Abstract
Objective
Disparities in unintended pregnancy in the United States are related, in part, to black and Hispanic women being overall less likely to use effective contraceptive methods. However, the fact that these same groups are more likely to use female sterilization, a highly effective method, suggests there may be variability in disparities in contraceptive use across a woman’s life course. We sought to assess the relationship between race/ethnicity and contraceptive use in a nationally representative sample and to approximate a life-course perspective by examining effect modification on these disparities by women’s age, parity and history of unintended pregnancy.
Study Design
We conducted an analysis of the 2006–2010 National Survey of Family Growth to determine the association between race/ethnicity and 1) use of any method; 2) use of a highly or moderately effective method among women using contraception; and 3) use of a highly effective method among women using contraception. We then performed analyses to assess interactions between race/ethnicity and age, parity and history of unintended pregnancy (ies).
Results
Our sample included 7,214 women aged 15–44. Compared to whites, blacks were less likely to use any contraceptive method (AOR: 0.65); and blacks and Hispanics were less likely to use a highly or moderately effective method (AORs: 0.49 and 0.57, respectively). Interaction analyses revealed that racial/ethnic disparities in contraceptive use varied by women’s age, with younger women having more prominent disparities.
Conclusions
Interventions designed to address disparities in unintended pregnancy should focus on improving contraceptive use among younger women.
Keywords: Contraception, disparities, race/ethnicity
Introduction
Nearly half of all pregnancies in the United States are unintended.1 There are prominent racial and ethnic disparities in unintended pregnancy rates, with black and Hispanic women having a significantly higher rate of unintended pregnancy than white women.1,2 Unintended pregnancy is directly related to use of contraception as well as to the type of contraceptive method used, with hormonal methods being superior to barrier methods for pregnancy prevention and sterilization, intrauterine devices (IUDs), and implants being the most effective.3,4
Black women have been found to have higher rates of contraceptive non-use than whites in analyses using a variety of datasets,5–8 and similarly both blacks and Hispanics have been found to be more likely than white women to use condoms, a lower efficacy method.7,9,10 While this suggests that racial/ethnic differences in contraceptive patterns may underlie differences in unintended pregnancies, cross-sectional studies have also found a countervailing trend, in that female sterilization, a highly effective method, is used more commonly as a contraceptive method by black and Hispanic women.7,11 As sterilization is used more often by older women7 and by those who have completed childbearing, while younger women and women with lower parity are more likely to use condoms or no method at all,7 these trends raise the question of whether racial/ethnic disparities in use of contraception vary over women’s life course. Understanding how racial/ethnic differences in overall contraceptive use, as well as in the type of method used, vary across age and reproductive experiences may provide insight into factors that shape contraceptive behavior. In addition, this understanding can help to guide interventions designed to address disparities in contraceptive use and, ultimately, unintended pregnancy through identifying which women are at highest risk.
We used data from the 2006–2010 cycle of the National Survey of Family Growth (NSFG) to analyze patterns of contraceptive use by race/ethnicity with regard to both overall use and the effectiveness of the method used, as well as to assess how the relationship between race/ethnicity and contraceptive use was modified by age and reproductive experiences.
Materials and Methods
Study design
We conducted a secondary analysis of cross-sectional data collected in the 2006–2010 NSFG. The NSFG is conducted by the National Center for Health Statistics, an agency of the US Department of Health and Human Services. The purpose of the survey is to provide nationally representative data on factors affecting men's and women's reproductive health.
Study sample
The NSFG uses a national probability sample designed to represent men and women aged 15–44 in the household population of all 50 states and the District of Columbia. For the 2006–2010 NSFG, face-to-face interviews were conducted between June 2006 and June 2010. Blacks, Hispanics, and individuals aged 15–24 were oversampled; the overall response rate was 77%. A more complete description of the sampling methods for 2006–2010 cycle of the NSFG is described elsewhere.12
The study population for the 2006–2010 NSFG included 12,279 women and 10,403 men for a total sample size of 22,692. For this analysis, we included only data from women participants who were at risk for unintended pregnancy. Women were considered at risk for unintended pregnancy if they had had sexual intercourse with a man in the 3 months prior to interview and were not pregnant, trying to get pregnant, or postpartum at the time of interview. We excluded women who reported that they or their partners were infertile as well as women who were using contraception in the 3 months prior to the interview but were not sexually active during that period.
Study variables
We sought to examine the relationship between race/ethnicity and current use of any contraceptive method (defined as use in the month of the interview) as well as type of method (categorized by clinical effectiveness). The effectiveness of contraceptive methods were categorized based on the World Health Organization recommendations.13 Accordingly, we considered barrier methods (i.e., condoms, diaphragms/sponges, spermicides) to be “less effective” and hormonal methods (pills, patch, ring, and injectables) to be “moderately effective.” Intrauterine devices (IUDs), implants, and male or female sterilization were considered to be “highly effective.” For the main analysis, withdrawal and natural family planning methods were considered as “no method”, due to our desire to focus on the use or non-use of modern contraceptive methods. Women who reported using emergency contraception alone (n=8) were also classified as not using a method, as this form of pregnancy prevention is not designed for on-going use. If a woman reported more than one type of method in the month of interview, we used the most effective method for our analysis. We examined several contraceptive use outcomes, including: 1) use of any method; 2) use of a highly or moderately effective method among women using contraception; and 3) use of a highly effective method among women using contraception.
