Abstract
Summary:
Head injury in children is a major concern all over the world. The increasing level of poverty in the world is exposing more children to trauma situations. The future consequences of trauma in these children are enormous, hence prevention they say, is better than cure.
Aim of the Study:
The study was designed to determine the etiological pattern, age group affectation and treatment outcome in children managed for head injury in our center.
Methods:
It was a prospective, descriptive and cross-sectional study of children with head injuries managed in our center from July 2010 to December 2013. Data were collected using structured proforma that was part of our prospective Data Bank approved by our hospital Research and Ethics Committee. Data were collected in accident and emergency unit, Intensive Care Unit, wards and out-patient clinic. The data was analyzed using Epi Info 7 software.
Results:
Total of 76 children managed by the unit and followed-up to a minimum of 3 months qualified for the study. There were 42 males. The age ranged from 7 months to 18 years with a mean of 8.66 years. There were 30 adolescent/teenagers. Road traffic accident formed 63.15%. Pedestrian accident was more among preschool and school children. Thirty-seven patients had mild head injury. Sixty-six patients were managed conservatively. The commonest posttraumatic effect was seizure (15.79%). Good functional outcome (≥4) was seen in 92.1%. Mode of accident and severity of injury affected the outcome.
Conclusions:
The etiologies of traumatic brain injury, from our study, were age dependent with falls commonest in toddlers and pedestrian accident commonest in pre-school and school ages. The outcome of treatment was related to severity of injury.
Keywords: Children, epidemiology, head injury, outcome
Introduction
Head injury is among the leading causes of acquired disability and deaths in infants and children.[1] Children's maturing brains pass through maximal synaptogenesis, pruning and refinement circuitry, in experience-dependent fashion with increased levels of glucose metabolism,[2] higher neurotrophic factors,[3] and elevated excitatory amino acid receptor binding and expression.[4,5] Posttraumatic depression of neuronal activity may result in lost developmental potentials,[6,7] and increased levels of apoptosis.[8,9] Because head trauma is the commonest cause of trauma death in children,[1,10] efforts should be geared towards the prevention. We prospectively studied 76 children managed for head injuries in our center over a 3½ year period.
Methods
This is a prospective, observational, and cross-sectional study of children managed for head injuries in our center from July 2010 to December 2013. In accident and emergency, patients were managed using primary and secondary survey methods of Advanced Trauma Life Support. They were classified into mild, moderate and severe head injuries using Glasgow Coma Score. Those with severe head injuries were admitted into Intensive Care Unit (ICU). Others were admitted into the wards. Radiological investigations were carried out for those who could afford them. Those with mild head injuries without radiological abnormalities and neurological deficits were observed for 24 h and discharged. Parents were instructed to bring the children to hospital if there were any of these: loss of consciousness, seizure, vomiting, increasing headache or neurological deficit before the next appointment. Those who had lesions requiring surgery were operated, while others were managed conservatively. Associated injuries were treated accordingly. Analgesics for pains, infusions, multivitamins and antibiotics (in open wounds) were given accordingly. Antiepileptic drugs were given to control posttraumatic seizures. We commenced high energy mixture feeding in unconscious patients on the 3rd day postinjury. The mixture was constituted using Pap, soya bean powder, crayfish powder, powdered milk, and palm oil, and given to them based on their daily requirements calculated from the weights of the children. Patients were followed-up on out-patient basis upon discharge. The Glasgow Outcome Score (GOS) was used to determine the functional outcome of the patients at 3 months postinjury. It classifies patients into five categories: Dead (1), vegetative state (2), severe disability (3), moderate disability (4), and good recovery (5).[11] Data were collected using structured proforma that was a component of our prospective Data Bank that was approved by our Ethics and Research Committee. Data were collected in accident and emergency, ICU, wards and out-patient department for 3 months postinjury. The data was analyzed using Environmental Performance Index (EPI) Info 7 software (Center for Disease Control and Prevention, Atlanta, Georgia, USA, 2011).
