Abstract
In this study, we examine the feasibility of cognitive behavior therapy (CBT) for children with anxiety in primary care, using two modes of treatment delivery. A total of 48 parents and youth (8–13) with anxiety disorders were randomly assigned to receive 10-sessions of CBT either delivered by a child anxiety specialist in the primary care clinic or implemented by the parent with therapist support by telephone (i.e., face-to-face or therapist-supported bibliotherapy). Feasibility outcomes including satisfaction, barriers to treatment participation, safety, and dropout were assessed. Independent evaluators, blind to treatment condition, administered the Anxiety Disorders Interview Schedule for Children (ADIS) and the Clinical Global Impression of Improvement (CGI-I) at baseline, post-treatment and 3-month follow-up; clinical self-report questionnaires were also administered. Findings revealed high satisfaction, low endorsement of barriers, low drop out rates, and no adverse events across the two modalities. According to the CGI-I, 58.3%–75% of participants were considered responders (i.e., much or very much improved) at the various time points. Similar patterns were found for remission from “primary anxiety disorder” and “all anxiety disorders” as defined by the ADIS. Clinically significant improvement was seen on the various parent and child self-report measures of anxiety. Findings suggest that both therapy modalities are feasible and associated with significant treatment gains in the primary care setting.
Keywords: randomized controlled trial, child anxiety, therapist-supported bibliotherapy, primary care, cognitive behavior therapy
Child anxiety disorders are common but frequently go undetected and untreated. Although much of the child primary care literature has focused on detecting and treating behavior problems (Reiff & Stein, 2003), epidemiologic findings reveal that anxiety disorders are also common in this setting (lifetime prevalence = 6.6–17%) (Busch et al., 2002). Despite the remarkable prevalence of anxiety disorders and their associated impact, in a primary care sample, only 31% of children with a DSM-IV anxiety disorder had received mental health services compared to 40% of children with past-year depressive disorders and 70% of children with ADHD (Chavira, Stein, Bailey, & Stein, 2004). The primary care pediatrician’s practice, with its potential for access, emphasis on developmental assessment, and its frequently cited status as a de facto mental health service (Regier, Goldberg, & Taube, 1978) represents a viable setting for the detection and possible treatment of children with anxiety disorders. Treating children in primary care also comes with the added advantages of lessening stigma due to seeking services in a medical setting rather than a mental health clinic, increasing patient comfort and trust, and facilitating communication between mental health and medical providers (Asarnow, Jaycox, & Anderson, 2002; Weersing & Walker, 2008). Given the positioning of primary care as a front-line service for children with mental health problems, studies examining the feasibility and effectiveness of evidence-based interventions in primary care are necessary.
To our knowledge, three randomized controlled trials (RCT) for child anxiety have been conducted in the primary care setting. These studies have included Cognitive Behavior Therapy (CBT) for children with anxiety and comorbid physical complaints delivered by mental health specialists (Warner et al., 2011), CBT for disruptive behavior and emotional problems delivered by nurses (Kolko, Campo, Kelleher, & Cheng, 2010), and a telephone based CBT approach for children with mild-moderate disruptive behavior and anxiety disorders (McGrath et al., 2011) delivered by paraprofessionals. In this latter study, telephone sessions were focused on self-help material review, skill modeling, problem solving around presenting issues, and skill implementation. Findings from these studies have mostly been positive with response rates ranging from 45–65%.
Bibliotherapy, which relies on self-administration of an intervention, represents a more minimal contact approach that can address important barriers to treatment such as access, transportation, time, childcare, and convenience and may be useful for stepped models of care seen in primary care settings. At present, there is a small RCT literature supporting the use of child anxiety bibliotherapy approaches, which are parent guided, and include varying levels of therapist support. In those RCTs that have included bibliotherapy supplemented by therapist-initiated telephone calls, response rates have ranged from 45–79% (Cobham, 2012; Creswell et al., 2010; Leong, Cobham, de Groot, & McDermott, 2009; Lyneham & Rapee, 2006). Delivery which has relied on email or parent initiated contact has resulted in less favorable outcomes (i.e., approximately 30% response). In a RCT and feasibility trial of parent-guided CBT, which included self-help materials, four telephone contacts, and four face-to-face sessions, response rates have ranged from 34–55% (Creswell et al., 2010; Thirlwall et al., 2013). Most of these studies have been conducted in specialty clinics with patients recruited from various sources, with the exception of Creswell et al., which was based in primary care and relied on pediatrician and self-referral. Overall, findings suggest that therapist-supported bibliotherapy and other minimal contact methods can be feasibly delivered to families with significant treatment gains. Findings also suggest that families may not have to come to a clinic to benefit from evidence-based interventions (Cobham, 2012).
