Abstract
Background
Single-site studies have demonstrated inadequate quality of discharge summaries in timeliness, transmission and content, potentially contributing to adverse outcomes. However, degree of hospital-level variation in discharge summary quality for patients hospitalized with heart failure (HF) is uncertain.
Methods and Results
We analyzed discharge summaries of patients enrolled in the Telemonitoring to Improve Heart Failure Outcomes (Tele-HF) study. We assessed hospital-level performance on timeliness (fraction of summaries completed on the day of discharge), documented transmission to the follow-up physician, and content (presence of components suggested by the Transitions of Care Consensus Conference (TOCCC)).
We obtained 1,501 discharge summaries from 1,640 (91.5%) patients discharged alive from 46 hospitals. Among hospitals contributing 10 or more summaries, the median hospital dictated 69.2% of discharge summaries on the day of discharge (range: 0.0–98.0%, p<0.001); documented transmission of 33.3% of summaries to the follow-up physician (range: 0.0–75.7%, p<0.001); and included 3.6/7 TOCCC elements (range: 2.9–4.5, p<0.001). Hospital course was typically included (97.2%), but summaries were less likely to include discharge condition (30.7%), discharge volume status (16.0%) or discharge weight (15.7%). No discharge summary included all seven TOCCC-endorsed content elements, was dictated on the day of discharge, and was sent to a follow-up physician.
Conclusions
Even at the highest performing hospital, discharge summary quality is insufficient in terms of timeliness, transmission and content. Improvements in all aspects of discharge summary quality are necessary to enable the discharge summary to serve as an effective transitional care tool.
Keywords: heart failure, epidemiology, quality of care, discharge summary
There are nearly one million hospital discharges each year for heart failure (HF) in the United States.1 Most hospitalizations involve changes in medication,2 and two-fifths of patients are discharged with pending test results.3 At one institution, 28% of hospitalizations had recommended follow-up to be performed by the outpatient clinician.4 Yet, only 40% of patients were seen in the hospital by any of their outpatient physicians.5 There is, therefore, an urgent need for inpatient clinicians to inform outpatient clinicians of regimen changes and needed follow-up post-discharge. This communication often takes the form of a discharge summary. Though there are several negative studies,6–9 we have recently found that high quality discharge summaries may be associated with lower risk of readmission.10
Studies of discharge summaries have found that many are of low quality in three major domains: timeliness, transmission and content. Discharge summaries are often delayed, making them unavailable in the early follow-up period.11 Moreover, summaries are often not transmitted to the appropriate outpatient clinicians.8, 12 Finally, summaries are used as a means of documenting inpatient activity and do not always include content important for care transitions such as pending studies, clinical condition at discharge, or recommended follow-up.12, 13 For example, pending labs or studies are missing from 66–75% of relevant discharge summaries.13, 14
Discharge summaries of patients admitted with HF may require specific, additional information. For example, weight gain is associated with increased risk of hospitalization for heart failure.15 Therefore, specifying discharge weight and dose of diuretic at the time of discharge may improve outpatient care by assisting outpatient physicians to risk-stratify their patients and to identify early deterioration. One single-site study, however, found that discharge weight was specified in only 4% of discharge summaries for patients admitted with heart failure.12
Most studies of discharge summary quality have been single-site or focused on academic teaching institutions.8, 16–20 Performance at community hospitals and the degree to which hospitals differ in the quality of their discharge summaries is unknown. Accordingly, we reviewed discharge summaries for patients enrolled in the Telemonitoring to Improve Heart Failure Outcomes (Tele-HF) study, a randomized controlled trial of the effectiveness of tele-monitoring in patients with heart failure.21 Patients in Tele-HF were admitted to 46 hospitals across the country and discharge summaries were collected for enrolled patients as part of the study protocol. We assessed the timeliness, transmission and content of these discharge summaries to determine the degree of variation in discharge summary quality for patients with heart failure across institutions.
Methods
Study cohort and setting
The Tele-HF study was a randomized, controlled trial of patients living at home and hospitalized for heart failure in the previous 30 days.22 Patients in Tele-HF were recruited from 33 cardiology practices in 21 states and the District of Columbia. We obtained discharge summaries for the index hospitalization from the hospitals to which the patients had been admitted. Wherever possible, we obtained copies of the original summary, redacted by each institution for HIPAA-sensitive content. In the case of one hospital, we received Microsoft Word documents into which the text of the summary had been cut and pasted.
Data collection
The Yale Human Investigation Committee approved this study. Three clinicians with medical or nursing backgrounds (M.A-D., B.H. and N.P.) abstracted study data from the discharge summaries using a standardized review tool based on prior work;23 all abstractors were involved in the development and refinement of the abstraction tool. A random sampling of 30 charts was double-abstracted to confirm accuracy and consistency of abstraction practices (Kappa > 0.50 for all tested variables). The tool included 40 elements covering timeliness, content and transmission. We included all the elements required by The Joint Commission (TJC) for discharge summaries (reason for hospitalization, significant findings, procedures and treatment provided, patient’s discharge condition, patient and family instructions and attending physician’s signature)24 as well as the seven elements (principal diagnosis and problem list, medication list, transferring physician name and contact information, cognitive status of the patient, test results, and pending test results) recommended by the Transitions of Care Consensus Conference (TOCCC), a consensus statement produced by six major medical societies.25 We added additional variables likely to be of importance to patients with heart failure, such as discharge weight, and studies assessing left ventricle ejection fraction. Where possible, we also recorded the level of training of the person completing the discharge summary (trainee, physician extender [registered nurse, nurse practitioner or physician assistant], attending physician), the format of the discharge summary (electronic, handwritten, dictated); and the length of the summary in pages.
Hospital level data were retrieved from the American Heart Association annual survey database for the 2008 fiscal year. These data included urban status (metropolitan division, metropolis and micropolis), teaching status (major teaching, minor teaching and non-teaching), geographic region, and bed size (<200 beds, 200–499 beds, >499 beds). Urban status was defined using core-based statistical area (CBSA) types; ‘Metropolitan division’ – urban cluster with more than 2.5 million people, ‘Metropolis’ – urban cluster with at least 50,000 people but not more than 2.5 million people and ‘Micropolis’-urban cluster with less than 50,000 people. We defined major teaching status as membership in the Council of Teaching Hospitals and Health Systems, minor teaching status as having Accreditation Council for Graduate Medical Education programs on site, and non-teaching status as affiliation with neither. For geographic region, we used the Census Bureau classification. We had only one hospital from the East South Central region. We grouped that hospital with hospitals located in the West South Central region to form a South Central region.
