Abstract
Objective.
The goals of this paper were: (a) to promote research using the National Social Life, Health and Aging Project (NSHAP) Wave 2 data by providing relevant background information for a broad range of chronic conditions and (b) to provide a framework for combining these chronic conditions into informative comorbidity indices.
Method.
The chronic conditions measured in NSHAP Wave 2 were grouped across several health domains: cardiovascular, endocrine and metabolic, cancer, lung, inflammatory and bone, neurological, and sensorimotor. Prevalences for each condition were reported as percentages and were also estimated separately by age group and gender. Additionally, 2 comorbidity indices were created: a Modified Charlson Comorbidity Index (CCI) that included conditions associated with mortality risk and the NSHAP Comorbidity Index (NCI) that included conditions from the Modified CCI as well as additional conditions related to overall health and function.
Results.
Hypertension, incontinence, arthritis, heart conditions, cancer, and diabetes were the most prevalent conditions. In general, prevalences of most chronic conditions increased with age. Additionally, there were several notable gender differences in chronic condition prevalence. Due to the inclusion of highly prevalent conditions, such as hypertension and incontinence, the mean comorbidity index score of the NCI was higher than that of the Modified CCI.
Discussion.
Wave 2 of NSHAP included a variety of measures assessing the chronic conditions that are the most prevalent in older adults. These data are a valuable resource for the study of the impact of chronic conditions on overall health and aging.
Key Words: Aging, Comorbidity, Disease, Multimorbidity.
A major strength of Wave 2 of the National Social Life, Health and Aging Project (NSHAP) is its coverage of a broad range of health conditions that represent diverse aspects of aging, such as social, psychological, and physical dimensions of health. Elsewhere in this special issue, many of these health dimensions, including frailty, pain, sleep, sensory function, mental health, and sexual health, are covered in detail (Galinsky, McClintock, & Waite, 2014; Huisingh-Sheetz et al., 2014; Kern, Wroblewski, Schumm, Pinto, & McClintock, 2014; Lauderdale et al., 2014; Payne, McClintock, & Dale, 2014; Pinto, Kern, Wroblewski, Schumm, & McClintock, 2014; Shega, Sunkara et al., 2014; Shega, Tiedt, Grant, & Dale, 2014). This paper details the chronic condition measures of Wave 2 of NSHAP that are the leading causes of morbidity and mortality in older Americans.
By 2030, it is projected that 1 in 5 Americans will be 65 years or older (Vincent & Velkoff, 2010). More than 80% of Americans older than 65 years have at least one chronic condition, with hypertension, arthritis, heart disease, cancer, and diabetes being the top 5 most frequently occurring conditions (He, Sengupta, Velkoff, & Dellaros, 2005). NSHAP assessed many of the most prevalent chronic conditions, which, according to the Centers for Disease Control (CDC), account for 7 of the 10 leading causes of mortality in individuals aged 65 years and older. These chronic conditions include heart disease (31.8% of deaths), cancer (21.6%), stroke (7.9%), chronic respiratory diseases (6.0%), Alzheimer’s disease (3.2%), diabetes (3.0%), and kidney disease (1.9%) (Gorina, Hoyert, Lentzner, & Goulding, 2005). Chronic conditions are often used in assessing comorbidity, defined as the concomitant presence of 2 or more diseases. Several comorbidity indices, which group multiple chronic conditions into a composite score, have been developed in prior research and are shown to be strongly associated with increased mortality (Charlson, Pompei, Ales, & MacKenzie, 1987; de Groot, Beckerman, Lankhorst, & Bouter, 2003). Such indices allow one to assess how the burden of multiple chronic conditions, or multimorbidity, influences overall health in older adults.
Given the broad coverage of chronic conditions in NSHAP and the relevance of comorbidity to many aspects of aging, we have 4 main objectives for this paper: (a) to provide relevant background information describing the type and significance of the chronic conditions measured in NSHAP Wave 2, (b) to describe how each chronic condition was measured and report overall and age- and gender-specific prevalences of each chronic condition in NSHAP Wave 2, (c) to compare chronic condition prevalences in NSHAP Wave 2 to those from both national reports and NSHAP Wave 1, and (d) to provide a literature-supported framework to combine NSHAP’s chronic condition data into comorbidity indices for application in future studies.
Method
An overview of the study design for Wave 2 of NSHAP can be found elsewhere in this special issue (Jaszczak et al., 2014; O’Muircheartaigh, English, & Pedlow, 2014). Briefly, NSHAP is a longitudinal, population-based survey study of the social, biological, emotional, and environmental factors that influence health and aging. Data collection for Wave 1 of NSHAP occurred during 2005–2006 and included 3,005 adults aged 57–85 years. Wave 2 was conducted from 2010 to 2011. The final sample for Wave 2 included 3,377 individuals representing 3 different types of respondents: (a) respondents from Wave 1, (b) spouses and partners of these Wave 1 respondents, and (c) respondents who were sampled in Wave 1 but did not participate (W1 non-interview respondents [NIRs]). Data were collected from each participant through: (a) a computer-assisted in-person interview (CAPI); (b) self-administered questionnaire (SAQ), either completed via CAPI or paper-and-pencil questionnaire; (c) a collection of multiple biomarkers; and 4) a leave behind questionnaire that participants completed on their own and returned by mail to the project. To note, no proxy reports were collected for the leave-behind questionnaire. Data are publically available (NSHAP Wave 1: Waite, Linda J., Edward O. Laumann, Wendy Levinson, Stacy Tessler Lindau, and Colm A. O’Muircheartaigh. National Social Life, Health, and Aging Project (NSHAP): Wave 1. ICPSR20541-v6. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2014-04-30. doi:10.3886/ICPSR20541.v6. NSHAP Wave 2: Waite, Linda J., Kathleen Cagney, William Dale, Elbert Huang, Edward O. Laumann, Martha K. McClintock, Colm A. O’Muircheartaigh, L. Phillip Schumm, and Benjamin Cornwell. National Social Life, Health, and Aging Project (NSHAP): Wave 2 and Partner Data Collection. ICPSR34921-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2014-04-29. doi:10.3886/ICPSR34921.v1.).
Chronic Condition Ascertainment
As noted above, one objective of this paper is to compare chronic condition prevalences in NSHAP Wave 2 with those in NSHAP Wave 1, as well as with prevalences from other national surveys. Information on chronic conditions was collected in Waves 1 and 2 by self-report during the in-person interview. In Wave 1, chronic conditions were assessed by asking each participant “Has a medical doctor told you have (had) [condition]?” (Williams, Pham-Kanter, & Leitsch, 2009). This was followed by a long list of conditions that was read to the respondent, with the interviewer checking off each item the respondent reported. To optimize assessment of chronic conditions in this sample, the presentation and wording of chronic conditions questions were modified from Wave 1 to Wave 2. In Wave 2, each chronic condition was assessed through separate questions to the participant, with some chronic condition questions including follow-up questions to further clarify the condition. Below, we detail the rationale and data collection methods for each Wave 2 chronic condition by category: cardiovascular, endocrine and metabolic, cancer, lung, inflammatory and bone, neurological, and sensorimotor.
Cardiovascular conditions.