Results
There were 76 children, 42 males and 34 females. The age range was 7 months to 18 years with a mean age of 8.66 years. Thirty adolescent/teenagers and 11 toddlers were involved [Table 1].
Table 1.
Age group frequency
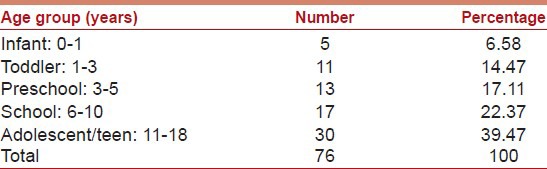
Among the infants, 80% were females and 20% males. In toddlers, 90.91% were males and 9.09% females. In preschool children, 53.85% were males and 46.15% were females. Among the school age group, males were 41.18% and females 58.82%. In adolescents/teenagers, males were 56.67%, while females were 43.33%.
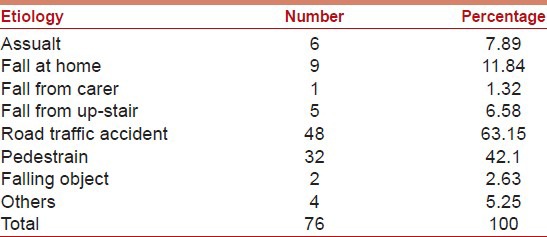
Forty-eight patients were involved in road traffic accident while 15 were from falls. Majority (66.67%) of the road traffic accident were pedestrian accident [Table 2].
Table 2.
Etiology frequency
Most toddlers were from falls (72.7%), while 69.2% of preschool and 76.47% of school children were pedestrian accident [Table 3].
Table 3.
Etiology versus age group
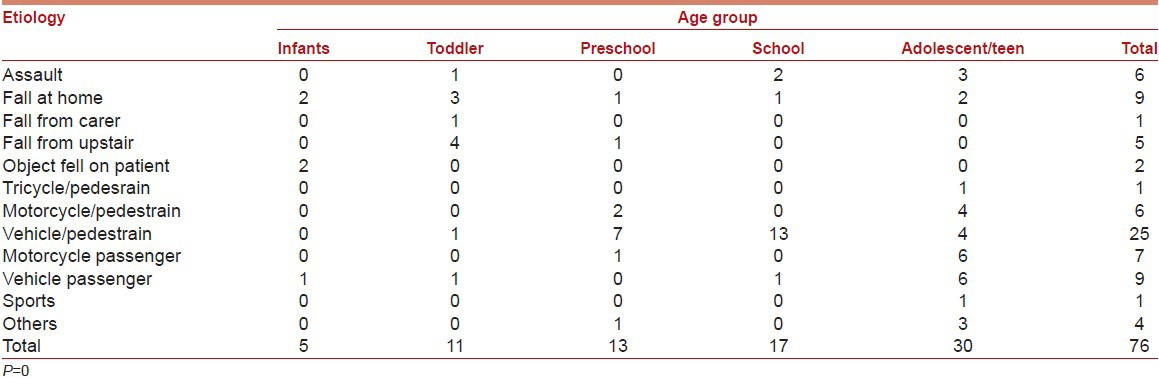
Among those that fell 66.67% were males, while 56.25% of the pedestrian accident was females. Among the passengers in vehicles/motorcycles, 56.25% were males. There was a significant relationship between age groups and etiological factors (P = 0) but age group did not affect the outcome significantly, P = 0.6832.
Thirty-seven children had mild head injury, and there was a significant relationship between severity of injury and outcome, P = 0.0017 [Table 4].
Table 4.
