Abstract
Background:
Poor sexual function is associated with impaired Health-Related Quality of Life (HRQoL), and patients with Coronary Artery Disease (CAD) are not exceptions. It is not known, however, if symptoms of depression mediate the effect of sexual function on HRQoL among men and women with CAD.
Objectives:
This study aimed to determine the mediating effect of depressive symptoms on the association between sexual function and HRQoL among men and women with CAD.
Patients and Methods:
This cross-sectional study was conducted on 401 men and 156 women with CAD. Sexual function, measured by the Relation and Sexuality Scale (RSS), was the independent variable. In addition, physical and mental HRQoL measured using physical and mental health summary scores of Short Form 36 (SF-36) were dependent variables. Besides, the severity of depressive symptoms measured by the Hospital Anxiety and Depression Scale (HADS) was conceptualized as the mediator. Age, income, education, and medical comorbidities (Ifudu index) were control variables, and gender was the moderator. Multi-group path analysis was conducted using AMOS20.0 for data analysis.
Results:
When the effects of age, education, income, and comorbidities were controlled, sexual function was correlated with poor mental HRQoL in both genders. However, the association between sexual function and poor physical HRQoL could be found only among men but not women. Evidence also supported partial mediation of depressive symptoms on the effect of sexual function on mental HRQoL of both men and women. Nonetheless, the results suggested partial mediation of depressive symptoms on the effect of sexual function on physical HRQoL only among men but not women.
Conclusions:
Symptoms of depression may not have a similar role in explaining the effect of sexual function on physical HRQoL of men and women with CAD. Our findings suggest that only among men, depressive symptoms might be the mechanism by which sexual function affects the CAD patients’ physical HRQoL.
Keywords: Coronary Artery Disease, Depression, Comorbidity
1. Background
Patients with Coronary Artery Disease (CAD) report poor sexual function (1). A considerable proportion of the patients with CAD report fear of intercourse (2) and avoid engagement in intercourse (3). Intercourse avoidance among the patients with CAD may be partially due to an unrealistic appraisal (over-estimation) of risk of cardiac events during the intercourse. Patients with CAD may have major concerns about the negative effects of sexual activity on their health (4). Among the patients with CAD, impaired sexual function is associated with poor Health Related Quality of Life (HRQoL) (5).
Depression or depressive symptoms may at least partially mediate the effect of poor sexual function on HRQoL among the patients with CAD. Yet, a recent study on men and women with CAD did not find gender differences in the mediating effects of depression on the link between sexual function and HRQoL. Unfortunately, that study did not control possible confounders, such as socioeconomics and medical comorbidities (6). Since socioeconomics and medical comorbidities are related to impairment of sexual function and HRQoL, studies on the mediators of the association between sexual function and HRQoL should control these two variables.
In addition to the need for controlling the possible confounders, there are other reasons that justify further research on gender differences in mediating effects of depressive symptoms on the association between sexual function and HRQoL among the patients with CAD. First, very few studies have investigated the mechanisms of the effect of sexual function on HRQoL among CAD patients (7). Second, although CAD impairs the patients’ sexual function regardless of gender (1, 4), most studies on sexual function of the CAD patients are limited to men (8, 9). Among patients with CAD, however, women may experience worse sexual relationships compared to men (10). In addition, sexual function may differently influence HRQoL of men and women. Based on a study, sexual satisfaction was related to physical HRQoL among men while sexual function was associated with mental HRQoL among women (11). Last but not least, distribution of sexual function, depression, and HRQoL varies among men and women with CAD (12).
2. Objectives
The present study aims to determine the possible gender differences in the mediating effects of depressive symptoms on the association between poor sexual function and physical and mental HRQoL among the patients with CAD.
3. Patients and Methods
3.1. Design and Setting
The current cross-sectional study was conducted in the outpatient cardiology clinic of a hospital in Tehran, Iran. The study protocol was approved by the institutional review board of the hospital. All tertiary hospital participants provided written informed consents for taking part in the study. Additionally, interviews were completed in a private setting and all the data were collected anonymously (13-15).
The study was conducted on 401 male and 156 female CAD patients. The inclusion criteria of the study were being in a relationship for a minimum of one year and having CAD defined as presence of stenosis higher than 50% in at least one major coronary artery on angiography. On the other hand, the exclusion criterion of the study was having a history of any complication of CAD (e.g. myocardial infarction or hospitalization) during the past 6 months.