Cardiovascular diseases (CVDs), including coronary artery disease, heart attack, and stroke, are the leading cause of death in the United States for both men and women (Gorina et al., 2005). As reported by the CDC (source: National Health Interview Survey or NHIS), the prevalence of heart disease CVD increases across adulthood, rising from 16.9% in 55- to 64-year olds to 25.6% in 65- to 74-year olds and to 36.0% in those older than 75–84 years (CDC, 2010). Elevated blood pressure, or hypertension, is a common risk factor for heart disease, affecting more than 60% of adults older than 65 years (NCHS, 2013). Wave 2 of NSHAP included several questions regarding the following chronic cardiovascular conditions: high blood pressure/hypertension, stroke/cerebrovascular accident (in the last 5 years), and any heart condition. Participants were asked “Has a doctor ever told you that you have [condition].” A “yes” response to the heart condition question triggered follow-up questions regarding the specific type of heart condition, including heart attack, congestive heart failure, and/or having had a procedure to treat coronary artery disease. It should be noted that the exact wording of each chronic condition question of this type differed slightly depending on respondent status. For spouses and partners and W1 NIRs, the question structure followed the wording already detailed above. However, for W1 respondents, the chronic conditions questions were preceded by a qualifying statement, “Since your last interview in [Month/Year]….”
Endocrine and metabolic conditions.
NSHAP measures the primary condition related to endocrine and metabolic pathways: diabetes. Diabetes is a complex disorder characterized by high levels of blood glucose and abnormal metabolism of essential nutrients, including carbohydrates, fats, and proteins due to impaired insulin production, secretion, and action (American Diabetes Association, 2013). Approximately 20% of individuals aged 65 years and older report having diabetes (CDC, 2010). Moreover, diabetes is one of the leading causes of mortality in this age group (Gorina et al., 2005). In NSHAP, respondents were asked “Has a doctor ever told you that you have diabetes or high blood sugar?” More detailed information about diabetes measurement in NSHAP, including assessment of glycosylated hemoglobin (Hemoglobin A1C) from blood spots, can be found elsewhere in this special issue (Gregg, O’Doherty, Schumm, McClintock, & Huang, 2014).
Cancer.
Cancer is a group of diseases characterized by uncontrolled cellular growth and spread of abnormal cells, which can be influenced by both biological and environmental factors (American Cancer Society, 2011). Over 20% of deaths in individuals aged 65 years and older are due to some type of cancer (Gorina et al., 2005). NSHAP includes several questions regarding cancer diagnoses. First, NSHAP asked questions regarding skin cancer, “Has a doctor ever told you had skin cancer?” A “yes” response to this question triggered a follow-up question on what type of skin cancer: melanoma, carcinoma, or other. Although melanoma skin cancer accounts for less than 5% of skin cancers, melanoma accounts for the majority of skin cancer–related deaths, and its prevalence and severity differs greatly by race and gender (American Cancer Society, 2011). NSHAP respondents were then asked the question “Has a doctor ever told you have cancer (other than skin cancer)?” Respondents were further asked about the number of cancers, their first cancer type, their most recent cancer type, and whether their first or most recent cancers had spread to other body parts/systems (i.e., metastasized).
Lung conditions.
Diseases of the airways, including emphysema, asthma, chronic bronchitis, and chronic obstructive pulmonary disease (COPD), are common in older adults and are typically characterized by airflow limitation and airway inflammation (Mannino, Homa, Akinbami, Ford, & Redd, 2002). Chronic lung disease is a rapidly increasing cause of mortality in the United States and is expected to rise to the third leading cause of death by 2020 (Chapman, Mannino, et al., 2006). In NSHAP, lung conditions were assessed by asking respondents “Has a doctor ever told you that you have emphysema, asthma, chronic bronchitis, or chronic obstructive pulmonary disease?”
Inflammatory and bone conditions.
Maintaining good bone and joint health can minimize risk of several poor outcomes. Inflammatory arthritis of various types are common conditions in the United States, leading to significant morbidity and disability in older adults (CDC, 2009). Chronic rheumatoid arthritis is associated with increased mortality risk, particularly in women (Mikuls et al., 2002). Osteoarthritis is a leading cause of pain and disability among older U.S. adults (Peat, McCarney, & Croft, 2001). In NSHAP, respondents were asked “Has a doctor ever told you that you have osteo or rheumatoid arthritis?” In response to a “yes” answer, respondents were then asked which type of arthritis that they have: osteo, rheumatoid, or both.
Osteoporosis is a condition characterized by loss of bone density, and women are 4 times more likely to develop it than men (He et al., 2005). Osteoporosis is also a major risk factor for hip fractures (He et al., 2005). Hip fracture is a leading cause of disability and is associated with increased mortality risk (Wolinsky, Fitzgerald, & Stump, 1997). Two additional chronic condition questions related to bone health were included in NSHAP, W2: “has a doctor ever told you that you have osteoporosis?” and “has a doctor ever told you that you have had a hip fracture?” More information on hip fracture and its relationship to overall frailty is detailed in elsewhere in this special issue (Huisingh-Sheetz et al., 2014).
Neurological conditions.
Dementia is a broad term for a group of conditions associated with declines in mental abilities, including deficits in memory, language, and judgment as well as behavioral and emotional impairments (Chapman, Williams, Strine, Anda, & Moore, 2006). Alzheimer’s disease is the most common form of dementia and is characterized by the progressive deterioration of memory and other mental abilities, eventually leading to the inability to carry out even basic activities of daily living (Chapman, Williams, et al., 2006; Hebert, Scherr, Bienias, Bennett, & Evans, 2003). Moreover, Alzheimer’s disease is one of the leading causes of mortality in adults aged 65 years and older (Gorina et al., 2005). Vascular dementia is the second most common type of dementia and typically is associated with one or more strokes (Chapman, Williams, et al., 2006). Individuals can have both conditions, called “mixed dementia.” NSHAP included 2 questions about dementia: “Has a doctor ever told you that you have Alzheimer’s disease?” A negative response prompted a follow-up question: “Has a doctor ever told you that you have dementia (including vascular dementia, mixed dementia, or Mild Cognitive Impairment)?” In addition to these questions, Wave 2 of NSHAP included a new multidomain measure of cognitive ability, termed the Chicago Cognitive Function Measure (CCFM), the development of which is detailed elsewhere in this special issue (Shega, Sunkara et al., 2014). Following Alzheimer’s disease, Parkinson’s disease is the second most common neurodegenerative disorder (de Lau & Breteler, 2006). The prevalence of Parkinson’s disease is 0.3%, with prevalence increasing with age (CDC, 2010). NSHAP included the question, “Has a doctor ever told you that you have Parkinson’s disease?”
Sensorimotor conditions.
Wave 2 of NSHAP contains extensive coverage of a wide range of sensorimotor functions and conditions; several are detailed elsewhere in this issue (Huisingh-Sheetz et al., 2014; Kern et al., 2014; Pinto et al., 2014). Incontinence, another sensorimotor function important to older adult health, is characterized by the inability to control evacuative functions, including bladder and bowel, and is a common problem among older adults, with physical, emotional, and social ramifications (Landefeld et al., 2008). There are gender differences in the prevalence of incontinence, with women reporting higher rates than men (Markland, Richter, Fwu, Eggers, & Kusek, 2011; Medicare Current Beneficiary Survey [MCBS], 2009). In both Waves 1 and 2, participants were asked about urine and stool incontinence. Due to the sensitive nature of these questions, for additional privacy, participants were given the option of providing either an electronic response using a computer or a paper response using a paper-and-pencil questionnaire. Participants were asked several questions about incontinence. First, they were asked, “In the past 12 months, have you had difficulty controlling your bladder, including leaking small amounts of urine, leaking when you cough or sneeze, or not being able to make it to the bathroom on time?” Second, participants were asked, “In the past 12 months, have you had other problems with urinating, such as incomplete emptying, a weak urinary stream, straining to begin urination, or difficulty in postponing urination?” Finally, participants were asked, “Now we would like to know if you have experienced stool incontinence. In the past 12 months, have you lost control of your bowels (stool incontinence or anal incontinence)?” Affirmative responses to any of the previous questions prompted a follow-up question about frequency. Frequency answer options included (a) every day, (b) a few times a week, (c) a few times a month, or (d) a few times a year.
