Abstract
Objective.
Despite theoretical advances in our conceptualization of disability, the “environment” remains a largely unspecified term in disablement models. The purpose of this research is to draw upon on a unique state-of-the-art nationally representative data set with innovative measures that provide the opportunity to tease apart and specify the role of different environmental factors in the disablement process.
Method.
Using multinomial logistic regression with data from the first round of the recently launched National Health and Aging Trends Study (N = 6,578 community-dwelling Americans age 65+), this paper examines the role of the built environment (e.g., stairs or ramps leading up to the home) and mobility devices on reported difficulty going outside by oneself.
Results.
Almost three quarters of community-dwelling older Americans live in a residence that has stairs at the entrance. Older adults who use a walker to help them get around are adversely affected by stairs at the entrance to their home, effectively doubling the odds of reporting difficulty going outside independently. Roughly 10% of community-dwelling older Americans live in a residence with a ramp at the entryway, which reduces the odds of outdoor mobility difficulty threefold among those using wheeled mobility devices. However, ramps at the entryway are associated with a higher likelihood of reporting difficulty going outdoors among those who do not use any type of mobility device.
Discussion.
A better understanding of the complexities of the environment in the disablement process is critical for the planning and development of age-friendly environments allowing older adults to age in place.
Key Words: Assistive technology, Built environment, Mobility disability
Since the Institute of Medicine’s milestone report on Disability in America (Pope & Tarlov, 1991), disablement models have conceptualized disability as a process, with the aim of better understanding how to prevent potentially disabling conditions from developing into disabilities. (Nagi, 1965; Verbrugge & Jette, 1994; World Health Organization, 2001) For example, the WHO’s International Classification of Functioning Disability and Health (known as the ICF [World Health Organization, 2001]) conceptualizes disability as an umbrella term that captures the consequences of disease at three levels (Figure 1): (a) at the level of the body, impairments in body functions and structures; (b) at the level of the person, restrictions in everyday activities; and (c) at the level of society, participation in life situations and social roles (Jette & Badley, 2000).
Figure 1.
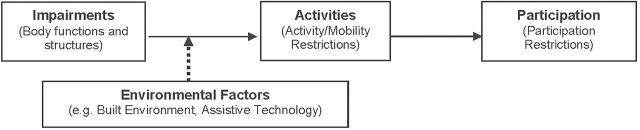
Conceptual model: the dynamic nature of disability (adapted from WHO 2001).
There is also recognition of the dynamic and contingent nature of the disablement process. Current models of disability (Verbrugge & Jette, 1994; World Health Organization, 2001) have drawn attention to environmental factors that can interact with underlying impairments to impede or enhance a person’s ability to carry out activities (dashed arrow in Figure 1). There are multiple types of environmental factors that can either serve as barriers or facilitators to independence for people with underlying health conditions (Srinivasan, O’Fallon, & Dearry, 2003). The ICF identifies products and technology (e.g., mobility devices), services and policies, attitudes, supports and relationships, as well as natural and human-made built environments (World Health Organization, 2001). For example, following a stroke an individual may experience hemiparesis (impairments in body functions and structures) that leads to severe difficulty in walking a quarter mile (mobility restriction), which then restricts his or her involvement in life situations, such as meeting with neighbors or close friends (participation restriction). But living on a street with continuous, barrier-free sidewalks may facilitate outdoor mobility, with positive consequences for his/her ability to visit with friends down the street (participation).
Motivated in part by these conceptual models, researchers have begun to examine the role of the environment in the disablement process by focusing on the modifying effect of the urban-built environment in the pathway between impairments and outdoor mobility (Clarke & George, 2005; Michael, Beard, Choi, Farquhar, & Carlson, 2006; Clarke, Ailshire, Bader, Morenoff, & House, 2008; Freedman, Grafova, Schoeni, & Rogowski, 2008; Clarke, Ailshire, & Lantz, 2009; Clarke, Ailshire, Nieuwenhuijsen, & de Kleijn-de Vrankrijker, 2011). Results indicate that uneven sidewalks and sidewalk obstacles (i.e., loose stones and other debris) are responsible for the vast majority of outdoor falls among older adults (Berg, Alessio Mills, & Tong, 1997; Li et al., 2006) and poor street and sidewalk conditions are associated with fourfold higher odds of mobility difficulty among older adults with underlying lower extremity weakness (Clarke et al., 2008). Moreover, compared with functionally independent older adults, older adults with lower extremity impairment avoid grassy terrain or terrain with other obstacles (Shumway-Cook et al., 2002, 2003). These findings highlight the importance of considering not only an individual’s physical capacity but also the demands created by the environment (person–environment fit), as they jointly influence independent mobility (Lawton, 1985; Balfour & Kaplan, 2002; Iwarsson, Horstmann, Carlsson, Oswald, & Wahl, 2009).