Diagnosis versus GOS
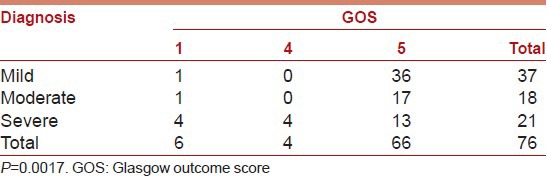
Sixty-six patients were managed conservatively while 10 had surgical care. Mode of treatment did not affect the outcome significantly, P = 0.7104. 70 children (92.1%) had good functional outcome of GOS ≥ 4, but mortality was 7.9%. Posttraumatic seizure was seen in 15.9% of our patients.
Discussion
There were 76 children in our study with males 55.26% and females 44.74%. Udoh and Adeyemo[12] in Benin, Nigerian, found males 51.2% and females 48.8%. Emejulu and Shokunbi[13] in Nnewi, Nigeria, found males 62% in their study. Chinda et al.[14] in Maiduguri, Nigeria, found males 66.7% in their study. This may be due to males being more active than females. Further analysis of the sex with age groups and etiological factors threw more light to our culture, effects of poverty, and environmental effects on growing children. 80% of the infants were females. In our culture, infant males are more protected because they are to continue the lineage of their fathers in our patrilineal society. In India, Vaghani, et al.[15] in their study of 29 infants found more males (59%) involved. This is contrary to our finding. However, India is mostly matrilineal; hence, females would be protected more than males in this age group.
Among the toddlers, males were 90.91%. Among them, 72.7% were from fall. At this age, the brain is growing with more excitatory neurotransmitters making the child to explore the environment.[4,5] In our environment, when the child starts to walk, the male is provided with a football while the female is provided with a baby toy. While the female tries to take care of the toy, the boy will be kicking his ball and pursuing it. For those living upstairs, when the ball falls to the ground the boy tends to follow the same route to go and pick the ball, hence the falling from the balconies and staircases. At times when children see their mates through the balconies playing downstairs, they try to join them through openings in the balconies or climb the balconies leading to fall through or from above the balconies. It is commonly seen in those living in uncompleted buildings and in barracks where the rails and balconies are in disrepairs. Some of our patients came from nearby barrack. Inside the house, the boy throws the ball and runs to pick it where it falls. If the ball falls on top of the object in the house, he climbs the object to get the ball, leading to falls inside the house. These have been documented by other authors.[16,17,18]
Among the preschool and school children, pedestrian accident was more. In preschool, there were 7 males and 6 females, showing even care for these children mainly in nursery schools. However, they are knocked down when minors try to cross roads with them. Among the school age group, there were 7 males and 10 females. This reflects the trend in our society where more females are sent to school than boys who are mainly sent to learn technical works and how to trade. While these boys stay in shops, those in school trek to schools and cross roads, thus exposing them to being knocked down by careless drivers. Due to poverty, many children cannot afford transport to schools hence they trek to and from schools. The springing up of private schools in our cities without zebra crossing in front of the schools, and poorly educated drivers on traffic signs are contributing factors to pedestrian accidents. The level could have been higher but for the ban on street hawking in our state. In many cities, children hawk wares along the roads to sustain their families, thereby exposing them to accident.
Among adolescents/teenagers, there were more males (56.67%) than females. They were involved in pedestrian and passenger accidents in 30% and 40% respectively. In this age group, the hormones[19] of puberty influence their behavior. Females tend to take care of their shiny bodies while boys tend to be more complacent and more daring in their behavior. In our environment, you often see adolescent/teenage males sauntering across the road wanting cars to wait for them to cross instead of the other way round, thus taking unnecessary risk of being knocked down by vehicles, tricycles and motorcycles.
In our study, majority were mild head injuries (48.68%). Chinda et al.[14] studied 45 children and found mild head injury in 46.7%. They formed the majority. Other authors found mild head injuries commonest in their studies.[13,15,20,21,22,23,24,25,26] Udoh and Adeyemo[12] in 127 cases studied found severe head injury commonest. This is contrary to our finding. In their study, they excluded all mild head injuries that were neuro-radiologically normal, thus excluding a large number of mild head injuries, and reducing their relative percentage.