3.2. Measurements
Socio-demographic characteristics (age, education level, and family income) and medical comorbidity were the study covariates. In addition, sexual function was the independent variable and symptoms of depression were the possible mediators. The participants filled out the self-administered questionnaires using paper and pencil. In case they needed help, information or assistance was provided by a trained sex-matched researcher assistant.
3.3. Measures
3.3.1. Sexual Function
The patients’ sexual function over the past two weeks was assessed using the Relation and Sexuality Scale (RSS). RSS is composed of 10 items that investigate the impact of the disease and treatment on different aspects of sexual behavior. This scale has been frequently utilized for evaluating the sexual activity of male and female patients with CAD in Iran (11). The reliability of this measure was 0.694 in our study.
3.3.2. Symptoms of Depression
The Hospital Anxiety and Depression Scale (HADS) was used to measure the symptoms of depression in the present study. This questionnaire includes 7 four-option items for measurement of depressive symptoms (16). Accordingly, the minimum and maximum depressive scores were 0 and 21, respectively and higher scores represented higher depressive symptoms (16). The Cronbach's alpha coefficient for depressive symptoms of the translated version of HADS in this study was 0.86. Also, this scale has been previously validated in Iran (17).
Medical comorbidity: The Ifudu scale was used to measure medical comorbidities. The modified Ifudu scale that was used in the current study included the following 12 items:
non-ischemic cardiovascular problems,
respiratory diseases,
autonomic neuropathy,
other neurologic problems,
neuromuscular disorders,
infections including AIDS,
liver, pancreases, and biliary diseases (hepatitis, hepatic disorder, and pancreatic enzyme defect),
hematologic problems,
vertebral column problems, low back pain, orarthritis,
visual disorders,
limb amputation (from finger amputation up to lower extremity amputation), and
genitourinary diseases. Each item received a score between 0 (absence of comorbidities) and 3 (presence of severe comorbidities) and the total comorbidity score ranged from 0 to 36.
A high comorbidity score represented the presence of more comorbidities (18). This scale has been commonly used in several chronic conditions including but not limited to CAD (19-24).
3.3.3. Main Outcome Measurement
The Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) was used to measure HRQoL (25). The SF-36 is a generic multidimensional measure of HRQoL that contains eight subscales representing physical functioning, social functioning, role limitations due to physical health problems, role limitations due to emotional problems, mental health, vitality, bodily pain, and general health perceptions. Physical and mental components of the eight scales are combined into Physical Component Summary (PCS) and Mental Component Summary (MCS) scores (26). The reliability and validity of SF-36 have been proved in the Iranian general population (27, 28).
3.4. Statistical Analysis
In this study, univariate and bivariate analyses were performed using the SPSS statistical software, while AMOS20 was used for multivariate analysis (multi-group path analysis). In Model I and Model II, sexual function was the independent variable, while age, income, education, pain, and comorbidities were the control variables. Besides, the level of depressive symptoms was the mediator and gender was the moderator. Moreover, physical HRQoL in Model I and mental HRQoL in Model II were the outcomes. P < 0.05 was considered as statistically significant.
4. Results
4.1. Descriptive Statistics
This study was conducted on 401 men and 156 women with CAD. The mean (SD) age of the patients was 57 ± 11 years. The participants’ mean (SD) and range of socioeconomics, medical comorbidities, sexual function, depressive symptoms, and physical and mental HRQoL have been presented in Table 1.
Table 1. Baseline Characteristics of the Men and Women with Coronary Artery Disease.