Yet, despite theoretical advances in our conceptualization of disability, the “environment” remains a largely unspecified term in disablement models. With respect to mobility disability, we do not know which particular environmental features matter most and for whom. Do environmental factors matter more for people with lower levels of functional capacity (impairment in ICF terms), and less so for people without any impairments? Mobility devices (e.g., cane, walker, wheelchair) also fall under the rubric of “environmental factors” in conceptual models. Yet we know very little about which ones are the most important facilitators for mobility and how they interact with other built environment features. For example, people who use wheeled mobility devices rely heavily on ramps and curb cuts for outdoor mobility. But for someone using a cane, curb cuts may not be as important. In addition, research to date has not differentiated between older adults residing in single family homes and multi-unit apartment buildings. Are outdoor built environment features less important for those in multi-unit dwellings where factors located inside the building are more likely to influence the level of difficulty going outside? Finally, for how many people does the environment play a role in mobility? To date, a lack of nationally representative data on these concepts has prevented us from quantifying the potential impact of particular environmental features on mobility in older Americans.
The purpose of this research is to draw on data from the first round of the National Health and Aging Trends Study (NHATS) to tease apart and specify the complex role of the environment in the disablement process (Freedman et al., 2011). Funded by the National Institute on Aging, NHATS is an annual, nationally representative study of Americans age 65 and older, with the first wave conducted in 2011. NHATS provides a unique opportunity to disentangle the role of individual and environmental factors in the disablement process due to a rigorous disability measurement protocol that seeks to disaggregate measures of activity limitations into impairments (using performance-based assessments of physical capacity), compensatory strategies, and environmental factors. For example, rather than simply asking respondents about difficulty with outdoor mobility, NHATS first asks how often they use a cane, walker, wheelchair, or scooter for outdoor mobility. Then, respondents are specifically asked how much difficulty they have with outdoor mobility when using that particular device. In addition, NHATS also collects standardized data on each respondent’s home and outdoor environment using interviewer observations. Thus, the NHATS framework provides a unique opportunity to distinguish between the role of assistive devices (accommodations) and the environment in outdoor mobility disability.
Method
Data
NHATS follows a nationally representative sample of 8,245 Medicare beneficiaries age 65 and older through annual in-person interviews. The study design and procedures have been described in detail elsewhere, (Freedman et al., 2011; Montaquila et al., 2012) but, briefly, a stratified random sample of adults age 65+ in the Medicare enrollment database, living in the coterminous United States, was selected for the first round of data collection in 2011 (71% response rate). African Americans and adults in the oldest age groups were oversampled. In-person interviews were used to collect detailed information on activities of daily life, living arrangements, economic status, the social and physical environment, as well as performance-based measures of physical capacity. Data from Round 1 were publicly released in May 2012, and the analyses for this paper focus on 7,609 community-dwelling respondents, excluding those residing in nursing homes.
Individual Measures
The primary outcome of interest, difficulty with outdoor mobility, was assessed in NHATS using the reference point of the past month, and focused on the ability to go outside by oneself, with whatever aids or devices the respondent typically used. For example, the exact question wording for someone who uses a cane to go outside was, “In the last month, when you used your cane, how much difficulty did you have leaving your home/building to go outside by yourself?”. Response options were “none,” “a little,” “some,” “a lot.” NHATS respondents who reported that they were not able to go outside by themselves were coded as having “a lot” of difficulty going outside.
Functional capacity (body functions and structures in ICF terminology [World Health Organization, 2001]) was objectively measured using the short physical performance battery (SPPB) (Vasunilashorn et al., 2009), a brief (<10min), reliable, performance battery of lower extremity function that is predictive of mobility, disability, institutionalization, and mortality (Guralnik et al., 1994). The SPPB includes three tests: gait speed over a 3-m course, standing balance, and time to rise from a chair five times. Each performance test is assigned a score ranging from 0 to 4 (where 4 captures high performance) (Gill, 2010). Scores from the three tests were summed into a composite score ranging 0–12, with higher scores reflecting better physical function. We also include a measure of comorbidity based on the number of medically diagnosed chronic health problems (including heart disease, hypertension, cancer, lung disease, osteoporosis, arthritis, diabetes, stroke), summed to create an index of chronic health problems ranging from 0 to 8.
Other covariates capture personal factors or resources likely to be important in the disablement process (Verbrugge & Jette, 1994; World Health Organization, 2001), including age (in years), gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other race/ethnicity [including Asians]), marital status (married, separated/divorced, widowed, never married), and highest level of attained education (less than high school degree, high school diploma [but less than college degree], and college degree or higher).
Environmental Measures
Information on the use of mobility devices was gathered by asking respondents if, in the past month, they used a cane, walker, wheelchair, or scooter to get around more easily, safely, or on their own (including whether they had these devices with them where they lived). Data on the immediate built environment were collected using interviewer observations, capitalizing on the in-person interview at the respondent’s home. Interviewers were asked, “When standing in front of the respondent’s home/building, and looking around in every direction, how much of the following did you see?” A question asked about “uneven walking surfaces or broken steps in the area leading up to the home/building” and answers are recorded dichotomously (yes/no). Additional data was gathered on the physical structure of the residence (e.g., detached single-family dwelling, multi-unit building), the presence of stairs or steps at the entrance, and whether there was a ramp.
