Intacs group, gained one or more lines of CDVA. 11 (61.1%) eyes in the Intacs SK group gained one or more lines of CDVA [Figure 3]. The safety index for Intacs group was 1.57 at 12 months postoperatively indicating a gain of 57% in visual acuity. For the Intacs SK group, the safety index was 1.60 at 12 months, indicating a gain of 60% in visual acuity. There were no intra-operative or postoperative complications or any other adverse events during the 12 months follow - up in both groups. In Intacs group, 7 (43.8%) eyes achieved 0.3 logMAR (6/12) UDVA with an efficacy index of 0.8 and in the Intacs SK group 9 (50%) eyes achieved 0.3 logMAR (6/12) UDVA with an efficacy of 0.8 at 12 months postoperatively.
Figure 1.
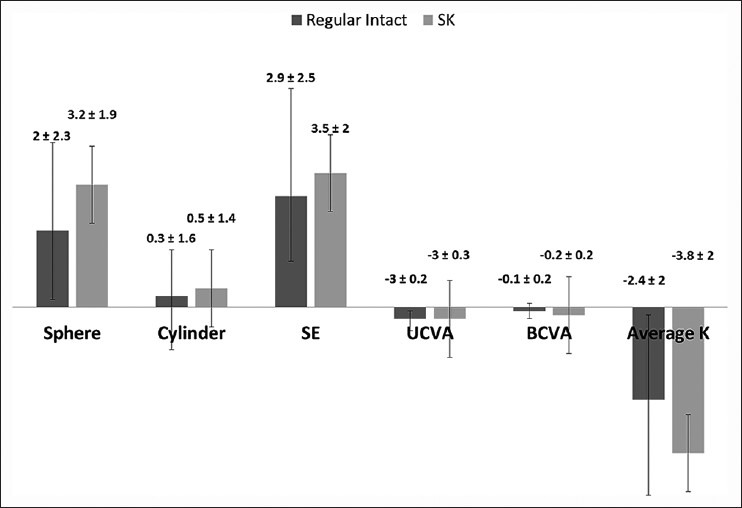
Differences in mean (standard deviation) visual acuity indices preoperatively and 6 months postoperatively
Figure 2.
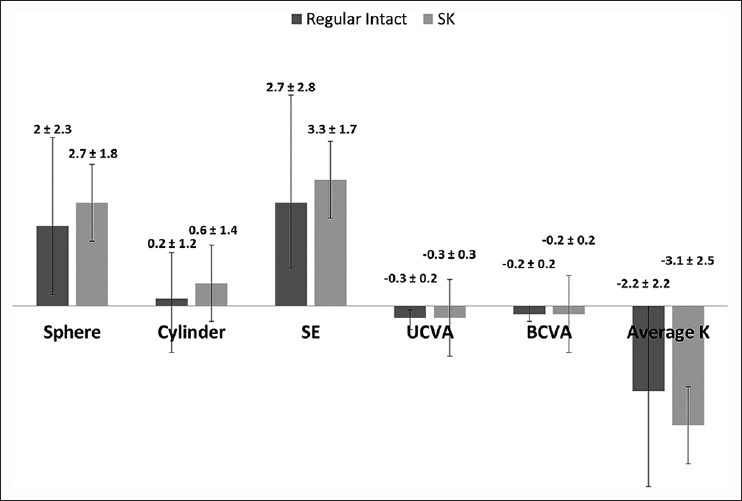
Differences in mean (standard deviation) visual acuity indices preoperatively and 1-year postoperatively
Figure 3.
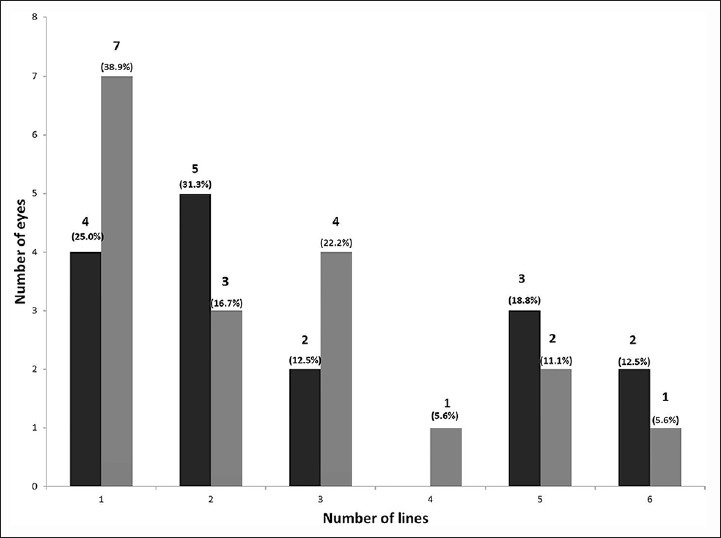
Distribution of gain in corrected distance visual acuity in eyes underwent eyes with mild to moderate keratoconus that underwent implantation of Intacs or Intacs severe keratoconus
DISCUSSION
Visual rehabilitation in patients with keratoconus is challenging. ICRS was introduced to provide refractive correction and to improve UDVA and CDVA. The resulting increase in vision may increase the chances that patients can wear spectacles or hard contact lenses. In addition, ICRS implantation may postpone or avoid the need for keratoplasty.
