Abstract
Objectives.
This paper introduces new measures of neighborhood context that are included in the second wave of the National Social Life, Health, and Aging Project (NSHAP). We describe the use of field interviewer ratings of respondents’ neighborhood conditions, as well as the adaptation of existing measures for the assessment of neighborhood social context among urban and nonurban older adults.
Method.
We construct scales of neighborhood problems, neighborhood social cohesion, neighborhood social ties, and perceived neighborhood danger, and assess their reliability and validity. We then calculate descriptive statistics for measures of neighborhood context across respondent age, gender, and racial/ethnic background, and across low-, moderate-, and high-density residential blocks.
Results.
We find that older women report greater neighborhood cohesion and more neighborhood ties than older men, but women also perceive more neighborhood danger. Black and Hispanic older adults reside in neighborhoods with more problems, lower cohesion, fewer social ties, and greater perceived danger. Neighborhood characteristics also vary across residential densities. Neighborhood problems and perceived danger increase with block-level density, but neighborhood social cohesion and social ties were lowest among residents of moderate-density blocks.
Discussion.
The inclusion of neighborhood context measures in the second wave of NSHAP provides a unique opportunity to explore associations among neighborhood context, social connectedness, and indicators of health and function among older adults. We discuss limitations of the measures and provide recommendations for their use.
Key Words: Aging, Environment, Fear, Neighborhood context, Neighborhood disorder.
As the proportion of older adults who are aging in their communities increases, so does evidence of the critical role of neighborhood context for health and well-being in later life (for reviews, see Cagney & York Cornwell, 2010; Diez Roux & Mair, 2010; Yen, Michael, & Perdue, 2009). In fact, older adults may be more vulnerable to—and more dependent upon—the physical conditions and social resources in their residential environment than middle-aged and younger adults (Cannuscio, Block, & Kawachi, 2003; Robert & Li, 2001). Later life changes, such as retirement from work and declines in health and physical function, contribute to a centering of daily activities within the residential milieu (Moss & Lawton, 1982). At the same time, losses of friends and family members may increase older adults’ reliance on social resources and support available through community-based institutions such as senior centers and churches (Miner, Logan, & Spitze, 1993) and informal interactions with neighbors (Barker, 2002). As a primary locus for daily activities and social engagement, neighborhood environments can promote health, provide social capital, enhance coping with health problems, and reduce disablement (Clarke et al., 2008; Wen, Cagney, & Christakis, 2005). But disadvantaged neighborhoods that lack resources and social support can increase isolation, fear of victimization, and risks of illness, accidents, and decline (Schroder-Butterfill & Marianti, 2006; Taylor, Eitle, & Russell, 2009).
New indicators of neighborhood context in the second wave of the National Social Life, Health, and Aging Project (NSHAP) offer important opportunities to gain insight into the role of neighborhood context for community-residing older adults’ health and well-being. NSHAP Wave 2 introduces field interviewer assessments of neighborhood physical conditions, such as dilapidated buildings, litter, and traffic. Previous research indicates that such physical neighborhood problems may elicit stress, fear, or discomfort (Hill, Ross, & Angel, 2005; Steptoe & Feldman, 2001), heighten the risk of depression (Beard et al., 2009; Kim, 2010; Latkin & Curry, 2003), and shape health-related behaviors like smoking and walking for exercise (Echeverría, Diez-Roux, Shea, Borrell, & Jackson, 2008; Mendes de Leon et al., 2009).
The second wave of NSHAP also includes respondent reports of social cohesion in their neighborhood and their connectedness with their neighbors. Social cohesion is a form of neighborhood social capital—mutual trust and solidarity among residents form a resource that inheres in ties among neighbors. Collective efficacy theory further suggests that cohesion, along with informal social control, enhances a community’s ability to take action for the common good (Sampson, Raudenbush, & Earls, 1997). Connectedness and trust among residents of cohesive neighborhoods may also be critical for older adults’ health and well-being. Neighborhood social cohesion enables rapid diffusion of health-relevant information and increases residents’ sense of purpose and meaning in life (Kawachi & Berkman, 2000). It also has been associated with fewer depressive symptoms among middle-aged and older adults (Echeverría et al., 2008; Kim, 2010).
Social exchanges and support among neighbors, like visiting, sharing advice, and doing favors, are likely associated with neighborhood-level social cohesion. But these kinds of exchanges and activities are important to consider separately because they involve actual social ties and interactions, rather than the more general sense of solidarity and trust that characterizes social cohesion. These everyday exchanges and activities, especially when reciprocated or relatively equal, can strengthen community-level social capital and provide fertile ground for the emergence of social cohesion and informal social control (Cagney et al., 2009; Sampson, Morenoff, & Earls, 1999). Although they do not require close relationships among neighbors, social ties and exchanges of support in the neighborhood can enable older adults’ continued residence in the community and enhance coping with the loss of social ties, functional impairments, and illness (Barker, 2002; Mair, Diez Roux, & Morenoff, 2010; Shaw, 2005; Wethington & Kavey, 2000).
Finally, the second wave of NSHAP introduces assessments of respondents’ perceptions of neighborhood danger. Fear of victimization may be a key mechanism through which neighborhood context affects health; previous research suggests that neighborhood fear has both proximal and distal effects on a wide range of physical and mental health outcomes (Stafford, Chandola, & Marmot, 2007). For instance, fear can prevent older adults from leaving their homes, thereby limiting opportunities for healthy physical activity such as taking walks (Liska, Sanchirico, & Reed, 1988; Ross & Mirowsky, 2001). Older adults with functional limitations may feel especially threatened by their surroundings, leading to feelings of distress, vulnerability, and social isolation (Krause, 1993). And, when fear reduces street activity in the neighborhood, older adults may be further persuaded to remain indoors (Jacobs, 1961; Klinenberg, 2002).
The measures of neighborhood context in NSHAP open up several new directions for research. For example, the collection of these measures alongside data on social networks and biomeasures allow researchers to explore how neighborhood conditions are associated with prodromal health changes, physiological processes, and social connectedness. The inclusion of coresident partners in Wave 2 enables a closer look at gender differences in the perception of neighborhood context, and in associations between neighborhood conditions, neighborhood social resources, and health status.
In addition, neighborhood context measures in NSHAP Wave 2 will allow researchers to explore unanswered questions regarding the meaning and consequences of neighborhoods outside the confines of the city. Much of the sociological and gerontological research on the role of neighborhood context in health and aging has focused on urban areas, but an increasing proportion of older adults reside in suburban areas and small towns (Frey, 2003). Variations in population density across residential areas may shape social contexts and physical features of the neighborhood that are consequential for the health and well-being of community-residing older adults.
The purpose of this paper is to introduce the measures of neighborhood context that are included in the second wave of NSHAP. We devote particular attention to describing the adaptation of traditional measures of neighborhood social context to enhance their applicability across urban and nonurban areas. We use the NSHAP measures to construct reliable scales capturing neighborhood disorder, neighborhood social cohesion, neighborhood social ties, and perceived neighborhood danger. We demonstrate the validity of the scales, and then examine variations in neighborhood contexts across sociodemographic groups and residential densities. Finally, we provide recommendations regarding the use of measures of neighborhood context in the second wave of NSHAP.