The key independent variable of interest was self-reported race/ethnicity. Insurance status, income, education level, marital status, and religion were included as control variables. Age, parity, and history of unintended pregnancy (either “unwanted” or occurring “too soon”)11 were examined in more detail as potential moderators of the associations between race/ethnicity and contraceptive use.
Statistical Analysis
We examined socio-demographic characteristics of the study sample by effectiveness of their reported current contraceptive method (no method, less effective, moderately effective, and highly effective) using chi-square analysis. We then conducted multivariate logistic regression analyses, in which we controlled for all covariates for each of our three outcomes. We tested for interactions between race/ethnicity and each of three potential effect modifiers (age, parity, and history of unintended pregnancy). Given the potential for collinearity between our proposed effect modifiers, for outcomes in which more than one interaction was identified, we examined the relative importance of these interactions by constructing a model in which all significant interactions were included. Those interaction terms with a p value of <0.1 in these combined models were considered to be significant interactions. We then conducted stratified analyses for those variables that demonstrated significant interactions including all other covariates.
As history of abortion is known to be underreported in the NSFG,14 we did not include this in the primary model, but performed a sensitivity analysis to determine whether inclusion of this variable affected the association of other covariates with the outcomes in the multivariate models. We also performed a second sensitivity analysis in which we included natural family planning methods, withdrawal and emergency contraception as less effective methods.
Statistical analyses for this project were conducted using SAS software (version 9.2, SAS Institute Inc., Cary, NC), utilizing appropriate modifications for the NSFG’s complex sample design. All percentages shown have been weighted to reflect national estimates. This study was approved by the University of Pittsburgh Institutional Review Board.
Results
Sample
Table 1 presents the characteristics of the sample by race/ethnicity. Consistent with the representative sampling, there were no significant differences between race/ethnic groups by age. Across all other sociodemographic characteristics, there were significant racial/ethnic differences, including Hispanic and black women having lower income and educational achievement and higher incidence of prior unintended pregnancy (ies).
Table 1.
Characteristics of Sample, by Race/Ethnicity
| Overall (N=7214) |
White (n=3755) |
Hispanic (n=1589) |
Black (n=1326) |
Other (n=544) |
|||
|---|---|---|---|---|---|---|---|
| Socio-demographic characteristic |
Category | N (%) | n (%) | n (%) | n (%) | n (%) | p value χ2 |
| Age | 15–19 | 679 (8) | 358 (7) | 143 (8) | 125 (9) | 53 (9) | 0.1899 |
| 20–29 | 2841 (35) | 1408 (34) | 629 (36) | 572 (39) | 232 (35) | ||
| 30–39 | 2595 (38) | 1342 (38) | 621 (40) | 450 (34) | 182 (36) | ||
| 40–44 | 1099 (20) | 647 (21) | 196 (17) | 179 (18) | 77 (20) | ||
| Income | < 100 poverty level | 1775 (19) | 610 (13) | 521 (32) | 521 (35) | 123 (19) | <.0001 |
| 100–299 poverty level | 3082 (42) | 1527 (40) | 765 (49) | 556 (43) | 234 (44) | ||
| >299 poverty level | 2357 (38) | 1618 (47) | 303 (19) | 249 (22) | 187 (37) | ||
| Education | HS diploma or less | 3447 (44) | 1449 (37) | 1032 (66) | 763 (56) | 203 (31) | <.0001 |
| Some college | 3767 (56) | 2306 (63) | 557 (34) | 563 (44) | 341 (69) | ||
| Insurance Status | Private | 4095 (64) | 2573 (73) | 654 (41) | 561 (48) | 307 (60) | <.0001 |
| Public/None | 3119 (36) | 1182 (27) | 935 (59) | 765 (52) | 237 (40) | ||
| Marital Status | Ever been married | 3971 (65) | 2312 (69) | 906 (63) | 469 (46) | 284 (60) | <.0001 |
| Never been married | 3243 (35) | 1443 (31) | 683 (37) | 857 (54) | 260 (40) | ||
| Religion | None | 1470 (19) | 952 (22) | 245 (13) | 160 (11) | 113 (19) | <.0001 |
| Catholic | 1856 (25) | 743 (19) | 933 (59) | 68 (6) | 112 (22) | ||
| Protestant | 3327 (48) | 1709 (50) | 357 (23) | 1057 (79) | 204 (36) | ||
| Other | 561 (9) | 351 (9) | 54 (4) | 41 (4) | 115 (23) | ||
| Parity | 0 | 2466 (32) | 1525 (36) | 373 (22) | 337 (25) | 231 (36) | <.0001 |
| 1 | 1372 (17) | 685 (17) | 299 (16) | 298 (21) | 90 (17) | ||
| 2 | 1765 (27) | 940 (28) | 383 (23) | 331 (27) | 111 (23) | ||