In the current study, we build upon this existing literature by examining the feasibility of two modalities of CBT for child anxiety delivered to families in the primary care setting. The first modality was a standard individual therapy approach where a mental health specialist met with the parent and child in the primary care clinic for weekly sessions. The second modality, was therapist-supported, parent implemented CBT (i.e., therapist-supported bibliotherapy), where all therapist contact occurred by telephone. We examine whether these modalities can be feasibly delivered in the primary care setting, with a particular focus on issues of satisfaction, acceptability, barriers to treatment, safety, and attrition.
METHOD
Participants and Procedure
A total of 48 parents and youth (ages 8–13 years) with anxiety disorders participated in this study. Baseline characteristics are presented in Table 1.
Table 1.
Baseline Parent and Child Characteristics
| All n (%) | FF n (%) | TSB n (%) | p value | |
|---|---|---|---|---|
| Child Age, mean (SD), y | 48 | M= 9.75, SD = 1.7 | M = 9.50, SD = 1.6 | .61 |
| Parent Age, mean (SD), y | 48 | M = 41.69, SD=5.44 | M = 42.31, SD = 3.18 | .70 |
| Female | 27 (56.3) | 14 (58.3) | 13 (54.2) | .77 |
| Ethnicity | .22 | |||
| Caucasian | 35 (72.9) | 20 (83.3) | 15 (62.5) | |
| Latino | 5 (10.4) | 2 (8.3) | 3 (12.5) | |
| Multicultural | 8 (16.67) | 3 (12.5) | 5 (20.8) | |
| Parent Education | .47 | |||
| High school or tech | 7 (14.6) | 4 (16.7) | 3 (12.5) | |
| Some college | 10(20.8) | 4 (16.7) | 6 (25.0) | |
| College graduate | 31 (64.6) | 16 (33) | 15 (45.8) | |
| Married or Living Together | 41 (85.4) | 20 (83.3) | 21 (87.5) | .78 |
| Primary Anxiety disorder | .63 | |||
| Specific Phobia | 4 (8.3) | 2 (8.3) | 2 (8.3) | |
| Generalized anxiety | 12 (25) | 7(29.2) | 5 (20.8) | |
| Social anxiety | 16 (33.3) | 8(33.3) | 8 (33.3) | |
| Separation Anxiety | 10 (20.8) | 3(12.5) | 7 (29.2) | |
| Obsessive Compulsive | 6 (12.5) | 4 (16.7) | 2 (8.3) | |
| Comorbid Conditions | ||||
| Depressive disorders | 4 (8.3) | 3 (12.5) | 1 (4.2) | .30 |
| Disruptive Behavior Disorders | 9 (22.9) | 3 (12.5) | 6 (25.0) | .27 |
| Autism Spectrum Disorders | 2 (4.2) | 1 (4.2) | 1 (4.2) | 1.00 |
| Drop out | 7 (14.6) | 3 (12.5) | 4 (16.7) | .68 |
| Any prior counseling use (n=47) | 18 (38.3) | 8 (34.8) | 10 (41.7) | .63 |
| Any prior medication use | 5 (12.5) | 2 (10) | 3 (15) | .63 |
FF = face to face; TSB = therapist-supported bibliotherapy
Families were recruited from three primary care clinics through physician or self-referral. Recruitment materials included brochures, flyers, and signs describing the CBT program, which were posted in waiting areas and all clinic exam rooms. Parent informed consent and assent from the child were obtained at the baseline assessment visit. All procedures were approved by the appropriate Institutional Review Boards. Inclusion/Exclusion: Children between the ages of 8–13 years, who could speak English (as well as their parents) and had a primary diagnosis of social anxiety disorder, separation anxiety disorder, obsessive compulsive disorder, specific phobia, and/or generalized anxiety disorder based on the ADIS, were eligible to participate. Children receiving psychotropic medication were also included; medication dose was required to be stable for at least 3 months prior to study entry and for the duration of the study. Comorbid conditions were permitted provided they were not the child’s predominant (i.e., primary) diagnosis. All parents gave permission for the primary care providers to be a part of the intervention, which included pediatrician notification about child’s participation in the study and treatment progress.