Method
NSHAP is a nationally representative, population-based longitudinal study of community-residing older adults in the contiguous United States. The NSHAP sample for the first wave of data collection was based on a multistage area probability design screened by the Institute for Social Research for the Health and Retirement Study (HRS). The HRS design oversampled by race/ethnicity; NSHAP additionally stratified by age and gender to equalize cases across age/gender categories (for more details, see O’Muircheartaigh, Eckman, & Smith, 2009). Data for Wave 1 were collected in 2005–2006 through in-person interviews with 3,005 older adults, aged 57–85 years. The weighted response rate was 75.5%. Measures of neighborhood context were introduced in the second wave of NSHAP, conducted in 2010–2011. This wave included 2,261 returning respondents from Wave 1 (weighted response rate of 88.8%), 161 respondents who were sampled for Wave 1 but did not participate then, and 955 cohabiting spouses or romantic partners of Wave 2 respondents (774 of whom are within the NSHAP age range; see Jaszczak et al., in this issue). Measures and descriptive statistics provided in this paper are based on Wave 2 respondents and their age-eligible partners. Data are publicly available (NSHAP Wave 2: Waite, Linda J., Kathleen Cagney, William Dale, Elbert Huang, Edward O. Laumann, Martha K. McClintock, Colm A. O’Muircheartaigh, L. Phillip Schumm, and Benjamin Cornwell. National Social Life, Health, and Aging Project (NSHAP): Wave 2 and Partner Data Collection. ICPSR34921-v1. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2014-04-29. doi:10.3886/ICPSR34921.v1.).
Although NSHAP captured the majority of biological, psychological, and social measures during in-person interviews, items assessing neighborhood context are captured in a leave-behind questionnaire (LBQ) and the Field Interviewer Questionnaire (FIQ). Following the in-person interview, respondents were given a LBQ to complete on their own time and return to NORC at the University of Chicago using a stamped envelope that was provided. If the LBQ was not returned within 3 weeks of the interview, NORC contacted respondents by phone to encourage them to return the LBQ. The final return rate for the Wave 2 LBQ was 87%.
The FIQ was completed by the field interviewer at the conclusion of his or her interview with the respondent. Field interviewers were required to complete the FIQ in order to close each case; they were instructed to do this on the same day as the interview. The FIQ included questions regarding the respondent and his or her neighborhood context and interior living conditions (see York Cornwell, in press), as well as administrative aspects of the case.
Field Interviewer Ratings of Neighborhood Characteristics
NSHAP’s use of in-home interviews affords field interviewers a unique opportunity to observe respondents’ residential contexts. We capitalize on this by asking field interviewers to provide information about physical and ambient or environmental conditions of respondents’ neighborhoods. Our approach draws from methods of systematic social observation of neighborhood disorder introduced in the Project on Human Development in Chicago Neighborhoods, in which trained observers visited residential blocks in Chicago and tallied the presence of particular features of social and physical disorder (Sampson & Raudenbush, 1999). At the conclusion of each NSHAP interview, the field interviewer completed the FIQ, during which he or she was asked to “describe the street (one block, both sides) where the respondent lives” on five metrics. In addition, field interviewers were asked to evaluate the overall condition of the buildings on the street.
This approach allows us to glean valuable information about the conditions of the respondent’s residential environment without adding to respondent burden. However, interviewer-rated neighborhood characteristics are not available for respondents who were not interviewed in their own homes. Although the vast majority (96.81%) of Wave 2 age-eligible respondents completed in-home interviews, 103 respondents were interviewed in another location. Nonhome interviews in locations such as a family member’s home, a workplace, or a community library were in line with administrative protocols when requested by respondents (e.g., due to privacy concerns or convenience).
Neighborhood density.
Field interviewer assessments of the street where the respondent lives (“one block, both sides”) include a rating of residential density. This was captured on a five-point continuum ranging from “buildings/houses are close together” to “buildings/houses are far apart.” We reverse code this item so that higher values indicate greater density. Summary statistics are presented in Table 1. Nearly, 25% of NSHAP respondents reside on low-density blocks (response categories 1–2; n = 756), about 33% on moderate-density blocks (response category 3; n = 1,006), and about 43% on high-density blocks (response categories 4–5; n = 1,324).
Table 1.
Descriptive Statistics for Interviewer-Rated Neighborhood Conditions
| Variable | Range | Mean | Standard deviation | N a |
|---|---|---|---|---|
| 1 → 5 | ||||
| Densityb | Buildings are far apart → Buildings are close together | 3.222 | 1.195 | 3,086 |
| Litter | Clean → Full of litter or rubble | 1.587 | .842 | 3,085 |
| Noise | Quiet → Noisy | 1.655 | .949 | 3,084 |
| Traffic | No traffic on street → Heavy traffic on street | 1.985 | 1.032 | 3,088 |
| Odor/pollution | No smell or air pollution → Strong smell or air pollution | 1.319 | .672 | 3,089 |
| R’s buildingb | 1 = Very well kept to 4 = Very poorly kept (needs major repairs) | 1.567 | .760 | 3,084 |
| Other buildingsb | 1 = Very well kept to 4 = Very poorly kept (needs major repairs) | 1.652 | .727 | 3,044 |
Note. aDescriptive statistics provided are for all age-eligible Wave 2 respondents who were interviewed in their homes.
bResponse categories are reverse coded from their presentation in the Field Interviewer Questionnaire.
Neighborhood problems.
NSHAP used field interviewer observations to examine a set of neighborhood physical conditions that may threaten older adults’ health and well-being. Our approach is informed by neighborhood effects research and social disorganization theory, in which physical disorder such as litter, graffiti, and poorly maintained buildings is indicative of neighborhood socioeconomic disadvantage as well as weak social control and a lack of social cohesion at the neighborhood level (Ross & Mirowsky, 1999; Sampson et al., 1997, 1999; Shaw & McKay, 1942). Research suggests that neighborhood disorder may be an important mechanism through which neighborhood socioeconomic disadvantage affects health (Kim, 2010; Ross & Mirowsky, 2001; Wen, Browning, & Cagney, 2003).
Six interviewer-rated items capture the extent of problems or disorder on the respondent’s face block. NSHAP field interviewers assessed the presence of litter, noise, traffic, and odor/pollution as well as the overall condition of the respondent’s residence and other buildings on the block (see Table 1). Following previous research (e.g., Ross & Mirowsky, 1999), we combine these items into a scale assessing neighborhood problems. Because the number of response categories varies across the items, we first standardize them by calculating the deviance of each rating from the sample mean and dividing it by the standard deviation for that rating. Then, we average the standardized scores on individual items to arrive at a scale score for each respondent who had valid data on all of the ratings (n = 3,031). The resulting mean score for the neighborhood problems scale is 0.00 and the standard deviation is 0.728.
The scale has good internal consistency reliability. Cronbach’s α is maximized at .82 with the inclusion of all six items, and item-rest correlations range from .47 to .71. Scale reliability across residential densities and respondent gender is shown in Table 2. Recall that the Wave 2 sample includes 774 age-eligible coresident partners of respondents. These partner dyads coreside, but each partner was interviewed separately, so the data include two assessments of the conditions of their face blocks. To reduce the possibility that estimates of scale reliability are inflated by the similarity of neighborhood ratings within partner dyads, we test the reliability of the neighborhood problems scale (and the following neighborhood context scales) separately across male and female respondents. The partner dyads include only two same-sex couples, so gender-stratified analyses separate most of the partner dyads. Table 2 shows that the reliability of the scale is generally consistent across male and female respondents, as we would expect due to the fact that these conditions were assessed by the field interviewer. Reliability is highest for residents of mid-density blocks (α’s of .84 and .86) and high-density blocks (α’s of .82 and .82), but the scale also has good reliability for those who live on low-density blocks (α’s of .73).
Table 2.
