Abstract
Objective
To assess how a checklist reminding clinicians to deliver a bundled intervention affects contraceptive knowledge and use 3 months after women seek walk-in pregnancy testing.
Methods
Pre-intervention, an inner-city family planning clinic provided unstructured care; during the intervention period, clinic staff used a checklist to ensure women received needed services. Women seeking walk-in pregnancy testing who wished to avoid pregnancy for at least 6 months were asked to complete surveys about their contraceptive knowledge and use immediately after and 3-months after visiting the study clinic. To assess the significance of changes over time, we used logistic regression models.
Results
Between January 2011 and May 2013, over 1500 women sought pregnancy testing from the study clinic; 323 completed surveys (95 pre-intervention and 228 during the intervention period). With this checklist intervention, participants were more likely to receive emergency contraception (EC) (22% vs. 5%, aOR=4.64, 95% CI 1.77-12.17), have an intrauterine device or implant placed at the time of their clinic visit (5% vs. 0%, p=0.02), or receive a contraceptive prescription (23% vs. 10%, p<0.001). Three months after visiting the study clinic, participants from the intervention period were more knowledgeable about intrauterine and subdermal contraception and were more likely to be using intrauterine, subdermal or injectable contraception (aOR=2.18, 95% CI 1.09-4.35).
Conclusions
Women seeking walk-in pregnancy testing appear more likely to receive EC and to have switched to a more effective form of birth control in 3 months following their visit when clinic staff used a 3-item checklist and provided scripted counseling.
Implications
A checklist reminding clinic staff to assess pregnancy intentions, provide scripted counseling about both emergency and highly-effective reversible contraception, and offer same-day contraceptive initiation to women seeking walk-in pregnancy testing appears to increase use of more effective contraception.
Keywords: Pregnancy testing, checklist, contraceptive counseling, emergency contraception, Intrauterine Contraception
Introduction
The incidence of unintended pregnancy is one indicator of a society's reproductive health. Unintended childbearing is associated with several negative maternal and child health outcomes.(1) Thus, the US Department of Health and Human Services' Healthy People 2020 initiative includes the goal of reducing the incidence of unintended pregnancy.(2) Unfortunately, this goal has been difficult to achieve, with recent data indicating that unintended pregnancy rates have increased to 51% of US pregnancies. (3) In addition, disparities in unintended pregnancy have also increased, with the most vulnerable women facing the highest rates of unintended pregnancy.(3)
While the majority of unplanned pregnancies in the US occurred to women who were not using any method of contraception in the month they conceived,(4, 5) more than 40% of women with unplanned pregnancies conceived after using contraception inconsistently or incorrectly.(5) Women seeking pregnancy testing are at particularly high risk for recent contraceptive difficulties. In a prior study of women seeking walk-in pregnancy testing, most reported trying to avoid pregnancy and almost 40% were found to have potentially benefited from same-day emergency contraception (EC). (6) Another recent study found that among women who presented for walk-in pregnancy testing, 12-24% indicated they might be interested in same-day placement of an intrauterine device (IUD).(7) The purpose of this study was therefore to examine how a checklist which reminded clinic staff caring for women seeking pregnancy testing to: (a) assess pregnancy intentions, (b) provide structured contraceptive counseling, and (c) offer same-day contraceptive initiation to women wishing to avoid pregnancy affected women's subsequent contraceptive knowledge and use.
