Abstract
OBJECTIVE
To explore racial differences in reporting of early postpartum depressive symptoms. To explore whether racial differences in early postpartum experience (such as mother’s health status and social context) might account for racial differences in reported postpartum depressive symptoms.
METHODS
This was a telephone survey of 655 white, African-American, and Hispanic mothers between 2 and 6 weeks postpartum. Mothers reported on demographic factors, physical symptoms, daily function, infant behaviors, social support, skills in managing infant and household, access, and trust in the medical system. We explored racial differences in report of early postpartum depressive symptoms using bivariate and multivariate statistics.
RESULTS
African-American and Hispanic women more commonly reported postpartum depressive symptoms (43.9% and 46.8%, respectively) than white women (31.3%, P < .001). Similar factors (physical symptom burden, lack of social support, and lack of self-efficacy) were associated with early postpartum depressive symptoms in white, African-American, and Hispanic mothers. In a comprehensive model including other demographic factors, history of depression, physical symptoms, daily function, infant behavior, social support, skills in managing infant and household, access, and trust, the adjusted odds ratio for reported postpartum depressive symptoms remained elevated for African-American women at 2.16 (95% confidence interval 1.26–3.70) and Hispanic women at 1.89 (95% confidence interval 1.19–3.01) as compared with white women.
CONCLUSION
African-American and Hispanic mothers are at higher risk for reporting early postpartum depressive symptoms as compared with white mothers. Factors associated with these symptoms are similar among African-American, Hispanic, and white mothers.
Racial differences in traditional obstetric health outcomes are well documented. Higher rates of infant and maternal mortality are reported for African-American women as compared with white women.1,2 Although racial differences in specific obstetric complications (such as hypertensive disorders)3 have been reported, little research has investigated racial differences in immediate patient-focused health outcomes such as physical symptom burden and daily function. In fact, research on racial differences in the physical symptom burden and daily function of new mothers is virtually absent from the medical literature. Data do exist on 1 immediate health outcome new mothers may experience, symptoms of depression. However, the relationship between race and postpartum depressive symptoms has not been well established.
A great deal of research has focused on symptoms of depression postpartum because of its high prevalence and its negative consequences on patient well-being, functioning, mother–infant interaction, and cognitive child development.4–9 Prevalence rates vary from 10% to more than 50% based on the screening instrument used and the population studied.3,10,11 Although some investigators have reported that women of color have higher levels of depressive symptoms than white women, this assertion is difficult to evaluate, because race or ethnicity and low socioeconomic status are often confounded, and women of low socioeconomic status typically report higher levels of depressive symptoms.11 In addition, other studies that controlled for sociodemographic factors have found no racial differences in reports of depressive symptoms.11,12
Researchers have consistently reported that a past history of depression and lack of social support predict postpartum depressive symptoms.13 However, there is inadequate documentation of racial group differences in these factors and differences among the groups in other factors present in the immediate postpartum setting that may be responsible for racial differences in reports of depressive symptoms. For example, few studies have examined the association between depressive symptoms and physical factors such as postpartum symptoms and functional limitations. Likewise, the extent to which postpartum physical symptom burden, daily function, and infant characteristics differ for minority and majority women has not been studied. Although research on racial and ethnic disparities in other areas of medicine have found that access and trust often differ by patient race and sometimes explain differences in medical outcomes,14 the extent to which access to healthcare providers and trust in obstetric providers is associated with racial and ethnic disparities in prevalence rates of postpartum depressive symptoms also has not been investigated.
