SUMMARY
Objective.
In the last few decades the implantology has achieved excellent results in the prosthetic rehabilitation of the partially or totally edentulous patients. The clinicians, given the pressing demand by patients, must deal with the situations in which the lack of the availability and sometimes the low quality of the bone can lead to the treatment failure. Although the manufacturers recommend to follow codified surgical protocols, alternative techniques of preparation, apt to ensure a better primary implant stability, have been developed.
The aim of this study was to determine in vitro, by using the resonance frequency (Osstell mentor), which technique of implant site preparation (piezo surgery, conventional, under-preparation, bone compaction, osteodistraction) is able to improve implant stability of type IV cancellous bone.
Methods.
10 pig ribs were prepared, and a surgical pre-drilled and calibrated guide for proper implant placement was used. On each rib, 5 implant sites were prepared, one for each technique.
Results.
One-way ANOVA did not show statistically significant differences among the “implant stability quotient” (ISQ) values of the 5 techniques utilized.
Conclusions.
Thus, in light of these results, in the clinical practice of the type IV bone one technique is replaceable with the others, as none of them improves implant stability. The choice should instead be directed to the technique that accelerates the healing process and the osseointegration.
Keywords: primary implant stability, resonance frequency analysis, implant site preparation
Introduction
Osseointegration is the biological process that leads to the direct structural connection between the vital bone and the surface of an implant under functional load.
This process is attributed to a number of consecutive events in osteoblast activation, with subsequent production and mineralization of the peri-implant osteoid tissue.
However, in case of reduced stability, micromotion threshold passing (50–150 nm) or bone necrosis caused by overheating (47°C), the present literature recommends that the fibrous encapsulation should prevail on the osseointegration (1, 2).
Many authors have described some of the key factors for achievement of osseointegration around the implants, underlining the importance of the bone implant coupling during the surgical phase (3, 4). Thus the primary implant stability represents one of the fundamental prerequisites for the achievement of the osseointegration and it must be maintained for the entire healing period. The primary stability is a mechanical phenomenon influenced by several factors such as the implant (design, size, macro and micro surface), the patient (quality and quantity of the bone) and the operator (surgical technique).
Numerous studies have compare both in vivo and in vitro the improvement of the primary stability in conical versus cylindrical implants (5–7). Also the implant surface treatment modalities increase the primary stability, since an increase in roughness may improve the contact between the bone and the implant. In addition, in vitro studies have shown that the sandblasted and etched implants promote the osteogenesis by improving the osteoblastic activity, as compared to the machined ones (8–10).
Regarding the quantity and the quality of the bone, there is a consistent literature showing that most of the failures in implantology are more linked to the quality than to the quantity of bone. Friberg et al. previously found a large number of failures in the resorbed maxillary with the soft bone (11). In a retrospective study, Jaffin and Bernam also reported implant failure in patients with poor bone density, besides other authors who documented that the major cause of implant failures was not linked to the healing, but rather to the indisputable influence of reduced bone density, with a failure rate ranging from 28 to 65% (12–14).
Several studies are present on factors related to the surgical technique in order to improve the implant stability. Indeed, some authors proposed the technique of dimensional under-preparation of the implant site in order to improve the bone-implant coupling and thus the implant stability (15–17). Other authors such as Summers, recommend the bone compaction through osteotomes to change the bone density and improve the stability (18).
With the technique of the expanders adopted by Sethi, it is possible to reach a 97% successful rate implant along with the implant stability improvement in the upper maxilla. Such improvement is confirmed by in vitro studies by Kraft, who compared the standard technique with that of the expanders where a considerable increase in stability and a high insertion torque were found (19–21).
The introduction of new tools for implant site preparation, such as piezo surgery, has generated an interest in the scientific community documented by various works. This technique favors a bone density improvement as compared to the conventional technique, with a rate of success of 100% (22). Stacchi-Vercellotti et al., by comparing the conventional technique with the piezo surgery, reach the conclusion that the two techniques are comparable as for the implant stability (23, 24).