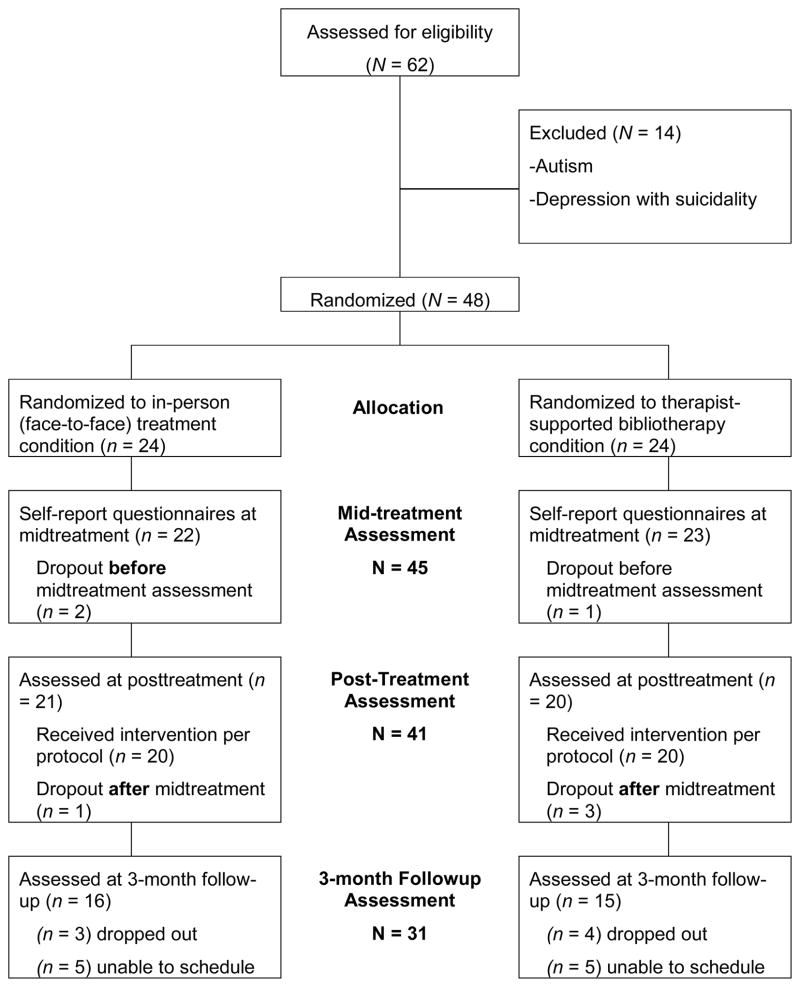
A total of 62 families were contacted and assessed for eligibility (see Figure 1). Of these families, 14 were excluded and 48 families were randomized. Given the feasibility focus and small sample size, a block randomization procedure was used to minimize potential imbalances in assignment to treatment condition; subjects were randomized in blocks of four. In total, 24 families received CBT delivered in-person at their primary care clinic and 24 families received a therapist-supported, parent implemented CBT intervention (i.e., therapist-supported bibliotherapy-TSB). Parent-child dyads completed interviews at baseline, post-treatment and three-month follow-up by an independent evaluator who was blind to treatment condition. Standardized anxiety questionnaires were administered at the three time points; a satisfaction measure was administered at post-treatment and three-month follow-up and a questionnaire about barriers was administered at post-treatment.
Figure 1.
CONSORT Chart
Treatments
Cool Kids Face-to-Face (FF)
The Cool Kids program (Lyneham & Rapee, 2006; Rapee, Abbott, & Lyneham, 2006) consists of 10 weekly sessions each lasting approximately 60–90 minutes and conducted with both the parent and child in the clinic. Parents are typically present for the first and last ten minutes of the session. The major components of the intervention include psychoeducation, changing unhelpful thoughts, exposures, problem solving exercises, parent management exercises, and assertiveness skills. The first eight sessions occur weekly and the last 2 sessions biweekly; treatment duration is three to four months.
Cool Kids Outreach-Therapist-supported Bibliotherapy (TSB)
As part of this program, families receive a parent workbook and a child workbook, based on the book, Helping Your Anxious Child, 2nd Edition (Rapee, Wignall, Spence, Cobham, & Lyneham, 2008) which includes the same core topics as the face-to-face condition. Each week parents are directed to read a chapter on a given CBT skill, complete activities designed to help them apply what they learned to their child’s fears and worries, and conduct various activities with their child. The child also has specific worksheets and activities to complete. During telephone sessions, the parent reviews what they worked on in the previous week and the therapist clarifies concepts and provides additional support as necessary regarding how to apply the skills. TSB telephone sessions occur exclusively with the parent and typically last 35–45 minutes. There are 10 sessions and the duration of the treatment is three to four months.
Engagement
All families in each condition also received engagement strategies at sessions 1, 5, and 7. These strategies focused on clarifying the need for treatment, increasing the family’s confidence in their ability to successfully complete the treatment, addressing attitudes about mental health care that may affect treatment, and problem solving regarding potential logistical barriers to services. This supplemental focus was limited to 15 minutes.
Role of primary care provider and clinic
All primary care providers received education in the form of a brief manual and pocket cards about anxiety, anxiety assessment, and treatment so that they could be aware of the Cool Kids program, facilitate referral, and respond to families’ questions and possible requests for medication. Parents who wanted their child to receive medication were referred back to their primary care provider for treatment or referral. In general, participation in this program did not require additional visits with the primary care provider, unless there were medical comorbidities that complicated diagnosis or treatment.