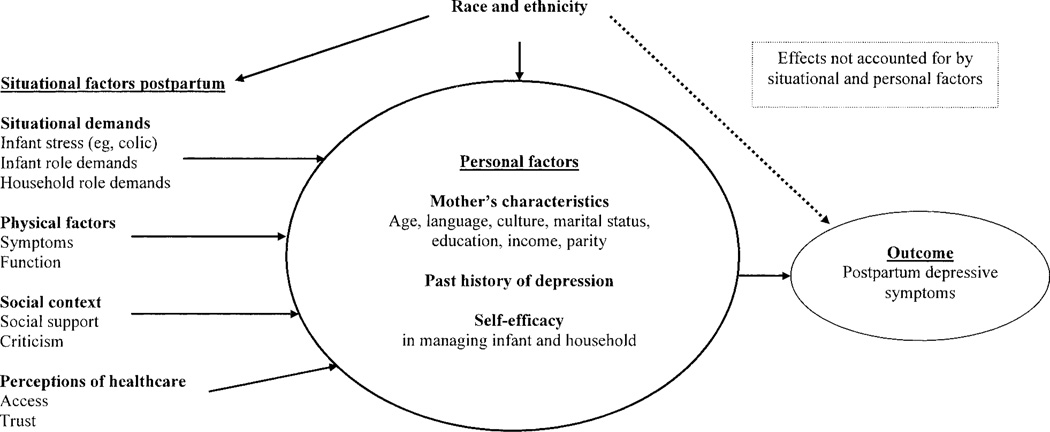
The theoretical model underlying our study of racial differences in the early postpartum experience assumes that depressive symptoms are a product of factors that may differ among the races such as situational demands (eg, infant stress—a colicky infant—and infant-related and household demands), the physical status of the mother affecting her ability to meet these demands (eg, physical symptoms and function postpartum), personal factors such as her sense of efficacy in managing the environment (eg, confidence to perform tasks related to the management of infants and household), and features of the social context that can buffer (eg, social support) or exacerbate stress (eg, social criticism) (Fig. 1). The model also assumes that each mother brings a set of characteristics to the birthing situation that affect the presence of environmental stressors and buffers (eg, the mother’s age, language, culture, marital status, education, income, parity), vulnerability to depressive symptoms (eg, past history of depression), and her perceptions of the availability of assistance from the health care system (eg access, trust). Our goal, therefore, was to describe racial differences in reporting of depressive symptoms and if these differences exist, to assess whether racial differences in situational factors, ie, situational demands, the mother’s health status, and the social context, might account for the differences in symptom reporting.
Fig. 1. Theoretical model.
Howell. Race and Postpartum Depression. Obstet Gynecol 2005.
METHODS
As part of a longitudinal cohort study, we interviewed postpartum white, Hispanic or Latina, and African-American or black women between 2 and 6 weeks postpartum, asking questions on demographics, physical symptoms, emotional symptoms, daily function, social support, personal factors, and perceptions of their health care providers. The overall study consists of 3 surveys and medical chart review. The analysis used data from the first of the 3 surveys and the medical chart review and examined racial differences in the early postpartum experience and their association with early postpartum depressive symptoms.
Our patient population included postpartum mothers who delivered at an urban tertiary care academic medical center between January and September of 2002. After obtaining approval from our institutional review board and acquiring written consent from physicians delivering patients at the study hospital, we approached women who met the following eligibility requirements: aged 18 years or older, English or Spanish speaking, delivered infants with birth weights 2,500 g or more, and had 5-minute Apgar scores greater than 6. In addition, mothers were excluded if they were hospitalized for more than 3 days after vaginal deliveries and more than 5 days after cesarean delivery. We used length of hospital stay as a proxy for maternal complications, because the Labor and Delivery log book did not reliably code complications.
We identified postpartum mothers through the Labor and Delivery Log and approached consecutive eligible (except for length of stay eligibility requirements) patients (Monday through Friday) to participate during their postpartum hospitalization. After acquiring written consent from participants, patients were called at home between 2 and 6 weeks postpartum (mean 31.2 days) for the baseline interview. Ten attempts to contact patients were made. Interviews were conducted in English and Spanish and lasted between 35 and 45 minutes. All participants received a monetary incentive to participate. We approached 1,166 patients who met all of our eligibility requirements; 202 refused to participate (17%), and 240 patients were unreachable by telephone (21%). We completed 724 surveys and successfully reached and interviewed 62% of eligible mothers we approached. In this analysis, we excluded women who were not white, Hispanic, or African American (69 patients). The final sample for this analysis was 655 patients. Patients who refused to participate were more likely to be white and to have a vaginal delivery as compared with women who participated in our survey.
Our survey instrument used validated scales when available and developed new scales based on the results of earlier focus groups with postpartum mothers and providers as well as extensive literature searches. Survey questions were written to address specific issues that were raised by postpartum mother focus group participants. The wording of our survey reflects content and language used by mothers in our focus groups. In addition our survey was pilot tested in a sample of 18 women to make sure the questions were understandable to participants. Patients were asked to think back to the first 2 weeks after they delivered their infants when answering questions on physical and psychological symptoms, daily function, infant behaviors, social support, self-efficacy (skills in managing infant and household), and perceptions of their health care provider (access and trust). Mothers also reported on demographic factors.