| 3+ | 1611 (24) | 605 (19) | 534 (40) | 360 (28) | 112 (24) | ||
| Unintended Pregnancies | 0 | 3525 (51) | 2139 (56) | 674 (42) | 420 (32) | 292 (52) | <.0001 |
| 1 | 1814 (26) | 908 (25) | 449 (28) | 333 (25) | 124 (26) | ||
| 2 | 992 (13) | 423 (12) | 259 (16) | 256 (19) | 54 (9) | ||
| 3+ | 883 (11) | 285 (7) | 207 (14) | 317 (23) | 74 (13) | ||
| Ever had an Abortion | No | 6074 (85) | 3243 (87) | 1370 (87) | 992 (77) | 469 (86) | <.0001 |
| Yes | 1140 (15) | 512 (13) | 219 (13) | 334 (23) | 75 (14) |
Bivariate Results
In bivariate analyses of contraceptive use (Table 2), 18% of all women reported using no method, 16% used a less effective method, 28% used a moderately effective method, and 37% used a highly effective method. The distribution of contraceptive use varied significantly by race/ethnicity (p<0.001), with both Hispanics and blacks being more likely than white women to report no method use (19% and 24% vs. 16%, respectively). In addition, these same groups were more likely to use a less effective method (18% and 18% vs. 14%), and, therefore, less likely to use a moderately or highly effective method (64% and 58% vs. 70%). Among all women using highly effective methods, 85% relied on sterilization and 15% reported IUD or implant use, and there were no racial/ethnic differences in the distribution of these highly effective methods (data not shown). However, white women were more likely to rely on male sterilization and less likely to rely on female sterilization, when compared to Hispanic and black women (p<0.001). Other demographic variables that were associated with use of contraception included age, income, education, insurance, marital status, religion, parity, as well as history of either unintended pregnancy or having had an abortion.
Table 2.
Percent of women using each category of contraceptive method*
| Socio-demographic characteristic |
Category | No method (n=1405) |
Less effective method (n=1321) |
Moderately effective method (n=2080) |
Highly effective method (n=2408) |
p value |
|---|---|---|---|---|---|---|
| All women | 18 | 16 | 28 | 37 | ||
| Race/Ethnicity | White | 16 | 14 | 31 | 39 | <.0001 |
| Hispanic | 19 | 18 | 25 | 39 | ||
| Black | 24 | 18 | 24 | 34 | ||
| Other | 26 | 25 | 22 | 27 | ||
| Age | 15–19 | 32 | 21 | 44 | 3 | <.0001 |
| 20–29 | 19 | 22 | 42 | 17 | ||
| 30–39 | 17 | 14 | 21 | 48 | ||
| 40–44 | 15 | 10 | 10 | 65 | ||
| Income | < 100 poverty level | 21 | 15 | 26 | 39 | <.0001 |
| 100–299 poverty level | 19 | 17 | 25 | 39 | ||
| > 299 poverty level | 16 | 16 | 33 | 34 | ||
| Education | HS diploma or less | 21 | 14 | 23 | 43 | <.0001 |
| Some college | 16 | 18 | 32 | 33 | ||
| Insurance Status | Private | 16 | 16 | 31 | 37 | <.0001 |
| Public/None | 22 | 17 | 23 | 38 | ||
| Marital Status | Ever been married | 15 | 14 | 21 | 50 | <.0001 |
| Never been married | 24 | 21 | 42 | 14 | ||
| Religion | None | 21 | 16 | 30 | 33 | <.0001 |
| Catholic | 19 | 18 | 30 | 33 | ||
| Protestant | 17 | 14 | 27 | 43 | ||
| Other | 18 | 25 | 26 | 31 | ||
| Parity | 0 | 22 | 24 | 49 | 6 | <.0001 |
| 1 | 26 | 20 | 30 | 24 | ||
| 2 | 13 | 13 | 17 | 57 | ||
| 3+ | 13 | 7 | 11 | 68 | ||
| Unintended Pregnancies | 0 | 19 | 20 | 37 | 24 | <.0001 |
| 1 | 18 | 14 | 22 | 46 | ||
| 2 | 16 | 12 | 17 | 55 | ||
| 3+ | 19 | 10 | 14 | 57 | ||
| Ever had an Abortion | No | 18 | 16 | 29 | 37 | 0.0325 |
| Yes | 20 | 16 | 23 | 41 |
No method includes all women reporting no pregnancy prevention measures, as well as those using emergency contraception, natural family planning, and withdrawal. Less effective methods include condoms, diaphragms/sponges and spermicides. Moderately effective methods are the pill, patch, ring, and contraceptive injection. Highly effective methods are the IUD, implant, and male and female sterilization.
Multivariate Results
Adjusted analyses are presented in Table 3. With regard to any contraceptive use, blacks were less likely to use a method compared to whites (adjusted odds ratio (AOR) 0.65; 95% CI: 0.51–0.83) while the difference between Hispanics and non-Hispanic whites in use of any method was not statistically significant. Among women using contraception, Hispanics and blacks were less likely than whites to use a highly or moderately effective method vs. a less effective method (AOR 0.57; 95% CI: 0.43–0.76 and AOR 0.49; 95% CI: 0.37–0.65, respectively). In addition, significant disparities between both Hispanics and blacks compared to whites in use of highly effective methods were evident (AOR 0.59; 95% CI: 0.46–0.77 and AOR: 0.63; 95% CI: 0.46–0.84, respectively).