The aim of this work was to evaluate the primary stability of 5 techniques of implant site preparation using the resonance frequency (Osstell mentor) in an animal model of type IV cancellous bone.
Materials and methods
In this study 50 Conical Active implants (Maco international) of conical shape, length 10 mm and diameter 3.9 mm mono coil were used. The surface treatment was performed by blasting with aluminum oxide particles (150–200 microns) followed by a double acid attack (Fig. 1).
Figure 1.
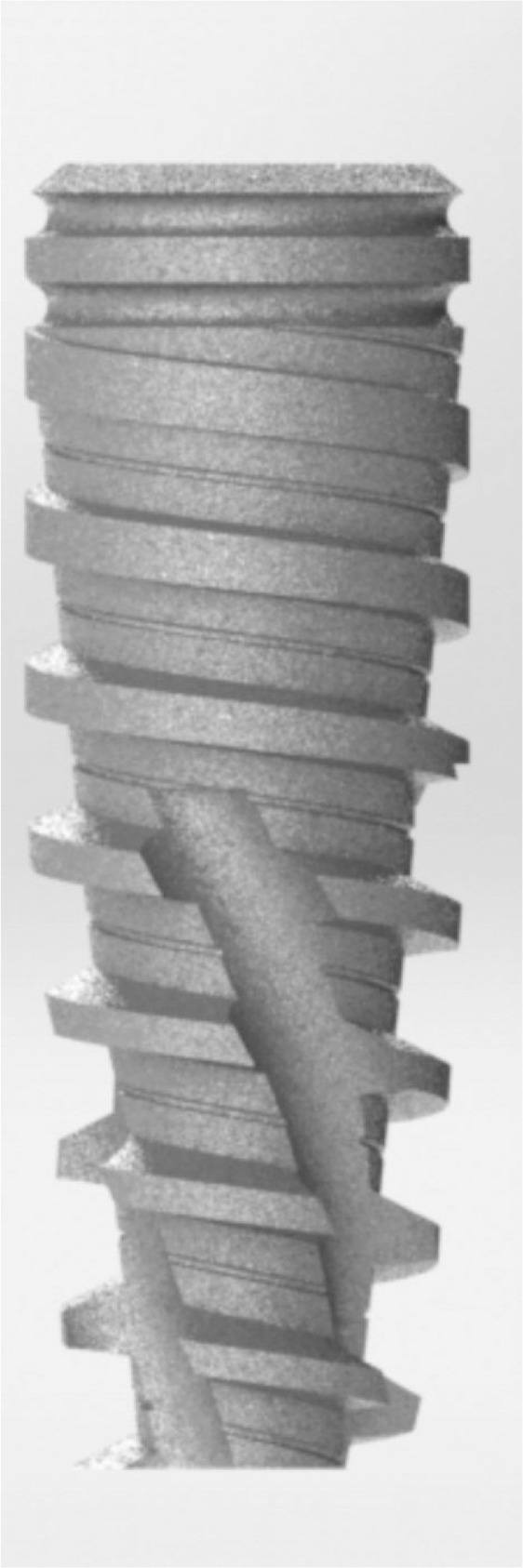
Conical Active implant (Maco International).
Ten samples of fresh bone pig ribs (7 cm length) were prepared.
In order to obtain a type 4 bone, the proximal part of the ribs was used, where the cortical component was reduced. Additionally, the cortical component was completely eliminated, leaving exposed only the medullary part for implant placement (25). The bone was further treated with a 20% glacial acetic acid solution one hour before performing the experiment, in order to increase the decalcification of the bone trabeculae (26). A reference template was also prepared in order to encode both the distance between the implants and the used technique.
For each rib, the sequence of the implant site preparation technique was randomly assigned by using a computer generated table, to increase the statistical rigor.
The surgical techniques used were the following ones:
1) conventional surgical technique (TC) with dedicated surgical cutters, as indicated by the manufacturer with a sequential cutter passage: 1.2 mm pilot cutter, 2.2 mm intermediate preparation cutter, 3.2 mm terminal cutter, to apply the implants in the soft bone.