Comorbidity Indices
We use 2 methods for combining the chronic conditions collected in NSHAP into relevant weighted comorbidity indices (Table 1): the Modified Charlson Comorbidity Index (CCI) and the NSHAP Comorbidity Index (NCI). The Modified CCI is based on the previously validated and widely used CCI (Charlson et al., 1987). Initially created for studies using medical records, the CCI has been subsequently modified and validated for survey/self-report data (Katz, Chang, Sangha, Fossel, & Bates, 1996). An important feature of the CCI is that it assigns weighted scores to conditions based on their relationship to mortality risk. Each condition receives a score of 1, 2, 3, or 6, with higher scores assigned to conditions associated with a higher mortality (such as metastatic cancer). Scores are then summed to produce an index score. NSHAP Wave 2 included 10 of the 19 conditions of the original Charlson, which were summed together to create the Modified CCI, which ranged from 0 to 16. We compared our Modified CCI to the full CCI using a separate sample from the Successful Aging and Frailty Evaluations (SAFE) Clinic at the University of Chicago. This sample includes 93 ethnically diverse, frail older adults who were administered a health questionnaire, including all CCI items, by physicians and trained research assistants. The full CCI and modified CCI were highly correlated (r = .89).
Table 1.
Weighting for Comorbidity Indices Used in NSHAP Wave 2
| Conditions | Modified Charlson Comorbidity Index | NSHAP Comorbidity Index |
|---|---|---|
| Cardiovascular conditions | ||
| Hypertension | 0 | 1 |
| Heart condition (any) | ||
| Heart attack/myocardial infarction | 1 | 1 |
| Congestive heart failure | 1 | 1 |
| Procedure for coronary artery disease | 1a | 1 |
| Stroke/cerebrovascular disease | 1 | 1 |
| Endocrine and metabolic conditions | ||
| Diabetes | 1 | 1 |
| Cancer | ||
| Skin cancer – melanoma | 0 | 1 |
| Cancer/lymphoma/leukemiab | 2 | 2 |
| Metastatic cancer | 6 | 6 |
| Lung conditions | ||
| COPD/asthma | 1 | 1 |
| Inflammatory and bone conditions | ||
| Arthritis (any) | ||
| Osteoarthritis | 0 | 1c |
| Rheumatoid arthritis | 1 | 1 |
| Osteoporosis | 0 | 1c |
| Hip fracture | 0 | 1c |
| Neurological conditions | ||
| Dementia (any) | ||
| Alzheimer’s | 1d | 1d |
| Other | 1d | 1d |
| Parkinson’s disease | 0 | 1 |
| Sensorimotor conditions | ||
| Incontinence (any) | ||
| Urinary | 0 | 1e |
| Stool | 0 | 1e |
| Other urinary problems | 0 | 1e |
| Total conditions | 10 conditions | 15 conditions |
| Possible points | 0–16 points | 0–21 points |
Notes. Modified Charlson Index utilizes the weights from the Charlson Comorbidity Index (Charlson et al., 1987), it does not include several conditions from the original index, such as: ulcer disease, hemiplegia, renal disease, diabetes with end organ damage, liver disease, or AIDS. COPD = chronic obstructive pulmonary disease; NSHAP = National Social Life, Health and Aging Project.
aProcedure for coronary artery disease is used instead of the peripheral vascular disease item.
bThese include all non-metastatic cancers other than skin cancers.
cRespondents get a single point if they any of the following: osteoarthritis, osteoporosis, or hip fracture.
dRespondents get a single point if they have Alzheimer’s dementia or another form of dementia.
eRespondents get a single point if they have urinary incontinence, stool incontinence, or other urinary problems.
Additionally, we created the broader NCI that incorporated an additional 5 conditions or classes of conditions, including hypertension, bone health (osteoarthritis, osteoporosis, hip fracture), skin cancer (melanoma), and incontinence. While the conditions included in the original CCI, as well as the Modified CCI, were chosen due to their association with increased mortality risk, the additional conditions included in the NCI were chosen due to their high prevalence in our sample and their implications for overall physical, psychological, and social function. Specifically, the conditions included have been associated with increased risk for other medical conditions (e.g., hypertension) and increased risk for disability (e.g., osteoporosis, Parkinson’s disease, incontinence). The NCI utilized the weights of the original CCI as described above (Table 1), with the newly included items receiving a weight of 1; scores ranged from 0 to 21.
Other conditions and physical health indicators.
NSHAP included the question “Are there any other medical diseases or conditions that are important to your health now, that we have not talked about?” to assess any other important health conditions that were not covered by the questions detailed above. Additionally, NSHAP included extensive measurement of biomeasures to better characterize physical health in our participants, including measures of anthropometrics, cardiovascular function, immune function, anemia, urinary tract function, social proteins, stress, reproductive steroids, and vaginal microbiology. Details of these biomeasures are discussed elsewhere in this special issue (Hoffman, McClintock, & You, 2014; Kozloski & McClintock, 2014; O’Doherty et al., 2014; Reyes, Galinsky, You, McClintock, & Hoffman, 2014).
Statistical Analysis
Prevalences for each chronic condition were calculated as percentages with standard errors for the total sample and for gender and age subgroups. Analysis was limited to the 3,196 individuals considered to be age-eligible in Wave 2 based on the criteria of being born between 1920 and 1947. To account for unequal probabilities of selection and nonresponse, the weights distributed with the dataset were used for all analyses, and design-based standard errors (taking account of the strata and clustering) were obtained using linearization. Analyses were conducted in Stata 12 and SAS 9.3.
Results
The unweighted mean age of the study sample was 72.4 years and 53% were women. For these analyses, participants were categorized into 3 age groups: 62–69 years, 70–79 years, and 80–90 years (a few respondents born in 1947 who were 61 at the time of the interview were included in the 62–69 group, and a few born in 1920 who were 91 were included in the 80–90 group). Table 2 reports the weighted prevalence of each chronic condition and comparisons of the prevalences of selected chronic conditions in NSHAP Wave 2 with those of similar conditions from other nationally representative studies, including the NHIS, MCBS, and the Aging, Demographics, and Memory Study (ADAMS) (CDC, 2010; MCBS, 2009; NCHS, 2013; Plassman et al., 2007). Hypertension (59.9%), incontinence (45.8%), arthritis (34.9%), any heart condition (29.9%), cancer (27.8%), and diabetes (22.1%) were the most prevalent conditions. This rank order matches the most prevalent conditions reported from the NHIS data, except for incontinence which was not included in the NHIS. For incontinence, urinary incontinence (42.3%) was more prevalent than stool incontinence (10.5%). Table 3 reports the frequency on incontinence and other urinary problems, with urinary incontinence more likely to occur daily (25.1%) than stool incontinence (6.0%).
Table 2.