Table 3.
Adjusted associations between socio-demographic variables and contraceptive use
| Any method vs no method N=7214 |
High/Mod vs Less Effective (excluding non-users) N=5809 |
High vs Mod/Less Effective (excluding non- users) N=5809 |
|||||
|---|---|---|---|---|---|---|---|
| Socio- demographic characteristic |
Category | Adjusted OR | p value | Adjusted OR | p value | Adjusted OR | p value |
| Race/ Ethnicity | White | Ref | Ref | Ref | |||
| Hispanic | 0.94 (0.76, 1.17) | 0.6085 | 0.57 (0.43, 0.76) | 0.0001 | 0.59 (0.46, 0.77) | <.0001 | |
| Black | 0.65 (0.51, 0.83) | 0.0004 | 0.49 (0.37, 0.65) | <.0001 | 0.63 (0.46, 0.84) | 0.0021 | |
| Other | 0.59 (0.45, 0.77) | <.0001 | 0.41 (0.28, 0.61) | <.0001 | 0.58 (0.38, 0.88) | 0.0106 | |
| Age | 15–19 | Ref | Ref | Ref | |||
| 20–29 | 1.51 (1.09, 2.10) | 0.0123 | 0.99 (0.72, 1.38) | 0.9709 | 2.26 (1.11, 4.62) | 0.0252 | |
| 30–39 | 1.15 (0.79, 1.68) | 0.4710 | 1.19 (0.81, 1.74) | 0.3673 | 5.79 (2.72, 12.3) | <.0001 | |
| 40–44 | 1.25 (0.85, 1.84) | 0.2624 | 1.49 (0.94, 2.39) | 0.0931 | 12.0 (5.69, 25.3) | <.0001 | |
| Income | < 100 poverty level | Ref | Ref | Ref | |||
| 100–299 poverty level | 0.95 (0.73, 1.23) | 0.6953 | 0.78 (0.60, 1.01) | 0.0604 | 1.08 (0.81, 1.44) | 0.5907 | |
| > 299 poverty level | 1.02 (0.76, 1.39) | 0.8785 | 1.00 (0.71, 1.41) | 0.9968 | 1.16 (0.79, 1.69) | 0.4439 | |
| Education | HS diploma or less | Ref | Ref | Ref | |||
| At least some college | 1.24 (1.02, 1.51) | 0.0274 | 0.79 (0.63, 0.98) | 0.0326 | 0.55 (0.43, 0.71) | <.0001 | |
| Insurance status | Private | Ref | Ref | Ref | |||
| Public/None | 0.75 (0.61, 0.92) | 0.0066 | 0.76 (0.60, 0.98) | 0.0313 | 1.15 (0.86, 1.55) | 0.3384 | |
| Marital status | Ever been married | Ref | Ref | Ref | |||
| Never been married | 0.89 (0.73, 1.08) | 0.2483 | 0.97 (0.77, 1.23) | 0.8315 | 0.56 (0.44, 0.73) | <.0001 | |
| Religion | Catholic | Ref | Ref | Ref | |||
| None | 1.08 (0.82, 1.42) | 0.6020 | 1.22 (0.89, 1.66) | 0.2148 | 1.94 (1.38, 2.74) | 0.0001 | |
| Protestant | 1.29 (0.99, 1.67) | 0.0567 | 1.35 (1.02, 1.79) | 0.0329 | 1.74 (1.32, 2.28) | <.0001 | |
| Other | 1.11 (0.76, 1.62) | 0.5884 | 0.65 (0.43, 0.97) | 0.0355 | 0.85 (0.54, 1.32) | 0.4668 | |
| Parity | 0 | Ref | Ref | Ref | |||
| 1 | 0.89 (0.67, 1.18) | 0.4063 | 1.07 (0.79, 1.43) | 0.6724 | 3.15 (2.15, 4.59) | <.0001 | |
| 2 | 2.11 (1.51, 2.95) | <.0001 | 1.97 (1.40, 2.77) | 0.0001 | 9.62 (6.93, 13.3) | <.0001 | |
| 3+ | 2.37 (1.61, 3.50) | <.0001 | 4.30 (3.01, 6.14) | <.0001 | 20.0 (13.2, 30.3) | <.0001 | |
| Unintended pregnancies | 0 | Ref | Ref | Ref | |||
| 1 | 0.94 (0.74, 1.20) | 0.6458 | 1.31 (1.02, 1.69) | 0.0346 | 1.59 (1.24, 2.04) | 0.0002 | |
| 2 | 0.97 (0.69, 1.36) | 0.8629 | 1.17 (0.85, 1.61) | 0.3437 | 1.49 (1.10, 2.01) | 0.0107 | |
| 3+ | 0.74 (0.52, 1.04) | 0.0853 | 1.24 (0.77, 1.99) | 0.3741 | 1.37 (0.98, 1.91) | 0.0659 | |
With respect to other variables, older age and having been married were associated with use of a highly effective method, higher parity was associated with use of any method and with more effective methods, and a history of having had one or two unintended pregnancies was significantly associated with use of a highly effective method, although the association with having had 3 or more unintended pregnancies did not reach statistical significance. Educational attainment had inconsistent associations with contraceptive use, while income was not associated with any of the outcomes. Women with public or no insurance were significantly less likely to use a method, as well as being less likely to use a highly or moderately effective method.