Independent Evaluator Training
Two masters-level and one PhD-level research assistant served as independent evaluators and administered diagnostic interviews and clinician- administered questionnaires. Training included 10-hours of didactics, the review and scoring of multiple (i.e., 5–6) mock interviews, observation of two in-person interviews conducted by a senior evaluator, and the administration of at least two in-person interviews while being observed. A final 80% agreement rate on severity ratings, and diagnoses was required.
Therapist Training
Child anxiety specialists (CAS), the therapists who provided the CBT, had at least a Masters level education in a counseling-related profession. All CASs were trained to fidelity using preparatory self-study, a 2-day didactic workshop, viewing of exemplar case sessions, proficiency exams, supervised administration of at least two full cases, and ongoing supervision. Adherence with at least 80% of the core components/skills of the protocol (were the components administered or not), and a mean score reflecting good competence (a score of 6 or above) for each skill that was reviewed in the session (range from 0 – 7) were required. Further, mean ratings consistent with good competence were required on non-specific therapy components including rapport, empathy, and goal consensus.
Measures
Anxiety Disorders Interview Schedule for Children-Child and Parent Report (ADIS-C/P) (Silverman & Albano, 1996)
The ADIS is a gold-standard semi-structured diagnostic interview designed to assess DSM-IV childhood anxiety disorders as well as depressive and behavioral disorders. Clinical severity ratings (CSR) range from 0–8 and a CSR of at least 4 is required for a clinical diagnosis. In this study, a child’s primary diagnosis was determined by CSR ratings from both parent and child interviews. Remission from a disorder was defined as a CSR rating of <= 3 based on both the parent and child ADIS.
Screen for Anxiety and Related Disorders (SCARED) (Birmaher et al., 1999)
The SCARED is a 41-item measure that has excellent psychometric properties and was developed as a self-and parent-report screening tool to assess anxiety disorders in youth. For each item, severity of symptoms is rated using a 0- to 2-point scale. For the current sample, Cronbach alpha coefficients were .87 for the parent SCARED and .93 for the child SCARED.
Clinical Global Impression Scale – Improvement (CGI–I) (Guy, 1976)
The CGI-I is a well-established clinician-rated global rating of change in illness symptom severity and impairment (CGI-I) that has been used in numerous pediatric randomized controlled trials. The CGI-I anchors include: 1 = very much improved, 2 = much improved, 3 = minimally improved, 4 = no change, 5 = minimally worse, 6 = much worse, and 7 = very much worse. In this study, a child was considered a responder if rated by the independent evaluator as “much improved” or “very much improved” based on interviews with parents and children.
Children’s Global Assessment Scale (C-GAS) (Shaffer et al., 1983)
The C-GAS is measure of global functional impairment and uses a 0–100 scale, with higher scores indicating better overall functioning. A score of 60 or below is usually assigned to children with clinically significant functional impairment. Ratings on the C-GAS were assigned following the completion of the child and parent interviews.
Parent Consumer Satisfaction Scale (March, 1999)
This measure consists of 14 items rating parents’ level of satisfaction with the intervention that their child received. Eleven of the items use a 7-point Likert scale, where higher scores reflect more favorable responses (e.g., 1 = “very unacceptable,” 4 = “neutral,” and 7 = “very acceptable”); the remaining 3 items are open-ended questions regarding the intervention. The Cronbach alpha coefficient in the current sample was .85.
Barriers to Treatment Participation Scales (Kazdin, Holland, Crowley, & Breton, 1997)
This measure consists of 44 items and assesses parents’ experiences of obstacles to participating in their child’s treatment. There are four subscales: 1) stressors or obstacles that compete with treatment (e.g., family stress, time etc.); 2) treatment demands and issues (e.g., treatment as too difficult, confusing, long etc.); 3) perceived relevance of treatment and; 4) relationship with therapist. Items are rated on a 5 point Likert scale; 1 = never a problem, 2 = occasionally, 3 = sometimes, 4 = often; 5 = very often. The Cronbach alpha coefficient in the current sample was .86.
Data Analysis Plan
Using appropriate statistics, variables were tested for normality. Analyses were performed to assess baseline differences between the treatment conditions (see Table 1). Intent-to-treat guidelines were applied for all analyses. Multilevel modeling analyses were exploratory given small sample size and lack of power. For each continuous outcome, multilevel modeling was used to account for the nested data structure (repeated-measures nested within individuals). A statistically non-significant interaction term reflected no intervention group differences in the changes in target outcomes across time. In these cases, a second multilevel model was run removing the interaction term. Chi-square analyses were used to examine response rates and diagnostic remission; multiple imputation was used to account for missing data at 3 - month follow-up.
RESULTS
Descriptive analyses
Descriptive findings are presented in Table 1. The majority of the child participants in the study were Caucasian (73%) and from households where the primary caregiver had a college education and parents were married. Social phobia was the most common primary disorder and the majority of participants had more than one anxiety disorder diagnosis (75%). Among the 12 participants who had only one anxiety disorder, three had a specific phobia diagnosis. There were no pre-treatment differences on any demographic or clinical variable across groups.