| Mean | SD | Mean | SD | Mean | SD | |
|---|---|---|---|---|---|---|
| Age | All | Men | Women | |||
| Education | 57.1 | 10.7 | 57.2 | 11.3 | 56.6 | 9.4 |
| Family income | 3.1 | 1.36 | 3.1 | 1.4 | 1.9 | 1 |
| Depressive symptoms | 2.13 | 0.91 | 2.1 | 0.9 | 1.7 | 0.7 |
| Comorbidity | 4.72 | 3.13 | 4.7 | 3.1 | 6.5 | 3.2 |
| Sexual function | 56.43 | 9.54 | 56.4 | 9.5 | 51.5 | 13.1 |
| Physical health-related quality of life | 64.2 | 21.28 | 38.89 | 21.24 | 64.2 | 21.28 |
| Mental health-related quality of life | 59.12 | 21.31 | 38.68 | 21.56 | 59.12 | 21.31 |
Abbreviations: SD, Standard Deviation
4.2. Biavriate Analysis
The study results revealed a correlation between impaired sexual function and poor physical and mental HRQoL. However, no significant relationship was observed between sexual function and depressive symptoms and medical comorbidities among men. On the other hand, impairment in sexual function was correlated to higher depressive symptoms, medical comorbidities, and poor physical and mental HRQoL among women (Table 2).
Table 2. Correlations among Socioeconomic Characteristics, Depressive Symptoms, Comorbidities, Sexual Function, and Physical and Mental Health-Related Quality of Life among Men and Women with Coronary Artery Disease.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1 Age | 1 | -0.009 | 0.053 | -0.011 | 0.015 | -0.004 | -0.067 | 0.093 |
| 2 Education | -0.353** | 1 | 0.527** | 0.027 | -0.131** | -0.084 | -0.045 | 0.077 |
| 3 Income | -0.178* | 0.473** | 1 | -0.163** | -0.064 | -0.158** | 0.158** | 0.077 |
| 4 Depressive symptoms | 0.067 | -0.101 | -0.035 | 1 | 0.194** | 0.107 | -0.308** | -0.392* |
| 5 Comorbidities | -0.045 | -0.122 | -0.110 | 0.241** | 1 | 0.060 | -0.397** | -0.432* |
| 6 Sexual function | 0.172* | -0.078 | -0.072 | -0.183** | 0.268 | 1 | -0.251** | -0.214* |
| 7 Physical health-related quality of life * | -0.279** | 0.384** | 0.220** | -0.321** | -0.318 | -0.161* | 1 | |
| 8 Mental health-related quality of life | -0.004 | 0.189* | 0.137* | -0.357** | -0.397 | -0.208** | 0.604 | 1 |
*P < 0.05,
**P < 0.01; Correlation coefficients for men appear above the diagonal
Nonetheless, no significant associations were found between the number of involved vessels in angiography and sexual function and HRQoL among men and women.
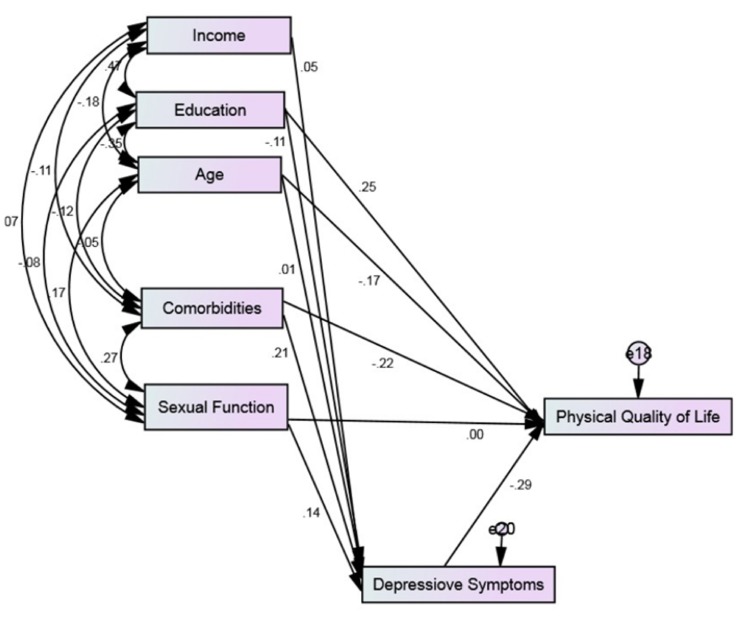
4.3. Model I (Physical HRQoL as Outcome)
Model I fit the data very well (Chisquare = 3.518, P = 0.172, CFI = 0.996, x2/df = 1.759, RMSEA = 0.037). Among the men with CAD, impairment in sexual function was associated with high depressive symptoms (Standardized B = 0.12) which was in turn associated with poor physical HRQoL (Standardized B = -0.26). Also, a direct association was observed between impaired sexual function and poor physical HRQoL (Standardized B = -0.19) (Figure 1).