2) The under-preparation technique (TS) with the preparation sequence, pilot cutter 1.2 mm, preparation cutter 2.2 mm and terminal cutter 3 mm. For the implant site with the conventional and under-preparation techniques, the Brane-mark protocol was adopted, in which the speed rotation of the cutters does not exceed 800 rpm under continuous irrigation.
3) Technique of bone expanders (TE): following the manufacturer’s instructions, the protocol contemplated to perform the hole to the desired length with a 1.2 mm pilot cutter and to reach the established 3 mm diameter by using bone expanders of various sizes in a sequential manner.
4) Bone compaction technique (TO): the Summers protocol was followed, with this preparation sequence: pilot cutter and bone compactors n° 1, 2 and 3, to obtain the 3 mm diameter.
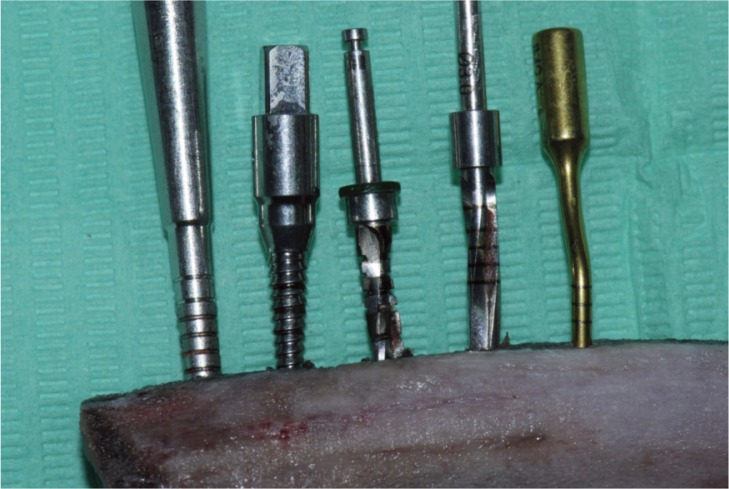
5) Technique with the piezo surgery (TP): the protocol contemplated the utilization of an handpiece with a pressure of 300g, the use of OP5 drill with coupled movement back and forth and 1/4 rotation, and then the passage in sequence of the other drills, IM2 (2 mm), OT4 (2mm), up to the final IM3 (3 mm) (Fig. 2).
Figure 2.
Five surgical techniques.
All implants were screwed using a manual ratchet and then exposed to bi-dimensional evaluation of the implant stability with the Osstell Mentor instrument (Osstell instrument, Integration Diagnostics AB, Gothenburg, Sweden) (Figs. 3, 4) (27–29).
Figure 3.
Implants placed in the bone.
Figure 4.
The Osstell Mentor instrument.
Statistical analysis
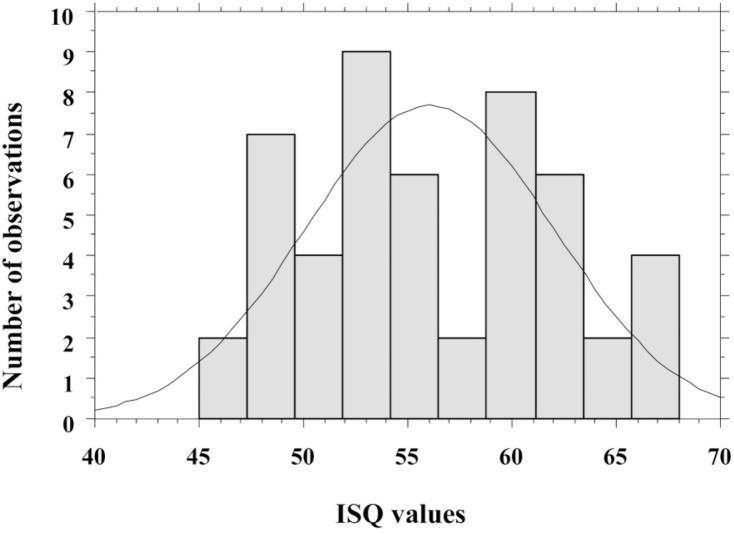
For each used technique, the statistical evaluation of central tendency (mean, median, mode) and variability (quartiles, variance, standard deviation, coefficient of variation, standard error) was performed (Tab. 1). For this type of analysis the “implant stability quotient” (ISQ) value was used as an independent variable, while the implantation technique was used as an explanatory qualitative variable at five levels. First, the distribution of the ISQ values was compared to the normal distribution using three tests (Kolmogorov -Smirnov, Lilliefors and Shapir-Wilk) (Fig. 5).