Interviewers were also asked about indicators of social disorder in the immediate vicinity of the respondent’s home, including litter or broken glass on sidewalks and streets, graffiti on buildings and walls, and vacant or deserted houses or storefronts. Interviewers documented the presence of such features on a four-point scale (none, a little, some, a lot). An overall index of social disorder was created by averaging scores across all items (alpha reliability = 0.76), and included as an environmental control in the analyses to account for other social factors in the surrounding environment which could deter people from going outside (Cagney et al., 2009). We also account for length of time at current residence (in years) in order to control for the level of familiarity with one’s immediate environment.
Statistical Analysis
Based on the conceptual model in Figure 1, we first examine the relationship between physical capacity and level of difficulty with outdoor mobility, controlling for sociodemographic characteristics and comorbid health status. Models examine the effects of different environmental features on mobility difficulty, identifying which environmental features (e.g., unbroken steps, ramps at entryways, quality walkways) are most important for mobility controlling for individual covariates, neighborhood social disorder, and length of residence in a particular environment. Subsequent models incorporate statistical interactions between individual capacity and environmental features in order to identify which environments are most salient for those with more impaired physical function.
Because the key dependent variable, difficulty with outdoor mobility, is captured using multiple response options, multinomial logistic regression is used to contrast those reporting “a little” and “some/a lot” of difficulty going outside with those who report no difficulty. Due to missing data on the SPPB (N = 1,031 missing due to factors such as insufficient space, no chair for chair stands, or proxy interview), analyses are restricted to 6,578 community-dwelling respondents with complete data on the SPPB performance testing. All models are estimated in SAS version 9.2 and statistical significance is assessed with a two-tailed p value of .05. Data are weighted to take account of different rates of selection into the NHATS study and adjust for potential bias related to unit nonresponse.
Results
Descriptive statistics for the study sample are presented in Table 1. Roughly half of these community-dwelling respondents were between the ages of 65 and 74 at the first round of data collection, and half are female. The majority are white, married, with a high school diploma. The mean SPPB score was 6.7 on a scale from 0 to 12 (with a high score indicating more physical capacity). Respondents have on average about 2 comorbid health conditions. The vast majority of respondents do not use any mobility device when going outdoors, but almost 15% use some kind of device (most often cane or walker) on a regular basis (every time or most times) when going outside. Even when using these devices almost 20% reported some difficulty going outside on their own.
Table 1.
Descriptive Statistics for Community-Dwelling Sample, N = 6,578, National Health and Aging Trends Study (2011)
| Weighted percent or mean (SD) | |
|---|---|
| Age | |
| Age 65–74 | 52.9 |
| Age 74–84 | 33.7 |
| Age 85+ | 13.4 |
| Gender | |
| Female | 56.6 |
| Race/ethnicity | |
| White | 80.5 |
| Non-Hispanic black | 8.1 |
| Hispanic | 6.7 |
| Other race/ethnicity | 4.6 |
| Education | |
| Less than high school | 21.5 |
| High school diploma | 53.2 |
| College degree | 24.1 |
| Marital status | |
| Married | 57.0 |
| Separated/divorce | 12.3 |
| Widowed | 27.1 |
| Never married | 3.7 |
| Health and functional capacity | |
| SPPB score (range 0–12) | 6.7 (3.5) |
| Number of chronic health problems (range 0–8) | 2.3 (1.4) |
| Housing/residence | |
| House | 80.7 |
| Multi-unit structure | 13.5 |
| Other (including mobile home) | 5.8 |
| Length of time in current residence (range 0–96 years) | 21.6 (18.2) |
| Neighborhood disorder (range 1–4) | 1.07 (0.29) |
| Use of mobility devices | |
| None | 86.2 |
| Cane | 6.7 |
| Walker | 4.9 |
| Wheelchair/scooter | 2.2 |
| Level of difficulty going outside (with device) | |
| None | 82.1 |
| A Little | 6.5 |
| Some | 3.4 |
| A Lot | 8.0 |
| Built environment | |
| Broken steps/walkway at entryway | 13.2 |
| Stairs at entryway | 74.9 |
| Ramp at entryway | 9.6 |
Note. SPPB = short physical performance battery.
Most of these community-dwelling respondents reside in single-unit houses, but about 13% live in multi-unit (e.g., apartment) complexes (for subsequent analyses single-unit homes and other housing structures are combined in contrast to multi-unit structures). They are generally long-term residents of their homes, residing at their current address for over 20 years. Indicators of neighborhood social disorder are relatively low (on a four-point scale). The vast majority (75%) have stairs at the entryway to their homes, whereas a small minority (around 10%) has a ramp at their entryway. Around 13% of these residences have uneven walking surfaces or broken steps leading to the home/building.