Methods
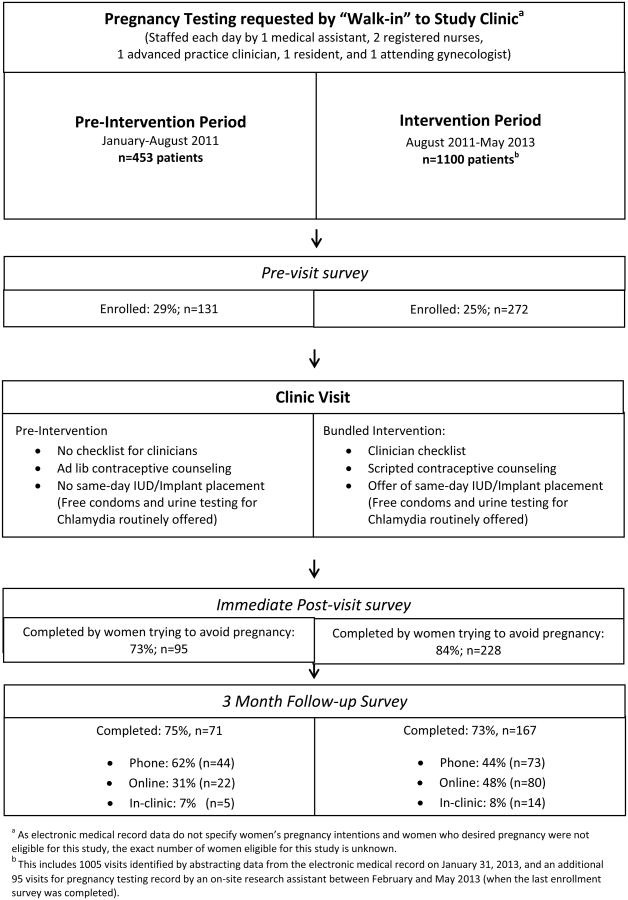
We studied the effects of this bundled intervention in an inner-city Title X-funded family planning clinic using a pre/post design (Figure 1). Women who were found to be pregnant, using an IUD or implant, at the time of their clinic visit, or had undergone tubal ligation were not eligible for this study. Women who reported that they desired (or “wouldn't mind”) pregnancy in the next 6 months were excluded from analyses of survey data.
Figure 1. Study Flow.
During the pre-intervention period (January to August 2011) women seeking walk-in pregnancy testing received “usual care” which simply included the pregnancy test that the woman requested without structured contraceptive. During the pre-intervention period contraceptive counseling was not discouraged, but occurred sporadically in an unstructured fashion, without same-day placement of IUDs or implants.
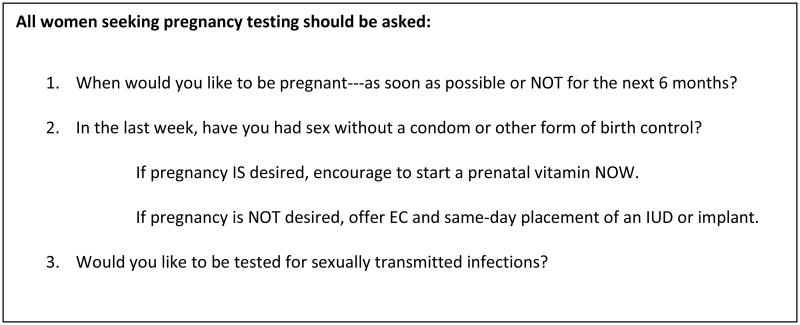
During the intervention period (August 2011 to May 2013) a checklist (Figure 2) was used to remind clinic staff to deliver a bundled intervention which began by asking women seeking walk-in pregnancy testing about their pregnancy intentions and when they last had unprotected intercourse. Those who wished to avoid pregnancy and reported recent unprotected intercourse were offered EC and all women who wished to avoid pregnancy received scripted contraceptive counseling about highly effective reversible contraception (Appendix 1), with the offer of same-day placement of an IUD or implant. However, same-day placement of an IUD was limited to women who reported no unprotected intercourse during the 8-14 days prior to their clinic visit (due to concerns of luteal phase pregnancy), and to women who had no evidence of cervicitis on exam. As a resident training clinic staffed by a large pool of individuals who work in multiple clinical settings, the study clinic regularly experienced staff turnover during both the pre-intervention and intervention periods (i.e., over the course of this study, the clinic was staffed by a total of 10 medical assistants, 22 registered nurses, 5 advance practice clinicians, 16 residents and 17 attending gynecologists).
Figure 2. Pregnancy testing checklist.
On the day of their clinic visit, all patients were invited to participate in this study by clinic staff. Patients who expressed interest in participating were referred to an on-site research assistant (the same individual during both study periods) who discussed the study with potential participants in detail. Those who provided signed informed consent (during both the pre-intervention and intervention periods) completed surveys which asked about the counseling and contraceptive services received during their clinic visit. In addition, the surveys assessed women's contraceptive knowledge with nine questions regarding the effectiveness, reversibility, and contraceptive duration for IUDs, implants and injectable contraception.(8) Before each participant left the study clinic, the on-site research assistant recorded whether participants had received EC, an IUD or implant.