Feasibility Related Outcomes
Therapist Adherence
Approximately 20% of digital audio recordings were rated for adherence. Overall, adherence rates for treatment components (number of components delivered/total possible components) were high ranging from 80–100% with a mean of 95.2%. The mean score for how competently the components were delivered was M = 6.19 (SD = .23), using a 7-point Likert scale where higher scores reflect greater competence. The mean score for nonspecific therapy skills such as empathy and rapport was M = 6.67 (SD = .65) using a 7 point scale. There were no significant differences in adherence ratings between the FF and TSB groups.
Safety and attrition
All families accepted the randomization process, the measures and procedures were completed without incident, and there were no reported difficulties with understanding the program materials. Seven families (15%) dropped out of treatment; 3 (12.5%) from the FF condition and 4 (17%) from the TSB condition. Reasons for drop out included scheduling conflicts (n = 3), child non-compliance (i.e., child not doing any exercises and child refusing to attend FF session due to embarrassment) (n = 2), child improvement (n = 1), and initiation of new dosage for ADHD medication (n = 1). None of the parents reported a worsening of their child’s anxiety symptoms during participation in the treatment. Also, none of the parent’s requested a referral to the pediatrician for medication to treat their child’s anxiety.
Treatment Duration and Engagement
The length of time it took for patients to complete the Cool Kids program was M= 98.25 days (approximately 3 months and 8 days) for families attending FF sessions and M = 103.10 days (3 months and 13 days) for families receiving TSB. The number of no-shows/missed appointments was M = .61 among families in the FF group and M = 1.65 in the TSB group (F = 2.93, p = .10). The duration of treatment sessions in the TSB condition ranged from M = 35.28 to 57.31 minutes. In the FF condition, which involved the therapist meeting separately and conjointly with parent and child, session length ranged from M = 61.5 to M = 89.73 minutes. Using one-way ANOVAs, the duration of each of the respective 10 sessions was significantly shorter using TSB compared to the FF approach (supplementary Table online). Important to note, the duration of sessions in both conditions was lengthened because of adjunctive engagement strategies at sessions 1, 5, and 7. Parent satisfaction with treatment ranged from M = 6.4 to M = 6.53 at post-treatment and 3-month follow up (see Table 2), with a score of 6 indicating high satisfaction and a score of 7 indicating superior satisfaction. Mean scores on the treatment barriers subscales (i.e., competing stressors and obstacles, perceived relevance of treatment, treatment demands and issues, and relationship with therapist) ranged from M = 1.00 to 1.7 on 1 – 5 point scale, suggesting that barriers ranged from “never a problem” to “occasionally a problem”. There were no significant differences between treatment groups on satisfaction or endorsement of barriers (supplementary Table online).
Table 2.
Means (M), Standard Deviations (SD) and multilevel regression models for continuous outcomes
| Baseline | Post-Treatment | 3 month Followup | Time X Group | Time | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| FF M (SD) | TSB M (SD) | FF M (SD) | TSB M (SD) | FF M (SD) | TSB M (SD) | B p value | B p value | |
| SCARED-C | 25.20 (16.23) | 27.57 (14.01) | 8.59 (6.55) | 14.71 (10.23) | 10.24 (10.16) | 16.33 (14.21) |
B= −2.19 p = .08 |
B= −5.31 p < .001 |
| SCARED-P | 33.03 (11.19) | 32.13 (9.66) | 12.5 (9.79) | 12.6 (8.27) | 13.9 (10.33) | 17.18 (12.27) |
B= −1.09 p = .35 |
B= −7.34 p < .001 |
| Satisfaction | --------- | ---------- | 6.50 (.44) | 6.51 (.48) | 6.63 (.30) | 6.44 (.62) | ----------- | ------------ |
| CSR-primary Anx | 5.46 (.78) | 5.54 (.66) | 1.50 (1.16) | 2.00 (1.41) | 1.95 (1.47) | 2.15 (1.46) |
B= −0.12 p = .87 |
B= −1.77 p < .001 |
| ADIS # of Anx Dxs | 2.42 (1.35) | 2.67 (1.27) | .33 (.97) | .55 (.83) | .07 (.26) | .43 (1.16) |
B= 0.22 p = .92 |
B= −1.16 p < .001 |
| CGAS | 53.42 (5.89) | 53.21 (4.26) | 80.00 (9.07) | 77.67 (8.94) | ---------- | ---------- |
B= 3.30 p = .21 |
B= 25.46 p < .001 |
Note:--------- = not administered; FF = face-to-face; TSB = therapist-supported bibliotherapy; SCARED = Screen for Anxiety Related Emotional Disorders-P/C (Parent and Child Versions); CSR = Clinician Severity Rating from ADIS (for primary anxiety disorder) (0–8); ADIS-P/C = Anxiety Disorders Interview Schedule (Parent and Child Versions); # anx dxs = sum of anxiety disorders; CGAS = Children’s Global Assessment Scale (based on child and parent diagnostic interviews).