The primary variable of interest was race. Race was self-classified in 3 categories: white, African American or black, and Hispanic or Latina. Other maternal demographic variables included age (coded as a continuous variable), marital status (classified as single, not legally married but living as if married, married, separated, divorced, and widowed; later collapsed into single or not single), education (coded as less than eighth grade, less than high school, high school graduate, some college, and college graduate and collapsed into less than or equal to a high school education compared with those with more education), and household income (classified as less than $5000, $5000 to $15,000, more than $15,000 to $30,000, more than $30,000 to $45,000, more than $45,000 to $60,000, and more than $60,000). For some analyses, income was dichotomized into those whose annual incomes were up to $30,000 compared with those with greater incomes.
Parity and delivery type were obtained from review of medical records. Parity was classified as primiparous compared with multiparous. Delivery type was classified as vaginal (spontaneous, forceps, and vacuum) or cesarean. Past history of depression was defined by whether participants ever noted a time in the past that they felt depressed for 2 or more weeks or that they received treatment for depression. The time after delivery (in days) when the interview took place was coded as a continuous variable.
Physical symptoms were assessed by self-report, with a range of 0 to 8. Participants were asked about the presence or absence of 8 physical symptoms (vaginal bleeding, cesarean or episiotomy site pain, urinary incontinence, hemorrhoids, headaches, back pain, and hair loss). Physical functional limitations included the 4 items on physical function from the 12-Item Short-Form Health Survey (Cronbach alpha—a measure of the internal consistency of the scale—was 0.78).15 Role functioning was adapted from work by Tulman et al,16 and included 3 items focused on taking care of the newborn (feeding, bathing, and diapering). Each question had a 5-point response scale, and the possible range for role demands was 3–15 (Cronbach alpha = .68).
We evaluated the social context of participants in 2 ways. First we asked 5 questions on social support, which included questions on emotional support, instrumental support (support with managing every day task of…) with the baby, instrumental support with the household, and questions about partner support. Each question had a 5-point response scale, and the possible range for social support was 5–25 (Cronbach alpha = .65). Second, we asked 2 questions about negative social support in the form of criticism.
We also developed 5 questions on self-efficacy, the confidence that one can carry out a behavior necessary to reach a desired goal,17 including questions such as “How much of time did you feel that you were able to do all of the things needed to take good care of your baby… how much of time did you feel that you were able to do all of the things needed to take good care of your of your household?” All questions had a 5-point response scale with a possible range of 5–25 (Cronbach alpha = .71).
We developed 3 questions on access to provider based on work from Safran and others.18 Patients rated their ability to get through to the doctor’s or midwife’s office by telephone, ability to speak to their provider by telephone, and ability to see provider if the patient felt she needed to. All questions had 6-point response scales, with a possible range of 0–15 (Cronbach alpha = 0.87). We assessed overall trust in the provider by asking patients how much they trusted their providers on a 5-point scale.
We measured depressive symptoms with 2 items from the Primary Care Evaluation of Mental Disorders Procedure screening questionnaire.19 The item assessing depressed mood asked 1) “During the past two weeks, have you often been bothered by feeling down, depressed, or hopeless?” The item assessing anhedonia asked 2) “During the past two weeks, have you often been bothered by little interest or pleasure in doing things?”19 We changed the time reference from 1 month to 2 weeks to fit the time frame of our study. We chose to use the first 2 items of the Primary Care Evaluation of Mental Disorders Procedure to measure depressive symptoms rather than the Edinburgh Postnatal Depression Scale because the Edinburgh Postnatal Depression Scale is a multifactorial instrument of depression. Principal-component factor analysis has revealed that 4 items of this 10-item Edinburgh Postnatal Depression Scale load on depression and 3 items load on anxiety.20
The original Primary Care Evaluation of Mental Disorders Procedure study reported that a “yes” answer to 1 of these 2 questions was 86% sensitive and 75% specific compared with a subsequent telephone interview diagnosis of major depressive disorder. Later, Whooley et al19 compared the test characteristics of this 2-question finding instrument with 6 previously validated case instruments (long and short from of the Center for Epidemiologic Studies Depression Scale, long and short forms of the Beck Depression Inventory, the Symptom-Driven Diagnostic System for Primary Care, and the Medical Outcomes Study depression measure) and simultaneously administered a diagnostic interview (Quick Diagnostic Interview Schedule). A positive response to the 2-item instrument had similar test characteristics to other case-finding instruments.