Main measures
We categorized quality in three domains: timeliness, transmission and content. Following methods developed for a previous study, we defined timeliness as days between discharge date and preparation date (i.e., dictation date, not final signature date, which may occur later), and measured both median timeliness and proportion of discharge summaries completed on the day of discharge.23 We defined transmission as any notation on the discharge summary that it was sent to any of the clinicians listed as having a follow up appointment with the patient. We defined 25 individual content items and assessed the frequency of each individual content item. We also measured compliance with TJC mandates and TOCCC recommendations, which included several of the individual content items. The means by which we aligned our abstraction tool with guideline recommendations is shown in the Appendix.
To measure compliance with TJC requirements, we created a composite score in which one point was provided for the presence of each of the required elements. We omitted one element (“patient and family discharge instructions”) because these were not appended to the discharge summaries we received. Consequently the maximum score for the TJC mandate composite was 5. We defined discharge condition as any comment made about the discharge day exam (including generic statements like “back to baseline”).
To measure compliance with TOCCC recommendations for discharge summaries, we created a composite score in which one point was provided for the presence of each of the seven recommended elements (maximum score=7).
Statistical analysis
We used descriptive statistics to describe characteristics of the sample and to describe summary measures of timeliness, transmission and content. Categorical variables were summarized as frequencies and proportions. Continuous variables were presented as means and standard deviations. We examined differences in discharge summary quality between sites using chi square tests and non-parametric tests, as appropriate, restricting the sample to hospitals with 10 or more summaries. To determine whether differences in quality were explained by hospital characteristics, we constructed hierarchical, mixed effect logistic regression analyses for timeliness and transmission, and hierarchical, mixed effect linear regression analyses for the composite scores of recommended content. All explanatory variables were introduced in the models as fixed effects, except hospital, which was included as a random effect to account for clustering of observations within hospitals. In these analyses, we included all observations, including from hospitals with fewer than 10 summaries. Prior to model fitting, we imputed missing values using the ‘multiple imputations by chained equations’ (MICE) method (20 iterations) to avoid bias introduced by missing data. MICE was performed using SAS add-on, IVEware (Imputation and Variance Estimation Software) version 0.2. The largest set of missing data was for transmission (11.1% imputed); all other variables had less than 5% missing data. All analyses were conducted with SAS 9.2 (SAS Institute, Cary, NC). We considered a p value < 0.05 to be statistically significant; all tests were two-sided.
Results
Study sample
A total of 1653 patients were enrolled in Tele-HF. Of these, we were unable to obtain discharge summaries for 105 patients. Of the remainder, 8 died during the index enrollment hospitalization, 13 discharge summaries were incomplete and 26 admissions were not for an acute exacerbation of heart failure, leaving 1501 summaries from 46 hospitals in the final study sample. A total of 16/46 hospitals (35%) contributed fewer than 10 summaries each, leaving 1,473 summaries from 30 hospitals. Of these, the median number of discharge summaries per hospital was 24 (inter-quartile range: 11–67 summaries). One hospital, contributing 205 discharge summaries, provided only a pasted copy of the discharge summary into a Microsoft Word document in which no dates or notations about transmission were included. Consequently, we excluded this hospital from analyses of timeliness and transmission.
Of the 46 participating hospitals, 10 (22%) hospitals were based in a metropolitan division, 33 (94%) hospitals were based in a metropolitan area and 3 (6%) hospitals were located in a micropolitan area (Table 1). A total of 41% of the hospitals were major teaching centers, 28% were minor teaching centers and the remaining 31% were non-teaching centers. Hospitals were located in diverse geographic regions: 13% in New England, 9% in Mid Atlantic, 26% in South Atlantic, 11% in East North Central, 20% West North Central, 13% in South Central and 9% in Pacific. Participating hospitals varied in bed size: 24% of the hospitals had less than 200 beds, 48% of the hospitals had 200–499 beds and 28% of the hospitals had more than 500 beds.
Table 1.
Characteristics of discharge summaries and hospitals
| Variable | Discharge summaries N=1501 (%) |
Hospitals N=46 (%) |
|---|---|---|
| Training Level | ||
| Trainee | 526 (35.0) | — |
| Physician Extender | 169 (11.3) | — |
| Attending | 540 (36.0) | — |
| Unknown | 266 (17.7) | — |
| Hospital Location | ||
| Micropolis | 53 (3.5) | 3 (6.5) |
| Metropolis | 1321 (88.0) | 33 (71.7) |
| Division | 127 (8.5) | 10 (21.7) |
| Teaching status | ||
| Major | 832 (55.4) | 19 (41.3) |
| Minor | 565 (37.6) | 13 (28.3) |
| Non-teaching | 104 (6.9) | 14 (30.4) |
| Geographic Region | ||
| East North Central | 82 (5.5) | 5 (10.9) |
| Mid-Atlantic | 44 (2.9) | 4 (8.7) |
| New England | 153 (10.2) | 6 (13.0) |
| Pacific / Associated Territories | 258 (17.2) | 4 (8.7) |
| South Atlantic | 571 (38.0) | 12 (26.1) |
| South Central | 238 (15.9) | 6 (13.0) |
| West North Central | 155 (10.3) | 9 (19.6) |
| Hospital size by number of beds | ||
| <200 | 204 (13.6) | 11 (23.9) |
| 200–499 | 771 (51.4) | 22 (47.8) |
| >499 | 526 (35.0) | 13 (28.3) |
Format
The majority of the discharge summaries were dictated (82%). The remaining summaries were either generated from the electronic medical record (16%) or handwritten (2%). The median discharge summary length was 3 pages (inter-quartile range: 2–3 pages).
Timeliness
Of the 1501 summaries in the study, 205 were from the site without time stamps and an additional 53 did not provide either discharge date (N=10) or date of summary (N=43). In the remaining 1243 summaries, the median days to preparation was 0 days with inter-quartile range of 0–2 days. A total of 835 (67.2%) summaries were prepared on the day of discharge; an additional 137 (11.0%) were prepared within 3 days of discharge. However, 90 (7.3%) were prepared more than 30 days after discharge. Of the hospitals contributing more than 10 discharge summaries, the median hospital prepared 69.2% of discharge summaries on day of discharge (range: 0.0% – 98.0%, p<0.001). The rate of summary completion on day of discharge by site is presented in Figure 1.
