Abstract
Objective
Postoperative facet joint syndrome requiring radiofrequency neurotomy (RFN) is a relatively common problem following microscopic discectomy. However, the efficacy of repeated RFN after microscopic discectomy has not been clearly documented. The purpose of this study was to determine the success rate and symptom-free duration of repeated RFN for facet joint syndrome after microscopic discectomy.
Methods
Medical records from 56 patients, who had undergone successful initial RFN following microscopic discectomy, experienced recurrence of pain, and subsequently had repeated RFN, were reviewed and evaluated. Responses of repeated RFN were compared with initial radiofrequency neurotomy for success rates and duration of relief. The criterion for RFN to be successful was defined as greater than 50% relief from pain and sufficient satisfaction of patients with prior RFN to have repeated RFN.
Results
Fifty-six patients (41 women and 15 men; mean age=48 years) had repeated RFNs, which were successful in all except three patients. RFN denervated three bilateral segments (L3-L4, L4-L5, and L5-S1) in all patients. Mean duration of relief after initial RFN was 9.2 months (range 3-14). The mean duration of relief after secondary RFN in 53 patients was 9.0 months (range 4-14). The success rates and duration of relief remained consistent after subsequent RFNs.
Conclusion
Repeated RFN for lumbar facet joint pain after microscopic discectomy is an effective palliative treatment. It provided a mean duration of relief of 9.0 months and >94% success rate.
Keywords: Facet syndrome, Radiofrequency, Neurotomy, Discectomy
INTRODUCTION
Microscopic discectomy is a standard surgical procedure for lumbar disc herniation and has been approved as a safe method to alleviate radiating pain and other neurological symptoms. However, postoperative facet joint syndrome following microscopic discectomy is a relatively common problem requiring intervention1). The prevalence of facet joint syndrome in patients after lumbar intervention is 8-32 cases per 1008). The diagnosis of facet joint syndrome is confirmed when there is at least 50% relief from the targeted pain after a local anesthetic blockade of the medial branches of the posterior rami of spinal nerves that supply the facet joint3).
It has been demonstrated that medial branch block and RFN are effective, but temporary, management of lumbar facet joint syndrome2,5,6,7,9,10,11,12,13,15). Although the duration of relief after an initial RFN has not been established firmly, the benefits of RFN eventually dissipate in most, if not all, patients. Dreyfuss et al.2,3) found that 60% of patients can expect 90% relief, and 87% can expect at least 60% relief from pain for about 12 months. A few of these patients had modest relapses between 6 and 12 months. Van Kleef et al.16) also reported successful RFN in 10 out of 15 patients. It has been recommended that when pain reappears after successful RFN, RFN may be repeated, but the outcome and duration of relief for repeated RFNs after microscopic discectomy are not clearly confirmed. In this study, the experiences with repeated RFN for facet joint syndrome following microscopic discectomy have been reviewed in order to determine the success rate and duration of relief as compared to initial RFN.
MATERIALS AND METHODS
Among 624 patients who underwent microscopic discectomy for single level disc herniation from 2005 to 2011, the medical records of patients who underwent repeated RFN for facet joint syndrome after microscopic discectomy were reviewed. We included three criteria for study entry: (1) greater than 50% reduction in the target pain after the initial RFN for at least 3 months, (2) return of pain, and (3) sufficient patient satisfaction with the initial RFN to have it repeated when pain recurred. These patients were re-evaluated by follow-up magnetic resonance image to make sure they did not have recurred or ongoing compressive lesion that were clearly indicated for microscopic discectomy. Patients with previous lumbar spine surgery, compensable disability, or work injury were excluded in our study. No patient responded to intensive conservative treatments that included physical therapy, medications, and other types of spinal injections. Patients who had less than 50% relief for 3 months after initial RFN or who were not satisfied with their outcome after initial RFN were excluded from our study as they were not candidates for repeated RFN. To minimize the chance of a false positive (placebo) response, medial branch block was performed twice before repeated RFN and provided relief each time. Evaluation of the pain relief was done using the visual analog scale (VAS). Pain alleviation of more than 50% after 3 months was considered as a successful response for repeated RFN. Response to each repeated RFN was compared with the initial successful RFN and graded as success (more than 50% relief from pain for 3 months) or failure (less than 50% relief from pain for 3 months). RFN was performed using a modification of the technique described by Dreyfuss et al.2,3)
1. Surgical Procedure
On the radiolucent operative table, the patient was placed in a prone position, and the C-arm fluoroscopy was adjusted to an anteroposterior view, such that the superior and inferior margins of the vertebral body were aligned. Next, in order to detect the pedicle properly, the imaging intensifier was rotated approximately 10-20 degrees. Under X-ray inspection, an SMKC10 needle (22 gauge with 5-mm active tip and 100-mm cannula) was inserted at Burton's point where the grooves made by the superior articular and transverse processes meet. On confirming the accurate location of the cannula, an electrode was inserted for electric stimulation. Once we confirmed that no fasciculation occurred in the muscles of lower limbs, a lesion was made at 80℃ for approximately 90s. This was followed by the administration of 0.5mL of 1% lidocaine and 5mg triamcinolone acetonide (Tamcetone R, Hanol Inc., Korea) at the end of the surgical procedure, to prevent discomfort and development of neuritis.