Weighted Frequency of Conditions in the National Social Life Health and Aging Project (n = 3,196)
| Conditions | % (Weighted) | SE | % Other reports |
|---|---|---|---|
| Cardiovascular conditions | |||
| Hypertension | 59.9 | 1.3 | 61.6a |
| Heart condition (any) | 29.9 | 1.1 | 30.6a |
| Heart attack/myocardial infarction | 9.0 | 0.7 | — |
| Congestive heart failure | 4.7 | 0.4 | — |
| Procedure for coronary artery disease | 12.5 | 1.0 | — |
| Stroke/cerebrovascular disease | 10.1 | 0.7 | 8.5a |
| Endocrine and metabolic conditions | |||
| Diabetes | 22.1 | 1.2 | 20.5a |
| Cancer | |||
| Cancer (all types) | 27.8 | 1.3 | 21.6a |
| Skin cancer – melanoma | 3.5 | 0.6 | 8.3a |
| Cancer/lymphoma/leukemiab | 14.9 | 1 | — |
| Metastatic cancer | 1.4 | 0.4 | — |
| Lung conditions | |||
| COPD/asthma | 15.7 | 0.8 | 14.1a |
| Inflammatory and bone conditions | |||
| Arthritis (any) | 34.9 | 1.3 | 50.9a |
| Osteoarthritis | 20.3 | 0.9 | — |
| Rheumatoid arthritis | 8.4 | 0.6 | — |
| Osteoporosis | 15.6 | 0.8 | 22.9c,d |
| Hip fracture | 2.7 | 0.4 | |
| Neurological conditions | |||
| Dementia (any) | 2.1 | 0.5 | 13.9e |
| Alzheimer’s | 0.6 | 0.1 | 9.7e |
| Other | 1.4 | 0.5 | — |
| Parkinson’s disease | 0.9 | 0.2 | 1.6c |
| Sensorimotor conditions | |||
| Incontinence (any) | 45.8 | 1.4 | — |
| Urinary | 42.3 | 1.3 | 29.8c |
| Stool | 10.5 | 0.5 | — |
| Other urinary problems | 25.7 | 1.0 | — |
Notes. COPD = chronic obstructive pulmonary disease.
aNational Health Interview Survey (NHIS; CDC, 2010; NCHS, 2013).
bNonmetastatic cancers not including skin cancers.
cMedicare Current Beneficiary Survey (MCBS, 2009).
dPrevalence includes both osteoporosis and hip fracture.
eThe Aging, Demographics, and Memory Study (ADAMS; Plassman et al., 2007).
Table 3.
Frequency of Incontinence and Other Urinary Problems (reported as percentages, %)
| Urinary incontinence (N = 1,233) | Stool incontinence (N = 343) | Other urinary problems (N = 742) | |
|---|---|---|---|
| A few times a year | 21.1 | 59.4 | 13.5 |
| A few times a month | 25.1 | 22.4 | 23.3 |
| A few times a week | 28.6 | 12.1 | 29.4 |
| Every day | 25.1 | 6.0 | 33.8 |
Table 4 (Wave 2) shows condition prevalence by age and gender subgroups for the most prevalent conditions in NSHAP Wave 2, as well as the conditions that are part of the top 10 leading causes of mortality. Of note, the prevalence for many conditions increased with age. In general, these increases were greatest between the 62–69 and 70–79 age groups. However, for several chronic conditions, the prevalence either did not change or only had a slight change across age groups, particularly between the 70–79 and 80–90 age groups. For example, between the 70–79 and 80–90 age groups, cancer prevalence increased by only 1.4% in women and decreased by 0.9% in men. Similarly, for urinary incontinence in women, although the prevalence increased from the 62–69 age group (46.3%) to the 70–79 age group (55.1%), the prevalence slightly decreased in the 80–90 age group (53.4%). The greatest increases in disease prevalence between the 62–69 and 80–90 age groups, for both genders, occurred for heart conditions (~17–22% increase), arthritis (~7–14%), urinary incontinence (~7–15%) and stroke (~9–11%).
Table 4.
Selected Chronic Conditions by Age and Gender for Waves 1 and 2 of NSHAP
| Wave 2 | Men | Women | ||||||||||
| 62–69 | 70–79 | 80–90 | 62–69 | 70–79 | 80–90 | |||||||
| n = 566 | n = 610 | n = 338 | n = 655 | n = 633 | n = 394 | |||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |
| Heart condition | 27.8 | 2.8 | 35.7 | 3.4 | 49.6 | 4.4 | 19.3 | 1.8 | 26.2 | 1.6 | 36.2 | 3.3 |
| Cancera | 24.2 | 2.3 | 40.1 | 2.5 | 39.2 | 3.0 | 18.4 | 2.6 | 26.0 | 2.1 | 27.4 | 3.0 |
| Stroke | 8.3 | 2.0 | 10.2 | 1.5 | 18.8 | 3.7 | 7.8 | 1.3 | 6.8 | 1.1 | 16.3 | 2.9 |
| COPD/asthma | 11.4 | 1.4 | 15.0 | 1.7 | 15.6 | 2.6 | 20.1 | 2.1 | 16.6 | 1.5 | 14.8 | 2.1 |
| Alzheimer’s disease or dementia | 2.7 | 1.8 | 1.9 | 0.5 | 1.3 | 1.0 | 1.0 | 0.5 | 1.0 | 0.4 | 4.2 | 1.3 |
| Diabetes | 22.7 | 2.4 | 27.3 | 2.8 | 24.4 | 3.7 | 18.2 | 1.7 | 21.1 | 1.8 | 19.7 | 2.4 |
| Hypertension | 58.3 | 2.3 | 63.2 | 2.7 | 58.1 | 4.2 | 54.3 | 2.7 | 64.2 | 2.3 | 63.9 | 3.0 |
| Arthritis | 25.8 | 2.1 | 27.9 | 1.9 | 32.9 | 2.9 | 35.9 | 2.9 | 43.3 | 2.8 | 50.0 | 3.0 |
| Urinary incontinence | 25.8 | 2.3 | 38.4 | 3.0 | 40.5 | 3.6 | 46.3 | 2.7 | 55.1 | 2.8 | 53.4 | 3.4 |
| Wave 1 | Men | Women | ||||||||||
| 57–64 | 65–74 | 75–85 | 57–64 | 65–74 | 75–85 | |||||||
| n = 528 | n = 547 | n = 379 | n = 492 | n = 545 | n = 514 | |||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | |
| Heart conditionb | 15.0 | 2.3 | 22.0 | 1.7 | 32.4 | 2.6 | 10.5 | 1.5 | 9.8 | 1.0 | 16.6 | 1.7 |
| Cancera | 19.4 | 2.1 | 29.7 | 2.2 | 38.2 | 2.5 | 18.0 | 2.0 | 7.3 | 2.1 | 30.4 | 2.7 |
| Stroke | 4.7 | 0.8 | 8.1 | 1.4 | 14.5 | 2.1 | 6.7 | 1.1 | 7.5 | 1.1 | 11.5 | 1.2 |
| COPD/asthma | 12.2 | 1.9 | 16.2 | 1.8 | 12.9 | 1.8 | 21.1 | 2.0 | 20.5 | 1.8 | 17.1 | 2.0 |
| Alzheimer’s disease or dementia | 0.0 | 0.0 | 0.3 | 0.2 | 2.3 | 0.6 | 0.4 | 0.3 | 1.1 | 0.4 | 1.3 | 0.4 |
| Diabetes | 20.4 | 1.9 | 22.8 | 2.1 | 21.6 | 2.2 | 17.8 | 2.2 | 20.3 | 1.8 | 15.7 | 1.7 |
| Hypertension | 45.2 | 3.2 | 61.9 | 2.1 | 56.4 | 2.9 | 47.9 | 2.4 | 53.8 | 2.8 | 64.5 | 2.7 |
| Arthritis (any) | 37.3 | 1.9 | 44.6 | 2.3 | 55.0 | 3.2 | 53.5 | 2.1 | 58.2 | 1.9 | 68.6 | 2.2 |
| Urinary incontinence | 19.1 | 2.1 | 28.3 | 2.1 | 35.5 | 2.7 | 58.3 | 2.4 | 51.3 | 2.3 | 57.3 | 2.1 |
Notes. COPD = chronic obstructive pulmonary disease; NSHAP = National Social Life, Health and Aging Project.
aIncluded all cancer types.
bIncluded respondents with any of the following conditions: heart attack, procedure for heart failure, surgery to unclog arteries in leg.