In the sensitivity analysis investigating the effect of including abortion in the models shown in Table 3, there were no significant changes to these findings (data not shown). In addition, having had an abortion was not associated with any of the outcomes in multivariate analyses. Similarly, including natural family planning methods, withdrawal, and emergency contraception as less effective methods did not change the racial/ethnic trends observed.
Interaction Analyses
Interactions between race/ethnicity and age were found for all three outcomes (p=0.046, p=0.003 and p<0.001 for any method vs. no method, high/moderate vs. less effective method, and high vs. moderate/less method, respectively) (data not shown). For parity, interactions were only found for the high/moderate vs. less effective method outcome (p=0.006). No substantial interactions between race/ethnicity and history of unintended pregnancy were identified. When both interaction terms (race/age and race/parity) were included in the high/moderate vs. less effective method analysis, only the interaction with age remained significant (p=0.003 for race/age interaction and p=0.11 for the race/parity interaction).
Table 4 presents stratified data by age for each racial/ethnic group. In assessing disparities in use of any method vs. no method, there were no clear trends by age. With respect to the high/moderate vs. less effective method outcome and the high vs. moderate/less effective outcome, there was notable variation by age, with more prominent disparities among younger women. The one exception was the youngest Hispanics, who were significantly more likely to use a high vs. moderate or less effective method than were non-Hispanic whites of the same age (AOR: 5.03; 95% CI: 1.43–17.7), and were not significantly different from whites in use of a high or moderate vs. less effective method
Table 4.
Adjusted odds of contraceptive use by race/ethnicity, stratified by age*
| Any vs no method N=7214 |
High/Mod vs Least (excluding non-users) N=5809 |
High vs Mod/Least (excluding non-users) N=5809 |
|||||
|---|---|---|---|---|---|---|---|
| Adj OR | P value | Adj OR | P value | Adj OR | P value | ||
| Race/Ethnicity | Age | ||||||
| Hispanic (Reference=White) | 15–19 | 0.83 (0.46, 1.47) | 0.5176 | 0.70 (0.34, 1.42) | 0.3212 | 5.03 (1.43, 17.7) | 0.0117 |
| 20–29 | 0.93 (0.63, 1.38) | 0.7311 | 0.50 (0.33, 0.75) | 0.0008 | 0.31 (0.20, 0.48) | <.0001 | |
| 30–39 | 0.98 (0.64, 1.51) | 0.9366 | 0.53 (0.34, 0.82) | 0.0046 | 0.64 (0.45, 0.90) | 0.0116 | |
| 40–44 | 0.94 (0.46, 1.94) | 0.8679 | 0.79 (0.37, 1.73) | 0.5608 | 0.90 (0.45, 1.78) | 0.7552 | |
| Black (Reference=White) | 15–19 | 0.98 (0.52, 1.86) | 0.9584 | 0.32 (0.16, 0.62) | 0.0008 | 0.10 (0.01, 1.46) | 0.0928 |
| 20–29 | 0.59 (0.42, 0.83) | 0.0025 | 0.39 (0.27, 0.56) | <.0001 | 0.38 (0.24, 0.61) | <.0001 | |
| 30–39 | 0.67 (0.40, 1.10) | 0.1121 | 0.78 (0.45, 1.34) | 0.3665 | 0.79 (0.51, 1.22) | 0.2861 | |
| 40+ | 0.76 (0.38, 1.49) | 0.419 | 1.06 (0.37, 3.01) | 0.9131 | 0.77 (0.37, 1.59) | 0.4776 | |
Controlling for age, income, education, insurance status, marital status, religion, parity and history of unintended pregnancies.