Figure 1. Model I, the Associations among Socioeconomics, Comorbidity, Sexual Function, Depressive Symptoms, and Physical Health-Related Quality of Life among Men and Women with Coronary Artery Disease (Chi-square = 3.518, P = 0.172, CFI = 0.996, x2/df = 1.759, RMSEA = 0.037).
However, the results indicated no significant association between sexual function and depressive symptoms and physical HRQoL among the women with CAD. Nevertheless, an association was observed between high depressive symptoms and poor physical HRQoL (Standardized B = -0.29) (Figure 1).(
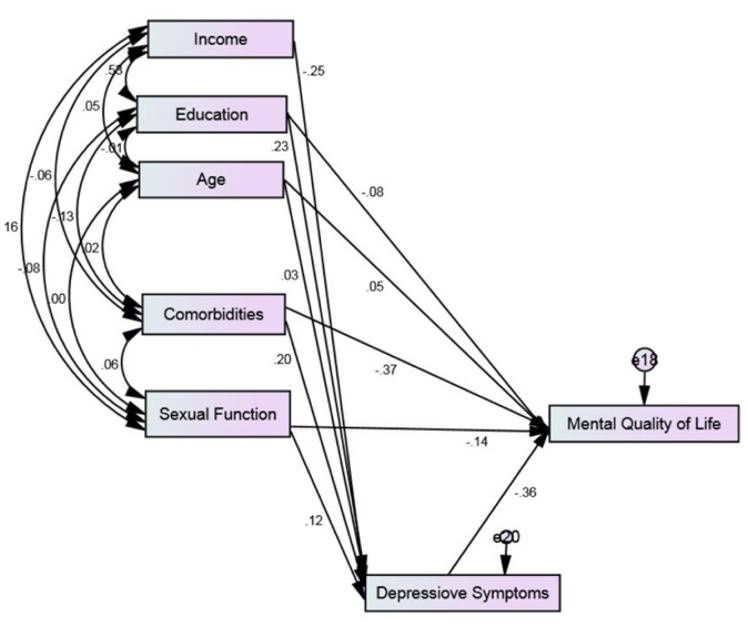
4.4. Model II (Mental HRQoL as Outcome)
Model II fit the data very well (2.538, P = 0.638, CFI = 1.000, x2/df = 0.634, RMSEA = 0.000). Among the men with CAD, impaired sexual function was associated with high depressive symptoms (Standardized B = 0.12) which was in turn associated with poor mental HRQoL (Standardized B = -0.36). There was also a direct association between impaired sexual function and poor mental HRQoL (Standardized B = -0.14) (Figure 2).
Figure 2. Model II, the Associations among Socioeconomics, Comorbidity, Sexual Function, Depressive Symptoms, and Mental Health-Related Quality of Life among Men and Women with Coronary Artery Disease (Chi-square = 2.538, P = 0.638, CFI = 1.000, x2/df = 0.634, RMSEA = 0.000).
Among the women, on the other hand, no significant association was found between sexual function and depressive symptoms and mental HRQoL. However, the results demonstrated a relationship between depressive symptoms and mental HRQoL (Standardized B = -0.36) (Figure 2).
5. Discussion
Our study revealed gender differences in the mediating effects of depression on the association between sexual function and HRQoL. The results showed such mediation only among men but not women with CAD.
Moreover, when socioeconomics and comorbidities were controlled, impaired sexual function was associated with high depressive symptoms among men but not women with CAD. The multinational survey of aging males suggested that 83% of men aging 40 – 70 years believed that their sexual desire and interest were important or very important components of their lives (29). Our findings were also in line with the reports on the effect of sexual dysfunction on HRQoL among men in the general population (30).
A recent review suggested that intercourse, not other sexual activities, was linked to physical and mental health in men and women (31). In a study on men and women with CAD, depression, sexual function, and physical and mental HRQoL were associated (32). Although most studies on the patients with chronic conditions have suggested an association between sexual function and HRQoL (33-35), there are also studies reporting no relationships between the two (36).
In a study among renal transplant recipients, sexual function and sexual frequency were correlated to the total SF-36 score among men but not women. That study concluded that sexual function and satisfaction were associated with physical and mental health in men and women, respectively. Thus, the researchers stated that improvement of sexual function might have different health implications for men and women with chronic medical conditions (11).