Reliability of Neighborhood Scales, by Residential Density and Respondent Gender
| Overall | Low-density blocks | Mid-density blocks | High-density blocks | ||||
|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | Women | Men | ||
| Neighborhood problems | |||||||
| Cronbach’s α for scale | .822 | .733 | .730 | .837 | .855 | .817 | .824 |
| N a | 3,031 | 374 | 347 | 509 | 483 | 725 | 590 |
| Neighborhood social cohesion | |||||||
| Cronbach’s α for scale | .681 | .694 | .695 | .712 | .665 | .678 | .661 |
| N b | 2,691 | 330 | 323 | 437 | 419 | 611 | 496 |
| Neighborhood social ties | |||||||
| Cronbach’s α for scale | .756 | .774 | .745 | .788 | .729 | .752 | .736 |
| N b | 2,747 | 341 | 323 | 448 | 425 | 628 | 507 |
| Perceived neighborhood danger | |||||||
| Cronbach’s α for scale | .812 | .813 | .836 | .824 | .798 | .786 | .814 |
| N b | 2,702 | 336 | 320 | 438 | 424 | 610 | 500 |
Note. aIncludes all age-eligible Wave 2 respondents who were interviewed in their homes.
bIncludes all age-eligible Wave 2 respondents who were interviewed in their homes, returned the leave-behind questionnaire, and had valid data on all items in the scale.
Factor analysis using oblique rotation indicates that the scale has a two-factor structure. The first factor comprises items that are indicative of ambient/environmental conditions: noise, pollution/odors, and traffic (loadings of .89, .67, and .91, respectively). The second factor includes traditional indicators of physical neighborhood disorder: litter and disrepair of the respondent’s building and other buildings on the block (loadings of .57, .94, and .91, respectively). Researchers who wish to examine only one of these sets of neighborhood problems should be mindful that the factors are strongly correlated (interfactor correlation = .45). Therefore, if one is analyzing the unique contribution of one factor to an outcome such as self-rated health, the other factor should be included as in the model to adjust for the covariance between factors.
Measurement variability in neighborhood ratings.
The possibility of between-interviewer variability in the measurement of neighborhood conditions warrants careful consideration. A total of 124 members of NORC’s field staff conducted interviews for Wave 2 of NSHAP, with an average of 27.20 interviews (and range of 1–118 interviews) per interviewer. Recent research has revealed variation in respondents’ and observers’ perceptions of neighborhood disorder (Jones, Pebley, & Sastry, 2011; Sampson & Raudenbush, 2004), so attention to subjectivities in the observation of neighborhood conditions is important. In random intercept models, we find that approximately 24% of the variance in neighborhood density and neighborhood problems is attributable to the interviewer level.
We cannot directly assess interrater reliability in these measures, but the inclusion of coresident partners affords an opportunity to compare two different field interviewers’ ratings of the same neighborhood. Of the 949 coresident partner pairs, 208 (21.92%) had in-home interviews conducted by different field interviewers. Not all of these interviews occurred on the same day, but they did take place within a six-month time frame. Given this, more transient neighborhood conditions such as noise, traffic, pollution, and litter may vary across the two time points, but residential density and the structural conditions of the respondent’s building and other buildings on the block should be relatively durable. Correlations between the ratings of these conditions, given by two different interviewers, are r = .50 for density, r = .53 for the respondent’s building, and r = .37 for other buildings on the block. Although these are moderate in strength (and all are significant at the level of p < .001), they also point to nontrivial variability across interviewers.
There are at least two reasons why neighborhood ratings may vary across interviewers. First, some interviewers may have given higher or lower ratings across all of their respondents. This may reflect systematic differences between interviewers in their tendency to give higher or lower ratings based on their own perceptions of neighborhood conditions, the types of neighborhoods in which they conducted interviews, and the types of neighborhoods where they reside themselves. Related to this is the possibility that the level of variation in neighborhood ratings differs across field interviewers, with some field interviewers recording more extreme differences across respondents’ neighborhoods than other field interviewers. These may also reflect systematic differences in field interviewers’ perceptions or evaluations.
Second, field interviewers’ evaluations of neighborhood conditions may differ according to characteristics of the respondent and his or her local area. That is, interviewers may have tended to rate certain types of neighborhoods or the neighborhoods of certain types of respondents especially positively or negatively. Social distance or status asymmetry between interviewer and respondent may also contribute to systematic variations in neighborhood assessments. Nevertheless, NORC interviewers are highly trained and experienced in carrying out their work as data collectors, which should lessen the degree to which field interviewers’ ratings are clouded by subjectivities or prejudice.
The nonrandom assignment of interviewers makes it difficult to ascertain the source or extent of measurement variability between interviewers. Many interviewers were assigned to contiguous geographic areas, which are likely to have similar neighborhood characteristics. As a result, their mean ratings may be higher or lower than those of other interviewers. Therefore, we cannot determine whether variation in ratings across interviewers reflects systematic differences in evaluations or real characteristics of the neighborhoods they visited. Applying survey adjustments, including clusters, provided with the NSHAP data set should account, in part, for the nonrandom assignment of interviewers.
A variety of other approaches can be used to mitigate between-interviewer differences in neighborhood ratings. First, when considering neighborhood problems as an outcome, incorporating fixed effects for field interviewers would attenuate variation in mean ratings across interviewers. Second, when considering neighborhood density or neighborhood problems as covariates, researchers could standardize, or norm, neighborhood density or neighborhood problems scores within interviewers. This can be achieved by calculating, for each respondent, the deviance of his or her neighborhood score from the mean score given by his or her interviewer. (A comparison of unadjusted and interviewer-normed neighborhood problems ratings is presented in the Results section) Finally, researchers could fit a structural equation model that combines a measurement model for the neighborhood ratings with a substantive model including neighborhood ratings as a covariate.
However, attenuating or eliminating measurement variability between interviewers carries the risk of over-controlling for variation in neighborhood characteristics. Because interviewers were nonrandomly assigned to neighborhoods, reducing variability in the neighborhood ratings between interviewers is also likely to reduce some proportion of variation in the measures that is due to real differences in neighborhood conditions. This may result in underestimation of the effects of neighborhood problems. Further research could exploit the coresident partners in the data set to shed more light on these issues, but such analysis is beyond the scope of this paper.
Respondent Reports of Neighborhood Social Context
Data from the second wave of NSHAP provide a rare opportunity to examine neighborhood social context within a nationally representative sample of older adults who reside in different types of residential areas—including urban, suburban, small town, and rural areas. However, ensuring the validity of self-reported neighborhood measures across urban and nonurban areas presents a challenge. In dense, mixed-use urban areas, landmarks, streets, services, and shared histories often delineate particular geographic spaces as recognizable neighborhoods within which residents perform many of the routine tasks of their daily lives (Sampson et al., 1997, p. 638). But the term “neighborhood” may conjure different meanings for residents of suburban, small town, and rural areas. Nonurban residents may not recognize their local area as a neighborhood, and the spaces of their routine tasks such as shopping and visiting others may extend well beyond their immediate residential area.
For these reasons, NSHAP items assessing the respondent’s neighborhood social context do not refer to the respondent’s “neighborhood.” Instead, respondents are asked to consider their “local area” as “everywhere within a 20-minute walk or within about a mile of your home.” This operationalization builds from recent studies such as the nationally representative HRS and the five-city Multiethnic Study of Artherosclerosis (Mujahid, Diez Roux, Morenoff, & Raghunathan, 2007), which also query respondents about their “local area.” It is also consistent with research on neighborhood context that emphasizes the relevance of ego-centric spaces and walkable areas rather than administrative boundaries like census tracts (e.g., Cagney, Browning, Jackson, & Soller, 2013; Grannis, 1998). Although the neighborhood as traditionally or administratively defined may not perfectly overlap with the space of respondents’ “local areas,” we determined this to be the best approach for capturing the relevant and proximal residential context across urban and nonurban areas. Following common parlance, we refer to our measures as indicators of neighborhood context. Next, we describe the measurement of neighborhood social cohesion, neighborhood social ties, and perceived neighborhood danger.