Outcomes of standard Intacs for keratoconus have showed significant improvements in UDVA and CDVA and significant decreases in spherical refraction, SE, and keratometry.3,4,5,6,7,10 Our results concur with previous studies.3,4,5,6,7,10 However, the number of eyes that achieved statistically significant improvement were higher in our study. This observation may be because we included eyes with mild to moderate keratoconus that are known to have betters outcomes compared to severe keratoconus, whereas other studies3,4,5,6,7,10 included the entire spectrum of keratoconus cases.
Our evaluation of astigmatism-related parameters indicated that the manifest cylinder improved by 0.2 ± 1.2 D that was not statistically significant (P > 0.05). Similar results have been reported in two previous studies on standard Intacs with the magnitude of improvement of 0.29 D (306 eyes)5 and 0.75 D (30 eyes).7 However, Levinger and Pokroy3 and Colin et al.6 reported a statistically significant improvement in cylinder of 1.37 D (58 eyes) and 2.9 D (57 eyes), respectively. The statistical improvement reported in these papers could be due to enrollment of a different spectrum of cases that included more severe keratoconus cases with high cylinder that show greater improvement resulting in statistically significant changes.
We found that no eyes lost CDVA in the Intacs group, which differs from previous reports of loss of CDVA in 10% of eyes.10,11,12 The differences between studies are likely that the previous studies10,11,12 found loss of CDVA occurred in advanced cases of keratoconus.
The new design of the ICRS segment, the Intacs SK, was introduced with a reduced inner diameter of 6 mm, thus allowing enhanced refractive and visual correction in the central cornea and an oval cross-section to minimize chances of glare or halos that may arise due to a reduced inner diameter. Intacs SK implantation of 0.35, 0.4 and 0.45 mm segments are safe and effective for moderate to severe keratoconus eyes.1,8,13,14,15 Haddad et al.1 and Fahd et al.3 reported statistically significant improvement in all parameters which concurs with most of our results apart from the changes in the manifest cylinder. The different spectrum of patients included in our study, and the small sample might explain the differences between studies.1,13
The safety and maintenance of CDVA after Intacs SK for keratoconus eyes in our study are similar to previous reports.1,8 However, our study and other studies of Intacs SK enrolled small sample sizes and we believe a larger sample is required to determine the safety of Intacs SK for keratoconus.
There are some published studies comparing standard Intacs and other ICRS with smaller optical zones. Kubaloglu et al.16 compared the outcomes of the Keraring ICRS (Mediphacos, Belo Horizonte, Brazil) and standard Intacs for mild to moderate keratoconus. They16 found a significant improvement in visual, refractive and topographic parameters. However, the Keraring ICRS had statistically significantly better UDVA, CDVA, and decrease in maximum K.16 Kaya et al.17 compared standard Intacs and Ferrara ICRS (Ferrara Ophthalmics Ltda., Belo Horizonte, Brazil) and found that both ICRS significantly improved UDVA, CDVA, SE and maximum K. However, refractive and visual outcomes were better in Ferrara group.17 The two studies16,17 mentioned above concluded that a better result achieved with Keraring and Ferrara ICRS were related to the smaller optical zone and more effect on the center of the cornea. Our result was in agreement with two studies mentioned above where intacs SK was better than standard Intacs for all parameters. However, the differences were not statistically significant.
To our knowledge, there are no published papers reporting the outcomes of the new Intacs SK using 0.21, 0.25, 0.30 mm thickness as well as comparing results of Intacs SK and standard Intacs. However, we encourage a detailed study with an increased sample size, more sophisticated analysis (including vector analysis for cylinder assessment), and longer duration of follow for more conclusive results on the differences between Intacs and Intacs SK for keratoconus.
CONCLUSIONS
The current study showed that Intacs SK was effective and safe in treating mild to moderate keratoconus. Our results showed that standard Intacs and Intacs SK were comparable. However, we cannot be completely certain as there were differences in preoperative parameters with more Grade II keratoconus cases in the Intacs SK group than in Intacs group. In addition, the statistically significant differences in minimum K and average K and also the retrospective nature of the study with a small sample size are all important caveats to this study.