Figure 1.
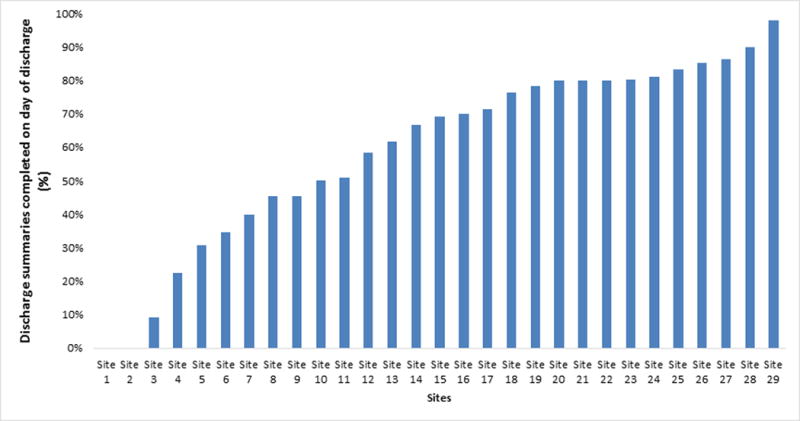
Proportion of discharge summaries completed on day of discharge by site, by hospital
*Among hospitals with 10 or more summaries; site 30 was excluded from timeliness analysis
In unadjusted analysis, trainees were less likely than attending level physicians or physician extenders to dictate the summary on the discharge day (59.0% trainees, 77.0% physician extenders, 72.6% attendings, p<0.001). Major teaching centers and non-teaching centers were more likely to prepare the summary on the discharge day compared to minor teaching centers (70.9% major teaching, 57.9% minor teaching, 70.1% non-teaching, p<0.001) There was a considerable timeliness difference across geographic regions, ranging from 27.9% in the Pacific region to 77.9% in the East North Central region (p<0.001). Smaller bed size hospitals were also less likely to prepare the discharge summary on the discharge day (44.9% <200 beds, 75.2% 200–400 beds, 67.2% >500 beds, p<0.001). However, level of training, teaching status, geographic region and hospital bed size were not associated with timely discharge summary in multivariable analysis (Table 2).
Table 2.
Factors associated with dictation on day of discharge
| Explanatory variable | Proportion dictated on day of discharge | Odds ratio for dictation on day of discharge (95% CI)* | Adjusted p value |
|---|---|---|---|
| Training Level | 0.27 | ||
| Trainees | 59.0% | Ref | |
| Physician extender | 77.0% | 1.28 (0.73 – 2.26) | |
| Attending | 72.6% | 1.40 (0.91 – 2.14) | |
| Length of stay (days) | — | 0.97 (0.94 – 0.99) | 0.02 |
| Hospital location setting | 0.01 | ||
| Division | 32.7% | Ref | |
| Micropolis | 66.0% | 9.41 (0.88 – 100.16) | |
| Metropolis | 70.8% | 6.63 (1.87 – 23.54) | |
| Hospital teaching status | 0.42 | ||
| Minor | 57.9% | Ref | |
| Major | 70.9% | 1.33 (0.42 – 4.27) | |
| Non-teaching | 70.1% | 2.43 (0.60 – 9.76) | |
| Geographic region | 0.77 | ||
| South Central | 41.7% | Ref | |
| East North Central | 77.9% | 3.80 (0.68 – 21.22) | |
| Mid Atlantic | 45.2% | 2.83 (0.42 – 18.87) | |
| New England | 74.8% | 1.70 (0.33 – 8.68) | |
| Pacific | 27.9% | 1.82 (0.20 – 16.27) | |
| South Atlantic | 77.5% | 2.71 (0.66 – 11.08) | |
| West North Central | 72.7% | 2.03 (0.45 – 9.08) | |
| Hospital bed size | 0.19 | ||
| <200 | 44.9% | Ref | |
| 200–499 | 75.2% | 3.29 (0.85 – 12.67) | |
| >499 | 67.2% | 2.96 (0.60 – 14.46) |
Based on hierarchical, multivariate mixed effect logistic model
Transmission
Of the 1,501 summaries in the study, 205 were from the site without notations about transmission, and 85 of the remainder listed no clinicians for follow-up. A total of 464 (38.3 %) of the remaining 1,211 summaries were explicitly noted as being sent to any of the clinicians listed as having a follow-up appointment with the patient. Of the hospitals with more than 10 discharge summaries, the median hospital transmitted 33.3% of discharge summaries (range: 0.0% – 75.7%, p<0.001) (Figure 2).
Figure 2.
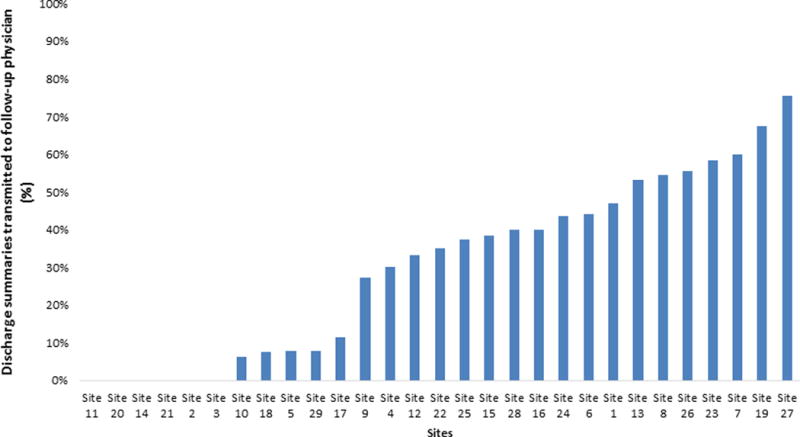
Proportion of discharge summaries transmitted to follow-up physician, by site*
*Among hospitals with 10 or more summaries; site 30 was excluded from transmission analysis
Summaries completed by trainees were less likely to be sent to any follow-up physician (23.5 %) than those completed by physician extenders (66.0 %) or attendings (52.9 %), p<0.001. In addition, summaries completed on the day of discharge were more likely to be transmitted (42.7% vs. 35.5%, p=0.02). Summaries completed in non-teaching hospitals were more likely to be transmitted (37.9% major teaching, 42.8% minor teaching, 50.6% non-teaching, p=0.05). Summaries dictated in large bed size hospitals were less likely to be transmitted (47.0% <200 beds, 52.3% 200–499 beds, 24.7% >499 beds, p<0.001) as well as summaries from hospitals located in a micropolitan area (32.2% metropolitan division, 45.5% metropolis, 0.0% micropolis, p<0.001). Hospitals showed a statistically significant difference in rates of transmission across geographic regions (min: 25.7% East North Central, max: 75% New England, p<0.001). After adjusting for site random effects, attending physicians and physician extenders remained significantly more likely to transmit discharge summaries to follow-up physicians compared to trainees (Table 3). However, in multivariate analysis, timely summaries, urban status, teaching status, geographic region and bed size were no longer associated with transmission.