Additionally, there were several notable trends in gender differences. First, men more frequently reported heart conditions, cancer, diabetes, and stroke than women, regardless of age. The greatest gender difference occurred in heart conditions, with the prevalence difference ranging from 8.5% to 13.5% across the age groups. In contrast, women had a higher prevalence of arthritis, with the greatest difference in the oldest age group (50.0% vs. 32.9%). Similarly, women had a higher prevalence of urinary incontinence across all age groups, with this difference being greatest in the youngest age group (46.3% vs. 25.8%). Finally, certain chronic conditions were more prevalent among one gender in the youngest age group, but the gender differences reversed among older cohorts. For example, hypertension and Alzheimer’s disease were more common among men in the 62–69 age group (58.8% vs. 54.4% and 2.7% vs. 1.0%, respectively) but were more common among women in the 80–90 age group (63.9% vs. 58.1% and 4.2% vs. 1.3%, respectively). Conversely, COPD and Asthma were more common among women (vs. men) aged 62–69 years (20.1% vs. 11.4%) and were more common among men (vs. women) aged 80–90 years (15.6% vs. 14.8%) than women.
For comparison, Table 4 (Wave 1) displays prevalence rates in NSHAP Wave 1 for analogous chronic conditions by age and gender. For the majority of these conditions, the prevalence rates and trends in these rates were similar; however, there were a few observed differences. For example, both heart conditions and Alzheimer’s disease were more commonly reported in Wave 2 than in Wave 1. In contrast, a diagnosis of arthritis was less commonly reported in Wave 2 compared with Wave 1. To examine these observed differences further, prevalences for these conditions were compared across Waves 1 and 2 holding age constant at the Wave 2 age groups for both waves (62–69, 70–79, and 80–90). For both men and women, the prevalence of heart conditions was significantly (p < .01) higher and the prevalence of arthritis was significantly lower in Wave 2 compared with Wave 1 across all ages. For men, the prevalence of Alzheimer’s disease and dementia was significantly higher in Wave 2 compared with Wave 1 in the youngest age group, with this difference approaching statistical significance in women (p = .085; Table 5).
Table 5.
Comparison Between Prevalences for Heart Conditions, Alzheimer’s Disease/Dementia, and Arthritis Across Waves 1 (W1) and 2 (W2) of NSHAP, Holding Age Constant
| Men | 62–69 | 70–79 | 80–90 | ||||||
| W1 | W2 | p a | W1 | W2 | p | W1 | W2 | p | |
| n = 481 | n = 566 | n = 477 | n = 610 | n = 158 | n = 338 | ||||
| % | % | % | % | % | % | ||||
| Heart conditions | 19.3 | 27.8 | .001 | 25.8 | 35.7 | .001 | 34.0 | 49.6 | .004 |
| Alzheimer’s disease or dementia | 0 | 2.7 | <.001 | 1.1 | 1.9 | .317 | 3.0 | 3.2 | .939 |
| Arthritis | 40.8 | 25.8 | <.001 | 49.8 | 27.9 | <.001 | 54.9 | 32.9 | <.001 |
| Women | W1 | W2 | p a | W1 | W2 | P | W1 | W2 | p |
| n = 502 | n = 655 | n = 528 | n = 633 | n = 231 | n = 394 | ||||
| % | % | % | % | % | % | ||||
| Heart conditions | 9.9 | 19.3 | <.001 | 13.0 | 26.2 | <.001 | 20.2 | 35.5 | <.001 |
| Alzheimer’s disease or dementia | 0.2 | 1.0 | .085 | 1.6 | 1.0 | .775 | 1.4 | 4.3 | .078 |
| Arthritis | 58.5 | 35.9 | <.001 | 62.7 | 43.3 | <.001 | 67.5 | 50.5 | <.001 |
Notes. NSHAP = National Social Life, Health and Aging Project.
a p Value derived from Z-score calculation based on the difference between proportions (weighted) and sample sizes of each group.
The Modified CCI and the NCI were highly correlated in this sample (r = .89). The distributions of both the Modified CCI and NCI are presented for the entire sample (Figure 1). As to be expected, the mean Modified CCI was lower (M = 1.2, SE = 0.1) than that of the NCI (M = 2.7, SE = 0.1), as a result of its inclusion of fewer conditions. Additionally, fewer respondents scored a 0 using the NCI (8.3%) compared with the Modified CCI (42.1%). Likewise, more individuals had an index score of 2 or greater using the NCI (70.6%) as compared to the Modified CCI (32.4%). Table 6 reports the distributions and mean scores for each index stratified by gender and age group. For both indices, mean scores were lowest for the 62–69 age group; men had slightly higher mean scores than women across all age groups for the Modified CCI, with this gender difference less evident for the NCI. The distributions of the index scores also differed by age group. The highest percentage of individuals with index scores of 0 was found in the 62–69 age group. Likewise, the lowest percentage of individuals with index scores of 2 or greater were found in this group, with the percentage of individuals with scores 2 or greater increasing across the age groups. Men were more likely than women to have index scores of 0 for the NCI; however, this trend was reversed for the Modified CCI. Similarly, while women were more likely to have index scores of 2 or greater, compared with men, for the NCI, this trend reversed for the Modified CCI.
Figure 1.
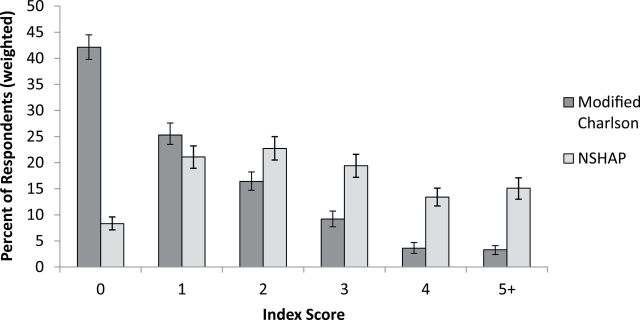
Distribution of comorbidity indices. Each bar represents the percent of respondents with that index score, with separate bars for the Modified Charlson Comorbidity Index and the NSHAP Comorbidity Index. Error bars represent 95% confidence intervals.
Table 6.