Al statistical analyses were done using PC SAS 8.2 (SAS Institute Inc., Cary, NC). Bivariate analyses were conducted using χ2 tests to evaluate the association between race and categorical variables (ie, marital status) . One-way analysis of variance was used to assess the association between race and continuous variables: (ie, physical symptoms, physical functioning, role functioning, infant characteristics, social support, self efficacy, and access). Education and income were found to be highly correlated (r = 0.76) and moderately correlated with the outcome variable, so education was used in all multivariate analyses as a proxy for socioeconomic status. All independent variables were stratified by race, and the association between depressive symptoms and maternal demographics, physical and environmental factors, social factors, personal factors, and perception of health care were assessed using χ2 tests for categorical variables, and t tests for continuous variables. Multivariate logistic regression models were developed to assess the independent association of race, other demographics, past history of depression, physical symptom burden, physical functioning, infant-related role demands, infant characteristics, social support, self-efficacy, access, and trust with early postpartum depressive symptoms.
Additional analyses were conducted to assess whether time from delivery to interview affected reporting of other variables, eg, physical symptoms and depressive symptoms. There were no correlations between the time of interview and symptom reporting, indicating that time was not a confounder in these data.
RESULTS
Of 655 patients, 55% (n = 361) were white, 16% (n = 107) were African American, and 29% (n = 187) were Hispanic or Latina (Table 1). White women were older (mean age 33 years) as compared with African-American and Hispanic women (mean ages 27 and 28 years, respectively, P <.001). White women were more likely to be married (99%) compared with African-American and Hispanic women (44% and 69%, respectively, P <.001). White women also had significantly higher levels of education and income. White women were more likely to be primiparous than African-American or Hispanic women. There was no significant difference among white, African-American, and Hispanic women by delivery type. In addition, there was no significant difference by race in prevalence rates of past history of depression.
Table 1.
Postpartum Patient Population and Race
| White |
African American |
Hispanic |
||||
|---|---|---|---|---|---|---|
| Demographics | n | % | n | % | n | % |
| Study participants | 361 | 100 | 107 | 100 | 187 | 100 |
| Age* | ||||||
| 18–25 | 28 | 7.8 | 44 | 41.5 | 86 | 46.0 |
| 26–34 | 187 | 51.8 | 46 | 43.4 | 79 | 42.3 |
| ≥35 | 146 | 40.4 | 16 | 15.1 | 22 | 11.8 |
| Marital status* | ||||||
| Single or no partner | 5 | 1.4 | 60 | 56.1 | 59 | 31.6 |
| Married or living with partner | 356 | 98.6 | 47 | 43.9 | 128 | 68.5 |
| Education* | ||||||
| Less than high school | 4 | 1.1 | 14 | 13.1 | 45 | 24.1 |
| High school | 30 | 8.3 | 33 | 30.8 | 54 | 28.9 |
| Greater than high school | 327 | 90.6 | 60 | 56.1 | 88 | 47.1 |
| Annual household income* ($) | ||||||
| ≤ 30,000 | 27 | 8.0 | 56 | 56.0 | 100 | 61.4 |
| > 30,000–45,000 | 12 | 3.5 | 24 | 24.0 | 19 | 11.7 |
| > 45,000 | 300 | 88.5 | 20 | 20.0 | 44 | 27.0 |
| Parity* | ||||||
| Primiparous | 183 | 50.7 | 33 | 30.8 | 68 | 36.4 |
| Multiparous | 178 | 49.3 | 74 | 69.2 | 119 | 63.6 |
| Delivery | ||||||
| Vaginal | 254 | 70.4 | 70 | 65.4 | 132 | 71.0 |
| Cesarean | 107 | 29.6 | 37 | 34.6 | 54 | 29.0 |
| History of depression | ||||||
| Yes | 66 | 18.3 | 19 | 17.8 | 41 | 21.9 |
| No | 295 | 81.7 | 88 | 82.2 | 146 | 78.1 |
P < 05.