In contrast to our findings, the results of a study by Kriston et al. showed no gender difference in the mediating effects of depressive symptoms on the association between sexual function and HRQoL among the patients with CAD. Those researchers, however, did not control demographics, socioeconomics, and comorbid medical conditions (37). According to that study, at least a part of the effect of sexual function on the CAD patients’ HRQoL was due to an increase in the severity of depressive symptoms in both genders.
The current study was conducted in response to the knowledge gap regarding gender differences in the possible mechanisms by which impaired sexual function and HRQoL are correlated (10, 37).
Limited information exists about gender differences in the risk factors and consequences of impaired sexual function in the context of CAD (37). There is also a gap in our understanding about differences between men and women with CAD concerning on the mechanisms by which impaired sexual function results in poor HRQoL. This study extended our knowledge in both of these areas by revealing gender differences in the role of depression as a mediator for the effect of sexual function on the CAD patients’ HRQoL.
Our findings also expanded the current knowledge about the possible mechanisms explaining the link between impaired sexual function and poor HRQoL. Although there are a few exceptions (36), there is a well-established association between poor sexual function and poor HRQoL among the patients with different illnesses and conditions (33, 34). We hope that our findings will be beneficial to the clinicians who wish to treat the CAD patients with poor sexual function (1, 7).
Based on the present study results, targeting depressive symptoms may be an approach to break vicious circle between sexual impairment and poor life quality of the male patients with CAD. Overall, 31 - 45% of the patients with CAD reported clinically significant levels of depressive symptoms and 15 - 20% met the criteria for major depressive disorder (38). Yet, high rate of depression provides an opportunity to intervene. In fact, depressive symptoms are modifiable and may decline by multiple ways, such as cognitive behavioral and pharmaceutical interventions (39).
Our findings may help clinicians and public health practitioners who wish to promote HRQoL of the CAD patients with impaired sexual functioning. Although sexual functioning and HRQoL are intertwined phenomena (40), based on our findings, programs and interventions may be tailored to the gender of the patients. Future research should assess whether the interventions that reduce depressive symptoms of the CAD patients with impaired sexual function will result in a larger improvement in HRQoL in men compared to women. Considering women, sexual dysfunctions, such as dyspareunia (41) or libido disorders (42), that limit HRQoL may need to be the direct target of the interventions instead of the associated depressive symptoms.
This study may also help cardiologists and other healthcare providers who provide care services for the men or women with CAD who suffer from impaired sexual function and poor HRQoL. According to the results, reduction of sexual dysfunction may enhance HRQoL of both men and women with CAD. Reduction of depressive symptoms, however, may enhance physical HRQoL of men but not women with CAD. Thus, evaluation and treatment of sexual function, depression, medical comorbidities, and HRQoL of the patients with CAD may need to be tailored to the patients’ gender.
In the present study, the mediating effect of depression on the link between HRQoL and sexual impairment was limited to the male population. Therefore, we can hypothesize that erectile dysfunction may be the reason why the relationships among sexual relations, depression, and HRQoL are only found among men. Hence, future studies are recommended to focus on the moderating and mediating effects of erectile dysfunction on the associations among sexual relations, mental health, and well-being. Unfortunately, we were not aware of the male participants’ erectile dysfunction status in this study. The prevalence of erectile dysfunction has been reported to be up to 75% among the men with CAD. Endothelial dysfunction is one of the markers for atherosclerosis and several predisposing risk factors of atherosclerosis can lead to endothelial dysfunction. Also, CAD is associated with an imbalance of vasomodulators at the endothelial level which further favors vasoconstriction and can lead to erectile dysfunction (43). Thus, sexual impairment due to erectile dysfunction results in depression in men but not women (44).
The current study findings revealed a significant difference between the men and women with CAD with respect to the role of depressive symptoms as a possible mediator for the effect of sexual function on physical HRQoL. The researchers hope that the results would help healthcare providers who wish to improve the CAD patients’ HRQoL through promotion of sexual wellbeing.