RESULTS
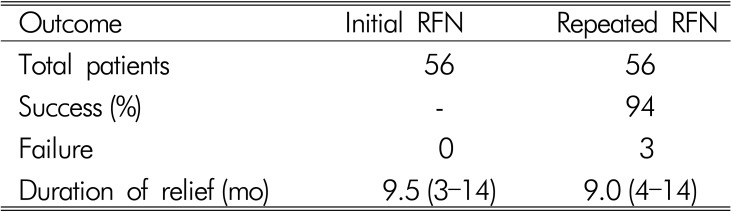
There were 56 patients (41 women and 15 men). Mean age was 48 years (range 30-67 years). All patients underwent microscopic discectomy for lumbar disc herniation at L4-5 or L5-S1 level. Secondary RFN denervated three segments (L3-L4, L4-L5, and L5-S1) bilaterally in all patients because each joint is innervated by two nerve which branch out into the posterior lumbar nerve trunks. In the 56 patients who had initial successful RFN, mean duration of relief was 9.2 months (range 3-14). The repeated secondary RFNs were successful in 53 (94%), but unsuccessful in three patients. The mean duration of relief in the 53 patients was 9.0 months (range 4-14) for the secondary RFN. There were no neurologic complications such as sensory dysesthesia and neuritis. These results are summarized in (Table 1).
Table 1.
Frequency of success and duration of relief of repeated radiofrequency neurotomy as compared to initial radiofrequency neurotomy
RFN=radiofrequency neurotomy
DISCUSSION
Weight bearing on the lumbar spine is distributed and supported by the anterior and posterior structures of the vertebrae. In the anterior, the vertebral body and disc play an important role. In the posterior, the facet joint, along with the ligaments, plays a main role in maintaining the stability of the posterior structures and intervertebral discs6). When discectomy is performed for the lumbar disc herniation, the disc space becomes narrow, resulting in an imbalance in the weight bearing on spinal structures, and consequently, leads to enhanced stress on the facet joint. Hence, postoperative facet joint syndrome can result from microscopic discectomy.
RFN offers profound and lasting relief from back pain or buttock pain originating from the facet joint11). If patients are rigorously evaluated and accurate surgical techniques are used, more than 60% of patients can expect at least a 90% reduction in pain, and 87% can expect at least a 60% reduction lasting for about 12 months, although some may experience shorter or longer period of pain relief3,4,10,14,16). RFN does not cure facet joint syndrome, and the effects of facet denervation are not usually permanent due to nerve regeneration. Benefits eventually dissipate, and RFN may need to be repeated. However, the outcome and duration of relief for repeated RFN after microscopic discectomy are not well established. In the present study, we have shown that after an initial successful lumbar RFN, repeat RFNs are successful in about 94% of patients. We have chosen 50% reduction in pain relief as an indicator of success as it has been shown to correlate with a high degree of patient satisfaction16). We did not evaluate the outcomes of all patients who had an initial RFN, as this was not the purpose of the study. The sustained success after repeated RFNs provided circumstantial evidence that the successful responses were true positives, at least clinically. Certainly, the RFNs were worthwhile in these patients.
Two out of three patients who showed unsuccessful result had instability at the segment at the segment where the microscopic discectomy was performed, pain relief and its duration was less.