Tables 2 and 3 reports the results from the multinomial logistic regression analyses for the log odds of reporting a little difficulty going outside (Table 2) and some/a lot of difficulty going outside (Table 3). The tables present the logistic regression coefficients and odds ratios (ORs) for the independent variables as they relate to no difficulty going outside. As expected, physical capacity according to the SPPB is strongly inversely associated with reported difficulty going outside. For a one unit increase in physical capacity, the log odds of reporting a little difficulty going outside decrease by 0.27 (Model A, Table 2), for an adjusted OR of 0.76 (95% confidence interval [CI]: 0.73, 0.79). The log odds of reporting some or a lot of difficulty going outside (Model A, Table 3) decreases by 0.53 for each unit increase in physical capacity, for an adjusted OR of 0.58 (95% CI: 0.56, 0.61). Controlling for functional capacity, a greater number of chronic health problems is associated with greater difficulty going outside (OR = 1.24 for a little difficulty and OR = 1.34 for some/lot of difficulty, Tables 2 and 3, respectively).
Table 2.
Multinomial Logistic Regression Results for Reporting a Little Difficulty Going Outa, National Health and Aging Trends Study (2011) N = 6,578
| Model A | Model B | |||||
|---|---|---|---|---|---|---|
| Estimate | OR | 95% CI | Estimate | OR | 95% CI | |
| Intercept | −1.45*** | −1.47*** | ||||
| Sociodemographic characteristics | ||||||
| Male (ref) | ||||||
| Female | −0.06 | 0.94 | 0.75, 1.19 | −0.05 | 0.95 | 0.75, 1.20 |
| Age 65–74 (ref) | ||||||
| Age 74–84 | −0.21 | 0.81 | 0.63, 1.05 | −0.21 | 0.81 | 0.63, 1.05 |
| Age 85+ | −0.21 | 0.81 | 0.59, 1.12 | −0.21 | 0.81 | 0.59, 1.12 |
| White (ref) | ||||||
| Non-Hispanic black | −0.05 | 0.95 | 0.73, 1.24 | −0.05 | 0.95 | 0.73, 1.24 |
| Hispanic | 0.21 | 1.23 | 0.81, 1.89 | 0.21 | 1.23 | 0.80, 1.88 |
| Other race/ethnicity | 0.11 | 1.11 | 0.61, 2.05 | 0.11 | 1.11 | 0.61, 2.05 |
| College degree (ref) | ||||||
| Less than high school | 0.10 | 1.10 | 0.80, 1.52 | 0.11 | 1.11 | 0.81, 1.53 |
| High school diploma | −0.06 | 0.94 | 0.70, 1.25 | −0.05 | 0.95 | 0.71, 1.27 |
| Married (ref) | ||||||
| Separated/divorce | 0.10 | 1.10 | 0.77, 1.59 | 0.09 | 1.10 | 0.76, 1.58 |
| Widowed | 0.34** | 1.40 | 1.08, 1.82 | 0.33* | 1.40 | 1.08, 1.82 |
| Never married | 0.54* | 1.72 | 1.05, 2.82 | 0.52* | 1.68 | 1.03, 2.77 |
| Health and functional capacity | ||||||
| Physical capacity (SPPB) | −0.27*** | 0.76 | 0.73, 0.79 | −0.27*** | 0.76 | 0.73, 0.79 |
| Number of chronic health problems | 0.21*** | 1.24 | 1.15, 1.33 | 0.21*** | 1.24 | 1.15, 1.33 |
| Housing/residence | ||||||
| Single unit (ref) | ||||||
| Multi-unit structure | −0.17 | 0.84 | 0.61, 1.16 | −0.18 | 0.84 | 0.61, 1.15 |
| Length of time in current residence (decades) | 0.05 | 1.05 | 0.99, 1.11 | 0.05 | 1.05 | 0.099, 1.11 |
| Neighborhood disorder | −0.38 | 0.68 | 0.44, 1.04 | −0.38 | 0.68 | 0.44, 1.04 |
| Environmental factors | ||||||
| Uses no mobility device (ref) | ||||||
| Cane | 0.66*** | 1.93 | 1.45, 2.58 | 0.37 | 1.45 | 0.79, 2.61 |
| Walker | 0.46* | 1.58 | 1.06, 2.35 | 0.48 | 1.62 | 0.86, 3.03 |
| Wheelchair/scooter | 0.11 | 1.12 | 0.52, 2.39 | 0.90 | 2.46 | 0.79, 7.66 |
| Stairs at entryway | 0.11 | 1.12 | 0.86, 1.44 | 0.10 | 1.11 | 0.02, 1.48 |
| Ramp at entryway | 0.08 | 1.08 | 0.78, 1.50 | 0.16 | 1.17 | 0.79, 1.74 |
| Wheelchair × ramp at entryway | −0.70 | 0.50 | 0.11, 2.25 | |||
| Cane × ramp at entryway | −0.17 | 0.84 | 0.36, 2.00 | |||
| Walker × ramp at entryway | −0.11 | 0.90 | 0.37, 2.16 | |||
| Wheelchair × stairs at entryway | −1.81 | 0.16 | 0.02, 1.53 | |||
| Cane × stairs at entryway | 0.41 | 1.51 | 0.79, 2.88 | |||
| Walker × stairs at entryway | 0.04 | 1.04 | 0.48, 2.28 | |||
Notes. CI = confidence interval; OR = odds ratio; SPPB = short physical performance battery.
aReference is no difficulty going out.