Exploratory analyses; Multilevel Models
Mean scores for the continuous measures of anxiety symptoms, number of anxiety disorders, and clinical severity at the three assessment points are presented in Table 2. Using multilevel models, there were no statistically significant cross-level Time X Intervention Group interactions for any of these measures (see Table 2). There were, however, statistically significant Time effects for each of the outcomes, suggesting significant decreases in scores over time.
Responder Status and Remission Rates
Responder status as defined by the CGI and remission rates as defined by the ADIS are presented in Table 3.
Table 3.
Chi Square analyses for categorical indices of treatment response based on independent evaluator ratings (multiple imputation used to account for missing data at 3 month followup)
| FF N = 24 n (%) |
TSB N = 24 n (%) |
X2 p value |
|
|---|---|---|---|
| Post Treatment | |||
| CGI-I; Much or Very Much Improved | 18 (75) | 18 (75) | X2 = 0 p = 1.00 |
| ADIS; Remission from Primary Anxiety Disorder | 18 (75) | 15 (62.5) | X2 = .87 p = .35 |
| ADIS; Remission from All Anxiety Disorders | 18 (75) | 13 (54.2) | X2 = 2.27 p = .13 |
| 3 Month Follow Up | |||
| CGI-I; Much or Very Much Improved | 16 (66.7) | 14 (58.3) | X2 = 0.36 p = .55 |
| ADIS; Remission from Primary Anxiety Disorder | 21 (82.5) | 17 (70.8) | X2 = 2.02 p = .16 |
| ADIS; Remission from All Anxiety Disorders | 15 (62.5) | 14 (58.3) | X2 = .09 p = .77 |
Note: FF = face-to-face; TSB = therapist-supported bibliotherapy; ADIS = Anxiety Disorders Interview Schedule (remission ratings are based on combination of parent and child reports on ADIS); CGI-I = Clinician Global Impression of Improvement (a combined rating derived from parent and child interviews).
DISCUSSION
This study evaluates the feasibility of two therapy modalities for the treatment of child anxiety in a primary care setting. Findings reveal that both modalities are feasible in primary care and associated with treatment gains. Families completed the treatment program without incident, and there were no reported difficulties with understanding the program materials in either group. On a standardized measure of barriers to treatment, families reported that barriers such as competing demands, time, family stress, etc. were only “occasionally a problem”. Importantly, attrition rates in both groups were low (approximately 15%) and parents reported high satisfaction with the CBT program regardless of whether they received the intervention in-person at the primary care clinic or implemented the intervention using self-help materials with therapist support by telephone. Such outcomes are consistent with previous studies using parent-guided CBT in primary care, which included four in-person contacts and four telephone contacts (Creswell et al., 2010; Thirlwall et al., 2013). Further, the length of time it took participants to finish the treatment program was as expected and similar across groups, approximately 3 months and 1–2 weeks. On average, TSB telephone contacts, which were conducted solely with parents, took approximately 30 minutes less than corresponding face-to-face sessions.
On the anxiety symptom measures, clinically meaningful reductions were found, with participants demonstrating mean levels of anxiety and overall functioning that moved from a clinical to a normative level by the end of treatment based on both parent and child report. In the current study, mean total scores on the SCARED at post-treatment were 10.11–10.23 for the FF condition and 14.70–16.33 for the TSB condition, all far below the cutoff for caseness (cutoff = 25) (Birmaher et al., 1999). On the CGAS, good functioning is identified by scores greater than 70, “no more than slight impairment in functioning”. On average, children in both conditions had post-treatment mean scores that were greater than 77.
Response rates in this study are consistent with those from large-scale efficacy trials, using more traditional formats and settings (e.g., face to face and academic settings), where improvement rates range from 60–85% and the average remission rate is 56% (Cartwright-Hatton, Roberts, Chitsabesan, Fothergill, & Harrington, 2004; Ginsburg et al., 2011). The majority participants in both groups (62.5–75%) were “much” or “very much” improved and free of their primary anxiety disorder by the end of the 10-session treatment. In the current study, remission rates for “all anxiety disorders” (i.e., anxiety free) were 54.2% and 75% for the TSB and FF groups respectively at post-treatment, and 58.2% and 62.5% at 3-month follow-up. Overall, these “anxiety free” remission rates are mostly consistent and in some instances more favorable than previous studies with primary care patients, which have found “anxiety free” remission rates of approximately 35% at post-treatment and 55% at 6 month follow-up (Creswell et al., 2010; Thirlwall et al., 2013). However remission rates are lower than studies of TSB from other settings (e.g., specialty clinics) where 69–79% of children were without any anxiety disorder diagnosis at post-treatment (Leong et al., 2009; Lyneham & Rapee, 2006). Also, response rates for some of the CGI and ADIS outcomes are somewhat attenuated by 3-month follow-up, underscoring the need for longer term assessments.