5.1. Limitations
Our study had several limitations. First and foremost, sexual disorders which are the major contributors to sexual behaviors (45) were not measured in this study. In addition, the medications used for CAD, depression, or sexual function were not included in the analysis. Furthermore, other factors, such as body mass index, anxiety, and fatigue, may also contribute to sexual function and confound or mediate the association interest in this study. Hence, future researches are suggested to investigate the possible effects of enhancement of sexual function on depressive symptoms and HRQoL among the CAD patients.
Acknowledgments
There is no acknowledgement.
Footnotes
Implication for health policy/ practice/ research/ medical education:Our findings may help clinicians and public health practitioners who wish to promote well-being of CAD patients with impaired sexual functioning. Interventions that target depressive symptoms possibly due to sexual impairment may better work for men than women. Based on our findings, interventions may benefit from tailoring to gender of the participants or the target population.
Authors’ Contribution:This article has only one author. Shervin Assari has designed, analyzed, drafted, and revised the manuscript.
Financial disclosure:There is no financial disclosure.
Funding/Support:Publication of this manuscript was possible with the Cornely Fellowship fund awarded by the Center for Research on Ethnicity, Culture and Health, School of Public Health, University of Michigan to the author.
References
- 1.Bedell SE, Duperval M, Goldberg R. Cardiologists' discussions about sexuality with patients with chronic coronary artery disease. Am Heart J. 2002;144(2):239–42. doi: 10.1067/mhj.2002.124053. [DOI] [PubMed] [Google Scholar]
- 2.Kazemi-Saleh D, Pishgou B, Assari S, Tavallaii SA. Fear of sexual intercourse in patients with coronary artery disease: a pilot study of associated morbidity. J Sex Med. 2007;4(6):1619–25. doi: 10.1111/j.1743-6109.2007.00619.x. [DOI] [PubMed] [Google Scholar]
- 3.Assari S. Intercourse Avoidance among Women with Coronary Artery Disease. The journal of sexual medicine. 2014 doi: 10.1111/jsm.12459. [DOI] [PubMed] [Google Scholar]
- 4.Steinke EE, Jaarsma T, Barnason SA, Byrne M, Doherty S, Dougherty CM, et al. Sexual counselling for individuals with cardiovascular disease and their partners: a consensus document from the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP). Eur Heart J. 2013;34(41):3217–35. doi: 10.1093/eurheartj/eht270. [DOI] [PubMed] [Google Scholar]
- 5.Kazemi-Saleh D, Pishgoo B, Farrokhi F, Fotros A, Assari S. Sexual function and psychological status among males and females with ischemic heart disease. J Sex Med. 2008;5(10):2330–7. doi: 10.1111/j.1743-6109.2008.00788.x. [DOI] [PubMed] [Google Scholar]
- 6.Kriston L, Gunzler C, Agyemang A, Bengel J, Berner MM. Effect of sexual function on health-related quality of life mediated by depressive symptoms in cardiac rehabilitation. findings of the SPARK project in 493 patients. J Sex Med. 2010;7(6):2044–55. doi: 10.1111/j.1743-6109.2010.01761.x. [DOI] [PubMed] [Google Scholar]
- 7.KOSKIMÄKI J, HAKAMA M, HUHTALA H, TAMMELA TL. Effect of erectile dysfunction on frequency of intercourse: a population based prevalence study in Finland. The Journal of urology. 2000;164(2):367–70. [PubMed] [Google Scholar]
- 8.Kaya C, Yilmaz G, Nurkalem Z, Ilktac A, Karaman MI. Sexual function in women with coronary artery disease: a preliminary study. Int J Impot Res. 2007;19(3):326–9. doi: 10.1038/sj.ijir.3901530. [DOI] [PubMed] [Google Scholar]
- 9.Megiddo E, Justo D, Arbel Y, Oren A, Heruti R, Banai S. [Sexual dysfunction and coronary artery disease in adult women]. Harefuah. 2009;148(9):611–4. 657. [PubMed] [Google Scholar]