*p < .05. **p < .01. ***p < .001 (two-tailed tests; bold font indicates significant effects).
Table 3.
Multinomial Logistic Regression Results for Reporting Some/Lot Difficulty Going Outa, National Health and Aging Trends Study (2011), N = 6578
| Model A | Model B | |||||
|---|---|---|---|---|---|---|
| Estimate | OR | 95% CI | Estimate | OR | 95% CI | |
| Intercept | −1.41*** | −1.24*** | ||||
| Sociodemographic characteristics | ||||||
| Male (ref) | ||||||
| Female | 0.56*** | 1.75 | 1.40, 2.18 | 0.56*** | 1.75 | 1.40, 2.18 |
| Age 65–74 (ref) | ||||||
| Age 74–84 | −0.04 | 0.96 | 0.75, 1.23 | −0.06 | 0.96 | 0.75, 1.23 |
| Age 85+ | 0.30* | 1.35 | 1.02, 1.78 | 0.29* | 1.35 | 1.02, 1.78 |
| White (ref) | ||||||
| Non-Hispanic black | 0.01 | 1.01 | 0.79, 1.27 | 0.01 | 1.01 | 0.79, 1.27 |
| Hispanic | 0.56*** | 1.75 | 1.23, 2.48 | 0.52** | 1.75 | 1.23, 2.48 |
| Other race/ethnicity | 0.48 | 1.62 | 0.98, 2.66 | 0.47 | 1.62 | 0.98, 2.66 |
| College degree (ref) | ||||||
| Less than high school | 0.30* | 1.34 | 1.01, 1.81 | 0.29 | 1.34 | 1.01, 1.81 |
| High school diploma | −0.03 | 0.97 | 0.73, 1.28 | −0.03 | 0.97 | 0.73, 1.28 |
| Married (ref) | ||||||
| Separated/divorce | −0.13 | 0.88 | 0.63, 1.22 | −0.14 | 0.88 | 0.63, 1.22 |
| Widowed | 0.03 | 1.01 | 0.80, 1.27 | 0.01 | 1.01 | 0.80, 1.27 |
| Never married | 0.07 | 1.72 | 0.67, 1.72 | 0.10 | 1.72 | 0.67, 1.72 |
| Health and functional capacity | ||||||
| Physical capacity (SPPB) | −0.53*** | 0.58 | 0.56, 0.61 | −0.53*** | 0.58 | 0.56, 0.61 |
| Number of chronic health problems | 0.30*** | 1.34 | 1.25, 1.43 | 0.29*** | 1.34 | 1.25, 1.43 |
| Housing/residence | ||||||
| Single unit (ref) | ||||||
| Multi-unit structure | −0.24 | 0.78 | 0.60, 1.02 | −0.26 | 0.78 | 0.60, 1.02 |
| Length of time in current residence (decades) | −0.03 | 0.97 | 0.92, 1.02 | −0.03 | 0.97 | 0.92, 1.02 |
| Neighborhood disorder | −0.05 | 0.95 | 0.71, 1.29 | −0.03 | 0.95 | 0.71, 1.29 |
| Environmental factors | ||||||
| Uses no mobility device (ref) | ||||||
| Cane | 0.44*** | 1.55 | 1.21, 1.98 | 0.14 | 1.15 | 0.70, 1.88 |
| Walker | 0.97*** | 2.63 | 1.98, 3.51 | 0.65** | 1.92 | 1.20, 3.07 |
| Wheelchair/scooter | 1.43*** | 4.18 | 2.64, 6.63 | 1.68*** | 5.36 | 2.50, 11.52 |
| Stairs at entryway | 0.42*** | 1.52 | 1.21, 1.91 | 0.18 | 1.20 | 0.91, 1.56 |
| Ramp at entryway | 0.24 | 1.27 | 0.98, 1.66 | 0.41** | 1.51 | 1.08, 2.10 |
| Wheelchair × ramp at entryway | −1.00* | 0.37 | 0.15, 0.92 | |||
| Cane × ramp at entryway | 0.09 | 1.09 | 0.55, 2.17 | |||
| Walker × ramp at entryway | −0.41 | 0.66 | 0.35, 1.27 | |||
| Wheelchair × stairs at entryway | 0.42 | 1.51 | 0.61, 3.75 | |||
| Cane × stairs at entryway | 0.37 | 1.45 | 0.84, 2.51 | |||
| Walker × stairs at entryway | 0.69** | 1.99 | 1.12, 3.51 | |||
Notes. CI = confidence interval; OR = odds ratio; SPPB = short physical performance battery.
aReference is no difficulty going out.
*p < .05. **p < .01. ***p < .001 (two-tailed tests; bold font indicates significant effects).