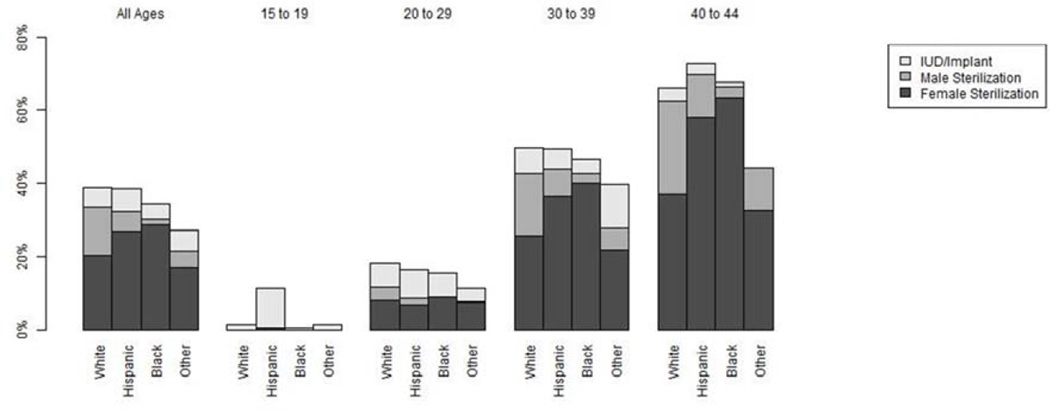
To better understand differences in use of highly effective methods, we performed stratified analyses by age, race/ethnicity and type of high-efficacy method (male or female sterilization vs. IUD or implant) (Figure 1). The difference between Hispanics, whites and blacks in the 15–19 year old age group was driven by differences in use of IUDs or implants, with Hispanics being most likely to use these methods (11%) followed by whites (1.3%) and blacks (0.7%). Differences in use of highly effective methods in women ages 20–29 were due to differences in sterilization, with whites having the highest proportion using sterilization in this age group. In fact, Hispanics and blacks between the ages of 20 and 29 were slightly more likely to use IUDs or implants than were whites (8% and 7% vs. 6%, respectively). The difference in sterilization in this age group between whites and Hispanics was due to whites being more likely to rely on both male and female sterilization, while for blacks this difference was driven only by a higher percentage of white women relying on male sterilization. Among women in the 40+ age year group, 70% of Hispanic women and 66% of black women relied on sterilization (12% male and 58% female sterilization for Hispanics and 3% male and 63% female sterilization for blacks), while only 62% of whites relied on this method (25% male and 37% female sterilization). Blacks in this age group were less likely to use IUDs or implants than white and Hispanic women (4% for whites, 3% for Hispanics and 1% for blacks).
Figure 1.
Use of highly effective methods (intrauterine contraception, female sterilization, and male sterilization), by age and race/ethnicity
Comment
This analysis of the 2006–2010 NSFG confirms the existence of substantial racial/ethnic disparities in contraceptive use in the United States, with both Hispanic and black women being less likely to use effective methods of contraception than white women. In addition, black women at risk for unintended pregnancy are less likely to be using any method of contraception. In assessing variation in disparities across age and reproductive life experiences, we found that these disparities are concentrated in younger women, especially when assessing disparities between blacks and whites.
One particular finding of interest, which has not been previously described, is the presence of racial/ethnic disparities in use of highly effective methods in the multivariable model. These disparities are somewhat surprising given the higher rate of female sterilization among non-white women as compared to white women.11 This finding is largely explained by white women being more likely to rely on male sterilization than the other racial/ethnic groups, as well as the effect of controlling for other demographic characteristics. The concentration of the disparities in use of highly effective methods in the younger age groups, with the exception of Hispanic women aged 15–19, appears to be driven by both differential use of the IUD and implant between blacks and whites ages 15–19 as well as by different timing of sterilization by racial/ethnic group. Surprisingly, we found that white women in the 20–29 year old group were more likely to rely on sterilization than Hispanic and black women. At older ages, Hispanic and black women outpace white women with regard to relying on sterilization, though they remain far less likely to rely on male sterilization throughout their reproductive years.
Possible reasons for disparities in contraceptive use include differences in patient knowledge and higher levels of concerns about the safety of birth control.15–18 Disparities in contraceptive use could also result from differential access to medical care,19 as well as differences in the experience interfacing with the medical system, even when financial and access barriers are removed, as racial/ethnic minorities report more distrust of the health care system than whites.20–22 This distrust could be amplified in the context of contraception given a history in which some family planning programs in the United States were associated with coercion of minorities to use highly effective methods.23–25,26 In addition, some studies have suggested that minority women may receive lower quality of family planning care,27,28 as well as specifically experience pressure to use birth control from medical providers.27,29 The experience of being pressured may elicit a contradictory response, as one study found that women’s perception of being pressured to choose a specific method was associated with early discontinuation of this method.30 Our findings regarding the concentration of disparities among younger women suggests that life experience may help black and Hispanic women to overcome these barriers to contraceptive use.
The presence of variation in contraceptive disparities by age has implications for interventions designed to decrease disparities in contraceptive use. The sub-groups of blacks and, to a lesser extent, Hispanics at highest risk of non-use of contraception or use of less effective methods are those who are younger. Public health interventions designed to reach these women, who may have had less exposure to the medical system, may benefit from using non-clinical methods of communicating information about contraceptive methods and the risk of unintended pregnancy, including social media and peer-to-peer interventions. The lower utilization of highly effective methods among young black women and Hispanic women between the age of 20 and 29, coupled with the higher rates of unintended pregnancy observed in these racial/ethnic groups and the finding that women of color may have less awareness about highly effective reversible methods,31 suggests the value of ensuring that these women have information about these methods. Recent evidence that racial disparities in contraceptive use are increasing over time further highlights the importance of this work.32 However, any such efforts need to be aware of and sensitive to the historical context regarding coercion of minority women to use highly effective contraception.23–25
In considering our results, it is important to be aware of some differences between how we conducted analyses and other previously reported analyses of the NSFG. First, we classified those who used withdrawal, natural family planning and emergency contraception as not using a method in order to focus our analysis on modern methods that are designed to be used on an on-going basis. However, sensitivity analysis including these methods as less effective methods did not alter our findings. In addition, our methodology differed in how we determined who was at risk for unintended pregnancy, in that we excluded women who were using contraception but were not sexually active in the previous three months. In contrast, all women using contraception, regardless of sexual activity, are often included in the at-risk group in analyses conducted of the NSFG.7 Together, these differences account for our finding of a higher rate of non-use of contraception (18% vs. 11%).7 An additional consideration is our inclusion of women who relied on sterilization in our analyses. The only other analyses to use multivariate modeling of contraceptive disparities using nationally representative samples excluded these women.8,10,33 Including these women provides a more comprehensive assessment of the number of women of risk for unintended pregnancy and their contraceptive use.