Good functional outcome (GOS ≥ 4) was 92.1%. Emejulu and Shokunbi[13] in their study found 71.15%. Agrawal et al.[20] found 65.12% in their study. The difference might have been our high energy mixture, though they did not discuss theirs. Energy requirement in this age group is high, and head injury increases the energy consumption of patients. Clinical studies showed the benefit of a more enriching socioeconomic environment in the recovery of traumatic brain injury.[27,28]
The mortality in our study was 7.9%. Some authors found mortality <10%[12,20] while others found >10%.[13,14,15,29,30] The difference might have been on the extent of the injuries or on the mode of care especially their energy requirement. Poor outcomes after pediatric head injury had been found to be associated with level and duration of unconsciousness, extent of diffuse cerebral edema and the extent of injury to the parenchyma.[31,32,33] Posttraumatic seizure was seen in 15.9% of our patients. Seizure in traumatic brain injuries was seen in other series.[34,35,36,37] Elevated excitatory amino acid receptor binding and expression[4,5] in the immature brain increases the risk of seizures.[38]
Conclusion
Our study showed that etiology of traumatic brain injury in children we treated was age dependent. Falls were common in toddlers, pedestrian accident more among preschool and school age groups, while pedestrian and passenger-related head injuries were common among adolescents/teenagers. The study also showed that outcome of head injury in children we managed depended on the severity of the injury.
Recommendations
Better construction of rails in staircases and balconies to prevent the passage of children between adjacent iron and constructing them up to the decking or roof with prompt repair of spoilt ones will help reduce falls from them. Educating children on how to cross roads should be in curricula of nursery and primary schools. The road authorities should ensure that zebra crossings are constructed on roads near schools. They should ensure that every driver should recognize and understand what zebra crossing stands for. Speed limits in roads within towns should be conspicuously placed, and drivers should respect them. Road safety should ensure the road worthiness of vehicles plying our roads and also enforce traffic rules. These measures will go a long way in preventing head injuries in our children, for prevention they say, is better than cure.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.National Center for Health Statistics. Washington DC: US Government Printing Office; 1987. Advance Report of Final Mortality Statistics 1985. [Google Scholar]
- 2.Chugani HT, Phelps ME, Mazziotta JC. Positron emission tomography study of human brain functional development. Ann Neurol. 1987;22:487–97. doi: 10.1002/ana.410220408. [DOI] [PubMed] [Google Scholar]
- 3.Friedman WJ, Olson L, Persson H. Cells that Express Brain-Derived Neurotrophic Factor mRNA in the Developing Postnatal Rat Brain. Eur J Neurosci. 1991;3:688–97. doi: 10.1111/j.1460-9568.1991.tb00854.x. [DOI] [PubMed] [Google Scholar]
- 4.Insel TR, Miller LP, Gelhard RE. The ontogeny of excitatory amino acid receptors in rat forebrain – I-N-methyl-D-aspartate and quisqualate receptors. Neuroscience. 1990;35:31–43. doi: 10.1016/0306-4522(90)90117-m. [DOI] [PubMed] [Google Scholar]