Neighborhood social cohesion.
The NSHAP Wave 2 LBQ includes the five-item social cohesion index used in the Project on Human Development in Chicago Neighborhoods Community Survey (PHDCN-CS). It is reproduced verbatim, except for the replacement of the PHDCN-CS term “neighborhood” with “local area.” The social cohesion items were introduced as follows: “Please indicate your agreement or disagreement with the following statements about your local area—that is, everywhere within a 20-minute walk or within about a mile of your home.” Full text and descriptive statistics for the items are presented in Table 3.
Table 3.
Mean (and Standard Deviation) for Neighborhood Social Context Scales and Scale Items
| Age-eligible Wave 2 respondentsa | ||
|---|---|---|
| Women | Men | |
| Neighborhood social cohesion scale (item response categories: 1 = strongly agree, 2 = agree, 3 = neither agree nor disagree, 4 = disagree, 5 = strongly disagree) | 3.507 (.576) | 3.464 (.553) |
| This is a close-knit areab | 3.200 (.918) | 3.132 (.925) |
| People around here are willing to help their neighborsb | 3.794 (.816) | 3.763 (.766) |
| People in this area generally don't get along with each other | 3.658 (.888) | 3.620 (.865) |
| People in this area don't share the same values | 3.197 (.871) | 3.128 (.870) |
| People in this area can be trustedb | 3.686 (.797) | 3.679 (.794) |
| Respondents with valid data on all scale items | n = 1,411 | n = 1,280 |
| Neighborhood social ties scale (item response categories: 1 = never, 2 = rarely, 3 = sometimes, 4 = often) | 3.544 (.754) | 3.489 (.678) |
| How often do you and people in this area visit in each other's homes or when you meet on the street? | 3.757 (.946) | 3.672 (.902) |
| How often do you and other people in this area do favors for each other? | 3.908 (.859) | 3.923 (.789) |
| How often do you and other people in this area ask each other for advice about personal things? | 2.968 (.928) | 2.873 (.820) |
| Respondents with valid data on all scale items | n = 1,450 | n = 1,297 |
| Perceived neighborhood danger scale (item response categories: 1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, 5 = strongly agree) | 2.497 (.894) | 2.368 (.935) |
| Many people in this area are afraid to go out at night | 2.578 (.986) | 2.403 (1.002) |
| There are places in this area where everyone knows “trouble” is expected | 2.411 (1.095) | 2.405 (1.149) |
| You're taking a big chance if you walk in this area alone after dark | 2.501 (1.079) | 2.296 (1.117) |
| Respondents with valid data on all scale items | n = 1,417 | n = 1,285 |
Note. Values in bold represent the overall means and standard deviations for the three scales (social cohesion scale, social ties scale, and perceived neighborhood disorder scale).a N’s for each scale exclude respondents who did not return the leave-behind questionnaire or having missing data on at least one scale item.
bItem is reverse coded so that higher values indicate greater neighborhood social cohesion.
We combine these items in a neighborhood social cohesion scale. Scores on the scale are calculated by averaging the values across all five cohesion items (see Echeverría, Diez-Roux, & Link, 2004; Mujahid et al., 2007). Respondents who did not have valid data on all five items are excluded. Using this approach, higher scores indicate the respondent’s perception of greater social cohesion in his or her local area. The social cohesion scale has acceptable internal consistency reliability. Cronbach’s α coefficient is maximized at .68 with the inclusion of all five variables. Item-rest correlations range from .40 to .56.
Table 2 reports Cronbach’s α coefficients for the scale across residential density and respondent gender. As noted previously, we examine men and women separately to ensure that measures of scale reliability are not inflated due to neighborhood concordance within partner dyads. The highest levels of scale reliability are found at lower residential densities—among male and female residents of low-density blocks and female residents of moderate-density blocks. But the social cohesion scale achieves acceptable reliability (i.e., > .60) across male and female residents of low-, moderate-, and high-residential densities.
Previous research using urban samples has found higher levels of internal reliability for this scale, although reliability varies across locations, age groups, and sample sizes. For example, Echeverría and colleagues (2004) found Cronbach’s α of .82 to .86 for these items in a sample of New York City adults; Mujahid et al. (2007) found an α of .74 for four of the items among adults in four urban areas; and Cagney et al. (2009) found α’s of .71 and .76 in clustered samples of older adults in Chicago and Baltimore, respectively. Lower reliability in scales based on older adults’ evaluations of neighborhood cohesion may reflect variations in the extent of neighborhood-based challenges they face, as well as variations in their levels of exposure to or dependence on the neighborhood. Older adults who suffer from health problems or functional limitations, for example, may be particularly challenged by their neighborhood environments (Lawton & Nahemow, 1973).
The neighborhood cohesion scale has a two-factor structure, which is consistent across respondents in low-, moderate-, and high-density areas. Using oblique rotation, we find that the first factor is defined by the items assessing whether the neighborhood is close-knit, whether neighbors help each other, and whether neighbors can be trusted (loadings of .89, .79, and .59, respectively). The second factor is defined by the extent to which neighbors get along and share values (loadings of .84 for both). The interfactor correlation is .36; researchers who wish to examine the contribution of only one of these factors should be mindful of the shared variance across the two factors.
NSHAP respondents are not clustered within neighborhoods, so we are unable to directly assess the reliability of our measures of neighborhood context within neighborhoods; nor can we conduct ecometric analyses to disaggregate the variance in neighborhood measures across neighborhood and individual levels (Raudenbush & Sampson, 1999). However, previous work has established the reliability and validity of respondent-reported measures of neighborhood social context, including neighborhood-level social cohesion (Cagney et al., 2009; Echeverría et al., 2004; Mujahid et al., 2007; Sampson et al., 1997). This research also suggests that a substantial portion of the variance in respondent self-reports of neighborhood cohesion occurs across neighborhoods (Mujahid et al., 2007), which provides support for the notion that the social cohesion scale taps, at least in part, a broader characteristic of the respondent’s local area.
Neighborhood social ties.
The assessment of neighborhood social ties in NSHAP Wave 2 draws from five items that were included in the PHDCN-CS (Sampson et al., 1997; and see Mujahid et al., 2007). From these, we selected three items based on their contributions to the PHDCN-CS scales and our assessment of their theoretical relevance for the NSHAP sample. The items were introduced in the Wave 2 LBQ with the statement: “The following questions ask about your local area—that is, everywhere within a 20-minute walk or within about a mile of your home.” The text of each of the items is reproduced verbatim from the PHDCN-CS, except for substitution of “neighborhood” with “area.” Respondents were asked how often they, and other people in their area, visit with each other, do favors for each other, and ask each other for advice. Full text and summary statistics are presented in Table 3.
Following previous research, we combine these items in a scale indicating neighborhood social ties. Scale scores are calculated by averaging responses for those respondents who have valid data on all three items. Higher scores on the scale indicate greater neighborhood social ties.