The overall status of patients 2 weeks after delivery differed for white, African-American, and Hispanic mothers on many factors within each category. Although all of the mothers regardless of group, experienced vaginal bleeding, white mothers experienced more cesarean or episiotomy site pain (87%) as compared with African-American and Hispanic women (66% and 70%, respectively, P <.001), less back pain (50%) than African-American and Hispanic women (74% and 70%, respectively; P <.001), and accomplished less because of their physical health (60%) than African-American and Hispanic women (42% and 51%, respectively, P <.001). White women experienced lower levels of infant-related role demands (bathing, diapering, and feeding) and reported more instrumental social support (receiving help taking care of their newborns). For example, 63% of white participants reported primary responsibility for diapering their babies as compared with 90% of African-American women and 92% of Hispanic women (P < .001). In contrast, 74% of white women reported instrumental social support (receiving help taking care of their newborns) as compared with 60% of African-American and 60% of Hispanic women (P < .001). In terms of access, white women rated their access to see their provider as excellent (47%) compared with African-American and Hispanic women (31% and 33%, respectively), P <.05). In addition, white women were more likely to completely trust their provider (76.1%) as compared with African-American and Hispanic women (66% and 61%, respectively, P <.01).
The status of patients on our key dependent measure, reports of depressive symptoms during the 2 weeks after delivery, differed for whites, African Americans, and Hispanics: 31% of white, 44% of African-American, and 47% of Hispanic women screened positive for depressive symptoms. These racial group differences on the depression screen led us to explore which factors differ among mothers not reporting symptoms of depression from those who do within each of the 3 racial or ethnic groups and to explore whether the pattern differs across the groups.
White mothers who reported depressive symptoms differed from those who did not on 6 factors (Table 2 and Table 3). Two of these referred to the poorer physical status and reduced physical functional competence among the mothers reporting symptoms of depression (physical symptoms, 4.6 compared with 4.3, P < .05: functional limitations, 7.6 compared with 7.0, P <.05) as compared with mothers not reporting symptoms of depression. Two additional factors referred to increased infant demands and less social support to buffer stress among the mothers reporting symptoms of depression (colicky infant, 1.3 compared with 1.1, P < 05; social support 20.4 compared with 21.4, P <.01) as compared with mothers not reporting these symptoms. The white mothers with depressive symptoms also reported feeling less efficacious in managing their infants and households (13.8 compared with 16.1, P < .01), and were less trusting of their providers (69.6% compared with 79.2%, P < .05) as compared with white mothers not reporting symptoms of depression.
Table 2.
Race, Depressive Symptoms, and Patient Characteristics
| White |
African American |
Hispanic |
||||
|---|---|---|---|---|---|---|
| Characteristics | Not Depressed (n = 246) |
Depressed (n = 112) |
Not Depressed (n = 60) |
Depressed (n = 47) |
Not Depressed (n = 99) |
Depressed (n = 86) |
| Age < 25 | 6.9 | 8.9 | 41.7 | 41.3 | 37.4 | 56.3* |
| Single or no partner | 1.2 | 1.8 | 58.3 | 53.2 | 30.3 | 33.3 |
| Education ≤ high school | 8.9 | 10.7 | 50.0 | 36.2 | 46.5 | 60.9† |
| Annual income < $30,000 | 6.9 | 9.5 | 61.4 | 48.8 | 57.3 | 67.1 |
| Primiparous | 50.8 | 50.0 | 31.7 | 29.8 | 36.4 | 36.8 |
| Vaginal delivery | 69.9 | 71.4 | 58.3 | 74.5 | 72.5 | 69.0 |
| History of depression | 16.7 | 21.4 | 11.7 | 25.5 | 16.2 | 27.6 |
Values are %.
P < .01.
P < .5.
Table 3.
Race, Depressive Symptoms, and Situational Factors
| White |
African American |
Hispanic |
||||
|---|---|---|---|---|---|---|
| Situational Factors | Not Depressed |
Depressed | Not Depressed |
Depressed | Not Depressed |
Depressed |
| Physical symptoms (0–8) | 4.3 | 4.6† | 3.9 | 4.8* | 4.1 | 4.8* |
| Physical function limitations (4–10) | 7.0 | 7.6† | 6.5 | 7.1 | 6.3 | 6.9† |
| Infant colic (1–3) | 1.1 | 1.3† | 1.1 | 1.2 | 1.1 | 1.4* |
| Criticism (1–4) | 1.2 | 1.3 | 1.2 | 1.3 | 1.1 | 1.3 |
| Infant-related demands (3–15) | 12.0 | 11.9 | 13.4 | 13.7 | 13.6 | 13.7 |
| Social support (5–25) | 21.4 | 20.4* | 20.2 | 18.2† | 20.4 | 17.8* |
| Self-efficacy (5–25) | 16.1 | 13.8* | 18.7 | 16.4* | 18.0 | 15.7* |
| Access (0–15) | 12.0 | 11.8 | 9.3 | 9.3 | 9.8 | 8.6† |
| Trust (1–5) | 4.8 | 4.6* | 4.5 | 4.6 | 4.5 | 4.3* |
Values are mean scores. The numbers in parentheses are the range for each scale.