Limitations of our analysis include the cross-sectional nature of our data. While we have attempted to approximate a life course perspective on women’s contraceptive use, our findings of variations in racial/ethnic disparities in contraceptive use potentially could reflect cohort effects rather than changes over individual women’s life courses. As with all analyses of the NSFG, we relied on self-report of contraceptive use rather than objective sources of data such as pharmacy records. Finally, the inclusion of all women in our sample who do not report that they are trying to get pregnant at the time of interview will result in the inclusion of some women who, while perhaps not actively trying to get pregnant, are not necessarily trying to avoid pregnancy (either due to ambivalence or other factors). Given some evidence that there may be racial/ethnic differences in pregnancy intentions and that ambivalence may be associated with use of less effective methods,34 these differences may underlie some of our findings.
In conclusion, these results provide further insight into disparities in contraceptive use, and offer guidance around how to best work to mitigate these disparities and the resulting disparities in unintended pregnancy. Ensuring that young women of color have information about and access to effective methods that can help them achieve their reproductive goals may be the best approach to reduce disparities in women’s reproductive outcomes.
Acknowledgments
The authors thank Lawrence Finer, PhD, of the Guttmacher Institute for assistance with conceptualization and editing of this manuscript.
This work was supported by Grant Numbers 1R21HD068736-01A1 (S.B.) and K23HD067197 (C.D.) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflict of interest.
This research was presented as a poster at the 2013 North American Forum on Family Planning, Seattle, WA, October 5–7, 2013.
Contributor Information
Christine Dehlendorf, Departments of Family and Community Medicine, Obstetrics, Gynecology and Reproductive Sciences, and Epidemiology and Biostatistics, University of California, San Francisco, San Francisco, CA..
Seo Young Park, Center for Research on Health Care Data Center, University of Pittsburgh, Pittsburgh, Pennsylvania Division of General Internal Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania..
Chetachi A. Emeremni, Center for Research on Health Care Data Center, University of Pittsburgh, Pittsburgh, Pennsylvania Division of General Internal Medicine, University of Pittsburgh School of Medicine. Dr. Emeremni is now with Novartis Pharmaceuticals Corporation, Pittsburgh, Pennsylvania.
Ms. Diane Comer, Center for Research on Health Care Data Center, University of Pittsburgh, Pittsburgh, Pennsylvania Division of General Internal Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania.
Ms. Kathryn Vincett, Amherst College, Amherst, MA.
Sonya Borrero, Division of General Internal Medicine, University of Pittsburgh School of Medicine, Center for Research on Health Care, University of Pittsburgh, and Center for Health Equity Research, VA Pittsburgh Healthcare System, Pittsburgh, Pennsylvania.
References
- 1.Finer L, Zolna M. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–485. [Google Scholar]
- 2.Borrero S, Moore CG, Qin L, et al. Unintended pregnancy influences racial disparity in tubal sterilization rates. J Gen Intern Med. 2010;25:122–128. doi: 10.1007/s11606-009-1197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 4.Hatcher RA, Trussell J, Nelson AL, Cates W, Stewart FH, D K. Contraceptive Technology. 19th ed. New York, NY: Ardent Media; 2007. [Google Scholar]
- 5.Raine T, Minnis AM, Padian NS. Determinants of contraceptive method among young women at risk for unintended pregnancy and sexually transmitted infections. Contraception. 2003;68:19–25. doi: 10.1016/s0010-7824(03)00107-0. [DOI] [PubMed] [Google Scholar]
- 6.Frost JJ, Singh S, Finer LB. Factors associated with contraceptive use and nonuse, United States, 2004. Perspect Sex Reprod Health. 2007;39:90–99. doi: 10.1363/3909007. [DOI] [PubMed] [Google Scholar]
- 7.Jones J, Mosher W, Daniels K. Current Contraceptive Use in the United States, 2006–2010, and Changes in Patterns of Use Since 1995. National Health Statistics Reports. 2012;60 [PubMed] [Google Scholar]
- 8.Wu J, Meldrum S, Dozier A, Stanwood N, Fiscella K. Contraceptive nonuse among US women at risk for unplanned pregnancy. Contraception. 2008;78:284–289. doi: 10.1016/j.contraception.2008.04.124. [DOI] [PubMed] [Google Scholar]
- 9.Dehlendorf C, Foster D, de Bocanegra H, Brindis C, Bradsberry M, Darney P. Race, ethnicity and differences in contraception among low-income women: methods received by Family PACT Clients, California, 2011–2007. Perspectives on Sexual and Reproductive Health. 2011;43:181–187. doi: 10.1363/4318111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40:94–104. doi: 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 11.Borrero S, Schwarz EB, Reeves MF, Bost JE, Creinin MD, Ibrahim SA. Race, insurance status, and tubal sterilization. Obstet Gynecol. 2007;109:94–100. doi: 10.1097/01.AOG.0000249604.78234.d3. [DOI] [PubMed] [Google Scholar]