- 10.Asadi-Lari M, Packham C, Gray D. Gender difference in health-related needs and quality of life in patients with acute chest pain. Br J Cardiol. 2005;12:459–64. [Google Scholar]
- 11.Tavallaii SA, Fathi-Ashtiani A, Nasiri M, Assari S, Maleki P, Einollahi B. Correlation between sexual function and postrenal transplant quality of life: does gender matter? J Sex Med. 2007;4(6):1610–8. doi: 10.1111/j.1743-6109.2007.00565.x. [DOI] [PubMed] [Google Scholar]
- 12.Shanmugasegaram S, Russell KL, Kovacs AH, Stewart DE, Grace SL. Gender and sex differences in prevalence of major depression in coronary artery disease patients: a meta-analysis. Maturitas. 2012;73(4):305–11. doi: 10.1016/j.maturitas.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Assari S, Ahmadi K, Kazemi Saleh D. Gender Differences in the Association between Lipid Profile and Sexual Function among Patients with Coronary Artery Disease. Int Cardiovasc Res J. 2014;8(1):9–14. [PMC free article] [PubMed] [Google Scholar]
- 14.Assari S, Moghani Lankarani M, Ahmadi K. Comorbidity influences multiple aspects of well-being of patients with ischemic heart disease. Int Cardiovasc Res J. 2013;7(4):118–23. [PMC free article] [PubMed] [Google Scholar]
- 15.Assari S, Moghani Lankarani M, Kazemi Saleh D, Ahmadi K. Gender modifies the effects of education and income on sleep quality of the patients with coronary artery disease. Int Cardiovasc Res J. 2013;7(4):141–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 17.Noohi S, Khaghani-Zadeh M, Javadipour M, Assari S, Najafi M, Ebrahiminia M, et al. Anxiety and depression are correlated with higher morbidity after kidney transplantation. Transplant Proc. 2007;39(4):1074–8. doi: 10.1016/j.transproceed.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Ifudu O, Paul HR, Homel P, Friedman EA. Predictive value of functional status for mortality in patients on maintenance hemodialysis. Am J Nephrol. 1998;18(2):109–16. doi: 10.1159/000013318. [DOI] [PubMed] [Google Scholar]
- 19.Alishiri GH, Bayat N, Fathi Ashtiani A, Tavallaii SA, Assari S, Moharamzad Y. Logistic regression models for predicting physical and mental health-related quality of life in rheumatoid arthritis patients. Mod Rheumatol. 2008;18(6):601–8. doi: 10.1007/s10165-008-0092-6. [DOI] [PubMed] [Google Scholar]
- 20.Aslani J, Nouhi S, Azizabadi-Farahani M, Moghani Lankarani M, Saadat S, Ghanei M. The socioeconomic statusand quality of life in patients with chronic obstructive pulmonary disease. Tanaffos. 2007;6(2):38–45. [Google Scholar]
- 21.Assari S, Soroush MR, Vishteh HRK, Mousavi B, Ghanei M, Karbalaeiesmaeil S. Marital relationship and its associated factors in veterans exposed to high dose chemical warfare agents. Journal of Family and Reproductive Health. 2008;2(2):69–74. [Google Scholar]
- 22.Azarkeivan A, Hajibeigi B, Alavian SM, Lankarani MM, Assari S. Associates of poor physical and mental health-related quality of life in beta thalassemia-major/intermedia. J Res Med Sci. 2009;14(6):349–55. [PMC free article] [PubMed] [Google Scholar]
- 23.Ghanei M, Aslani J, AzizAbadi-Farahani M, Assari S, Saadat S. Logistic regression model to predict chronic obstructive pulmonary disease exacerbation. Archives of Medical Science. 2007;3(4):360. [Google Scholar]
- 24.Moghani Lankarani M, Tavallaii S. Anxiety mediates the impact of medical comorbidities on quality of life. Dev World Epidemiol. 2010;1:31–6. [Google Scholar]
- 25.Ware JJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 26.Ware JE, Jr., Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. [Comparative Study Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.]. 1995;33(4 Suppl):AS264–79. [PubMed] [Google Scholar]
- 27.Alishiri GH, Bayat N, Salimzadeh A, Salari A, Hosseini SM, Rahimzadeh S, et al. Health-related quality of life and disease activity in rheumatoid arthritis. J Res Med Sci. 2011;16(7):897–903. [PMC free article] [PubMed] [Google Scholar]
