Although severe lower extremity peripheral arterial disease affects more than 12 million people in the United States,1,2 secular trends in the risk of amputation remain unexplored in recent years. Using national billing and survey data sets from the Centers for Medicare and Medicaid Services and the Behavioral Risk Factor Surveillance System, we examined trends in lower extremity amputation rates, diagnostic and therapeutic vascular procedures, and the use of preventive measures aimed at limiting the use of amputation procedures in the United States between 1996 and 2011.
Methods
We used Centers for Medicare and Medicaid Services claims to calculate rates of lower limb amputation between 1996 and 2011. Amputation procedures were categorized as above-knee, below-knee, and minor amputations. We included only the most proximal amputation per patient in any 1 year during the study period. Next, we calculated the number of revascularization procedures performed per 100 000 Medicare patients during the same time period, categorized as diagnostic lower extremity angiograms, endovascular lower extremity diagnostic and therapeutic interventions (such as angioplasty, stenting, or atherectomy), and lower extremity bypass surgery. Finally, we used data from the Behavioral Risk Factor Surveillance System(from 1996 to 1999) and Medicare beneficiary surveys (from 2000 to 2011) to examine secular trends in the prevalence of smoking and self-reported diabetes mellitus among patients older than 65 years of age, as well as rates of weekly glucose testing and annual foot examinations from a physician for diabetic patients. Frequency proportions were calculated by year, and significant changes were identified using nonparametric tests of trend. For our study, exemption from institutional board approval was granted.
Results
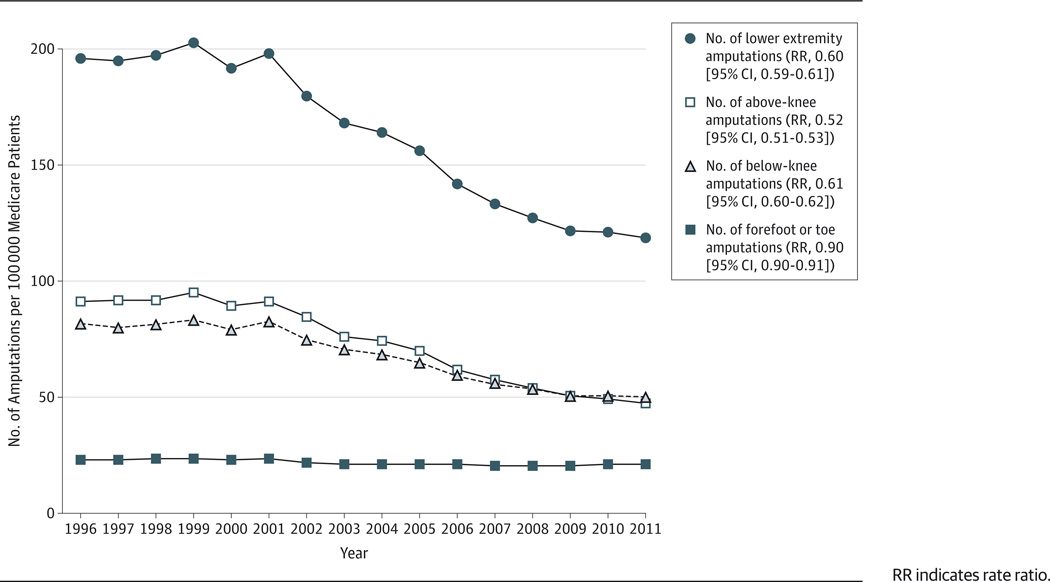
From1996 to 2011, the rate of lower limb amputations decreased by 45%, from196 to 119 procedures per 100 000 patients (rate ratio [RR], 0.60 [95% CI, 0.59–0.61]; P < .001) (Figure 1). These changes were driven by a 48%decrease in the rate of above-knee amputations (from91 to 47 procedures per 100 000 patients; RR, 0.52 [95% CI, 0.51–0.52]; P < .001) and a 39% decrease in the rate of below-knee amputations (from82 to 50 procedures per 100 000 patients; RR, 0.61 [95% CI, 0.60–62];P < .001). Rates of minor amputations (toe or forefoot) also decreased slightly during the study period (from 23 to 21 procedures per 100 000 patients; RR, 0.90 [95% CI, 0.90–0.91]; P = .01). While overall rates of amputation decreased during the study period, amputations remained common in high-risk subgroups such as African American patients with diabetes (555 procedures per 100 000 African American patients in 2011), especially when compared with low-risk subgroups (24 procedures per 100 000 nonblack, nondiabetic patients).