P < .01.
P < .05.
African-American mothers who reported depressive symptoms differed from those who did not on only 3 factors, all 3 overlapping with those reported by white mothers. African-American mothers who reported symptoms of depression also reported more physical symptoms (4.8 compared with 3.9, P < .01) and less social support (18.2 compared with 20.2, P < .05) and felt less efficacious in managing infant and household (16.4 compared with 18.7, P < .01) as compared with African-American mothers who did not report symptoms of depression. Although the pattern of associations between these 3 factors and depressive symptoms were similar in both white and African-American mothers, African-American mothers reported higher levels of efficacy overall than did their white counterparts.
Hispanic mothers reporting depressive symptoms differed on 8 factors from Hispanic mothers who did not report symptoms of depression. Some of these differences were unique to this group. First, a greater proportion of the Hispanic mothers reporting depressive symptoms were less than 25 years of age (56% compared with 37%, P <.01) and were more likely to have a high school or less education (61% compared with 46%, P <.01) as compared with Hispanic women not reporting depressive symptoms. Hispanic mothers reporting depressive symptoms also reported having less access to their health care providers (8.6 compared with 9.8, P < .05) as compared with Hispanic mothers who did not report symptoms of depression.
The remaining 5 factors differentiating Hispanic mothers reporting depressive symptoms compared with mothers not reporting depressive symptoms were similar to those found in both whites and African Americans. Thus, Hispanic mothers reporting depressive were more symptomatic (4.8 compared with 4.1, P < .01), less functional (6.9 compared with 6.3, P < .05), and had more demanding infants (infant colic, 1.4 compared with 1.1, P < .01). In addition, Hispanic mothers reporting depressive symptoms also reported less social support (17.8 compared with 20.4, P < .01) and less efficacy in managing the infant and household affairs (15.7 compared with 18.0, P < .01) as compared with Hispanic mothers who did not report symptoms of depression.
In a multivariate model for depressive symptoms that controlled for demographics (age, marital status, education, parity, delivery type) and past history of depression, only race was significantly associated with depressive symptoms in the early postpartum period (results not shown). In our final model, we included the primary variable of interest, race, as well as past history of depression (known risk factor), physical symptoms, physical functional limitations, infant colic, infant-related role demands, social support, criticism, self-efficacy, access, and trust. Race was independently associated with depressive symptoms in this model. African-American women had an odds ratio (OR) of 2.16 (95% confidence interval [CI] 1.26–3.70) and Hispanic women had an OR of 1.89 (95% CI 1.19–3.01) as compared with white women (Table 4). Four additional variables were independently associated with depressive symptoms: physical symptoms (OR 1.17, 95% CI 1.02–1.35), infant colic (OR 1.70, 95% CI 1.20–2.42), social support (OR 0.91, 95% CI 0.86–0.95), and self-efficacy in managing the infant and household (OR 0.90, 95% CI 0.86–0.95). Past history of depression, physical functional limitations, infant role demands, criticism, access, and trust were not independently associated with reports of depressive symptoms in the early postpartum period.
Table 4.
The Multivariate Association Between Race and Depressive Symptoms
| Adjusted Model | |
|---|---|
| Race | |
| African American | 2.16 (1.26–3.70) |
| Hispanic | 1.89 (1.19–3.01) |
| History of depression | 1.17 (0.74–1.83) |
| Physical or environmental factors | |
| Physical symptoms | 1.17 (1.02–1.35) |
| Infant colic | 1.70 (1.20–2.42) |
| Physical functional limitations | 1.07 (0.98–1.17) |
| Infant-related role demands | 0.98 (0.90–1.08) |
| Social factors | |
| Social support | 0.91 (0.86–0.95) |
| Criticism | 1.16 (0.80–1.69) |
| Personal factors | |
| Self-efficacy | 0.90 (0.86–0.95) |
| Perceptions of health care | |
| Access | 0.99 (0.94–1.05) |
| Trust | 0.92 (0.70–1.21) |
Values are odds ratio and (95% confidence interval).