Comorbidity Indices by Age and Gender
| Men | Women | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 62–69 | 70–79 | 80–90 | 62–69 | 70–79 | 80–90 | ||||||||
| n = 566 | n = 610 | n = 338 | n = 655 | n = 633 | n = 394 | ||||||||
| % | SE | % | SE | % | SE | % | SE | % | SE | % | SE | ||
| Modified Charlson Comorbidity Index | |||||||||||||
| 0 | 48.5 | 2.4 | 30.2 | 2.4 | 30.1 | 3.5 | 51.4 | 2.7 | 43.4 | 2.4 | 38.2 | 2.7 | |
| 1 | 20.6 | 1.9 | 24.0 | 2.9 | 22.5 | 2.5 | 28.8 | 2.2 | 27.8 | 2.3 | 27.6 | 2.9 | |
| 2 | 15.5 | 2.1 | 23.0 | 2.9 | 18.4 | 3.0 | 10.3 | 1.9 | 15.8 | 2.3 | 19.4 | 2.8 | |
| 3 | 10.1 | 1.7 | 11.0 | 1.7 | 13.5 | 2.5 | 5.1 | 1.5 | 9.2 | 1.7 | 9.2 | 1.8 | |
| 4 | 2.1 | 0.6 | 6.2 | 1.5 | 11.9 | 4.2 | 1.8 | 0.7 | 1.8 | 0.7 | 2.5 | 0.7 | |
| 5+ | 3.2 | 0.8 | 5.6 | 1.0 | 3.7 | 0.9 | 2.5 | 1.4 | 2.0 | 0.7 | 2.9 | 0.7 | |
| M | SE | M | SE | M | SE | M | SE | M | SE | M | SE | ||
| 1.1 | 0.1 | 1.7 | 0.1 | 1.7 | 0.1 | 0.9 | 0.1 | 1.1 | 0.1 | 1.2 | 0.1 | ||
| NSHAP Comorbidity Index | |||||||||||||
| 0 | 12.3 | 1.3 | 7.2 | 1.3 | 6.2 | 1.2 | 10.8 | 1.4 | 4.4 | 1.0 | 5.5 | 1.1 | |
| 1 | 27.4 | 2.7 | 19.5 | 2.4 | 16.4 | 2.5 | 23.9 | 2.2 | 16.9 | 1.8 | 15.9 | 2.3 | |
| 2 | 19.8 | 2.6 | 21.8 | 2.2 | 16.4 | 2.4 | 24.8 | 2.4 | 26.9 | 2.5 | 23.2 | 2.7 | |
| 3 | 17.3 | 2.4 | 18.5 | 2.2 | 18.1 | 2.6 | 20.4 | 1.9 | 22.3 | 1.7 | 19.2 | 2.2 | |
| 4 | 11.6 | 2.2 | 14.3 | 2.1 | 16.9 | 3.7 | 9.5 | 1.4 | 14.4 | 2.0 | 19.4 | 2.0 | |
| 5+ | 11.5 | 1.5 | 18.9 | 2.4 | 25.5 | 4.3 | 10.7 | 1.9 | 15.1 | 2.0 | 16.8 | 2.3 | |
| M | SE | M | SE | M | SE | M | SE | M | SE | M | SE | ||
| 2.2 | 0.1 | 2.7 | 0.1 | 3.0 | 0.1 | 2.3 | 0.1 | 2.7 | 0.1 | 2.8 | 0.1 | ||
Discussion
This paper reports the prevalence of several important chronic conditions in Wave 2 of NSHAP. Additionally, this study compares 2 approaches to combine the chronic illness data into useful comorbidity indices: the Modified CCI and the NCI.
Comparison to Reported National Prevalence Rates
The most prevalent conditions in NSHAP were hypertension, incontinence, arthritis, any heart condition, cancer, and diabetes. These conditions correspond with national reports of the most prevalent conditions in adults aged 65 years and older (CDC, 2010; He et al., 2005; NCHS, 2013). The most notable differences between chronic disease prevalence reported in NSHAP versus other national samples were for Alzheimer’s disease/dementia, arthritis, and incontinence. For Alzheimer’s disease/dementia, the overall prevalence was much lower (2.1%) than compared to other reports (ADAMS, 13.9%) (Plassman et al., 2007). This is likely due to the selection criteria for NSHAP Wave 1. Participants were excluded from Wave 1 if the interviewer felt the participant had inadequate cognitive ability to complete the survey questions, thus likely reducing the dementia prevalence in Wave 2. The prevalence of arthritis in NSHAP (34.1%) was also lower than the prevalence reported by the NHIS (50.0%). This is most likely because NSHAP only inquired about the 2 most prevalent arthritic conditions (osteoarthritis and rheumatoid arthritis) but did not ask about other forms of arthritis that were included in the NHIS prevalence estimates, which included any form of arthritis, gout, lupus, and/or fibromyalgia (CDC, 2010). Finally, the prevalence for urinary incontinence was higher in NSHAP Wave 2 compared with reports from the MCBS (MCBS, 2009).
Another interesting finding was that, for several conditions, there was a plateau in the prevalences between the 70–79 and 80–90 age groups. This trend was similar to those found in the NHIS for diabetes, COPD/asthma, and cancer (CDC, 2010). However, this trend differed between NSHAP Wave 2 and the MCBS for urinary incontinence, with the prevalence of urinary incontinence increasing between 65–74, 75–84 and 85+ age groups (MCBS, 2009). Interestingly, while the overall prevalence of urinary incontinence was higher in NSHAP Wave 2 compared with the MCBS (as noted above), prevalences for men and women in the 80–90 age group of NSHAP Wave 2 (40.5% and 53.4%, respectively) were similar to those of the 85+ age group in the MCBS (35.3% and 58.9%, respectively) (MCBS, 2009).
It is important to note that the national studies used for these comparisons (NHIS, ADAMS, and MCBS) are mainly community-based samples, though the MCBS also included institutionalized Medicare beneficiaries. In a paper using data from the National Long-Term Care Study, incidences for neurodegenerative diseases and heart failure were higher in individuals in institutions, as well as those with severe disabilities, as compared to non-disabled individuals (Akuschevich, Kravchenko, Ukraintseva, Arbeev, & Yashin, 2013). Interestingly, this study also reported that incidences for some conditions were actually lower in institutionalized individuals; these conditions included several types of cancer (e.g., melanoma and colon cancer) and asthma. Overall, we note that our estimates may differ with samples that primarily include institutionalized individuals.
Comparison Between Waves 1 and 2 of NSHAP
In general, the overall prevalence as well as age and gender trends were consistent between Waves 1 and 2 of NSHAP. However, there were notable differences in heart conditions, Alzheimer’s disease/dementia, and arthritis, worth considering when comparing health trends over time. In follow-up analyses holding age constant in both waves at the Wave 2 age groups (62–69, 70–79, and 80–90), these observed differences were statistically significant across all ages for heart conditions and arthritis. The prevalence of heart conditions was higher in Wave 2 than in Wave 1. In Wave 2, the respondents were asked the overall question “Has a doctor ever told you that you have a heart condition?”, whereas in Wave 1, an overall heart condition question was not asked. Thus, the heart condition prevalence for Wave 1 presented here combined 3 questions that asked the respondents to report about ever having had a heart attack, treatment for heart failure, or history of having a procedure to restore arterial circulation in the legs. For researchers interested in studying heart conditions in a longitudinal context (using both Waves 1 and 2), it may be more practical to use specific conditions, such as heart attack. Additionally, the prevalence for arthritis in Wave 2 was lower compared with Wave 1. As noted above, the Wave 2 question concerning arthritis was specific to osteoarthritis or rheumatoid arthritis, whereas the corresponding Wave 1 question asked if the respondent had arthritis, with no specifications. Thus, the prevalence rate for arthritis in Wave 1 is more similar to CDC prevalence rates, whereas the Wave 2 question is not strictly comparable to the CDC rate (and has a lower reported prevalence) because it does not include all arthritic conditions. Finally, for Alzheimer’s disease and dementia, the prevalence was significantly higher in Wave 2 compared with Wave 1 only in the youngest age group (62–69 years) and only in men. However, this difference approached significance in this age group in women. The prevalence for Alzheimer’s disease/dementia may be higher in Wave 2, especially in younger individuals, because the questions in Wave 2 specified the different forms of dementia and included mild cognitive impairment, whereas the question in Wave 1 asked broadly about having either dementia or Alzheimer’s disease. It is also important to note that another key difference in data collection between Wave 1 and Wave 2 of NSHAP was the inclusion of spouse/partner data. Wave 2 included not only prior Wave 1 respondents but also their spouses/partners; Wave 1 did not include these data. Previous research has found that spouses may have high concordance rates for some chronic conditions, including heart disease, thus their inclusion in Wave 2 may have altered the prevalences (Meyler, Stimpson, & Peek, 2007). However, analysis of NSHAP Wave 2 data included the use of sample weights (distributed with the dataset), which limit the effects of potential biases (O’Muircheartaigh et al., 2014). Overall, while the prevalences for the majority of the chronic conditions were consistent between Waves 1 and 2 of NSHAP, researchers who are interested in using the chronic condition data in a longitudinal context must be aware of changes in the assessment of chronic conditions between Waves 1 and 2 of NSHAP that have been detailed in both the Discussion and Method sections of this paper.