Table 1.
Descriptive statistics of ISQ values.
| Variable | ISQ TC | ISQ TS | ISQ TE | ISQ TO | ISQ TP |
|---|---|---|---|---|---|
| Number | 10 | 10 | 10 | 10 | 10 |
| Mean | 56.05 | 56.4 | 57.2 | 54.15 | 56.45 |
| Median | 55 | 57.75 | 55.5 | 53.5 | 57.25 |
| Mode | 55 | 61.5 | 52.0 | Multiple | Multiple |
| Frequency of Mode | 2 | 2 | 2 | 2 | 1 |
| Minimum | 49.0 | 46.0 | 48.5 | 49.0 | 45.0 |
| Maximum | 64.0 | 63.0 | 67.0 | 61.0 | 68.0 |
| Lower Quartile | 52.0 | 52.0 | 52.0 | 51.0 | 49.0 |
| Upper Quartile | 61.0 | 61.5 | 64.0 | 58.0 | 62.0 |
| Variance | 27.469 | 35.266 | 42.344 | 19.113 | 63.469 |
| Std. Dev. | 5.241 | 5.938 | 6.507 | 4.371 | 7.966 |
| Coef. Var. | 9.350 | 10.529 | 11.376 | 8.073 | 14.112 |
| Standard error | 1.657 | 1.877 | 2.057 | 1.382 | 2.519 |
TO: osteotomes technique; TE: expanders technique; TC: conventional technique; TS: under-preparation technique; TP: piezo surgery technique; ISQ: Implant Stability Quotient; Std. Dev: standard deviation; Coef. Var.: coefficient of variation.
Figure 5.
Frequency distribution of ISQ values.
Subsequently, one-way analysis of variance (one-way ANOVA) was used to test the effect of the technique on the in vitro implant stability, that is, to check whether the ISQ values of the five techniques differed in statistically significant manner.
Results
According to all three tests used, the distribution of ISQ values was not significantly different from a normal distribution, legitimizing the use of parametric analysis method such as ANOVA. The constructed one-way ANOVA model was not statistically significant and no statistically significant differences among the ISQ values of the different techniques were found (Tab. 2). Thus, the performed analysis shows that the five implantation techniques do not significantly differ in implant stability as measured in vitro by the ISQ value.
Table 2.
One-way analysis of variance (ANOVA) and post-hoc comparisons for ISQ values of the 5 techniques.
| ANOVA | F-value | P-value | Sum of squares | Mean square |
|
| ||||
| Main effect | 0.347 | 0.8445 | 52.150 | 13.038 |
|
| ||||
| Post-hoc comparisons (Fisher’s PLSD) | Mean Diff. | P-value | ||
|
| ||||
| TC-TE | −1.150 | 0.676 | ||
| TC-TO | 1.900 | 0.491 | ||
| TC-TP | −0.400 | 0.884 | ||
| TC-TS | −0.350 | 0.898 | ||
| TE-TO | 3.050 | 0.271 | ||
| TE-TP | 0.750 | 0.785 | ||
| TE-TS | 0.800 | 0.771 | ||
| TO-TP | −2.300 | 0.405 | ||
| TO-TS | −2.250 | 0.415 | ||
| TP-TS | 0.500 | 0.985 | ||
TO: osteotomes technique; TE: expanders technique; TC: conventional technique; TS: under-preparation technique; TP: piezo surgery technique; ISQ: Implant Stability Quotient.