DISCUSSION
Racial differences in reports of early postpartum depressive symptoms were present in our study. Nearly one half of Hispanic mothers and 45% of African-American mothers reported early postpartum depressive symptoms as compared with approximately 31% of white mothers. Further, even when controlling for demographic, personal, and situational factors, the differences in rates of depressive symptoms among ethnic groups persisted. In addition, racial differences in physical and environmental factors, social factors, personal factors, and perceptions of health care providers existed. Despite these findings, there were more similarities than differences among the major factors associated with depressive symptoms within each of the 3 groups of women.
First, comparisons among the 3 ethnic groups showed that the status of women at 2 weeks differed significantly. White women reported more cesarean or episiotomy site pain as compared with African-American or Hispanic mothers. Despite having lower cesarean rates, white women also reported more physical functional limitations than their Hispanic or African-American counterparts. Hispanic women experienced higher rates of infant colic and infant illness than either white or African-American women. Although white women reported fewer infant-related role demands (diapering, feeding, and bathing their babies), they had more social support at home as compared with women of color. Interestingly, Hispanic and African-American women had higher rates of self-efficacy as compared with white women. African-American and Hispanic women had less access to their providers and were less likely to completely trust their health care providers. The key question is whether these differences account for the less frequent reports of depressive symptoms by white than by African-American and Hispanic mothers, a question that has been addressed in few if any prior studies.
A detailed examination of our data showed a greater number of similarities than differences in the association of depressive symptom reporting with other contextual factors. More physical symptoms, physical functional limitations, and infant colic were associated with depressive symptoms in whites, African Americans, and His-panics, although not all of these associations were significant. In addition, more social support, and more self-efficacy were associated with fewer depressive symptoms in whites, African Americans, and Hispanics. The data support our assumption that situational factors play a critical role in the generation of depressive symptom reports and show that they do so in all 3 racial or ethnic groups. Thus, despite the fact that report of more physical symptoms, more physical functional limitations, more infant colic, less social support, less self-efficacy, less access, and less trust were all associated with depressive symptoms in our stratified bivariate analysis by race, differences among whites, African Americans, and Hispanics on these factors did not account for the observed differences in depressive symptoms among the 3 ethnic groups. Unlike previous research, we did not find a significant association between past history of depression and report of depressive symptoms in this early postpartum period.
Our study has a few limitations. The impact of depressive mood on function and quality of life may be less intense and of shorter duration given that we used a well-known screening instrument to identify women with depressive symptoms rather than identifying women meeting Diagnostic and Statistical Manual of Mental Disorders 4th Edition criteria for major depressive disorder. However, our prevalence rates are similar to rates found when others have investigated postpartum depression in minority women3,10 The depression screening instrument we used has good psychometric properties and has been validated in other populations. Furthermore, it was brief so the interviewer could minimize burden to the patients questioned. Second, the cross-sectional design of our study does not allow us to draw causal relationships between more physical symptoms, infant colic, less social support, and less self-efficacy with depressive symptoms. However, our findings are consistent with others who found that both lack of social support and infant colic are associated with postpartum depression.5,21 Finally, we included only uncomplicated deliveries, and therefore our estimate of depressive symptoms may be an underestimate, because patients with adverse pregnancy outcomes may be more likely to report depressive symptoms and to do so for longer periods of time. The strengths of our study are the diverse patient sample, which increases the likelihood that our findings will be replicated in other populations, and the detailed data collected on the experiences, environment, and social and personal factors that determine the context in which mothers live during the early postpartum period.
Our results suggest that screening for postpartum depressive symptoms is important, particularly in women of color. Our research documents substantial racial or ethnic differences in the prevalence of early postpartum depressive symptoms. We also found that similar factors are associated with early postpartum depressive symptoms in whites, African Americans and Hispanic women. This latter result suggests that interventions aimed at these processes (such as social support, teaching skills aimed at helping mothers deal with colicky infants, etc.) may reduce early postpartum depressive symptoms for all women. It is also conceivable that interventions targeting both common and unique factors associated with early postpartum depressive symptoms in white, African-American, and Hispanic women may reduce racial and ethnic disparities in postpartum depressive symptoms.