Based on previous research, it is possible that factors such as parent’s own psychopathology, parenting stress, and difficulty with child compliance may have lessened treatment response in the current sample (Cobham, Dadds, & Spence, 1998; Kazdin, 1995). Also, it may be that treatment gains in the TSB group could not completely emerge until parents had more time to comprehend the materials and practice the skills with their children. In a previous study of telephone based CBT in primary care, significant improvement for the anxious children did not emerge until longer-term follow-up (McGrath et al., 2011). Lastly, additional efforts may be required to improve the delivery and implementation of TSB with primary care samples.
Limitations
This study is limited by its small sample size. As such the repeated measures analyses were underpowered and should be interpreted with caution. Similarly as a feasibility study it did not include a control group or follow-up periods that extended beyond 3 months. From a cultural perspective, this study only reached an educated and predominantly Caucasian sample. One key issue was that the program was only available in English and thus not accessible to many families who were primarily Spanish speaking. It is still not known how well such an intervention would work with individuals who are ethnic minorities, non-English speaking, or from lower SES backgrounds. Further, the focus on anxiety and the use of mental health specialists limits the transportability of the intervention protocol to a generalist pediatric setting. Important to note, the Cool Kids program includes treatment modules that are relevant to children with varying comorbid disorders and were applied accordingly in this study. Additional efforts to develop and implement modular and transdiagnostic approaches for children with multiple psychiatric conditions in primary care, using varying modes of service delivery are warranted.
Conclusions
Data from this study further inform stepped models of mental health care, which call for initial minimal contact methods followed by more intensive approaches. Indeed, while the therapist supported bibliotherapy approach may not offer the same intensity of gains as face-to-face treatment, it comes with favorable satisfaction and engagement related outcomes, as well as notable clinical improvement. From a public health perspective the therapist-supported bibliotherapy approach may be favored given its potential to address barriers such as travel, time, childcare, convenience, and stigma. From a financial perspective, it may also be more affordable, given that it does not require separate office space, travel to appointments, and clinic staff to greet patients. The ability to provide families and children with feasible options to receive evidence-based interventions may lessen existing mental health disparities. While this study was not designed to address issues of equivalence, findings are promising and suggest that large-scale efforts aimed at examining the comparative effectiveness of therapist-supported bibliotherapy as well as other minimal contact interventions for children with anxiety are warranted.
Supplementary Material
Highlights.
The delivery of CBT for children with anxiety disorders in the primary care setting is feasible using therapist supported bibliotherapy or face to face modalities
Satisfaction, engagement, and remission outcomes are favorable for both therapist-supported bibliotherapy and face-to-face CBT delivered in primary care
Therapist supported bibliotherapy has the potential to address numerous service use barriers and reduce mental health disparities
Comparative effectiveness studies using larger sample sizes and equivalence designs are necessary
Acknowledgments
This study was supported by National Institute of Mental Health grants to DAC (K01MH072952), MBS (K24MH64122) and AD (K01MH093477). We would like to thank our clinic champions (Drs. Gollub, Johnson, and Kafka), primary care clinic staff, child anxiety specialists, independent evaluators, and research staff for their contributions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Asarnow JR, Jaycox LH, Anderson M. Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11(3):477–497. viii. doi: 10.1016/s1056-4993(02)00006-8. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. S0890–8567(09)63237–8 [pii] [DOI] [PubMed] [Google Scholar]
- Busch B, Biederman J, Cohen LG, Sayer JM, Monuteaux MC, Mick E, Faraone SV. Correlates of ADHD Among Children in Pediatric and Psychiatric Clinics. Psychiatr Serv. 2002;53(9):1103–1111. doi: 10.1176/appi.ps.53.9.1103. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, Roberts C, Chitsabesan P, Fothergill C, Harrington R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. Br J Clin Psychol. 2004;43(Pt 4):421–436. doi: 10.1348/0144665042388928. [DOI] [PubMed] [Google Scholar]