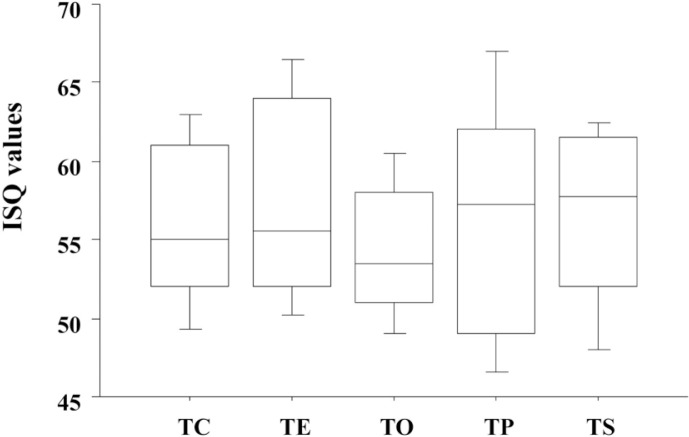
As shown in the descriptive statistics, the average ISQ values corresponding to the different techniques are very comparable, with the possible exception of the TO technique that shows a slightly lower stability (Fig. 6).
Figure 6.
Mean ISQ values of the various techniques.
TO: osteotomes technique, TE: expanders technique, TC: conventional technique, TS: under-preparation technique, TP: piezo surgery technique, ISQ: Implant Stability Quotient.
Discussion and conclusion
The implant stability plays a key role in the osseointegration process and is conditioned by the quality of the bone (cortical cancellous bone ratio). Indeed, some researchers have shown that there is a strong correlation between cortical thickness and ISQ, playing a crucial role on the implant stability. As reported in literature, the shape of the implant and the surface treatment may also improve the stability, as well as the experience of the operator (30, 31).
This study was performed to evaluate the primary implant stability of 5 preparation techniques by using the resonance frequency in peeled and etched pig ribs. The length and implant shape parameters, the quality of the type IV bone and the operator experience were maintained constant, while the surgical technique comprising 5 different preparation systems was the only variant introduced.
The results showed that the ISQ values obtained from 50 implants (10/technique) were comparable, and no statistical differences among these in vitro techniques in the type IV bone were found. The techniques appear to be comparable and the differences regarding the diameter of the preparation (3-mm for piezo, osteotomes, bone expanders and under-preparation techniques; 3,2 mm for the standard type IV bone technique) do not lead to increased stability.
These findings are in line with other in vitro studies that compared two (piezo vs standard) or at most three techniques (24, 26, 32–34). The emerging data is that none of the techniques can change the bone marrow density when the trabeculae are of poor quality. In fact, as already described by Martinez (35), in case of bones with low density and insufficient stability, it is advisable to use the bicortical anchorage. Thus, it is essential to follow some simple rules to improve the stability of the implant: to use conical implants active also at the level of the collar to achieve the maximum anchorage, to under-prepare the implant site to save as much as possible the residual cortical, and search for bicorticalism where possible.
Thus, in light of these results, in the clinical practice of the type IV bone one technique is replaceable with the other, as none of them improves implant stability. The choice should instead be directed to the technique that accelerates the healing process and the osseointegration.
Acknowledgments
We thank Maco International Ltd. for providing all the implant and instrumental material used in the study. Maco International Ltd. had no involvement in study design, in the collection, analysis and interpretation of data, in the writing of the report and in the decision to submit the report for publication.
Footnotes
Conflict of interest
The authors report no conflicts of interest related to this study.