Three months after study enrollment, participants again completed surveys assessing their contraceptive knowledge and use. Most follow-up surveys were completed by phone, although participants also had the option of completing the survey in person or using the internet (Figure 1). Participants were offered a small token of appreciation (worth approximately $5) for survey completion immediately after their clinic visit and $10 for completing the follow-up survey.
We used descriptive statistics to characterize the sociodemographic and reproductive characteristics of participants who completed surveys, using Chi-square tests, and Fisher exact tests when cells were small (i.e., n<5), to compare differences between the pre-intervention and intervention periods. We performed multivariable logistic regression, adjusting for theoretically relevant factors that differed significantly between groups: age, race, insurance status, and use of no method of contraception prior to visiting the study clinic, when considering the effect of study period on survey data regarding (a) receipt of emergency contraception at the time of clinic visit (b) use of highly effective reversible contraception (an IUD, implant, or injectable contraception) three months after clinic visit, and (c) use of a more effective method of contraception three months after initial clinic visit. To assess use of a more effective method three months after clinic visit, we created a dichotomous variable indicating whether participants reported using a contraceptive method at 3-month follow-up that was more effective than the method they reported using prior to their clinic visit with the following hierarchy of contraceptive effectiveness: no method < withdrawal<condoms < pill/patch/ring < injectable, IUD/implant. We also examined models with all variables shown in Table 1, and used stepwise elimination to create a parsimonious model from this full model (data not shown), both of which produced qualitatively similar results.
Table 1. Baseline sociodemographic and reproductive characteristics of women who completed surveys after seeking walk-in pregnancy testing.
| Pre-Intervention Group (n=95) | Intervention Group (n=228) | p-value | |
|---|---|---|---|
| Age mean, standard deviation | 21.4 (5.4) | 22.0 (5.1) | 0.35 |
| Race | |||
| Black | 70.5% (67) | 78.5% (179) | 0.12 |
| White | 20.0% (19) | 9.7% (22) | 0.01 |
| Bi-racial/Other | 9.5% (9) | 11.8% (27) | 0.55 |
| Health insurance | |||
| Public | 58.9% (56) | 75.4% (172) | 0.003 |
| Private | 11.6% (11) | 9.6% (22) | 0.59 |
| None/ No Answer | 29.5% (28) | 14.9% (34) | 0.002 |
| Committed Relationshipa | 53.7% (51) | 51.3% (117) | 0.70 |
| Employment status | |||
| Does not work | 51.6% (49) | 48.7% (111) | 0.63 |
| Work Full-time | 20.0% (19) | 16.2% (37) | 0.41 |
| Work Part-time | 26.3% (25) | 32.0% (73) | 0.31 |
| Education level | |||
| No high school degree | 34.8% (33) | 26.8% (61) | 0.15 |
| High school grad or GED | 33.7% (32) | 41.7% (95) | 0.18 |
| Some college /2 yr degree | 27.4% (26) | 28.9% (66) | 0.79 |
| College degree | 4.2% (4) | 1.3% (3) | 0.20b |
| Household income | |||
| <$5,000 | 14.7% (14) | 17.5% (40) | 0.54 |
| $5,000 to 20,000 | 24.2% (23) | 30.3% (69) | 0.27 |
| More than $20,000 | 7.4% (7) | 7.9% (18) | 0.89 |
| Don't know/No Answer | 53.7% (51) | 44.3% (101 | 0.12 |
| Pregnancy history | |||
| Prior pregnancy | 51.6% (49) | 56.1% (128) | 0.46 |
| Prior unwanted pregnancy | 31.6% (30) | 36.0% (82) | 0.45 |
| Most effective contraceptive used with last intercourse | |||
| None | 36.8% (35) | 48.7% (111) | 0.05 |
| Rhythm/Withdrawal | 8.4% (8) | 6.6% (15) | 0.57 |
| Condoms | 33.7% (32) | 29.4% (67) | 0.45 |
| Pills | 9.5% (9) | 5.7% (13) | 0.22 |
| Shot | 6.3% (6) | 7.5% (17) | 0.71 |
| Ring | 1.1% (1) | 1.3% (3) | 0.99b |
| No answer | 4.2% (4) | 0.9% (2) | 0.06b |
Includes a few women who reported being formally married
Fishers Exact test used when cell value <5
Deidentified electronic medical record (EMR) data abstracted on January 31, 2013 by an honest broker allowed us to assess receipt of contraceptive prescriptions, and placement of IUDs and implants during the two study periods by all women served by the study clinic. In cleaning this EMR data, we excluded visits with positive pregnancy test results. Analysis of EMR data was separate from all analysis of survey data. All analyses were performed using Stata 13.0 (StataCorp. College Station, TX). This study was approved by the Institutional Review Board of the University of Pittsburgh.