- 5.Miller LP, Johnson AE, Gelhard RE, Insel TR. The ontogeny of excitatory amino acid receptors in the rat forebrain – II. Kainic acid receptors. Neuroscience. 1990;35:45–51. doi: 10.1016/0306-4522(90)90118-n. [DOI] [PubMed] [Google Scholar]
- 6.Fineman I, Giza CC, Nahed BV, Lee SM, Hovda DA. Inhibition of neocortical plasticity during development by a moderate concussive brain injury. J Neurotrauma. 2000;17:739–49. doi: 10.1089/neu.2000.17.739. [DOI] [PubMed] [Google Scholar]
- 7.Giza CC, Griesbach GS, Hovda DA. Experience-dependent behavioral plasticity is disturbed following traumatic injury to the immature brain. Behav Brain Res. 2005;157:11–22. doi: 10.1016/j.bbr.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Bittigau P, Sifringer M, Pohl D, Stadthaus D, Ishimaru M, Shimizu H, et al. Apoptotic neurodegeneration following trauma is markedly enhanced in the immature brain. Ann Neurol. 1999;45:724–35. doi: 10.1002/1531-8249(199906)45:6<724::aid-ana6>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 9.Pohl D, Bittigau P, Ishimaru MJ, Stadthaus D, Hübner C, Olney JW, et al. N-Methyl-D-aspartate antagonists and apoptotic cell death triggered by head trauma in developing rat brain. Proc Natl Acad Sci U S A. 1999;96:2508–13. doi: 10.1073/pnas.96.5.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnstone AJ, Zuberi SH, Scobie WG. Skull fractures in children: A population study. J Accid Emerg Med. 1996;13:386–9. doi: 10.1136/emj.13.6.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 12.Udoh DO, Adeyemo AA. Traumatic brain injuries in children: A hospital-based study in Nigeria. Afr J Paediatr Surg. 2013;10:154–9. doi: 10.4103/0189-6725.115043. [DOI] [PubMed] [Google Scholar]
- 13.Emejulu JK, Shokunbi MT. Aetiological patterns and management outcome of paediatric head trauma: One-year prospective study. Niger J Clin Pract. 2010;13:276–9. [PubMed] [Google Scholar]
- 14.Chinda JY, Abubakar AM, Umaru H, Tahir C, Adamu S, Wabada S. Epidemiology and management of head injury in paediatric age group in North-Eastern Nigeria. Afr J Paediatr Surg. 2013;10:358–61. doi: 10.4103/0189-6725.125448. [DOI] [PubMed] [Google Scholar]
- 15.Vaghani G, Singh PK, Gupta DK, Agrawal D, Sinha S, Satyarthee G, et al. Outcome of patients with traumatic head injury in infants: An institutional experience at level 1 trauma center. J Pediatr Neurosci. 2013;8:104–7. doi: 10.4103/1817-1745.117836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruce DA. Pediatric head injury. In: Wilkin RH, Rengachary SS, editors. Neurosurgery. 2nd ed. New York: McGraw-Hill; 1996. pp. 2709–15. [Google Scholar]
- 17.Ingebrigtsen T, Mortensen K, Romner B. The epidemiology of hospital-referred head injury in northern Norway. Neuroepidemiology. 1998;17:139–46. doi: 10.1159/000026165. [DOI] [PubMed] [Google Scholar]
- 18.Greenes DS, Schutzman SA. Infants with isolated skull fracture: What are their clinical characteristics, and do they require hospitalization? Ann Emerg Med. 1997;30:253–9. doi: 10.1016/s0196-0644(97)70158-6. [DOI] [PubMed] [Google Scholar]
- 19.The adolescent brain: Beyond raging hormones. Neuroscience research is suggesting some reasons why teenagers are that way. Harv Ment Health Lett. 2005;22:1–3. [PubMed] [Google Scholar]
- 20.Agrawal A, Agrawal CS, Kumar A, Lewis O, Malla G, Khatiwada R, et al. Epidemiology and management of paediatric head injury in eastern Nepal. Afr J Paediatr Surg. 2008;5:15–8. doi: 10.4103/0189-6725.41630. [DOI] [PubMed] [Google Scholar]