Table 3.
Factors associated with discharge summary transmission
| Explanatory variable | Proportion transmitted | Odds ratio for transmission to follow-up physician (95% CI) | Adjusted p value |
|---|---|---|---|
| Training level | <0.01 | ||
| Trainees | 23.5% | Ref | |
| Physician extender | 66.0% | 2.70 (1.54 – 4.71) | |
| Attending | 52.9% | 1.62 (1.04 – 2.51) | |
| Dictated on day of discharge | 0.37 | ||
| No | 35.5% | Ref | |
| Yes | 42.7% | 1.17 (0.82 – 1.68) | |
| Length of stay (days) | — | 0.97 (0.94 – 0.99) | 0.02 |
| Hospital location setting | 0.04 | ||
| Micropolis | 0.0% | Ref | |
| Metropolis | 42.5% | 32.91 (0.78 – 1383.85) | |
| Metropolitan division | 35.2% | 9.04 (0.17 – 480.27) | |
| Hospital teaching status | 0.54 | ||
| Major | 37.9% | Ref | |
| Minor | 42.8% | 0.87 (0.21 – 3.62) | |
| Non-teaching | 50.6% | 2.13 (0.39 – 11.70) | |
| Geographic region | 0.17 | ||
| West North Central | 32.0% | Ref | |
| East North Central | 25.7% | 1.30 (0.19 – 8.72) | |
| Mid Atlantic | 45.7% | 7.25 (0.70 – 75.40) | |
| New England | 75.0% | 3.67 (0.65 – 20.59) | |
| Pacific | 29.2% | 3.45 (0.23 – 51.54) | |
| South Atlantic | 36.7% | 1.67 (0.35 – 7.94) | |
| South Central | 41.5% | 10.61 (1.51 – 74.75) | |
| Hospital bed size | 0.55 | ||
| >499 | 24.7% | Ref | |
| <200 | 47.0% | 0.97 (0.13 – 7.04) | |
| 200–499 | 52.3% | 1.75 (0.51 – 6.03) |
Based on hierarchical, multivariate mixed effect logistic model
Content
Rate of inclusion of individual content elements is shown in Table 4, overall and by training level. Summaries uniformly included information about chief complaint, principal and secondary diagnoses and hospital course. Content relating specifically to heart failure was less commonly included, except for ejection fraction. A total of 1082 (74.6%) reported either baseline or new ejection fraction, 406 (27.1%) reported the cause of the heart failure exacerbation, 240 (16.0%) commented on discharge volume status, and 137 (9.1%) provided the discharge weight. Content important for transitional care was variable. A total of 1458 (97.1%) summaries included some information about discharge medications, but 461 (30.7%) summaries included any comment about discharge condition, 25 (1.7%) mentioned pending labs or explicitly noted there were none, and only 11 (0.8%) included a phone number of the discharging physician.
Table 4.
Content of discharge summary – overall and by training level
| Discharge summary content component | Overall (n=1501) | Trainee (n= 526) | Physician extender (n= 169) | Attending (n= 540) | Unknown (n= 266) | p Value |
|---|---|---|---|---|---|---|
| Chief complaint* † | 1495 (99.6) | 525 (99.8) | 169 (100.0) | 535 (99.1) | 266 (100.0) | 0.11 |
| Cause of exacerbation | 406 (27.1) | 174 (33.1) | 32 (18.9) | 104 (19.3) | 96 (36.1) | <0.01 |
| List of secondary diagnosis† | 1434 (95.54) | 500 (95.1) | 163 (96.5) | 514 (95.2) | 257 (96.6) | 0.68 |
| Hospital course* | 1459 (97.2) | 517 (98.3) | 166 (98.2) | 515 (95.4) | 261 (98.1) | 0.02 |
| Baseline weight | 45 (3.0) | 20 (3.8) | 9 (5.3) | 10 (1.9) | 6 (2.3) | 0.06 |
| Weight on admission | 179 (11.9) | 47 (8.9) | 35 (20.7) | 63 (11.7) | 34 (12.8) | <0.01 |
| Baseline ejection fraction* | 543 (36.2) | 227 (43.2) | 79 (46.8) | 187 (34.6) | 50 (18.8) | <0.01 |
| Study assessing ejection fraction during this visit | 822 (54.76) | 283 (53.8) | 80 (47.3) | 278 (51.5) | 181 (68.1) | <0.01 |
| New study result (n=822)* † | 757 (92.1) | 251 (88.7) | 76 (95.0) | 257 (92.5) | 173 (95.6) | 0.04 |
| Labs pending† | 25 (1.7) | 2 (0.4) | 5 (3.0) | 18 (3.3) | 0 (0.0) | <0.01 |
| Outpatient follow-up tests | 773 (51.5) | 249 (47.3) | 113 (66.9) | 348 (64.4) | 63 (23.7) | <0.01 |
| Attending name mentioned† | 1401 (93.3) | 482 (91.6) | 141 (83.4) | 523 (96.9) | 255 (95.9) | <0.01 |
| Attending signature included* | 1019 (72.7) | 418 (86.7) | 108 (76.6) | 481 (92.0) | 12 (4.7) | <0.01 |
| Attending phone included† | 12 (0.9) | 0 (0.0) | 4 (2.8) | 8 (1.5) | 0 (0.0) | <0.01 |
| Discharge status* | 461 (30.71) | 159 (30.2) | 63 (37.3) | 151 (28.0) | 88 (33.1) | 0.11 |
| Discharge vitals | 291 (19.4) | 83 (15.8) | 63 (37.3) | 106 (19.6) | 39 (14.7) | <0.01 |
| Discharge physical exam | 373 (24.9) | 119 (22.6) | 47 (27.8) | 132 (24.4) | 75 (28.2) | 0.28 |
| Discharge breathing | 275 (18.3) | 95 (18.1) | 41 (24.3) | 96 (17.8) | 43 (16.2) | 0.18 |
| Discharge volume status | 240 (16.0) | 83 (15.8) | 30 (17.8) | 84 (15.6) | 43 (16.2) | 0.92 |
| Discharge weight | 137 (9.1) | 33 (6.3) | 15 (8.9) | 52 (9.6) | 37 (13.9) | 0.01 |
| Discharge functional status | 98 (6.5) | 24 (4.6) | 14 (8.3) | 45 (8.3) | 15 (5.6) | 0.06 |
| Discharge cognitive status† | 118 (7.9) | 38 (7.2) | 14 (8.3) | 40 (7.4) | 26 (9.8) | 0.61 |
| Discharge medication list provided† | 1458 (97.1) | 512 (97.3) | 166 (98.2) | 522 (96.7) | 258 (97.0) | 0.74 |
| Admission medication list provided | 325 (21.7) | 180 (34.2) | 34 (20.1) | 91 (16.9) | 20 (7.5) | <0.01 |
| Both discharge and admission medication lists provided | 312 (20.8) | 176 (33.5) | 33 (19.5) | 84 (15.6) | 19 (7.1) | <0.01 |
Included in TJC composite
Included in TOCCC composite.