The neighborhood social ties scale has good internal consistency reliability. Cronbach’s α coefficient is maximized at .76 with the inclusion of all three items, and item-rest correlations range from .54 to .61. Factor analysis using oblique rotation indicates that all three items have high loadings (.79–.84) on a single factor, which accounts for about 67.33% of the variance in the scale. As shown in Table 2, the scale has good reliability across low-, moderate-, and high-density areas, and across male and female respondents. These α levels are in line with those found in previous research utilizing all five of the PHDCN-CS items within urban samples (i.e., Mujahid et al. [2007] find α = .78 for four of the five items; Sampson and colleagues [1999] find α = .65 for all five items).
As discussed previously, the nature of the NSHAP sample does not permit ecometric analysis of these measures. But previous research with clustered samples finds that a relatively large portion of the variance in the five-item version of the scale stems from individual-level variations in perceiving or reporting neighborhood ties and support (Mujahid et al., 2007; Sampson et al., 1999). Therefore, this scale may tap both a respondent’s sense of connectedness with his or her community and community-level connectedness.
Perceived neighborhood danger.
Three conceptually related items included in the NSHAP Wave 2 LBQ assess the respondent’s perception of danger in his or her neighborhood. These items are drawn from the PHDCN-CS, but they are modified to refer to the respondent’s “area” rather than “neighborhood.” The perceived danger items directly follow the statements about social cohesion, so the introductory statement for those items also applies here. Full text and descriptive statistics for the three items are presented in Table 3.
To calculate scores on the perceived neighborhood danger scale, we reverse code all three items and average them. Respondents who had missing data on any of the items are excluded. Higher scores on the scale indicate greater perceived neighborhood danger. The scale has excellent internal consistency reliability. Cronbach’s α coefficient is maximized at .81, and the item-rest correlations are strong, ranging from .82 to .88. These are consistent with results from the urban sample in the PHDCN-CS, where Cronbach’s α is .81 (Oh & Kim, 2009). As shown in Table 2, scale reliability is very good (from .79 to .84) across male and female respondents who reside on low-, moderate-, and high-density blocks. Factor analysis using oblique rotation indicates that a single factor accounts for 72.70% of the variance in the scale, and loadings on this factor are high (.82–.88) for all three items.
Homeownership and Length of Residence
For many older adults, later life marks the culmination of decades of exposure to a particular residential environment, where they have developed strong ties and a sense of place attachment. Homeownership may further strengthen roots in a particular area and provide opportunities to interact with neighbors. For these reasons, researchers examining neighborhood context should also consider residential tenure and homeownership.
NSHAP assessed homeownership during the in-person interview. Respondents were asked if they (and their partners, if applicable) own or rent their homes. Excluding partner respondents, about 80% (n = 1,945) of the Wave 2 respondents own their homes. An item capturing residential tenure was included in the Wave 2 LBQ. Referring to the respondent’s “local area” as “everywhere within a 20-minute walk or within about a mile of your home,” each respondent was asked: “About how many years have you lived in this area?” Response categories began with “less than one year,” followed by five-year intervals (e.g., 1–5 years, 6–10 years) up to 25 years, and then “26–50 years,” and “more than 50 years.”
Results
In this section, we assess convergent validity of the scales and present descriptive statistics for key measures of neighborhood context collected in Wave 2 of the NSHAP study. Our main goal is not to test hypotheses, but rather to demonstrate how the interviewer assessments of neighborhood problems and the respondents’ reports of neighborhood social context are interrelated—and how these neighborhood characteristics vary across respondents and residential densities.
Convergent Validity of Neighborhood Scales
Previous research suggests that neighborhood physical conditions and neighborhood social context are interrelated. For example, older adults’ sense of neighborhood safety may stem, in part, from neighborhood physical conditions. Neighborhood disorder can promote criminal activity and thereby increase residents’ fear of victimization. At the same time, social disorganization theory suggests that high levels of neighborhood social cohesion, social ties, and informal social control deter deviant behavior, curb neighborhood disorder, and increase perceptions of safety (Cagney & York Cornwell, 2010; Sampson & Raudenbush, 1999; Sampson et al., 1997).
Drawing from this work, we explore pairwise correlations among the neighborhood context scales to examine the scales’ convergent validity (see Table 4). As previously mentioned, we examine male and female respondents separately so that correlations are not affected by concordance within partner dyads. Consistent with social disorganization theory, we find that neighborhood social cohesion is positively associated with neighborhood social ties among both women and men (r = .40 and r = .41, respectively) and negatively associated with neighborhood problems among women and men (r = −.24 and r = −.18, respectively).
Table 4.
Bivariate Correlations of Neighborhood Context Scales, by Gender
| Neighborhood problems | Neighborhood cohesion | Neighborhood ties | Perceived neighborhood danger | |
|---|---|---|---|---|
| Female respondents (n = 1,326)a | ||||
| Neighborhood problems | — | |||
| Neighborhood social cohesion | −.237*** | — | ||
| Neighborhood social ties | −.043 | .395*** | — | |
| Perceived neighborhood danger | .348*** | −.371*** | −.054* | — |
| Male respondents (n = 1,191)a | ||||
| Neighborhood problems | — | |||
| Neighborhood social cohesion | −.181*** | — | ||
| Neighborhood social ties | −.052 | .412*** | — | |
| Perceived neighborhood danger | .344*** | −.291*** | −.003 | — |
Note. aIncludes age-eligible respondents who have valid data on all items in all four scales.
*p < .05. **p < .01. ***p < .001.
Disparities Across Sociodemographic Groups
Table 5 presents weighted means for indicators of neighborhood context across respondents’ age, gender, and racial/ethnic background, as well as results from Wald tests of differences in means across groups. First, comparing women and men, we find no significant gender differences in interviewer-rated block-level density and neighborhood problems. However, women perceive their neighborhoods to be more social cohesive and having more social ties. And, consistent with previous research (e.g., Covington & Taylor, 1991), women perceive their neighborhoods to be more dangerous. Perceived neighborhood danger is also higher among the oldest old women and men—those who are 80–90 years old—compared with women and men ages 62–69. We find few other notable differences across age groups.
Table 5.