References
- 1.Brunski JB. Biomechanical factors affecting the bone-dental implant interface. Clin Mater. 1992;10:153–201. doi: 10.1016/0267-6605(92)90049-y. [DOI] [PubMed] [Google Scholar]
- 2.Brunski JB. Avoid pitfalls of overloading and micro-motion of intraosseous implants (interview) Dent Implantol Update. 1993;4:77–81. [PubMed] [Google Scholar]
- 3.Albrektsson T, Eriksson A. Thermally induced bone necrosis in rabbits: relation to implant failure in humans. Clin Orthop Relat Res. 1985;195:311–312. [PubMed] [Google Scholar]
- 4.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 5.O’Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000;2:85–92. doi: 10.1111/j.1708-8208.2000.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 6.Zonfrillo G, Matteoli S, Ciabattini A, Dolfi M, Lorenzini L, Corvi A. Analysis and comparison of clutch techniques of two dental implants. J Mech Behav Biomed Mater. 2014;34C:1–7. doi: 10.1016/j.jmbbm.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Toyoshima T, Tanaka H, Ayukawa Y, Howashi M, Masuzaki T, Kiyosue T, et al. Primary Stability of a Hybrid Implant Compared with Tapered and Cylindrical Implants in an Ex Vivo Model. Clin Implant Dent Relat Res. 2014 Feb 9; doi: 10.1111/cid.12205. [DOI] [PubMed] [Google Scholar]
- 8.Davies JE. Mechanisms of endosseous integration. Int J Prosthodont. 1998;11:391–401. [PubMed] [Google Scholar]
- 9.Guizzardi S, Galli C, Martini D, Belletti S, Tinti A, Raspanti M, et al. Different titanium surface treatment influences human mandibular osteoblast response. J Periodontol. 2004;75:273–82. doi: 10.1902/jop.2004.75.2.273. [DOI] [PubMed] [Google Scholar]
- 10.Franchi M, Bacchelli B, Giavaresi G, De Pasquale V, Martini D, Fini M, et al. Influence of different implant surfaces on peri-implant osteogenesis: Histomorphometric analysis in sheep. J Periodontol. 2007;78:879–88. doi: 10.1902/jop.2007.060280. [DOI] [PubMed] [Google Scholar]
- 11.Friberg B, Jemt T, Lekholm U. Early failures in 4,641 consecutively placed Brånemark dental implants: a study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants. 1991;6:142–6. [PubMed] [Google Scholar]
- 12.Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 13.Johns RB, Jemt T, Heath MR, Hutton JE, McKenna S, McNamara DC, van Steenberghe D, Taylor R, Watson RM, Herrmann I. A multicenter study of overdentures supported by Brånemark implants. Int J Oral Maxillofac Implants. 1992;7:513–22. [PubMed] [Google Scholar]
- 14.Herrmann I, Lekholm U, Holm S, Kultje C. Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failures. Int J Oral Maxillofac Implants. 2005;20:220–30. [PubMed] [Google Scholar]
- 15.Friberg B, Ekestubbe A, Sennerby L. Clinical outcome of Brånemark system implants of various diameters: A retrospective study. Int Oral Maxillofac Implants. 2002;17:671–7. [PubMed] [Google Scholar]
- 16.Turkyilmaz I, Aksoy U, McGlumphy EA. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res. 2008;10:231–7. doi: 10.1111/j.1708-8208.2008.00084.x. [DOI] [PubMed] [Google Scholar]
- 17.Alghamdi H, Anand PS, Anil S. Undersized Implant Site Preparation to Enhance Primary Implant Stability in Poor Bone Density: A Prospective Clinical Study. J Oral Maxillofac Surg. 2011;69:e506–e12. doi: 10.1016/j.joms.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Summers RB. A new concept in maxillary implant surgery: The osteotome technique. Compendium. 1994;15:152, 154–56, 158. passim; quiz 162. [PubMed] [Google Scholar]
- 19.Sethi A, Kaus T. Maxillary ridge expansion with simultaneous implant placement: 5-year results of an ongoing clinical study. Int J Oral Maxillofac Implants. 2000;15:491–9. [PubMed] [Google Scholar]
- 20.Krafft T, Graef F, Winter W, Wichmann M, Karl M. Use of osteotomes for implant bed preparation-effect on material properties of bone and primary implant stability. J Oral Implantol. 2013;39:241–7. [Google Scholar]