On average, summaries included 4.11 of 5 of TJC composite elements and 3.75 of 7 TOCCC composite elements. A total of 549 (36.6%) summaries included all of TJC composite elements whereas 0 (0%) summaries included all of the TOCCC composite elements. Of the hospitals which contributed more than 10 discharge summaries, the median hospital included 3.9 TJC composite elements (range: 2.9 – 4.8, p<0.001) and 3.6 TOCCC composite elements (range: 2.9 – 4.5, p<0.1) (Figure 3).
Figure 3.
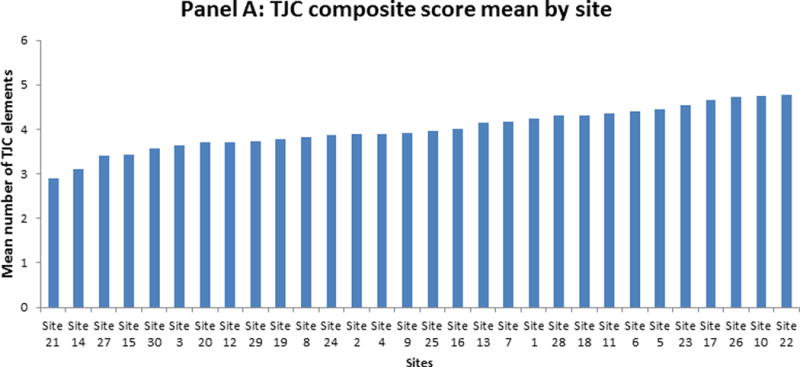
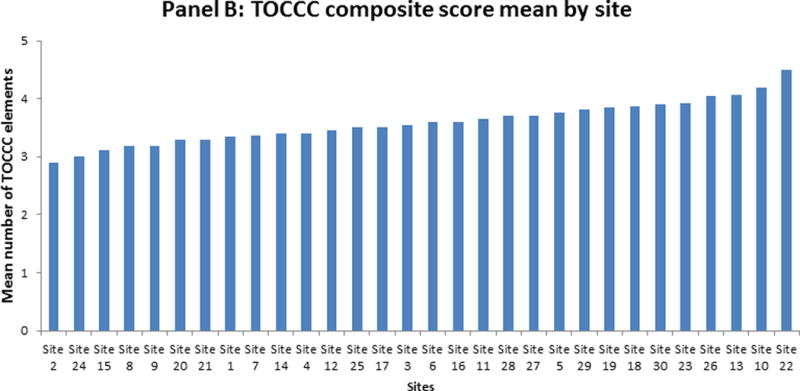
Composite score mean by site. Panel A: TJC, Panel B: TOCCC*
*Among hospitals with 10 or more summaries
TOCCC= transition of care consensus conference, TJC = The Joint Commission
In unadjusted analyses, timeliness and level of training were not associated with including more TJC composite elements. However, urban status and teaching status were significantly associated with TJC, such that metropolitan division hospitals and major teaching centers included the most TJC elements (p<0.001 for both). Moreover, rate of TJC composite inclusion showed significant variation across geographic regions (min: 3.76 New England, max: 4.42 South Atlantic, p<0.001). In a multivariate analysis adjusting for site random effects, urban status was the only predictor associated with TJC composite (Table 5).
Table 5.