Figure 1.
Trends in Major Amputation, by Amputation Type and Year, 1996–2011
RR indicates rate ratio.
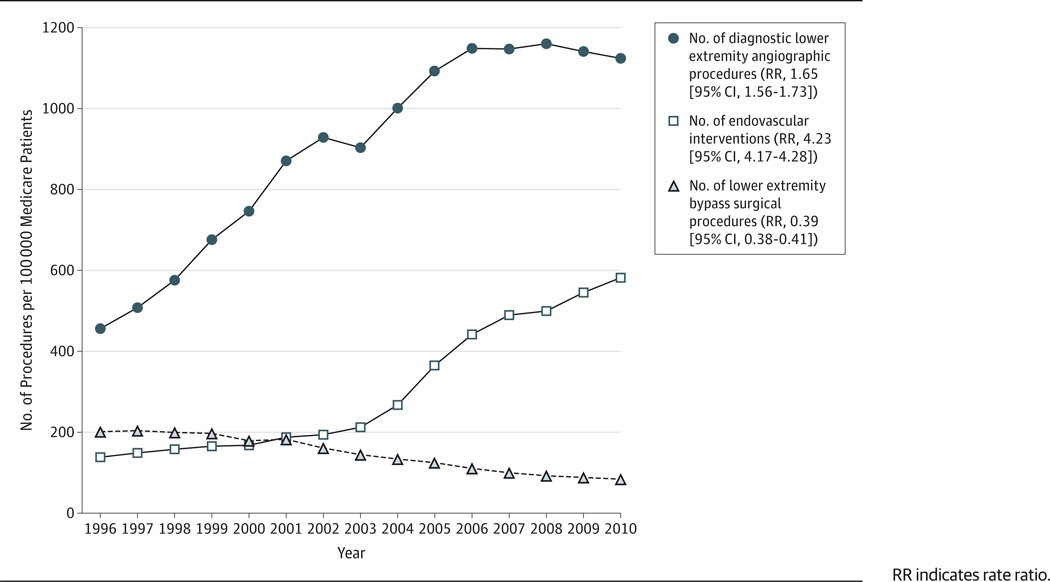
Use of peripheral endovascular interventions also increased during the study period (Figure 2). For example, the rate of diagnostic lower extremity arteriographic procedures increased by 165% from 1996 to 2011 (from 451 to 1124 procedures per 100 000 patients; RR, 1.65 [95% CI, 1.56–1.73]; P < .001). The rate of therapeutic endovascular interventions increased significantly as well (from138 to 584 interventions per 100 000 patients; RR, 4.23 [95% CI, 4.17–4.28]; P < .001). The rate of surgical bypass procedures decreased by 61%(from 201 to 83 procedures per 100 000 patients; RR, 0.39 [95% CI, 0.38–0.41]; P < .001).
Figure 2.
Trends in Diagnostic Angiography, Therapeutic Endovascular Interventions, and Lower Extremity Bypass Surgery, 1996–2010
RR indicates rate ratio.
Last, the prevalence of diabetes increased from 1996 to 2010 (from 16 to 26 cases per 100 patients; RR, 1.53 [95% CI, 1.23–1.91]), while the smoking rate remained unchanged (14 smokers per 100 patients; RR, 1.08 [95% CI, 0.96–1.21]). However, the use of preventive measures aimed at limiting the use of amputation procedures increased significantly; the number of diabetic patients treated with a routine foot examination increased by 70% (from40 to 68 diabetic patients per 100 patients; RR, 1.70 [95% CI, 1.13–2.57]), and routine blood glucose testing increased by 76%(from 41 to 72 tests per 100 patients; RR, 1.76 [95% CI, 1.03–3.02]).