Not surprisingly, older age is associated with some/lot of difficulty going outside, and women are more likely to report some/lot of difficulty than men (OR = 1.35, Model A Table 3). There are also differences in the odds of difficulty going outside by race/ethnicity, marital status, and education. Hispanics have a higher odds of reporting some/lot of difficulty compared with whites, all other things being equal (OR = 1.75, Model A, Table 3), while widowed and never married older adults are more likely to report a little difficulty going outside than married respondents (OR = 1.40 and 1.72, respectively, Model A, Table 2). Respondents with less than a high school diploma have an odds of reporting some/lot of difficulty going outside that is 30% higher than those with a college degree (OR = 1.34, Model A, Table 3), net of sociodemographic characteristics, health, and physical capacity.
With respect to environmental factors, stairs at the entryway to the home are associated with a 50% higher odds of reporting some/lot of difficulty going outside independently (OR = 1.52, Model A, Table 3). (There were no effects of broken steps or uneven walkways on mobility difficulty [nor in interaction with assistive technology] so these effects were excluded from Tables 2 and 3.) Older adults using assistive technology for mobility reported greater difficulty going outside on their own than those who do not use assistive technology, net of individual risk factors. But this represents an averaged effect across different built environments. Model B in Tables 2 and 3 adds the interaction terms to assess how the relationship between the use of mobility devices and mobility difficulty varies according to barriers at entryways. There were no significant interaction effects for the odds of reporting a little difficulty going outside (Table 2), but there were multiple modifying effects for the odds of reporting some or a lot of difficulty going outside by mobility devices and built environment features at the entry to the home (Table 3).
While the use of a wheeled mobility device was associated with a fivefold higher odds of some/a lot of difficulty going outside (OR = 5.36, Model B, Table 3), the effect was greatly attenuated when there was a ramp at the entrance to the home (OR = exp(1.68 − 1.00) = 1.97). Conversely, while use of a walker was associated with a twofold higher odds of reporting some/lot of difficulty going outside (OR = 1.92, Model B, Table 3), this effect was even greater for older adults with stairs at the entry to their home (OR = exp(0.65 + 0.69) = 3.82), effectively doubling the odds of reporting difficulty going outdoors on their own. Finally, among older adults who do not use any assistive technology to get around, ramps at the entry to their residence are associated with a 50% higher odds of reporting some/a lot of difficulty going out (OR = 1.51, Model B, Table 3) in comparison to those without ramps at the entryway. These interaction effects are plotted in Figure 2.
Figure 2.
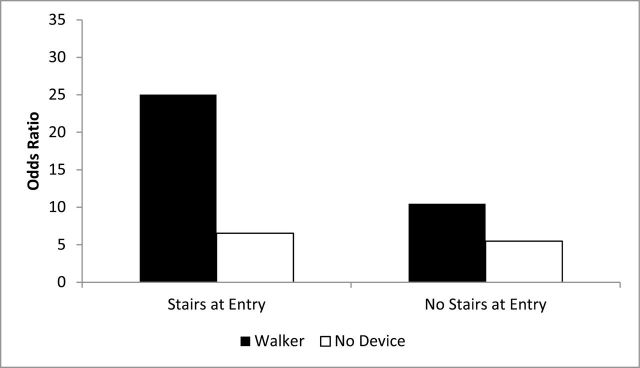
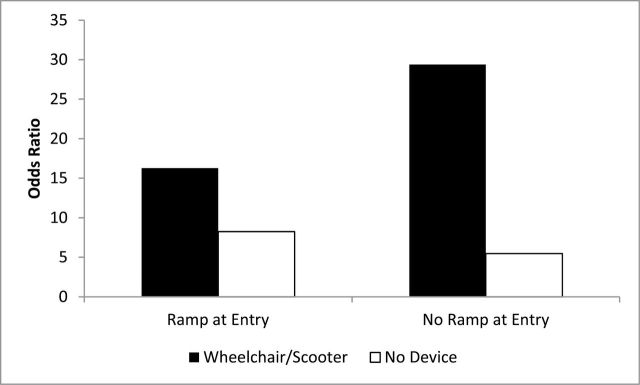
(a) Odds ratios of risk for some/lot outdoor mobility difficulty by use of walker and stairs at entry (National Health and Aging Trends Study: 2011). Note: Predicted values for the intercept are calculated for an African American female, age 85 years or more, with less than a high school education, widowed, living in a single unit house. (b) Odds ratios of risk for some/lot outdoor mobility difficulty by use of wheelchair/scooter and ramp at entry (National Health and Aging Trends Study: 2011). Note: Predicted values for the intercept are calculated for an African American female, age 85 years or more, with less than a high school education, widowed, living in a single unit house.
Discussion
The relationship between the environment and mobility disability is complex, incorporating interactions between individual capacity and environmental barriers and facilitators. We currently have very little understanding of the relative (or joint/interactive) contribution of the environment in creating difficulty for outdoor mobility (Alexander, 1996; Guralnik, 1993). To date, population level data have not been available to understand how particular environmental characteristics influence the degree to which limitations in physical functioning translate into actual disability in terms of locomotion outside of the home, and for whom. Direct observation of environmental factors in NHATS provides new insights into the role of environmental features for older adults’ ability to go out of their residence independently, as a basic first step in participating in activities outside the home. Going outside independently is a critical measure of outdoor mobility because it captures the ability to be mobile in the immediate vicinity outside the home, which is often the gateway to other activities (shopping, visiting with friends, getting to appointments, etc.).