Factors associated with including more elements recommended by The Joint Commission (TJC) mandate
| Explanatory variable | Mean number of TJC composite elements included | Parameter estimate (95% CI)* | Adjusted p value |
|---|---|---|---|
| Training level | 0.21 | ||
| Attending | 4.2 | Ref | |
| Trainee | 4.3 | 0.03 (−0.09 – 0.16) | |
| Physician extender | 4.1 | 0.13 (−0.02 – 0.27) | |
| Dictated on day of discharge | 0.06 | ||
| Yes | 4.2 | Ref | |
| No | 4.3 | 0.10 (−0.01 – 0.20) | |
| Length of stay (days) | — | −0.01 (−0.01–0.00) | 0.10 |
| Hospital location setting | 0.03 | ||
| Micropolis | 3.1 | Ref | |
| Metropolis | 4.1 | 1.03 (0.17 – 1.89) | |
| Metropolitan division | 4.2 | 0.75 (−0.21 – 1.72) | |
| Hospital teaching status | 0.36 | ||
| Minor | 4.0 | Ref | |
| Major | 4.3 | 0.33 (−0.15 – 0.81) | |
| Non-teaching | 3.8 | 0.10 (−0.46 – 0.66) | |
| Geographic region | 0.35 | ||
| New England | 3.8 | Ref | |
| East North Central | 4.1 | 0.36 (−0.32 – 1.05) | |
| Mid Atlantic | 3.9 | 0.26 (−0.55 – 1.08) | |
| Pacific | 3.8 | 0.63 (−0.25 – 1.51) | |
| South Atlantic | 4.4 | 0.51 (−0.08 – 1.10) | |
| South Central | 4.1 | 0.66 (−0.03 – 1.34) | |
| West North Central | 3.8 | 0.36 (−0.25 – 0.96) | |
| Hospital bed size | 0.99 | ||
| 200–499 | 4.1 | Ref | |
| <200 | 4.1 | −0.04 (−0.59 – 0.52) | |
| >499 | 4.1 | −0.01 (−0.44 – 0.42) |
Based on hierarchical, multivariate mixed effect linear model
In unadjusted analyses, discharge summaries completed on the day of the discharge included more TOCCC composite elements than summaries that were written after the day of discharge (mean TOCCC elements: 3.8 at discharge day vs. 3.7 after discharge day, p=0.02). Rates of TOCCC composite element inclusion did not differ by training level (3.75, 3.83 and 3.72, respectively, p=0.17). Hospitals located in a metropolitan area, major teaching centers and medium bed size hospitals had higher rates of TOCCC composite element inclusion (p<0.001 for all). Across geographic regions, discharge summaries showed considerable difference in rates of TOCCC element inclusion (min: 3.2 Mid Atlantic, max: 4.0 Pacific, p<0.001). In a multivariate analysis adjusting for site random effects, training level was the only significant predictor of TOCCC composite score. Attendings included fewer TOCCC composite elements than trainees and physician extenders (Table 6).
Table 6.
Factors associated with including more elements recommended by transition of care consensus conference (TOCCC)
| Explanatory variable | Mean number of TOCCC elements included | Parameter estimate (95% CI)* | Adjusted p value |
|---|---|---|---|
| Training level | 0.04 | ||
| Attending | 3.7 | Ref | |
| Physician extender | 3.8 | 0.12 (0.00 – 0.24) | |
| Trainee | 3.8 | 0.10 (0.00 – 0.21) | |
| Dictated on day of discharge | 0.92 | ||
| No | 3.7 | Ref | |
| Yes | 3.8 | 0.00 (−0.08 – 0.09) | |
| Length of Stay (days) | — | 0.00 (−0.01 – 0.00) | 0.43 |
| Hospital location setting | 0.23 | ||
| Metropolitan division | 3.7 | Ref | |
| Micropolis | 3.4 | 0.05 (−0.36 – 0.46) | |
| Metropolis | 3.8 | 0.11 (−0.60 – 0.82) | |
| Hospital teaching status | 0.26 | ||
| Non-teaching | 3.3 | Ref | |
| Major | 3.8 | 0.29 (−0.14 – 0.72) | |
| Minor | 3.7 | 0.05 (−0.36 – 0.46) | |
| Geographic region | 0.23 | ||
| Mid Atlantic | 3.2 | Ref | |
| East North Central | 3.4 | 0.18 (−0.40 – 0.76) | |
| New England | 3.8 | 0.38 (−0.22 – 0.98) | |
| Pacific | 4.0 | 0.69 (0.06 – 1.33) | |
| South Atlantic | 3.8 | 0.50 (−0.01 – 1.01) | |
| South Central | 3.5 | 0.41 (−0.15 – 0.97) | |
| West North Central | 3.8 | 0.33 (−0.25 – 0.91) | |
| Hospital bed size | 0.47 | ||
| >499 | 3.7 | Ref | |
| <200 | 3.5 | −0.04 (−0.52 – 0.45) | |
| 200–499 | 3.8 | 0.18 (−0.13 – 0.49) |
Based on hierarchical, multivariate mixed effect linear model
No discharge summary included all seven TOCCC-endorsed content elements, was dictated on the day of discharge, and was sent to a follow-up physician.
Discussion
In this multicenter study, we assessed discharge summaries completed for patients with heart failure across geographically and clinically diverse hospitals in the United States. Because hospitals have different practices regarding discharge summary timeliness, transmission and content, we predicted that there would be variation in discharge summary quality across these hospitals. We found that discharge summaries were prepared in a relatively timely manner; however, most of these discharge summaries did not include documentation of transmission to the follow-up outpatient physician. Furthermore, most of the included discharge summaries lacked details important for transitions of patients with heart failure such as condition at discharge and discharge weight. Compared to other health care providers, trainees were less likely to transmit discharge summaries to the outpatient physician, and attending hospitalists included less key content. No discharge summary met all three quality criteria of timeliness, transmission and content. Most importantly, we observed considerable variation among hospitals in their practices.
Our results about discharge summary quality are similar – though broader in scope – to those in several previous studies: like those, we found that most summaries were not timely, transmitted or comprehensive in content. In this study, though, we did observe substantial inter-hospital variation, spanning nearly the entire potential performance range. The range in hospital performance suggests that attention to transitional care processes might help produce consistently higher quality summaries. For example, prior research has suggested that early completion of discharge summaries is associated with increased comprehensiveness, more frequent transmission, and reductions in hospital readmissions.12, 26, 27 Other studies have focused on enhancing discharge summary content through the introduction of discharge summary templates, with a view to both providing structure for the summaries as well as decreasing their length.28–32 It has also been reported that automatic transmission to the follow-up physician may mitigate the failure of discharge summary dissemination and its effect on patient outcomes.4, 23, 33, 34 Unanticipated consequences are also possible. While physicians completing discharge summaries early may be more likely to recall details regarding patient care,26 mandating early completion may stress health care providers to prioritize discharge summaries over other important aspects of patient care, risking their premature completion.35
In our multicenter sample of discharge summaries, there were no differences in discharge summary timeliness across different levels of training. Compared with other health care providers, trainees were less likely to transmit discharge summaries and attending physicians included fewer TOCCC items. These findings are similar to those found in other single-center studies.13, 23, 26 For example, Kind et al found that trainees were less likely to include “future plan of care” components,26 and we previously found at our institution that trainees were less likely than hospitalists to transmit summaries and to include key content.23 Nonetheless, even attending physicians did not produce consistently high-quality discharge summaries. Collectively, these results suggest a need for quality improvement interventions, which might include a formal training process for discharge summary creation, institutional policy changes, audit/feedback or revision of electronic summary formats. Two recent studies examining discharge practices found that many trainees felt they lacked formal structured training about the discharge process, including the discharge documentation, with their learning depending mostly on instruction by other peer trainees and “learning by doing.”36, 37 Other health care providers, including physician extenders and attending physicians, have been reported as sharing these same concerns.38, 39 However, despite more general interest in improving discharge summary skills, available training curriculums and feedback interventions are still limited.35, 38, 40, 41
Several limitations and directions for future research should be considered when interpreting our findings. First, our study focused on omissions in content and was not designed to assess content accuracy, another important component of quality discharge summary.42, 43 Second, we used the TJC and TOCCC composites as proxies to assess the comprehensiveness of discharge summaries. Although these composites are endorsed by different specialty societies, their effect on patient outcomes is yet to be assessed. Moreover, some elements such as pending laboratory results, may only be included when relevant. We had no means of determining which patients actually had studies pending at discharge. Third, our sample of discharge summaries was completed for patients with heart failure and may not be generalizable to discharge summaries completed for patients with other conditions. Nevertheless, heart failure patients represent a cohort vulnerable to frequent hospital readmissions, and discharge documentation practices for this group have critical effect on transition of care and patient outcomes. Fourth, the reported discharge summary transmission rate may underestimate the actual transmission rate, as some institutions automatically transmit discharge summaries to follow-up physicians and may not note the transmission in the discharge summary. Or, physicians may have access to the summaries directly in the electronic record. As a result, we may have undercounted transmission to outside clinicians.