Comorbidity Indices
For this paper, we provided 2 approaches to grouping chronic conditions into weighted comorbidity indices: a Modified CCI and more robust NCI. Due to its inclusion of additional chronic conditions, the mean index score for the NCI was higher than the mean index score for the Modified CCI, both overall and across all age and gender groups; for both indices, index scores increased with age and women had higher scores compared with men. In regards to the overall distributions of the index scores, there was a higher percentage of individuals with index scores of 2 or greater using the NCI, compared with the Modified CCI. The key difference between these indices is that the NCI included several highly prevalent conditions (e.g., hypertension and incontinence) that the Modified CCI did not. In fact, hypertension and incontinence were the most prevalent chronic condition in this sample, with prevalences of approximately 60% and 47%, respectively. Thus, the addition of such highly prevalent conditions increased the number of respondents having at least one chronic condition. Unlike the majority of comorbidity indices that focus only on conditions linked to mortality, the NCI was specifically designed to be a broad index that includes conditions also related to overall morbidity and function; specifically, the NCI added measures of hypertension, bone health (osteoarthritis, osteoporosis, hip fracture), skin cancer (melanoma), and incontinence. Given the inclusion of a broader spectrum of conditions in the NCI, it may be a more useful index than the Modified CCI for studies examining the relationship between chronic conditions and other health and wellness phenotypes, such as disability, psychosocial functioning, and overall quality of life. For example, incontinence was the second most prevalent condition in our population and has been broadly associated with not only physical health but also with emotional and social functioning (Landefeld et al., 2008). The Modified CCI, though, may be more appropriate for research questions focusing specifically on mortality. Additionally, although, for these analyses, we have used the original CCI weights for the same conditions included in the Modified CCI and the NCI, as well as weights of one for the 5 additional conditions in the NCI, researchers may wish to explore the use of different weights for different purposes. However, small changes in the weights for specific items are unlikely to have a substantial impact on the overall score. Overall, we encourage researchers to utilize either of these indices, or to create their own index, depending on their research questions.
Conclusions
The goal of this paper was to provide relevant background information on the chronic conditions included in Wave 2 of NSHAP and to present possible approaches to creating useful comorbidity indices. NSHAP includes a wide variety of measures assessing the chronic conditions that are common in older adults and that are highly associated with mortality and disability. Furthermore, chronic conditions have been linked to several other aspects of health, including mental and social health (Fukukawa et al., 2004; Moussavi et al., 2007; Penninx et al., 1999; Vogt, Mullooly, Ernst, Pope, & Hollis, 1992). Additionally, this paper presents multiple approaches to creating comorbidity indices. Specifically, this paper introduces the NCI, which includes not only conditions associated with mortality, but also other prevalent chronic conditions, such as hypertension, osteoporosis, and incontinence. The inclusion of a broad range of conditions makes the NCI a potentially useful tool in examining the effects of multiple morbidities on other health conditions, disability, social interactions, psychological functioning, and overall quality of life. With age-specific mortality rates declining and the average life expectancy near 80 years, understanding the combined, and long-term, influence of chronic conditions is becoming ever more important (Miniño, 2013). In addition to health researchers, clinicians, and practitioners are continuing to focus on multimorbidity in efforts to adopt a more patient-center approach (Salive, 2013). Thus, more inclusive indices, such as the NCI, that can assess the influences of multimorbidity on overall health and functioning would also be useful in clinical practice. Thus, combined with its extensive assessment of sociological, mental, and biological health determinants, NSHAP provides a valuable resource for the study of the impact of chronic conditions and comorbidity on overall health and aging.
Key Points
NSHAP Wave 2 collected information on several chronic conditions that are the leading causes of mortality and morbidity in individuals aged 65 years and older.
Prevalences for these chronic conditions were similar to national reports, with these prevalences differing by age group and gender.
The chronic conditions in NSHAP can be combined into comorbidity indices, which can be used to understand how total disease burden influences health and aging.
Funding
This work was supported by the National Institutes of Health including the National Institute on Aging, the Division of Behavioral and Social Sciences Research for the National Health, Social Life, and Aging Project (NSHAP) (R01 AG021487, R37 AG030481), the NSHAP Wave 2 Partner Project (R01 AG033903), and by NORC, which was responsible for the data collection.
Acknowledgments
T. Vasilopoulos and A. Kotwal performed the statistical analyses. T. Vasilopoulos, A. Kotwal, and M. J. Huisingh-Scheetz contributed to writing and revising the manuscript. L. J. Waite, M. K. McClintock, and W. Dale planned the study and contributed to revising the manuscript.
References
- Akuschevich I., Kravchenko J., Ukraintseva S., Arbeev K., Yashin A. (2013). Population-based analysis of incidence rates of cancer and noncancer chronic diseases in the US elderly using NLTCS/Medicare-Linked Database. ISRN Geriatrics, 2013, 1–15. 10.1155/2013/943418 [Google Scholar]
- American Cancer Society. (2011). Cancer facts & figures 2011. Atlanta, GA: American Cancer Society. :10.1080/15398285.2012.701177 [Google Scholar]
- American Diabetes Association. (2013). Diagnosis and classification of diabetes mellitus. Diabetes Care, 36(Suppl. 1), S67–S74. 10.2337/dc13-S067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2009). Prevalence and most common causes of disability among adults – United States, 2005. MMWR Morbidity and Mortality Weekly Report, 58, 421–426. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2010). National Center for Health Statistics. Health Data Interactive Source data: National Health Interview Survey (NHIS) Retrieved from www.cdc.gov/nchs/hdi.htm [Google Scholar]
- Chapman D. P., Williams S. M., Strine T. W., Anda R. F., Moore M. J. (2006). Dementia and its implications for public health. Preventing Chronic Disease, 3, A34. [PMC free article] [PubMed] [Google Scholar]
- Chapman K. R., Mannino D. M., Soriano J. B., Vermeire P. A., Buist A. S., Thun M. J., … Beasley R. (2006). Epidemiology and costs of chronic obstructive pulmonary disease. European Respiratory Journal, 27, 188–207. 10.1183/09031936.06.00024505 [DOI] [PubMed] [Google Scholar]
- Charlson M. E., Pompei P., Ales K. L., MacKenzie C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40, 373–383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- de Groot V., Beckerman H., Lankhorst G. J., Bouter L. M. (2003). How to measure comorbidity: A critical review of available methods. Journal of Clinical Epidemiology, 56, 221–229. 10.1016/j.jclinepi.2003.09.002 [DOI] [PubMed] [Google Scholar]
- de Lau L. M. L., Breteler M. (2006). Epidemiology of Parkinson’s disease. The Lancet Neurology, 5, 525–535. 10.1016/S1474-4422(06)70471-9 [DOI] [PubMed] [Google Scholar]
- Fukukawa Y., Nakashima C., Tsuboi S., Niino N., Ando F., Kosugi S., Shimokata H. (2004). The impact of health problems on depression and activities in middle-aged and older adults: Age and social interactions as moderators. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 59, P19–P26. 10.1093/geronb/59.1.P19 [DOI] [PubMed] [Google Scholar]