Using direct independent observation of the built environment features at the entry to the home with a large, nationally representative sample of older Americans, we found that stairs are highly prevalent at the entryways to residential structures. Almost three quarters of community-dwelling older Americans live in a residence that has stairs at the entrance. This is in stark contrast to the model of a “zero-step” entryway that has been advocated and legislated for multi-unit dwellings under the Fair Housing Act Amendment of 1988 (Smith et al., 2012). A lack of access due to stairs can have adverse consequences for people with disabilities and their caregivers, including greater social isolation and elevated risk of injury (Smith et al., 2012). Almost one in five older Americans have at least some difficulty going out by themselves, and 15% use some kind of assistive device for mobility. Older adults who use a walker to help them get around are particularly affected by stairs at the entrance to their home, effectively doubling the odds of reporting difficulty going outside on their own.
Ramps are designed to increase accessibility for those who use wheeled mobility devices, and 15% of community-dwelling older Americans live in a residence with a ramp at the entryway. As intended, ramps have a significant impact in increasing mobility among those using wheelchairs or scooters, reducing the odds of outdoor mobility difficulty almost threefold. However, a rather surprising finding was that ramps at the entry to one’s residence are associated with a higher likelihood of reporting difficulty going outdoors independently among those who do not use any type of mobility device to get around. The unintended consequences of accessibility features for the unimpaired is noteworthy, and suggests better consideration of the design of accessibility features so that they facilitate mobility for all older adults across the full range of functioning. The findings in this paper beg for further research in understanding how older adults across a range of functioning and using a range of mobility devices move across different accessibility features in outdoor environments.
Contrary to expectations, we found no evidence of an interaction between individual capacity and built environment features for self-reported difficulty going outside. But the complexity of interactions between different types of assistive technology and the built environment, both of which are considered “environmental features” in disability models (Verbrugge & Jette, 1994; World Health Organization, 2001), points to a relatively unexplored interplay between different environmental features in the disablement process. These findings highlight the importance of disentangling the role of different environmental factors by distinguishing between products and technology for outdoor mobility and human-made changes to the physical built environment, including their joint interactive effects. Moreover, further attention should be paid to other “environmental factors” including social supports, attitudes, and services, as well as their complex interactions with the physical and natural environment. These results suggest that being married and having higher levels of education are facilitators for independent mobility. Future work should also consider broader features of the built environment including population density, transportation, and the presence of destinations within walking distance.
Collectively, these results highlight the complexity of the role of the environment in the disablement process. The advanced disability measurement protocol in NHATS, which distinguishes between individual compensatory strategies and independently observed environmental factors, permits a more nuanced and comprehensive understanding of the way that built environment features and assistive devices interact to shape the mobility of older Americans in day-to-day life. A better understanding of these dynamics is critical for the planning and development of “age-friendly” communities allowing older adults to “age in place.”
Funding
Funding was provided by the National Institute on Aging through U01-AG032947, P30-AG012846, and R03-AG043661. The views expressed are those of the author alone and do not represent their employers or the funding agency.
Acknowledgment
An earlier version of this paper was presented at the NHATS Early Results Workshop and annual Disability TRENDS Network meeting, April 25–26, 2013, Ann Arbor, MI.