- 28.Khedmat H, Karami GR, Pourfarziani V, Assari S, Rezailashkajani M, Naghizadeh MM. A logistic regression model for predicting health-related quality of life in kidney transplant recipients. Transplant Proc. 2007;39(4):917–22. doi: 10.1016/j.transproceed.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151(1):54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 30.Sanchez-Cruz JJ, Cabrera-Leon A, Martin-Morales A, Fernandez A, Burgos R, Rejas J. Male erectile dysfunction and health-related quality of life. European urology. [Comparative Study Research Support, Non-U.S. Gov’t]. 2003;44(2):245–53. doi: 10.1016/s0302-2838(03)00215-x. [DOI] [PubMed] [Google Scholar]
- 31.Brody S. The relative health benefits of different sexual activities. J Sex Med. 2010;7(4 Pt 1):1336–61. doi: 10.1111/j.1743-6109.2009.01677.x. [DOI] [PubMed] [Google Scholar]
- 32.Tasic I, Lazarevic G, Kostic S, Djordjevic D, Simonovic D, Rihter M, et al. Impact of depression on sexual dysfunction and HRQoL in CAD patients. Central European Journal of Medicine. 2014;9(1):54–63. [Google Scholar]
- 33.Gove WR, Hughes M, Style CB. Does marriage have positive effects on the psychological well-being of the individual? J Health Soc Behav. 1983;24(2):122–31. [PubMed] [Google Scholar]
- 34.Nickel JC, Tripp D, Teal V, Propert KJ, Burks D, Foster HE, et al. Sexual function is a determinant of poor quality of life for women with treatment refractory interstitial cystitis. J Urol. 2007;177(5):1832–6. doi: 10.1016/j.juro.2007.01.060. [DOI] [PubMed] [Google Scholar]
- 35.Uphold CR, Holmes W, Reid K, Findley K, Parada JP. Healthy lifestyles and health-related quality of life among men living with HIV infection. J Assoc Nurses AIDS Care. 2007;18(6):54–66. doi: 10.1016/j.jana.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 36.Coelho-Marques FZ, Wagner MB, Poli de Figueiredo CE, d'Avila DO. Quality of life and sexuality in chronic dialysis female patients. Int J Impot Res. 2006;18(6):539–43. doi: 10.1038/sj.ijir.3901470. [DOI] [PubMed] [Google Scholar]
- 37.Brezinka V, Kittel F. Psychosocial factors of coronary heart disease in women: a review. Soc Sci Med. 1996;42(10):1351–65. doi: 10.1016/0277-9536(95)00284-7. [DOI] [PubMed] [Google Scholar]
- 38.Meyer JP, Gillatt DA, Lockyer R, Macdonagh R. The effect of erectile dysfunction on the quality of life of men after radical prostatectomy. BJU Int. 2003;92(9):929–31. doi: 10.1111/j.1464-410x.2003.04530.x. [DOI] [PubMed] [Google Scholar]
- 39.Kaltenthaler E, Parry G, Beverley C, Ferriter M. Computerised cognitive-behavioural therapy for depression: systematic review. Br J Psychiatry. 2008;193(3):181–4. doi: 10.1192/bjp.bp.106.025981. [DOI] [PubMed] [Google Scholar]
- 40.Derogatis LR. Sexual function and quality of life: endpoints and outcomes. J Gend Specif Med. 2001;4(4):35–42. [PubMed] [Google Scholar]
- 41.Manjon JM. Pregnancy after laparoscopic uterine suspension for the treatment of dyspareunia caused by a retroverted and retroflexed uterus. J Minim Invasive Gynecol. 2007;14(4):506–8. doi: 10.1016/j.jmig.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 42.Monga TN, Monga M, Raina MS, Hardjasudarma M. Hypersexuality in stroke. Arch Phys Med Rehabil. 1986;67(6):415–7. [PubMed] [Google Scholar]
- 43.Kinlay S, Ganz P. Role of endothelial dysfunction in coronary artery disease and implications for therapy. Am J Cardiol. 1997;80(9A):11I–6I. doi: 10.1016/s0002-9149(97)00793-5. [DOI] [PubMed] [Google Scholar]
- 44.Nascimento ER, Maia AC, Pereira V, Soares-Filho G, Nardi AE, Silva AC. Sexual dysfunction and cardiovascular diseases: a systematic review of prevalence. Clinics (Sao Paulo). 2013;68(11):1462–8. doi: 10.6061/clinics/2013(11)13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morse WI. Inhibited sexual desire and sexual avoidance. Can Fam Physician. 1985;31:781–6. [PMC free article] [PubMed] [Google Scholar]