Estimated Scores for Measures of Neighborhood Context in National Social Life, Health, and Aging Project Wave 2, by Respondent Gender, Age, and Race/Ethnicity
| Residential density | Neighborhood problems (unadjusted) | Neighborhood problems (normed)a | Neighborhood cohesion | Neighborhood ties | Perceived neighborhood danger | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | |
| Female respondents | 3.215 | (.076) | −.074 | (031) | −.048 | (.032) | 3.535 | (.025) | 3.584 | (.025) | 2.452 | (.037) |
| Age group | ||||||||||||
| 62–69 (ref.) | 3.140 | (.100) | −.102 | (.040) | −.080 | (.049) | 3.520 | (.042) | 3.545 | (.038) | 2.346 | (.053) |
| 70–79 | 3.289 | (.090) | −.053 | (.043) | −.037 | (.042) | 3.555 | (.046) | 3.676* | (.038) | 2.520* | (.056) |
| 80–90 | 3.244 | (.101) | −.050 | (.047) | −.001 | (.064) | 3.533 | (.047) | 3.500 | (.049) | 2.572** | (.054) |
| N | 1,638 | 1,609 | 1,609 | 1,411 | 1,450 | 1,417 | ||||||
| Race/ethnicityb | ||||||||||||
| White, non- Hispanic (ref.) | 3.146 | (.085) | −.169 | (.033) | −.141 | (.039) | 3.569 | (.028) | 3.629 | (.027) | 2.373 | (.036) |
| Black, non-Hispanic | 3.750*** | (.144) | .373*** | (.071) | .473*** | (.116) | 3.331*** | (.058) | 3.411* | (.096) | 2.937*** | (.068) |
| Hispanic | 3.372 | (.145) | .492*** | (.132) | .327** | (.147) | 3.360** | (.065) | 3.373* | (.090) | 2.853*** | (.120) |
| N | 1,597 | 1,569 | 1,569 | 1,375 | 1,410 | 1,383 | ||||||
| Male respondentsc | 3.154 | (.081) | −.065 | (.037) | −.047 | (.039) | 3.465** | (.017) | 3.499* | (.021) | 2.304*** | (.037) |
| Age group | ||||||||||||
| 62–69 (ref.) | 3.103 | (.112) | −.076 | (.054) | −.018 | (.055) | 3.432 | (.034) | 3.490 | (.038) | 2.225 | (.056) |
| 70–79 | 3.195 | (.074) | −.054 | (.041) | −.064 | (.055) | 3.485 | (.025) | 3.499 | (.038) | 2.289 | (.049) |
| 80–90 | 3.193 | (.114) | −.061 | (.051) | −.082 | (.070) | 3.504 | (.036) | 3.522 | (.052) | 2.530** | (.081) |
| N | 1,448 | 1,422 | 1,422 | 1,280 | 1,297 | 1,285 | ||||||
| Race/ethnicityb | ||||||||||||
| White, non- Hispanic (ref.) | 3.065 | (.088) | −.187 | (.035) | −.164 | (.038) | 3.477 | (.020) | 3.492 | (.022) | 2.206 | (.038) |
| Black, non-Hispanic | 3.497** | (.142) | .340*** | (.098) | .509*** | (.116) | 3.398 | (.045) | 3.462 | (.077) | 3.005*** | (.100) |
| Hispanic | 3.624** | (.166) | .524*** | (.118) | .211*** | (.083) | 3.478 | (.062) | 3.628 | (.091) | 2.679** | (.165) |
| N | 1,407 | 1,382 | 1,382 | 1,245 | 1,262 | 1,250 | ||||||
Note. SE = standard error.
Estimates are based on age-eligible respondents who have valid data on each scale, and are survey-adjusted and weighted to account for the probability of selection, with poststratification adjustments for nonresponse. Values in bold show the overall means (and standard errors) for female and male respondents.
aInterviewer-normed neighborhood problems ratings are calculated by subtracting the respondent’s interviewer’s overall mean problems rating from the respondent’s neighborhood problems score, and then dividing by the standard deviation of the respondent's interviewer’s neighborhood problems ratings.
bRespondents who identified their race as American Indian, Alaskan Native, Asian or Pacific Islander, or Other are excluded.
cSignificance is based on Wald tests of the difference between mean scores for male and female respondents.
*p < .05. **p < .01.***p < .001 (two-tailed; based on Wald tests of differences in means).
Turning to differences across racial/ethnic groups, we find that Black and Hispanic older adults reside on more densely populated and disordered blocks than White older adults. Racial/ethnic disparities in neighborhood problems are particularly striking. Mean ratings of neighborhood problems are more than 0.50 higher for Black men and women compared with White men and women, and the differences are even larger when we compare Hispanic and White older adults (differences of 0.66 among women and 0.71 among men). These disparities do not substantially differ in the interviewer-normed version of the neighborhood problems scale, although the magnitude of the Black–White differences is larger in the normed ratings. Compared with White women, Black and Hispanic women report significantly lower levels of neighborhood social cohesion and fewer neighborhood social ties in their neighborhoods. Finally, Black and Hispanic older adults perceive more danger in their neighborhoods than White older adults.
Neighborhood Context and Residential Density
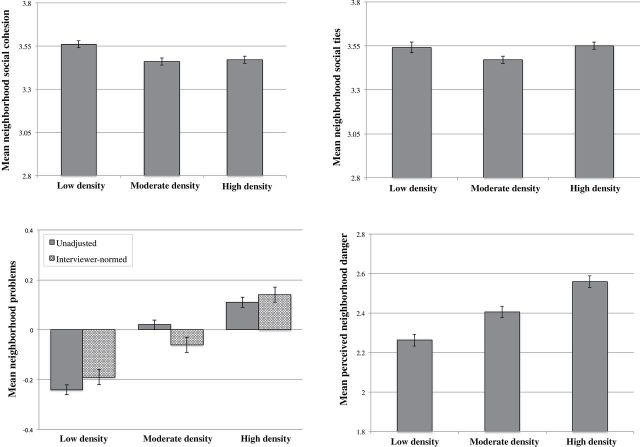
Figure 1 presents mean scores on the neighborhood scales across low-, moderate-, and high-density blocks. Means for neighborhood social cohesion and social ties are presented in the upper panel. Respondents who live on low-density blocks report greater neighborhood social cohesion (3.56) compared with those who live on moderate- and high-density blocks (3.46 and 3.47, respectively). However, ratings of neighborhood social ties are lowest among those who reside on moderate-density blocks (3.47, compared with 3.54 for low-density blocks and 3.55 for high-density blocks).
Figure 1.
Mean neighborhood context ratings, by residential density. Calculations are based on unweighted means and include age-eligible respondents who were interviewed in their homes and have valid data on each scale: for neighborhood problems, n = 3,028; for neighborhood social cohesion, n = 2,616; for neighborhood social ties, n = 2,672; and for perceived neighborhood danger, n = 2,628.
The bottom left panel of Figure 1 presents unadjusted and interviewer-normed means for neighborhood problems across block-level density. Although there are small differences in the means for unadjusted and interviewer-normed ratings, the general pattern is consistent across both operationalizations of the scale—neighborhood problems increase with residential density. The bottom right panel shows that perceived neighborhood danger also has a linear and positive relationship with block-level density, ranging from an average score of 2.26 for residents of low-density blocks to a score of 2.56 for those who reside on high-density blocks.
Discussion
NSHAP Wave 2 made important progress in assessing both neighborhood physical conditions and neighborhood social context within a nationally representative sample of community-residing older adults. Field interviewer ratings of neighborhood problems compose a scale that has good reliability and expected associations with neighborhood social context. Respondent reports of neighborhood social cohesion, neighborhood social ties, and perceived neighborhood danger also form scales with good reliability and validity.
Our descriptive analyses of the measures point to several directions for further research on neighborhood context and health and well-being in later life. First, we observe variations in neighborhood physical conditions and social context across sociodemographic groups, which may contribute to persistent disparities in health and well-being. For example, Black and Hispanic older adults reside on blocks with more neighborhood problems, and they report less cohesion, fewer ties, and more perceived danger in their local areas. The collection of biomeasures of health and function in NSHAP will allow researchers to explore new hypotheses about how neighborhood conditions are associated with prodromal health changes and physiological processes. This may help to pinpoint community-level interventions that could promote older adults’ independence and reduce racial disparities in trajectories of aging.
Second, respondent assessments of neighborhood social context suggest that older men and women may differentially evaluate and experience their neighborhood contexts. We find, for example, that older women perceive their neighborhoods to be not only more socially cohesive and connected but also more dangerous. The NSHAP Wave 2 data will allow researchers to assess whether and how the relationship between neighborhood context and health is conditioned by gender. In particular, the NSHAP Wave 2 partner sample provides a rare opportunity to examine within-couple differences in evaluations of neighborhood conditions. Given that both members of a given coresident partner dyad reside on the same block, researchers can explore how perceptions of the neighborhood differ within partner dyads, and the extent to which these differences in perceptions are associated with health and well-being.