In conclusion, discharge summaries completed for patients with heart failure are limited in terms of timeliness, transmission and content across different sites. These summaries are more often used as a tool to document events during the hospital stay, yet they are inadequate in their details regarding transition of care, particularly with regard to heart failure. Our study provides impetus for improvements in discharge summary quality, and guidance for interventions attempting to improve these deficiencies.
Acknowledgments
The senior author (Dr. Horwitz) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. Dr. Horwitz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Sources of Funding
This project was supported by a grant (5 R01 HL080228) from the National Heart, Lung, and Blood Institute. Dr. Horwitz is supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. Dr. Krumholz is supported by grant U01 HL105270-04 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. No funding source had any role in the study design; in the collection, analysis, and interpretation of data; or in the writing of the report.
Footnotes
Disclosures
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that all authors have support from the Centers for Medicare & Medicaid Services for the submitted work. Dr. Krumholz is a recipient of research grants from Medtronic and from Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing and is chair of a cardiac scientific advisory board for UnitedHealth.
Journal subject codes: Ethics and policy: [100] Health policy and outcomes research, Heart Failure: [11] Other heart failure
References
- 1.Chen J, Dharmarajan K, Wang Y, Krumholz HM. National trends in heart failure hospital stay rates, 2001 to 2009. J Am Coll Cardiol. 2013;61:1078–88. doi: 10.1016/j.jacc.2012.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ziaeian B, Araujo KL, Horwitz LI. Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012;27:1513–1520. doi: 10.1007/s11606-012-2168-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roy CL, Poon EG, Karson AS, Ladak-Merchant Z, Johnson RE, Maviglia SM, Gandhi TK. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143:121–8. doi: 10.7326/0003-4819-143-2-200507190-00011. [DOI] [PubMed] [Google Scholar]
- 4.Moore C, McGinn T, Halm E. Tying up loose ends: discharging patients with unresolved medical issues. Ann Intern Med. 2007;167:1305–11. doi: 10.1001/archinte.167.12.1305. [DOI] [PubMed] [Google Scholar]
- 5.Sharma G, Fletcher KE, Zhang D, Kuo YF, Freeman JL, Goodwin JS. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. JAMA. 2009;301:1671–80. doi: 10.1001/jama.2009.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17:186–92. doi: 10.1046/j.1525-1497.2002.10741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Walraven C, Taljaard M, Etchells E, Bell CM, Stiell IG, Zarnke K, Forster AJ. The independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists. J Hosp Med. 2010;5:398–405. doi: 10.1002/jhm.716. [DOI] [PubMed] [Google Scholar]
- 8.Hansen LO, Strater A, Smith L, Lee J, Press R, Ward N, Weigelt JA, Boling P, Williams MV. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20:773–8. doi: 10.1136/bmjqs.2010.048470. [DOI] [PubMed] [Google Scholar]
- 9.Bell CM, Schnipper JL, Auerbach AD, Kaboli PJ, Wetterneck TB, Gonzales DV, Arora VM, Zhang JX, Meltzer DO. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24:381–6. doi: 10.1007/s11606-008-0882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Damluji MS, Dzara K, Hodshon B, Punnanithinont N, Krumholz HM, Chaudhry SI, Horwitz LI. Association of discharge summary quality with readmission risk for patients hospitalized with heart failure exacerbation. Circ Card Qual Outcomes. doi: 10.1161/CIRCOUTCOMES.114.001476. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–41. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 12.Horwitz LI, Jenq GY, Brewster UC, Chen C, Kanade S, Van Ness PH, Araujo KL, Ziaeian B, Moriarty JP, Fogerty RL, Krumholz HM. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013;8:436–43. doi: 10.1002/jhm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Were MC, Li X, Kesterson J, Cadwallader J, Asirwa C, Khan B, Rosenman MB. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24:1002–6. doi: 10.1007/s11606-009-1057-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walz SE, Smith M, Cox E, Sattin J, Kind AJ. Pending laboratory tests and the hospital discharge summary in patients discharged to sub-acute care. J Gen Intern Med. 2011;26:393–8. doi: 10.1007/s11606-010-1583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaudhry SI, Wang Y, Concato J, Gill TM, Krumholz HM. Patterns of weight change preceding hospitalization for heart failure. Circulation. 2007;116:1549–54. doi: 10.1161/CIRCULATIONAHA.107.690768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson S, Ruscoe W, Chapman M, Miller R. General practitioner-hospital communications: a review of discharge summaries. J Qual Clin Pract. 2001;21:104–8. doi: 10.1046/j.1440-1762.2001.00430.x. [DOI] [PubMed] [Google Scholar]
- 17.Were MC, Li X, Kesterson J, Cadwallader J, Asirwa C, Khan B, Rosenman MB. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow-up providers. J Gen Intern Med. 2009;24:1002–6. doi: 10.1007/s11606-009-1057-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walz SE, Smith M, Cox E, Sattin J, Kind AJ. Pending laboratory tests and the hospital discharge summary in patients discharged to sub-acute care. J Gen Intern Med. 2011;26:393–8. doi: 10.1007/s11606-010-1583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Walraven C, Seth R, Laupacis A. Dissemination of discharge summaries. Not reaching follow-up physicians. Can Fam Physician. 2002;48:737–42. [PMC free article] [PubMed] [Google Scholar]