- 12.Lepkowski JM, Mosher WD, Davis KE, Groves RM, Van Hoewyk J. The 2006–2010 National Survey of Family Growth: sample design and analysis of a continuous survey. Vital Health Stat. 2010;2:1–36. [PubMed] [Google Scholar]
- 13.Steiner MJ, Trussell J, Mehta N, Condon S, Subramaniam S, Bourne D. Communicating contraceptive effectiveness: A randomized controlled trial to inform a World Health Organization family planning handbook. Am J Obstet Gynecol. 2006;195:85–91. doi: 10.1016/j.ajog.2005.12.053. [DOI] [PubMed] [Google Scholar]
- 14.Jones RK, Kost K. Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth. Stud Fam Plann. 2007;38:187–197. doi: 10.1111/j.1728-4465.2007.00130.x. [DOI] [PubMed] [Google Scholar]
- 15.Dehlendorf C, Rodriguez MI, Levy K, Borrero S, Steinauer J. Disparities in family planning. Am J Obstet Gynecol. 2010;202:214–220. doi: 10.1016/j.ajog.2009.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaye K, Suellentrop K, Sloup C. The Fog Zone: How Misperceptions, Magical Thinking, and Ambivalence Put Young Adults at Risk for Unplanned Pregnancy. Washington, DC: The National Campaign to Prevent Teen and Unintended Pregnancy; 2009. [Google Scholar]
- 17.Guendelman S, Denny C, Mauldon J, Chetkovich C. Perceptions of hormonal contraceptive safety and side effects among low-income Latina and non-Latina women. Matern Child Health J. 2000;4:233–239. doi: 10.1023/a:1026643621387. [DOI] [PubMed] [Google Scholar]
- 18.Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74:125–132. doi: 10.1016/j.contraception.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Todd S, Sommers B. Overview of the uninsured in the united states: a summary of the 2012 current population survey report. 2012 [Google Scholar]
- 20.Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. 2007;14:56–60. [PubMed] [Google Scholar]
- 21.Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in health. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 22.Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97:1283–1289. doi: 10.2105/AJPH.2005.080762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health. 2005;95:1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schoen J. Between choice and coercion: women and the politics of sterilization in North Carolina, 1929–1975. Journal Of Women's History. 2001;13:132–156. [Google Scholar]
- 25.Morgan M. The payment of drug addicts to increase their sterilisation rate is morally unjustified and not simply 'A Fine Balance'. J Obstet Gynaecol. 2004;24:119–123. doi: 10.1080/01443610410001645361. [DOI] [PubMed] [Google Scholar]
- 26.Thorburn S, Bogart LM. Conspiracy beliefs about birth control: barriers to pregnancy prevention among African Americans of reproductive age. Health Educ Behav. 2005;32:474–487. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- 27.Becker D, Tsui AO. Reproductive health service preferences and perceptions of quality among low-income women: racial, ethnic and language group differences. Perspect Sex Reprod Health. 2008;40:202–211. doi: 10.1363/4020208. [DOI] [PubMed] [Google Scholar]
- 28.Forrest JD, Frost JJ. The family planning attitudes and experiences of low-income women. Fam Plann Perspect. 1996;28:246–255. 77. [PubMed] [Google Scholar]
- 29.Downing RA, LaVeist TA, Bullock HE. Intersections of ethnicity and social class in provider advice regarding reproductive health. Am J Public Health. 2007;97:1803–1807. doi: 10.2105/AJPH.2006.092585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalmuss D, Davidson AR, Cushman LF, Heartwell S, Rulin M. Determinants of early implant discontinuation among low-income women. Fam Plann Perspect. 1996;28:256–260. [PubMed] [Google Scholar]
- 31.Borrero S, Abebe K, Dehlendorf C, et al. Racial variation in tubal sterilization rates: role of patientlevel factors. Fertil Steril. 2011;95:17–22. doi: 10.1016/j.fertnstert.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobs J, Stanfors M. Racial and ethnic differences in U.S. Women's choice of reversible contraceptives, 1995–2010. Perspect Sex Reprod Health. 2013;45:139–147. doi: 10.1363/4513913. [DOI] [PubMed] [Google Scholar]
- 33.Xu X, Macaluso M, Frost J, Anderson JE, Curtis K, Grosse SD. Characteristics of users of intrauterine devices and other reversible contraceptive methods in the United States. Fertil Steril. 2011;96:1138–1144. doi: 10.1016/j.fertnstert.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 34.Schwarz EB, Lohr PA, Gold MA, Gerbert B. Prevalence and correlates of ambivalence towards pregnancy among nonpregnant women. Contraception. 2007;75:305–310. doi: 10.1016/j.contraception.2006.12.002. [DOI] [PubMed] [Google Scholar]