We believe that a prospective study, with comparable groups of keratoconus cases, with a larger sample and measuring other parameters including subjective glare and halos, and higher order aberration will be valuable for a better conclusion regarding the comparison between standard Intacs and Intacs SK.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Haddad W, Fadlallah A, Dirani A, El Rami H, Fahd D, Khanafer D, et al. Comparison of 2 types of intrastromal corneal ring segments for keratoconus. J Cataract Refract Surg. 2012;38:1214–21. doi: 10.1016/j.jcrs.2012.02.039. [DOI] [PubMed] [Google Scholar]
- 2.Alió JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: Long-term follow-up. J Cataract Refract Surg. 2006;32:978–85. doi: 10.1016/j.jcrs.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 3.Colin J. European clinical evaluation: Use of Intacs for the treatment of keratoconus. J Cataract Refract Surg. 2006;32:747–55. doi: 10.1016/j.jcrs.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 4.Colin J, Cochener B, Savary G, Malet F, Holmes-Higgin D. INTACS inserts for treating keratoconus: One-year results. Ophthalmology. 2001;108:1409–14. doi: 10.1016/s0161-6420(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 5.Ertan A, Kamburoglu G. Intacs implantation using a femtosecond laser for management of keratoconus: Comparison of 306 cases in different stages. J Cataract Refract Surg. 2008;34:1521–6. doi: 10.1016/j.jcrs.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Levinger S, Pokroy R. Keratoconus managed with intacs: One-year results. Arch Ophthalmol. 2005;123:1308–14. doi: 10.1001/archopht.123.10.1308. [DOI] [PubMed] [Google Scholar]
- 7.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: Safety and efficacy. J Cataract Refract Surg. 2007;33:1886–91. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 8.Sansanayudh W, Bahar I, Kumar NL, Shehadeh-Mashour R, Ritenour R, Singal N, et al. Intrastromal corneal ring segment SK implantation for moderate to severe keratoconus. J Cataract Refract Surg. 2010;36:110–3. doi: 10.1016/j.jcrs.2009.07.040. [DOI] [PubMed] [Google Scholar]
- 9.Krumeich JH, Daniel J, Knülle A. Live-epikeratophakia for keratoconus. J Cataract Refract Surg. 1998;24:456–63. doi: 10.1016/s0886-3350(98)80284-8. [DOI] [PubMed] [Google Scholar]
- 10.Alió JL, Shabayek MH, Belda JI, Correas P, Feijoo ED. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus correction. J Cataract Refract Surg. 2006;32:756–61. doi: 10.1016/j.jcrs.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Ertan A, Kamburoglu G, Bahadir M. Intacs insertion with the femtosecond laser for the management of keratoconus: One-year results. J Cataract Refract Surg. 2006;32:2039–42. doi: 10.1016/j.jcrs.2006.08.032. [DOI] [PubMed] [Google Scholar]
- 12.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, et al. Long-term follow-up of Intacs in keratoconus. Am J Ophthalmol. 2007;143:236–44. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 13.Fahd DC, Jabbur NS, Awwad ST. Intrastromal corneal ring segment SK for moderate to severe keratoconus: A case series. J Refract Surg. 2012;28:701–5. doi: 10.3928/1081597X-20120921-05. [DOI] [PubMed] [Google Scholar]
- 14.Khan MI, Injarie A, Muhtaseb M. Intrastromal corneal ring segments for advanced keratoconus and cases with high keratometric asymmetry. J Cataract Refract Surg. 2012;38:129–36. doi: 10.1016/j.jcrs.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 15.Niknam S, Shamshiri M, Shahrzad SS, Alipour A, Rajabi MB, Rajabi MT. Treatment of moderate to severe keratoconus with 6-mm Intacs SK. Int J Ophthalmol. 2012;5:513–6. doi: 10.3980/j.issn.2222-3959.2012.04.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kubaloglu A, Cinar Y, Sari ES, Koytak A, Ozdemir B, Ozertürk Y. Comparison of 2 intrastromal corneal ring segment models in the management of keratoconus. J Cataract Refract Surg. 2010;36:978–85. doi: 10.1016/j.jcrs.2009.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Kaya V, Utine CA, Karakus SH, Kavadarli I, Yilmaz OF. Refractive and visual outcomes after Intacs vs ferrara intrastromal corneal ring segment implantation for keratoconus: A comparative study. J Refract Surg. 2011;27:907–12. doi: 10.3928/1081597X-20110906-03. [DOI] [PubMed] [Google Scholar]