- 20.Kind AJH, Smith MA. Documentation of Mandated Discharge Summary Components in Transitions from Acute to Subacute Care. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 2: Culture and Redesign) Rockville (MD): 2008. [PubMed] [Google Scholar]
- 21.Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301–9. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaudhry SI, Barton B, Mattera J, Spertus J, Krumholz HM. Randomized trial of Telemonitoring to Improve Heart Failure Outcomes (Tele-HF): study design. J Card Fail. 2007;13:709–14. doi: 10.1016/j.cardfail.2007.06.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwitz LI, Jenq GY, Brewster UC, Chen C, Kanade S, Van Ness PH, Araujo KL, Ziaeian B, Moriarty JP, Fogerty RL, Krumholz HM. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med: an official publication of the Society of Hospital Medicine. 2013;8:436–43. doi: 10.1002/jhm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joint Commission on Accreditation of Healthcare Organizations. Hospital Accreditation Standards Standard IM 6.10 EP 7–9. Oakbrook Terrace, Ill: TJC; 2008. [Google Scholar]
- 25.Snow V, Beck D, Budnitz T, Miller DC, Potter J, Wears RL, Weiss KB, Williams MV. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24:971–6. doi: 10.1007/s11606-009-0969-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kind AJ, Thorpe CT, Sattin JA, Walz SE, Smith MA. Provider characteristics, clinical-work processes and their relationship to discharge summary quality for sub-acute care patients. J Gen Intern Med. 2012;27:78–84. doi: 10.1007/s11606-011-1860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li JY, Yong TY, Hakendorf P, Ben-Tovim D, Thompson CH. Timeliness in discharge summary dissemination is associated with patients’ clinical outcomes. J Eval Clin Pract. 2013;19:76–9. doi: 10.1111/j.1365-2753.2011.01772.x. [DOI] [PubMed] [Google Scholar]
- 28.Rao P, Andrei A, Fried A, Gonzalez D, Shine D. Assessing quality and efficiency of discharge summaries. Am J Med Qual. 2005;20:337–43. doi: 10.1177/1062860605281078. [DOI] [PubMed] [Google Scholar]
- 29.Callen JL, Alderton M, McIntosh J. Evaluation of electronic discharge summaries: a comparison of documentation in electronic and handwritten discharge summaries. Int J Med Inform. 2008;77:613–20. doi: 10.1016/j.ijmedinf.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 30.Santana MJ, Holroyd-Leduc J, Flemons WW, O’Beirne M, White D, Clayden N, Forster AJ, Ghali WA. The Seamless Transfer of Care: A Pilot Study Assessing the Usability of an Electronic Transfer of Care Communication Tool. Am J Med Qual. 2014;29(6):476–83. doi: 10.1177/1062860613503982. [DOI] [PubMed] [Google Scholar]
- 31.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med: an official publication of the Society of Hospital Medicine. 2007;2:314–23. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 32.Maslove DM, Leiter RE, Griesman J, Arnott C, Mourad O, Chow CM, Bell CM. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Intern Med. 2009;24:995–1001. doi: 10.1007/s11606-009-1053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17:186–92. doi: 10.1046/j.1525-1497.2002.10741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Walraven C, Seth R, Laupacis A. Dissemination of discharge summaries. Not reaching follow-up physicians. Can Fam Physician. 2002;48:737–42. [PMC free article] [PubMed] [Google Scholar]
- 35.Bischoff K, Goel A, Hollander H, Ranji SR, Mourad M. The Housestaff Incentive Program: improving the timeliness and quality of discharge summaries by engaging residents in quality improvement. BMJ Qual Saf. 2013;22:768–74. doi: 10.1136/bmjqs-2012-001671. [DOI] [PubMed] [Google Scholar]
- 36.Greysen SR, Schiliro D, Curry L, Bradley EH, Horwitz LI. “Learning by doing”–resident perspectives on developing competency in high-quality discharge care. J Gen Intern Med. 2012;27:1188–94. doi: 10.1007/s11606-012-2094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. “Out of sight, out of mind”: housestaff perceptions of quality-limiting factors in discharge care at teaching hospitals. J Hosp Med: an official publication of the Society of Hospital Medicine. 2012;7:376–81. doi: 10.1002/jhm.1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mohta N, Vaishnava P, Liang C, Ye K, Vitale M, Dalal A, Schnipper J. The effects of a ‘discharge time-out’ on the quality of hospital discharge summaries. BMJ Qual Saf. 2012;21:885–90. doi: 10.1136/bmjqs-2011-000441. [DOI] [PubMed] [Google Scholar]
- 39.Davis MM, Devoe M, Kansagara D, Nicolaidis C, Englander H. “Did I do as best as the system would let me?” healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27:1649–56. doi: 10.1007/s11606-012-2169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Myers JS, Jaipaul CK, Kogan JR, Krekun S, Bellini LM, Shea JA. Are discharge summaries teachable? The effects of a discharge summary curriculum on the quality of discharge summaries in an internal medicine residency program. Acad Med. 2006;81:S5–8. doi: 10.1097/01.ACM.0000236516.63055.8b. [DOI] [PubMed] [Google Scholar]
- 41.Flyer B, Rubenstein LZ, Robbins AS, Wieland GD, Henry D, Cugalj N. An intervention to improve the hospital discharge summary. J Med Educ. 1988;63:407–9. doi: 10.1097/00001888-198805000-00010. [DOI] [PubMed] [Google Scholar]
- 42.McMillan TE, Allan W, Black PN. Accuracy of information on medicines in hospital discharge summaries. Intern Med J. 2006;36:221–5. doi: 10.1111/j.1445-5994.2006.01028.x. [DOI] [PubMed] [Google Scholar]
- 43.Callen J, McIntosh J, Li J. Accuracy of medication documentation in hospital discharge summaries: A retrospective analysis of medication transcription errors in manual and electronic discharge summaries. Int J Med Inform. 2010;79:58–64. doi: 10.1016/j.ijmedinf.2009.09.002. [DOI] [PubMed] [Google Scholar]