- 21.Yousefzadeh Chabok S, Ramezani S, Kouchakinejad L, Saneei Z. Epidemiology of pediatric head trauma in guilan. Arch Trauma Res. 2012;1:19–22. doi: 10.5812/atr.5289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Odebode TO, Abubakar AM. Childhood head injury: Causes, outcome, and outcome predictors. A Nigerian perspective. Pediatr Surg Int. 2004;20:348–52. doi: 10.1007/s00383-004-1196-5. [DOI] [PubMed] [Google Scholar]
- 23.Adesunkanmi AR, Oginni LM, Oyelami AO, Badru OS. Epidemiology of childhood injury. J Trauma. 1998;44:506–12. doi: 10.1097/00005373-199803000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Bener A, Al-Salman KM, Pugh RN. Injury mortality and morbidity among children in the United Arab Emirates. Eur J Epidemiol. 1998;14:175–8. doi: 10.1023/a:1007444109260. [DOI] [PubMed] [Google Scholar]
- 25.Shokunbi T, Olurin O. Childhood head injury in Ibadan: Causes, neurologic complications and outcome. West Afr J Med. 1994;13:38–42. [PubMed] [Google Scholar]
- 26.Csepregi G, Büki A, Futó J, Sándor J, Göbl G, Dóczi T. Management of patients with severe head injury in Hungary, in 2002. Orv Hetil. 2007;148:771–7. doi: 10.1556/OH.2007.27879. [DOI] [PubMed] [Google Scholar]
- 27.Hawley CA, Ward AB, Magnay AR, Long J. Outcomes following childhood head injury: A population study. J Neurol Neurosurg Psychiatry. 2004;75:737–42. doi: 10.1136/jnnp.2003.020651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 29.Adelson PD, Kochanek PM. Head injury in children. J Child Neurol. 1998;13:2–15. doi: 10.1177/088307389801300102. [DOI] [PubMed] [Google Scholar]
- 30.Glasgow JF, McGovern SJ. Initial management of the multiply injured child: Structured approach reduces morbidity and mortality. Curr Pediatr. 1997;7:187–92. [Google Scholar]
- 31.Feickert HJ, Drommer S, Heyer R. Severe head injury in children: Impact of risk factors on outcome. J Trauma. 1999;47:33–8. doi: 10.1097/00005373-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Jones PA, Andrews PJ, Easton VJ, Minns RA. Traumatic brain injury in childhood: Intensive care time series data and outcome. Br J Neurosurg. 2003;17:29–39. [PubMed] [Google Scholar]
- 33.Levin HS, Mendelsohn D, Lilly MA, Yeakley J, Song J, Scheibel RS, et al. Magnetic resonance imaging in relation to functional outcome of pediatric closed head injury: A test of the Ommaya-Gennarelli model. Neurosurgery. 1997;40:432–40. doi: 10.1097/00006123-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Vinchon M, Defoort-Dhellemmes S, Desurmont M, Dhellemmes P. Accidental and nonaccidental head injuries in infants: A prospective study. J Neurosurg. 2005;102:380–4. doi: 10.3171/ped.2005.102.4.0380. [DOI] [PubMed] [Google Scholar]
- 35.Barlow KM, Minns RA. Annual incidence of shaken impact syndrome in young children. Lancet. 2000;356:1571–2. doi: 10.1016/S0140-6736(00)03130-5. [DOI] [PubMed] [Google Scholar]
- 36.Myhre MC, Grøgaard JB, Dyb GA, Sandvik L, Nordhov M. Traumatic head injury in infants and toddlers. Acta Paediatr. 2007;96:1159–63. doi: 10.1111/j.1651-2227.2007.00356.x. [DOI] [PubMed] [Google Scholar]
- 37.Hymel KP, Stoiko MA, Herman BE, Combs A, Harper NS, Lowen D, et al. Head injury depth as an indicator of causes and mechanisms. Pediatrics. 2010;125:712–20. doi: 10.1542/peds.2009-2133. [DOI] [PubMed] [Google Scholar]
- 38.Annegers JF, Grabow JD, Groover RV, Laws ER, Jr, Elveback LR, Kurland LT. Seizures after head trauma: A population study. Neurology. 1980;30:683–9. doi: 10.1212/wnl.30.7.683. [DOI] [PubMed] [Google Scholar]