Discussion
The lower limb amputation rate has decreased by 45% over the last 15 years among Medicare patients, and the largest improvements have occurred in above- or below-knee amputations. During this same time period, significant increases have also occurred in the use of vascular procedures (both diagnostic and therapeutic) and preventive care.
Our observational findings cannot imply causation, and we recognize that our study presents no direct causative experimental evidence to explain the decrease in amputation risk. However, it is evident that the increasing use of vascular and preventive care, especially among patients with diabetes, has been temporally associated with lower rates of major amputation.3 While many debate whether open surgery, endovascular interventions, or hybrid strategies are most effective in limiting amputation,4,5 the importance of preventive measures has likely been underestimated. Future work examining relationships between preventive measures, revascularization, and amputation is necessary to help clinicians better define optimal strategies for limiting amputation.
Acknowledgments
Funding/Support: Dr Goodney was supported by a Career Development Award (K08HL05676-01) from the National Heart, Lung, and Blood Institute and a supplemental award from the Society for Vascular Surgery Foundation.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Goodney had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Goodney, Tarulli, Zwolak.
Acquisition, analysis, or interpretation of data: Goodney, Tarulli, Faerber, Schanzer.
Drafting of the manuscript: Goodney, Tarulli.
Critical revision of the manuscript for important intellectual content: Goodney, Faerber, Schanzer, Zwolak.
Statistical analysis: Goodney, Faerber.
Obtained funding: Goodney.
Administrative, technical, or material support: All authors.
Study supervision: Goodney, Zwolak.
Conflict of Interest Disclosures: None reported.
Contributor Information
Philip P. Goodney, Section of Vascular Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire; VA Outcomes Group, White River Junction, Vermont; Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth Medical School, Hanover, New Hampshire.
Massimo Tarulli, Section of Vascular Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire.
Adrienne E. Faerber, Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth Medical School, Hanover, New Hampshire.
Andreas Schanzer, Section of Vascular Surgery, University of Massachusetts School of Medicine, Worcester.
Robert M. Zwolak, Section of Vascular Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire; VA Outcomes Group, White River Junction, Vermont.
References
- 1.Hirsch AT, Murphy TP, Lovell MB, et al. Peripheral Arterial Disease Coalition. Gaps in public knowledge of peripheral arterial disease: the first national PAD public awareness survey. Circulation. 2007;116(18):2086–2094. doi: 10.1161/CIRCULATIONAHA.107.725101. [DOI] [PubMed] [Google Scholar]
- 2.Hirsch AT, Haskal ZJ, Hertzer NR, et al. American Association for Vascular Surgery; Society for Vascular Surgery; Society for Cardiovascular Angiography and Interventions; Society for Vascular Medicine and Biology; Society of Interventional Radiology; ACC/AHA Task Force on Practice Guidelines Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease; American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; Vascular Disease Foundation. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; Vascular Disease Foundation. Circulation. 2006;113(11):e463–e654. doi: 10.1161/CIRCULATIONAHA.106.174526. [DOI] [PubMed] [Google Scholar]
- 3.Goodney PP, Holman K, Henke PK, et al. Regional intensity of vascular care and lower extremity amputation rates. J Vasc Surg. 2013;57(6):1471–1480. doi: 10.1016/j.jvs.2012.11.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adam DJ, Beard JD, Cleveland T, et al. BASIL trial participants. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366(9501):1925–1934. doi: 10.1016/S0140-6736(05)67704-5. [DOI] [PubMed] [Google Scholar]
- 5.Conte MS. Diabetic revascularization: endovascular versus open bypass—do we have the answer? Semin Vasc Surg. 2012;25(2):108–114. doi: 10.1053/j.semvascsurg.2012.04.004. [DOI] [PubMed] [Google Scholar]