Technical failure is a possibility given the demanding nature of the procedure. However, this is not the case with our study, since all RFNs were performed by a single experienced doctor using established techniques. Although transient, repeated RFNs provided a mean duration of relief of 9.0 months and were successful more than 94%. Nevertheless, one of the limitations of our study is that the alleviation of pain in patients can only be evaluated by subjective measures and we have not quantified changes in pain or function after RFNs. The success rate was based on the patients' satisfaction, as demonstrated by their desire to have the RFN repeated, and subjective pain relief of greater than 50%. A long-term study with more repeated RFNs may be necessary for the validation of its usefulness in the management of facet joint syndrome following microscopic discectomy.
CONCLUSION
This study demonstrates that, similar to primary RFN, repeated RFN can be considered as an effective palliative treatment for facet joint syndrome after microscopic discectomy. It can be expected to provide pain relief similar to primary RFN.
References
- 1.Ahlhelm F, Reith W, Naumann N, Schulte-Altedorneburg G, Papanagiotou P, Kelm J, et al. Postoperative syndrome after spine surgery. Radiologe. 2006;46(6):486–494. doi: 10.1007/s00117-006-1386-3. [DOI] [PubMed] [Google Scholar]
- 2.Dreyfuss P, Dreyer SJ, Herring SA. Lumbar zygapophysial (facet) joint injections. Spine. 1995;20:2040–2047. doi: 10.1097/00007632-199509150-00019. [DOI] [PubMed] [Google Scholar]
- 3.Dreyfuss P, Halbrook B, Pauza K, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine. 2000;25:1270–1277. doi: 10.1097/00007632-200005150-00012. [DOI] [PubMed] [Google Scholar]
- 4.Dreyfuss P, Schwarzer AC, Lau P, Bogduk N. Specificity of lumbar medial branch and L5 dorsal ramus blocks. A computed tomography study. Spine. 1997;22:895–902. doi: 10.1097/00007632-199704150-00013. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan M, Dreyfuss P, Halbrook B, Bogduk N. The ability of lumbar medial branch blocks to anesthetize the zygapopysial joint. A physiologic challenge. Spine. 1998;23:1847–1852. doi: 10.1097/00007632-199809010-00008. [DOI] [PubMed] [Google Scholar]
- 6.Kim SW, Lee SM, Shin H. Radiofrequency facet denervation for low back pain after microscopic discectomy. J Korean Neurosurg Soc. 2005;38:442–444. [Google Scholar]
- 7.Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2001;26:1411–1417. doi: 10.1097/00007632-200107010-00003. [DOI] [PubMed] [Google Scholar]
- 8.Manchikanti L, Manchikanti KN, Pampati V, Brandon DE, Giordano J. The prevalence of facet-joint-related chronic neck pain in postsurgical and nonpostsurgical patients: a comparative evaluation. Pain Pract. 2008;8(1):5–10. doi: 10.1111/j.1533-2500.2007.00169.x. [DOI] [PubMed] [Google Scholar]
- 9.Manchikanti L, Singh V, Vilims BD. Medial branch neurotomy in management of chronic spinal pain: systematic review of the evidence. Pain Physician. 2002;5:405–418. [PubMed] [Google Scholar]
- 10.North RB, Han M, Zahurak M, Kidd DH. Radiofrequency lumbar facet denervation: analysis of prognostic factors. Pain. 1994;57:77–83. doi: 10.1016/0304-3959(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 11.Park JY. Radiofrequency Treatment for Chronic Low Back Pain. Korean J Spine. 2004;1(2):166–180. [Google Scholar]
- 12.Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. Clinical features of patients with pain stemming from the lumbar zygapopysial joints. Is the lumbar facet syndrome a clinical entity? Spine. 1994;19:1132–1137. doi: 10.1097/00007632-199405001-00006. [DOI] [PubMed] [Google Scholar]
- 13.Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The false positive rate of uncontrolled diagnostic blocks of the lumbar zygapopysial joints. Pain. 1994;58:195–200. doi: 10.1016/0304-3959(94)90199-6. [DOI] [PubMed] [Google Scholar]
- 14.Schwarzer AC, Wang S, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pains. a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54:100–106. doi: 10.1136/ard.54.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silvers HR. Lumbar percutaneous facet rhizotomy. Spine. 1990;15:36–40. doi: 10.1097/00007632-199001000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine. 1999;24:1937–1942. doi: 10.1097/00007632-199909150-00013. [DOI] [PubMed] [Google Scholar]