- 21.Rambla-Ferrer J, Peñarrocha-Diago M, Guarinos-Carbó J. Analysis of the use of expansion osteotomes for the creation of implant beds. Technical contributions and review of the literature. Med Oral Patol Oral Cir Bucal. 2006;11:E267–E71. [PubMed] [Google Scholar]
- 22.Di Alberti L, Donnini F, Di Alberti C, Camerino M. A comparative study of bone densitometry during osseointegration: piezoelectric surgery versus rotary protocols. Quintessence Int. 2010;41:639–44. [PubMed] [Google Scholar]
- 23.da Silva Neto UT, Joly JC, Gehrke SA. Clinical analysis of the stability of dental implants after preparation of the site by conventional drilling or piezosurgery. Br J Oral Maxillofac Surg. 2014;52:149–53. doi: 10.1016/j.bjoms.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Stacchi C, Vercellotti T, Torelli L, Furlan F, Di Lenarda R. Preparation Techniques: Twist Drills versus Piezo-surgery. A Single-Blinded, Randomized, Controlled Clinical Trial. Clin Implant Dent Relat Res. 2013;15:188–97. doi: 10.1111/j.1708-8208.2011.00341.x. [DOI] [PubMed] [Google Scholar]
- 25.Lekholm U, Zarb GA. Patient selection and preparation. In: Brånemark PI, Zarb GA, Albrektsson T, editors. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago: Quintessence Publishing; 1985. pp. 199–209. [Google Scholar]
- 26.Sang-Hyun Moon, Heung-Sik Um, Jae-Kwan Lee, Chang Beom-Seok, Lee Min-Ku. The effect of implant shape and bone preparation on primary stability. J Periodontal Implant Sci. 2010;40:239–43. doi: 10.5051/jpis.2010.40.5.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nedir R, Bischof M, Szmukler-Moncler S, Bernard J-P, Samson J. Predicting osseointegration by means of implant primary stability. Clin Oral Implants Res. 2004;15:520–8. doi: 10.1111/j.1600-0501.2004.01059.x. [DOI] [PubMed] [Google Scholar]
- 28.Gupta RK, Padmanabhan TV. Resonance frequency analysis. Indian J Dent Res. 2011;22:567–73. doi: 10.4103/0970-9290.90300. [DOI] [PubMed] [Google Scholar]
- 29.Choi HH, Chung CH, Kim SG, Son MK. Reliability of 2 implant stability measuring methods in assessment of various periimplant bone loss: an in vitro study with the Periotest and Osstell Mentor. Implant Dent. 2014;23:51–6. doi: 10.1097/ID.0000000000000000. [DOI] [PubMed] [Google Scholar]
- 30.Su YY, Wilmes B, Hönscheid R, Drescher D. Application of a wireless resonance frequency transducer to assess primary stability of orthodontic mini-implants: an in vitro study in pig ilia. Int J Oral Maxillofac Implants. 2009;24:647–54. [PubMed] [Google Scholar]
- 31.Rozé J, Babu S, Saffarzadeh A, Gayet-Delacroix M, Hoornaert A, Layrolle P. Correlating implant stability to bone structure. Clin Oral Implants Res. 2009;20:1140–5. doi: 10.1111/j.1600-0501.2009.01745.x. [DOI] [PubMed] [Google Scholar]
- 32.Cano J, Campo J. Bone implant sockets made using three different procedures: a stability study in dogs. J Clin Exp Dent. 2012;4:e217–20. doi: 10.4317/jced.50803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baker JA, Vora S, Bairam L, Kim HI, Davis EL, Andreana S. Piezoelectric vs. conventional implant site preparation: ex vivo implant primary stability. Clin Oral Impl Res. 2012;23:433–7. doi: 10.1111/j.1600-0501.2011.02286.x. [DOI] [PubMed] [Google Scholar]
- 34.Yoon HG, Heo SJ, Koak JY, Kim SK, Lee SY. Effect of bone quality and implant surgical technique on implant stability quotient (ISQ) value. J Adv Prosthodont. 2011;3:10–5. doi: 10.4047/jap.2011.3.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martinez H, Davarpanah M, Missika P, Celletti R, Lazzara R. Optimal implant stabilization in low density bone. Clin Oral Implants Res. 2001;12:423–32. doi: 10.1034/j.1600-0501.2001.120501.x. [DOI] [PubMed] [Google Scholar]