Acknowledgments
Supported by the Agency for Healthcare Research and Quality and Robert Wood Johnson Foundation. The opinions, view, and conclusions expressed in this article are those of the authors and not necessarily those of the Robert Wood Johnson Foundation or Agency for Healthcare Research and Quality.
REFERENCES
- 1.Harper MA, Espeleand MA, Dugan E, Meyer R, Land K, Williams S. Racial disparity in pregnancy-related mortality following a live birth outcome. Ann Epidemiol. 2004;14:274–279. doi: 10.1016/S1047-2797(03)00128-5. [DOI] [PubMed] [Google Scholar]
- 2.Chang J, Elam-Evans LD, Berg CJ, Herndon J, Flowers L, Seed KA, et al. Pregnancy-related mortality surveillance-United States, 1991–1999. MMWR Surveill Summ. 2003;52:1–8. [PubMed] [Google Scholar]
- 3.Zayas LH, Cunningham M, McKee MD, Jankowski KR. Depression and negative life events among pregnant African-American and Hispanic women. Womens Health Issues. 2002;12:16–21. doi: 10.1016/s1049-3867(01)00138-4. [DOI] [PubMed] [Google Scholar]
- 4.Seguin L, Potvin L, St-Denis M, Loiselle J. Depressive symptoms in the late postpartum among low socioeconomic status women. Birth. 1999;26:157–163. doi: 10.1046/j.1523-536x.1999.00157.x. [DOI] [PubMed] [Google Scholar]
- 5.McKee MD, Cunningham M, Jankowski KR, Zayas L. Health-related functional status in pregnancy: relationship to depression and social support in a multi-ethnic population. Obstet Gynecol. 2001;97:988–993. doi: 10.1016/s0029-7844(01)01377-1. [DOI] [PubMed] [Google Scholar]
- 6.Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA. 1989;262:914–919. [PubMed] [Google Scholar]
- 7.Cogill SR, Caplan HL, Alexandra H, Robson KM, Kumar R. Impact of maternal postnatal depression on cognitive development of young children. Br Med J (Clin Res Ed) 1986;292:1165–1167. doi: 10.1136/bmj.292.6529.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field T. Maternal depression effects on infants and early interventions. Prev Med. 1998;27:200–203. doi: 10.1006/pmed.1998.0293. [DOI] [PubMed] [Google Scholar]
- 9.Field T, Healy B, Goldstein S, Perry S, Bendell D, Schan-berg S, et al. Infants of depressed mothers show “depressed” behavior even with nondepressed adults. Child Dev. 1988;59:1569–1579. doi: 10.1111/j.1467-8624.1988.tb03684.x. [DOI] [PubMed] [Google Scholar]
- 10.Vera M, Alegria M, Freeman D, Robles RR, Rios R, Rios CF. Depressive symptoms among Puerto Ricans: island poor compared with residents of the New York City area. Am J Epidemiol. 1991;134:502–510. doi: 10.1093/oxfordjournals.aje.a116122. [DOI] [PubMed] [Google Scholar]
- 11.Beeghly M, Olson KL, Weinberg MK, Pierre SC, Downey N, Tronick EZ. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Matern Child Health J. 2003;7:157–168. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- 12.Hobfoll SE, Ritter C, Lavin J, Hulsizer MR, Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol. 1995;63:445–443. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- 13.Gjerdingen DK, Chaloner KM. The relationship of women’s postpartum mental health to employment, childbirth, and social support. J Fam Pract. 1994;38:465–472. [PubMed] [Google Scholar]
- 14.Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–1163. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- 15.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Fawcett J, Tulman L, Myers ST. Development of the inventory of functional status after childbirth. J Nurse Midwifery. 1988;33:252–260. doi: 10.1016/0091-2182(88)90080-8. [DOI] [PubMed] [Google Scholar]
- 17.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 18.Safran DG, Kosinski M, Tarlov AR, Rogers WH, Taira DH, Lieberman N, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–739. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression: two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross LE, Gilbert Evans SE, Sellers EM, Romach MK. Measurement issues in postpartum depression part 1: anxiety as a feature of postpartum depression. Arch Women Ment Health. 2003;6:51–57. doi: 10.1007/s00737-002-0155-1. [DOI] [PubMed] [Google Scholar]
- 21.Mayberry LJ, Affonso DD. Infant temperament and postpartum depression: a review. Health Care Women Int. 1993;14:201–211. doi: 10.1080/07399339309516041. [DOI] [PubMed] [Google Scholar]