- Galinsky A., McClintock M., Waite L. (this issue). Sexual motivation, sexual satisfaction and physical contact in NSHAP Wave 2. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorina Y., Hoyert D., Lentzner H., Goulding M. (2005). Trends in causes of death among older persons in the United States. Aging Trends, 6, 1–12. [PubMed] [Google Scholar]
- Gregg F., O’Doherty K., Schumm L. P., McClintock M. K., Huang E. (this issue). The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He W., Sengupta M., Velkoff V. A., Dellaros K. A. (2005). 65+ in the United States: 2005. Current population reports. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Hebert L. E., Scherr P. A., Bienias J. L., Bennett D. A., Evans D. A. (2003). Alzheimer disease in the US population: Prevalence estimates using the 2000 census. Archives of Neurology, 60, 1119–1122. 10.1001/archneur.60.8.1119 [DOI] [PubMed] [Google Scholar]
- Hoffman J., McClintock M. K., You H. (this issue). Vaginal microbiology in NSHAP Wave 2. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [Google Scholar]
- Huisingh-Sheetz M. J., Kocherginsky M., Schumm L. P., Engelman M., McClintock M. K., Dale W., … Waite L. J. (this issue). Measuring functional status in the National Social Life, Health and Aging Project (NSHAP): Rationale, measurement and preliminary findings. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz J. N., Chang L. C., Sangha O., Fossel A. H., Bates D. W. (1996). Can comorbidity be measured by questionnaire rather than medical record review? Medical Care, 34, 73–84. 10.1097/00005650-199601000-00006 [DOI] [PubMed] [Google Scholar]
- Kern D. W., Wroblewski K. E., Schumm L. P., Pinto J. M., McClintock M. K. (this issue). Olfactory function in Wave 2 of the National Social Life, Health and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozloski M., McClintock M. K. (this issue). The utility and dynamics of salivary sex hormone measurements in the National Social Life, Health and Aging Project, Wave 2. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaszczak A., O’Doherty K., Colicchia M., Satorius J., McPhillips J., Czaplewski M., … Smith S. (this issue). Continuity and innovation in the data collection protocols of the second wave of the National Social, Life Health and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landefeld C. S., Bowers B. J., Feld A. D., Hartmann K. E., Hoffman E., Ingber M. J., … Trock B. J. (2008). National Institutes of Health state-of-the-science conference statement: Prevention of fecal and urinary incontinence in adults. Annals of Internal Medicine, 148, 449–458. 10.7326/0003-4819-148-6-200803180-00210 [DOI] [PubMed] [Google Scholar]
- Lauderdale D. S., Schumm L. P., Kurina L. M., McClintock M. K., Thisted R. A., Chen J., Waite L. J. (this issue). Assessment of sleep in the National Social Life, Health and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannino D. M., Homa D. M., Akinbami L. J., Ford E. S., Redd S. C. (2002). Chronic obstructive pulmonary disease surveillance – United States, 1971–2000. Respiratory Care, 47, 1184–1199. [PubMed] [Google Scholar]
- Markland A. D., Richter H. E., Fwu C., Eggers P., Kusek J. W. (2011). Prevalence and trends of urinary incontinence in adults in the United States, 2011 to 2008. The Journal of Urology, 186, 589–593. 10.1016/j.juro.2011.03.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare Current Beneficiary Survey. (2009). 2009 Health and Health Care Population, Table 2.2. Centers for Medicare and Medicaid Services, Retrieved from https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/Data-Tables.html [Google Scholar]
- Meyler D., Stimpson J. P., Peek M. K. (2007). Health concordance within couples: A systematic review. Social Science & Medicine, 64, 2297–2310. 10.1016/j.socscimed.2007.02.007 [DOI] [PubMed] [Google Scholar]
- Mikuls T. R., Saag K. G., Criswell L. A., Merlino L. A., Kaslow R. A., Shelton B. J., Cerhan J. R. (2002). Mortality risk associated with rheumatoid arthritis in a prospective cohort of older women: Results from the Iowa Women’s Health Study. Annals of the Rheumatic Diseases, 61, 994–999. 10.1136/ard.61.11.994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miniño A. M. (2013). Death in the United State, 2011. NCHS data brief, no. 115. Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Moussavi S., Chatterji S., Verdes E., Tandon A., Patel V., Ustun B. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet, 370, 851–858. 10.1016/S0140-6736(07)61415-9 [DOI] [PubMed] [Google Scholar]
- National Center for Health Care Statistics (NCHS). (2013). Data file documentation, National Health Interview Survey 2012. Hyattsville, MD: National Center for Health Care Statistics, Centers for Disease Control and Prevention. [Google Scholar]
- O’Doherty K., You H., McClintock M. K., Dale W., Jaszczak A., Hoffman J., Kern D. W. (this issue). Biomeasure samples from the field to the lab in NSHAP Wave 2. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Muircheartaigh C., English N., Pedlow S. (this issue). Sampling in Wave 2 of the National Social Life, Health and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne C., McClintock M., Dale W. (this issue). Mental health measures in NSHAP Wave 2. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peat G., McCarney R., Croft P. (2001). Knee pain and osteoarthritis in older adults: A review of community burden and current use of primary health care. Annals of Rheumatic Diseases, 60, 91–97. 10.1136/ard.60.2.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx B. W., van Tilburg T., Kriegsman D. M., Boeke A. J., Deeg D. J., van Eijk J. T. (1999). Social network, social support, and loneliness in older persons with different chronic diseases. Journal of Aging and Health, 11, 151–168. 10.1177/089826439901100202 [DOI] [PubMed] [Google Scholar]
- Pinto J. M., Kern D. W., Wroblewski K. E., Schumm L. P., McClintock M. K. (this issue). Assessment of sensory function in Wave 2 of the National Social Life, Health and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plassman B. L., Langa K. M., Fisher G. G., Heeringa S. G., Weir D. R., Ofstedal M. B., … Wallace R. B. (2007). Prevalence of dementia in the United State: The Aging, Demographics and Memory Study. Neuroepidemiology, 29, 125–132 doi: 10.1159/0000109998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes T., Galinsky A., You H., McClintock M. K., Hoffman J. (this issue). Social proteins: Urine analysis in NSHAP Wave 2. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. [Google Scholar]
- Salive M. E. (2013). Multimorbidity in adults. Epidemiological Reviews, 35, 75–83. :10.1093/epirev/mxs009 [DOI] [PubMed] [Google Scholar]
- Shega J. W., Sunkara P. D., Kotwal A., Kern D. W., Leitch S. L., McClintock M. K., … Dale W. (2014). Measuring cognition: The Chicago Cognitive Function Measure (CCFM) in the National Social Life, Health and Aging Project (NSHAP), Wave 2. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shega J. W., Tiedt A., Grant K., Dale W. (2014). Pain measurement in the National Social Life, Health and Aging Project (NSHAP): Presence, intensity, and location. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent G. K., Velkoff V. A. (2010). The older population in the United States: 2010 to 2050: The next four decades. Current Population Reports. Washington, DC: U.S. Census Bureau. [Google Scholar]
- Vogt T. M., Mullooly J. P., Ernst D., Pope C. R., Hollis J. F. (1992). Social networks as predictors of ischemic heart disease, cancer, stroke and hypertension: Incidence, survival and mortality. Journal of Clinical Epidemiology, 45, 659–666. 10.1016/0895-4356(92)90138-D [DOI] [PubMed] [Google Scholar]
- Williams S. R., Pham-Kanter G., Leitsch S. A. (2009). Measures of chronic conditions and diseases associated with aging in the National Social Life, Health, and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64(Suppl. 1), i67. 10.1093/geronb/gbn015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky F. D., Fitzgerald J. F., Stump T. E. (1997). The effect of hip fracture on mortality, hospitalization, and functional status: A prospective study. American Journal of Public Health, 87, 398–403. 10.2105/AJPH.87.3.398 [DOI] [PMC free article] [PubMed] [Google Scholar]