- Chavira DA, Stein MB, Bailey K, Stein MT. Child anxiety in primary care: prevalent but untreated. Depress Anxiety. 2004;20(4):155–164. doi: 10.1002/da.20039. [DOI] [PubMed] [Google Scholar]
- Cobham VE. Do anxiety-disordered children need to come into the clinic for efficacious treatment? J Consult Clin Psychol. 2012;80(3):465–476. doi: 10.1037/a0028205. [DOI] [PubMed] [Google Scholar]
- Cobham VE, Dadds MR, Spence SH. The role of parental anxiety in the treatment of childhood anxiety. J Consult Clin Psychol. 1998;66(6):893–905. doi: 10.1037//0022-006x.66.6.893. [DOI] [PubMed] [Google Scholar]
- Creswell C, Hentges F, Parkinson M, Sheffield P, Willetts L, Cooper P. Feasibility of guided cognitive behaviour therapy (CBT) self-help for childhood anxiety disorders in primary care. Ment Health Fam Med. 2010;7(1):49–57. [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM, March J. Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. J Consult Clin Psychol. 2011;79(6):806–813. doi: 10.1037/a0025933. 2011–27142–002 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy W. ECDEU Assessment Manual for Psychopharmacology, Revised. Bethesda, MD: United States Department of Health, Education and Welfare; 1976. [Google Scholar]
- Kazdin AE. Child, parent and family dysfunction as predictors of outcome in cognitive-behavioral treatment of antisocial children. Behav Res Ther. 1995;33(3):271–281. doi: 10.1016/0005-7967(94)00053-m. 0005–7967(94)00053-M [pii] [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M, Breton S. Barriers to Treatment Participation Scale: evaluation and validation in the context of child outpatient treatment. J Child Psychol Psychiatry. 1997;38(8):1051–1062. doi: 10.1111/j.1469-7610.1997.tb01621.x. [DOI] [PubMed] [Google Scholar]
- Kolko DJ, Campo JV, Kelleher K, Cheng Y. Improving access to care and clinical outcome for pediatric behavioral problems: a randomized trial of a nurse-administered intervention in primary care. J Dev Behav Pediatr. 2010;31(5):393–404. doi: 10.1097/DBP.0b013e3181dff307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong J, Cobham VE, de Groot J, McDermott B. Comparing different modes of delivery: a pilot evaluation of a family-focused, cognitive-behavioral intervention for anxiety-disordered children. Eur Child Adolesc Psychiatry. 2009;18(4):231–239. doi: 10.1007/s00787-008-0723-7. [DOI] [PubMed] [Google Scholar]
- Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behav Res Ther. 2006;44(9):1287–1300. doi: 10.1016/j.brat.2005.09.009. S0005–7967(05)00209–3 [pii] [DOI] [PubMed] [Google Scholar]
- March J. Consumer Satisfaction Scale (unpublished measure) Durham, NC: Duke University; 1999. [Google Scholar]
- McGrath PJ, Lingley-Pottie P, Thurston C, MacLean C, Cunningham C, Waschbusch DA, Chaplin W. Telephone-based mental health interventions for child disruptive behavior or anxiety disorders: randomized trials and overall analysis. J Am Acad Child Adolesc Psychiatry. 2011;50(11):1162–1172. doi: 10.1016/j.jaac.2011.07.013. S0890–8567(11)00643–5 [pii] [DOI] [PubMed] [Google Scholar]
- Rapee R, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: A randomized controlled trial. J Consult Clin Psychol. 2006;74(3):436–444. doi: 10.1037/0022-006X.74.3.436. 2006–08433–004 [pii] [DOI] [PubMed] [Google Scholar]
- Rapee R, Wignall A, Spence SH, Cobham VE, Lyneham HJ. Helping Your Anxious Child. 2. Oakland: New Harbinger Publications, Inc; 2008. [Google Scholar]
- Regier DA, Goldberg ID, Taube CA. The de facto US mental health services system: a public health perspective. Arch Gen Psychiatry. 1978;35(6):685–693. doi: 10.1001/archpsyc.1978.01770300027002. [DOI] [PubMed] [Google Scholar]
- Reiff MI, Stein MT. Attention-deficit/hyperactivity disorder evaluation and diagnosis: a practical approach in office practice. Pediatr Clin North Am. 2003;50(5):1019–1048. doi: 10.1016/s0031-3955(03)00077-4. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MSJB, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A children’s global assessment scale (cgas) Arch Gen Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. San Antonio, TX: Physiological Corporation; 1996. [Google Scholar]
- Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, Creswell C. Treatment of child anxiety disorders via guided parent-delivered cognitive-behavioural therapy: randomised controlled trial. Br J Psychiatry. 2013;203(6):436–444. doi: 10.1192/bjp.bp.113.126698. [DOI] [PubMed] [Google Scholar]
- Warner CM, Colognori D, Kim RE, Reigada LC, Klein RG, Browner-Elhanan KJ, Benkov K. Cognitive-behavioral treatment of persistent functional somatic complaints and pediatric anxiety: an initial controlled trial. Depress Anxiety. 2011;28(7):551–559. doi: 10.1002/da.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing VR, Walker PN. Review: cognitive behavioural therapy for adolescents with depression. Evid Based Ment Health. 2008;11(3):76. doi: 10.1136/ebmh.11.3.76. 11/3/76 [pii] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.