Third, the relatively low levels of neighborhood cohesion and neighborhood social ties observed among respondents who reside on moderate-density blocks are particularly intriguing. Additional research using these data should unpack how neighborhood physical conditions and neighborhood social contexts provide resources or challenges for older adults residing in urban and nonurban areas. This is an important issue because the proportion of older adults in suburban settings is growing (Frey, 2003), and neighborhood social cohesion and support may be critical factors enabling older adults to continue to reside independently.
The interviewer assessments of block-level density capture the presence of other residences and/or businesses in close proximity to the respondent’s housing unit. This may be indicative of the propinquity of support (e.g., from neighbors) or access to amenities like grocery stores, and it provides a basis for the interviewer’s assessments of neighborhood problems such as building disrepair, litter, and noise. However, block-level density does not necessarily reflect urban, suburban, or rural residence. And, respondents’ assessments of their neighborhood social context are based on their local area, which will typically extend beyond their block. At this time, we are not able to consider variations in neighborhood context across higher-level indicators of urbanicity. Variables such as region, urbanicity, and size of place are not currently available with the NSHAP public use data, but may be incorporated in a later release.
In addition, researchers using these data should be aware of a number of limitations and complexities stemming from the NSHAP sample design. First, the location of the neighborhood social context measures on the LBQ leads to missing data on these variables for respondents who did not return the questionnaire, and respondents who were interviewed at a location other than their own homes have missing data on the field interviewer ratings of neighborhood conditions. The exclusion of respondents with missing data on neighborhood characteristics may introduce bias in analyses to the extent that the likelihood of having an out-of-home interview or not returning the LBQ is associated with other variables of interest, such as respondent or neighborhood characteristics. If so, imputing values for neighborhood characteristics or employing a model that accounts for sample selection (see Winship & Mare, 1992) may help to attenuate bias caused by missing data on neighborhood context.
Second, similarities in partners’ evaluations of their neighborhoods may lead to underestimation of standard errors. To avoid this, we recommend conducting gender-stratified analyses as we have here, or employing design-based standard errors (e.g., using the cluster variable provided with the Wave 2 data).
Finally, field interviewer ratings of neighborhood problems may include unobserved heterogeneity at the interviewer level due to differences in the observation or perception of neighborhood features. A detailed discussion of the potential sources of heterogeneity in ratings was provided in the Methods. As described in Methods, we recommend that researchers using the neighborhood problems scale evaluate the robustness of their results across a variety of operationalizations and model specifications.
Despite these limitations, the second wave of NSHAP provides an unprecedented opportunity to examine the physical conditions and social contexts of the neighborhoods of older Americans. Growing share of older adults are aging in their communities, and the characteristics of their residential environments may vary widely. Descriptive statistics presented in this study reveal disparities in neighborhood physical conditions and neighborhood social context across older adults’ gender and race/ethnicity. The patterns observed in this study suggest the need for further research on how variations in neighborhood physical conditions and social context inside and outside of the city shape trajectories of health and well-being among older adults.
Key Points .
NSHAP Wave 2 collected interviewer assessments of respondents’ neighborhood physical conditions and respondent reports of neighborhood social context.
These measures provide an opportunity to examine associations between neighborhood context and health among older adults in urban and nonurban areas.
Scales measuring neighborhood problems, social cohesion, social ties, and perceived danger have good reliability and convergent validity.
Neighborhood physical conditions and social context vary across residential densities, with lowest levels of neighborhood social cohesion and social ties among respondents who reside on moderate-density blocks
Variations in neighborhood context across sociodemographic groups may contribute to health disparities among older adults.
Funding
The National Social Life, Health, and Aging Project is supported by the National Institutes of Health, including the National Institute on Aging (R37AG030481; R01AG033903), the Office of Women’s Health Research, the Office of AIDS Research, and the Office of Behavioral and Social Sciences Research (R01AG021487), and by NORC which was responsible for the data collection.
Acknowledgments
We are grateful for comments during the development of this paper from Rachel Behler, Lea Bromell, Benjamin Cornwell, Ned English, Louise Hawkley, Mark Hayward, James Iveniuk, Juyeon Kim, Katie O’Doherty, Colm O’Muircheartaigh, Phil Schumm, and Linda Waite. We also thank Charna Albert, Alex Currit, Jennifer Hanis-Martin, Evan Hernandez, and Katherine Morris for their assistance with the preparation of this manuscript.
E. York Cornwell planned the study including instrumentation, performed the statistical analysis, and wrote the paper. K. A. Cagney planned the study including instrumentation, contributed to the statistical analysis, and revised the paper.
References
- Barker J. C. (2002). Neighbors, friends, and other nonkin caregivers of community-living dependent elders. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57, 158–167. 10.1093/geronb/57.3.S158 [DOI] [PubMed] [Google Scholar]
- Beard J. R., Cerdá M., Blaney S., Ahern J., Vlahov D., Galea S. (2009). Neighborhood characteristics and change in depressive symptoms among older residents of New York City. American Journal of Public Health, 99, 1308–1314. 10.2105/AJPH.2007.125104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagney K. A., Browning C. R., Jackson A. L., Soller B. (2013). Networks, neighborhoods, and institutions: An integrated ‘activity space’ approach to research on aging. In Waite L. (Ed.), New directions in the sociology of aging (pp. 60–80). Washington, DC: National Academies Press. [Google Scholar]
- Cagney K. A., Glass T. A., Skarupski K. A., Barnes L. L., Schwartz B. S., Mendes de Leon C. F. (2009). Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64, 415–424. 10.1093/geronb/gbn041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagney K. A., York Cornwell E. (2010). Neighborhoods and health in later life: The intersection of biology and community. Annual Review of Gerontology and Geriatrics, 30, 323–348. 10.1891/0198-8794.30.323 [Google Scholar]
- Cannuscio C., Block J., Kawachi I. (2003). Social capital and successful aging: The role of senior housing. Annals of Internal Medicine, 139, 395–399. 10.7326/0003-4819-139-5_Part_2-200309021-00003 [DOI] [PubMed] [Google Scholar]
- Clarke P., Ailshire J. A., Bader M., Morenoff J. D., House J. S. (2008). Mobility disability and the urban built environment. American Journal of Epidemiology, 168, 506–513. 10.1093/aje/kwn185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covington J., Taylor R. B. (1991). Fear of crime in urban residential neighborhoods. Sociological Quarterly, 32, 231–249. 10.1111/j.1533–8525.1991.tb00355.x [Google Scholar]
- Diez Roux A. V., Mair C. (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125–145. 10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]
- Echeverría S. E., Diez-Roux A. V., Link B. G. (2004). Reliability of self-reported neighborhood characteristics. Journal of Urban Health, 81, 682–701. 10.1093/jurban/jth151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echeverría S., Diez-Roux A. V., Shea S., Borrell L. N., Jackson S. (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The Multi-Ethnic Study of Atherosclerosis. Health & Place, 14, 853–865. 10.1016/j.healthplace.2008.01.004 [DOI] [PubMed] [Google Scholar]