References
- Alexander N. B. (1996). Gait disorders in older adults. Journal of the American Geriatrics Society, 44, 434–451. [DOI] [PubMed] [Google Scholar]
- Balfour J. L., Kaplan G. A. (2002). Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. American Journal of Epidemiology, 155, 507–515. :10.1093/aje/155.6.507 [DOI] [PubMed] [Google Scholar]
- Berg W. P., Alessio H. M., Mills E. M., Tong C. (1997). Circumstances and consequences of falls in independent community-dwelling older adults. Age and Ageing, 26, 261–268. :10.1093/ageing/26.4.261 [DOI] [PubMed] [Google Scholar]
- Berg W. P., Berg(1997). Circumstances and consequences of falls in independent community-dwelling older adults. Age and Ageing, 26, 261–268. [DOI] [PubMed] [Google Scholar]
- Cagney K. A., Glass T. A., Skarupski K. A., Barnes L. L., Schwartz B. S., Mendes de Leon C. F. (2009). Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 64, 415–424. :10.1093/geronb/gbn041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., Ailshire J. A., Bader M., Morenoff J. D., House J. S. (2008). Mobility disability and the urban built environment. American Journal of Epidemiology, 168, 506–513. :10.1093/aje/kwn185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., Ailshire J. A., Lantz P. (2009). Urban built environments and trajectories of mobility disability: Findings from a national sample of community-dwelling American adults (1986-2001). Social Science & Medicine (1982), 69, 964–970. :10.1016/j.socscimed.2009.06.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., George L. K. (2005). The role of the built environment in the disablement process. American Journal of Public Health, 95, 1933–1939. :10.2105/AJPH.2004.054494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P. J., Ailshire J. A., Nieuwenhuijsen E. R., de Kleijn-de Vrankrijker M. W. (2011). Participation among adults with disability: The role of the urban environment. Social Science & Medicine (1982), 72, 1674–1684. :10.1016/j.socscimed.2011.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V. A., Grafova I. B., Schoeni R. F., Rogowski J. (2008). Neighborhoods and disability in later life. Social Science & Medicine (1982), 66, 2253–2267. :10.1016/j.socscimed.2008.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V. A., Kasper J. D., Cornman J. C., Agree E. M., Bandeen-Roche K., Mor V. … Wolf D. A. (2011). Validation of new measures of disability and functioning in the National Health and Aging Trends Study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 66, 1013–1021. :10.1093/gerona/glr087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T. M. (2010). Assessment of function and disability in longitudinal studies. Journal of the American Geriatrics Society, 58(Suppl. 2), S308–S312. :10.1111/j.1532-5415.2010.02914.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik J. M., LaCroix A. Z., Abbott R. D., Berkman L. F., Satterfield S., Evans D. A., Wallace R. B. (1993). Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. American Journal of Epidemiology, 137, 845–857. [DOI] [PubMed] [Google Scholar]
- Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G., … Wallace R. B. (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49, M85–M94. :10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Iwarsson S., Horstmann V., Carlsson G., Oswald F., Wahl H. W. (2009). Person–environment fit predicts falls in older adults better than the consideration of environmental hazards only. Clinical Rehabilitation, 23, 558–567. :10.1177/0269215508101740 [DOI] [PubMed] [Google Scholar]
- Jette A. M., Badley E. (2000). Conceptual issues in the measurement of work disability, Committee to Review the Social Security Administration’s Disability Decision Process Research, N. Mathiowetz and G. S. Wunderlich, Committee on National Statistics, National Research Council, National Academies Press. [Google Scholar]
- Lawton M. P. (1985). “The elderly in context: Perspectives from environmental psychology and gerontology “ Environment and Behavior, 17, 501–519. [Google Scholar]
- Li W., Keegan T. H., Sternfeld B., Sidney S., Quesenberry C. P., Jr, Kelsey J. L. (2006). Outdoor falls among middle-aged and older adults: a neglected public health problem. American Journal of Public Health, 96, 1192–1200. :10.2105/AJPH.2005.083055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Y., Beard T., Choi D., Farquhar S., Carlson N. (2006). Measuring the influence of built neighborhood environments on walking in older adults. Journal of Aging and Physical Activity, 14, 302–312. [DOI] [PubMed] [Google Scholar]
- Montaquila J., Freedman V. A., et al. (2012). National Health and Aging Trends Study Round 1 Sample Design and Selection. NHATS Technical Paper #1. Baltimore: Johns Hopkins University School of Public Health. [Google Scholar]
- Nagi S. Z. (1965). Some conceptual issues in disability and rehabilitation. In Sussman M. B. Sociology and rehabilitation (pp. 100–113). Washington, DC: American Sociological Association. [Google Scholar]
- Pope A. M., Tarlov A. R. (1991). Disability in America: toward a National Agenda for Prevention. Washington, DC: National Academy Press. [Google Scholar]
- Shumway-Cook A., Patla A., Stewart A., Ferrucci L., Ciol M. A., Guralnik J. M. (2003). Environmental components of mobility disability in community-living older persons. Journal of the American Geriatrics Society, 51, 393–398. :10.1046/j.1532-5415.2003.51114.x [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A., Patla A. E., Stewart A., Ferrucci L., Ciol M. A., Guralnik J. M. (2002). Environmental demands associated with community mobility in older adults with and without mobility disabilities. Physical Therapy, 82, 670–681. [PubMed] [Google Scholar]
- Smith S. K., Rayer S., Smith E., Wang Z., Zeng Y., et al. (2012). Population aging, disability and housing accessibility: Implications for sub-national areas in the United States. Housing Studies, 27, 252–266. [Google Scholar]
- Srinivasan S., O’Fallon L. R., Dearry A. (2003). Creating healthy communities, healthy homes, healthy people: Initiating a research agenda on the built environment and public health. American Journal of Public Health, 93, 1446–1450. :10.2105/AJPH.93.9.1446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasunilashorn S., Coppin A. K., Patel K. V., Lauretani F., Ferrucci L., Bandinelli S., Guralnik J. M. (2009). Use of the Short Physical Performance Battery Score to predict loss of ability to walk 400 meters: Analysis from the InCHIANTI study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64, 223–229. :10.1093/gerona/gln022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge L. M., Jette A. M. (1994). The disablement process. Social Science & Medicine (1982), 38, 1–14. :10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2001). International Classification of Functioning, Disability and Health. Geneva: Switzerland World Health Organization. [Google Scholar]