- Frey W. H. (2003). Boomers and seniors in the suburbs: Aging patterns in census 2000. Washington, DC: The Brookings Institution. [Google Scholar]
- Grannis R. (1998). The importance of trivial streets: Pedestrian street networks and geographic patterns of residential segregation. American Journal of Sociology, 103, 1530–1564. 10.1086/231400 [Google Scholar]
- Hill T. D., Ross C. E., Angel R. J. (2005). Neighborhood disorder, psychophysiological distress, and health. Journal of Health and Social Behavior, 46, 170–186. 10.1177/002214650504600204 [DOI] [PubMed] [Google Scholar]
- Jacobs J. (1961). The death and life of great American cities. New York, NY: Vintage Books. [Google Scholar]
- Jones M., Pebley A. R., Sastry N. (2011). Eyes on the block: Measuring urban physical disorder through in-person observation. Social Science Research, 40, 523–537. 10.1016/j.ssresearch.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L. F. (2000). Social cohesion, social capital, and health. In Berkman L. F., Kawachi I. (Eds.), Social epidemiology. New York, NY: Oxford University Press. [Google Scholar]
- Kim J. (2010). Neighborhood disadvantage and mental health: The role of neighborhood disorder and social relationships. Social Science Research, 39, 260–271. 10.1016/j.ssresearch.2009.08.007 [Google Scholar]
- Klinenberg E. (2002). Heat wave: A social autopsy of disaster in Chicago. Chicago, IL: University of Chicago Press. 10.7208/chicago/9780226026718.001.0001 [DOI] [PubMed] [Google Scholar]
- Krause N. (1993). Neighborhood deterioration and social isolation in later life. International Journal of Aging and Human Development, 36, 9–38. 10.2190/UBR2-JW3W-LJEL-J1Y5 [DOI] [PubMed] [Google Scholar]
- Latkin C. A., Curry A. D. (2003). Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior, 44, 34–44. 10.2307/1519814 [PubMed] [Google Scholar]
- Lawton M. P., Nahemow L. (1973). Ecology and the aging process. In Eisdorfer C., Lawton M. P. (Eds.), Psychology of adult development and aging (pp. 619–674). Washington, DC: American Psychological Association. 10.1037/10044-020 [Google Scholar]
- Liska A. E., Sanchirico A., Reed M. D. (1988). Fear of crime and constrained behavior: Specifying and estimating a reciprocal effects model. Social Forces, 66, 827–837. 10.1093/sf/66.3.827 [Google Scholar]
- Mair C., Diez Roux A. V., Morenoff J. D. (2010). Neighborhood stressors and social support as predictors of depressive symptoms in the Chicago community adult health study. Health & Place, 16, 811–819. 10.1016/j.healthplace.2010.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon C. F., Cagney K. A., Bienias J. L., Barnes L. L., Skarupski K. A., Scherr P. A., Evans D. A. (2009). Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults: A multilevel analysis. Journal of Aging and Health, 21, 155–171. 10.1177/0898264308328650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner S., Logan J. R., Spitze G. (1993). Predicting the frequency of senior center attendance. The Gerontologist, 33, 650–657. 10.1093/geront/33.5.650 [DOI] [PubMed] [Google Scholar]
- Moss M. S., Lawton M. P. (1982). Time budgets of older people: A window on four lifestyles. Journal of Gerontology, 37, 115–123. 10.1093/geronj/37.1.115 [DOI] [PubMed] [Google Scholar]
- Mujahid M. S., Diez Roux A. V., Morenoff J. D., Raghunathan T. (2007). Assessing the measurement properties of neighborhood scales: From psychometrics to ecometrics. American Journal of Epidemiology, 165, 858–867. 10.1093/aje/kwm040 [DOI] [PubMed] [Google Scholar]
- O’Muircheartaigh C., Eckman S., Smith S. (2009). Statistical design and estimation for the National Social Life, Health, and Aging Project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64, 12–19. 10.1093/geronb/gbp045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh J., Kim S. (2009). Aging, neighborhood attachment, and fear of crime: Testing reciprocal effects. Journal of Community Psychology, 37, 21–40. 10.1002/jcop.20269 [Google Scholar]
- Raudenbush S. W., Sampson R. J. (1999). Ecometrics: Toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociological Methodology, 29, 1–41. 10.1111/0081-1750.00059 [Google Scholar]
- Robert S. A., Li L. W. (2001). Age variation in the relationship between community socioeconomic status and adult health. Research on Aging, 23, 233–258. 10.1177/0164027501232005 [Google Scholar]
- Ross C. E., Mirowsky J.(1999). Disorder and decay: The concept and measurement of perceived neighborhood disorder. Urban Affairs Review, 34, 412–432. 10.1177/10780879922184004 [Google Scholar]
- Ross C. E., Mirowsky J. (2001). Neighborhood disadvantage, disorder, and health. Journal of Health and Social Behavior, 42, 258–276. 10.2307/3090214 [PubMed] [Google Scholar]
- Sampson R. J., Raudenbush S. W. (1999). Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology, 105, 603–651. 10.1086/210356 [Google Scholar]
- Sampson R. J., Raudenbush S. W. (2004). Seeing disorder: Neighborhood stigma and the social construction of ‘Broken Windows.’ American Journal of Sociology, 105, 603–651. 10.1177/019027250406700401 [Google Scholar]
- Sampson R. J., Morenoff J. D., Earls F. (1999). Beyond social capital: Spatial dynamics of collective efficacy for children. American Sociological Review, 64, 633–660. 10.2307/2657367 [Google Scholar]
- Sampson R. J., Raudenbush S. W., Earls F. (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277, 918–924. 10.1126/science.277.5328.918 [DOI] [PubMed] [Google Scholar]
- Schroder-Butterfill E., Marianti R. (2006). A framework for understanding old-age vulnerabilities. Ageing & Society, 26, 9–35. 10.1017/S0144686X05004423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw B. A. (2005). Anticipated support from neighbors and physical functioning during later life. Research on Aging, 27, 503–525. 10.1177/0164027505277884 [Google Scholar]
- Shaw C., McKay H. (1942). Juvenile delinquency and urban areas. Chicago, IL: University of Chicago Press.
- Stafford M., Chandola T., Marmot M. (2007). Association between fear of crime and mental health and physical functioning. American Journal of Public Health, 97, 2076–2081. 10.2105/AJPH.2006.097154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A., Feldman P. J. (2001). Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and association with socioeconomic status and health. Annals of Behavioral Medicine, 23, 177–185. 10.1207/S15324796ABM2303_5 [DOI] [PubMed] [Google Scholar]
- Taylor J., Eitle D., Russell D. (2009). Racial/ethnic variation in the relationship between physical limitations and fear of crime: An examination of mediating and moderating factors. Deviant Behavior, 30, 144–174. 10.1080/01639620802050213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M., Browning C. R., Cagney K. A. (2003). Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Social Science & Medicine, 57, 843–860. 10.1016/S0277-9536(02)00457-4 [DOI] [PubMed] [Google Scholar]
- Wen M., Cagney K. A., Christakis N. (2005). Effect of specific aspects of community social environment on the mortality of individuals diagnosed with serious illness. Social Science & Medicine, 61, 1119–1134. 10.1016/j.socscimed.2005.01.026 [DOI] [PubMed] [Google Scholar]
- Wethington E., Kavey A. (2000). Neighboring as a form of social integration and support. In Pillemer K., Moen P., Wethington E., Glasgow N. (Eds.), Social integration in the second half of life (pp. 190–210). Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Winship C., Mare R. D. (1992). Models for sample selection bias. Annual Review of Sociology, 18, 327–350. 10.1146/annurev.so.18.080192.001551 [Google Scholar]
- Yen I. H., Michael Y. L., Perdue L. (2009). Neighborhood environment in studies of health of older adults: A systematic review. American Journal of Preventative Medicine, 37, 455–463. 10.1016/j.amepre.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- York Cornwell E.(in press). Social resources and disordered living conditions: Evidence from a national sample of community-residing older adults. Research on Aging. 10.1177/0164027513497369 [DOI] [PMC free article] [PubMed] [Google Scholar]