Results
During the pre-intervention period, surveys were completed by 131 women seeking walk-in pregnancy testing; during the intervention period, another 272 women completed surveys. The demographic characteristics of women who completed surveys were similar to those of all women served by the study clinic (Table 1 and Appendix Table 1). After excluding those who “wouldn't mind getting pregnant” (36 pre-intervention and 44 in the intervention period), data were available from 323 participants. Of these, 3-month follow-up surveys were completed by 74% (71 women pre-intervention and 167 of the intervention group), Figure 1.
Participants enrolled during the pre-intervention and intervention periods had similar sociodemographic characteristics, although during the intervention period more participants reported public insurance and during the pre-intervention period were more likely to have no high school degree (Table 1). The reproductive characteristics and recent contraceptive use of women served by the study clinic during the pre-intervention and intervention periods were also similar, although during the intervention period there was a trend towards more women reporting use of no form of contraception at last intercourse (48.7% vs 36.8% p=0.05).
During the intervention period, women seen by the study clinic appear more likely to report receipt of contraceptive counseling (p< 0.001), and to have greater knowledge regarding the effectiveness, duration of use and reversibility of intrauterine and intradermal contraception immediately after their clinic visit (P<0.05 for all), though knowledge regarding the injection did not significantly change compared to the pre-intervention period. In addition, women seen by the clinic appear more likely to report receipt of EC (22% vs 5%, p<0.001) and same-day placement of an IUD or subdermal implant (Table 2). Even after adjusting for having used no method prior to visiting the study clinic (Table 3), women remained significantly more likely to have received EC during the intervention than pre-intervention period (aOR=4.66 (1.76-12.35). Data abstracted from the EMR confirmed these increases in provision of contraception (Table 4).
Table 2. Change in contraceptive use following request for pregnancy testing from study clinic.
| Immediately after Clinic Visit | Pre-intervention Group (n=95) | Intervention Group (n=228) | P-Value |
|---|---|---|---|
| Received EC | 5.3% (5) | 21.9% (50) | <0.001 |
| IUD placed | 0.0% (0) | 4.4% (10) | 0.04 |
| Implant placed | 0.0% (0) | 0.9% (2) | 0.99c |
|
| |||
| 3-Month Follow-up | (n=71)a | (n=167)a | |
|
| |||
| Highly effective reversible | |||
| contraception at last intercourseb | 18.3% (13) | 32.4% (54) | 0.03 |
| Switched from none to any method | 16.9% (12) | 39.5% (66) | <0.001 |
| Switched to more effective method | 26.8% (19) | 49.7% (83) | 0.001 |
| Any condom use | 63.4% (45) | 59.9% (100) | 0.61 |
Surveys were completed by 95 women during the pre-intervention period and 228 women during the intervention period; however, loss to follow up at 3-months was 25% during the pre-intervention period and 27% during the intervention period.
Highly effective reversible contraceptives include intrauterine, subdermal, and injectable contraception.
Fishers Exact used when cell value <5
Table 3. Intervention effects on EC use on day of clinic visit and contraceptive use 3 months latera.
| EC dispensed at visit (n=323c) OR (95% CI) | Using highly effective reversible contraception at 3 month follow up (n=238d) OR (95% CI) | Changed to a more effective contraceptive by 3 month follow upb (n=238d) OR (95% CI) | |
|---|---|---|---|
| Interventione (vs. Pre-intervention) | 4.66 (1.76-12.35) | 1.91 (0.94-3.90) | 2.02 (1.03-3.96) |
| Teen (vs. 20+) | 1.29 (0.70-2.38) | 1.13 (0.63-2.03) | 0.93 (0.52-1.66) |
| Non-white (vs. White) | 0.88 (0.33-2.36) | 1.93 (0.69-5.40) | 1.45 (0.59-3.59) |
| Insured (vs. not) | 1.18 (0.50-2.75) | 1.97 (0.86-4.55) | 1.08 (0.51-2.28) |
| No Method prior to visit (vs. any method prior) | 3.12 (1.65-5.88) | 0.81 (0.45-1.47) | 5.67 (3.18-10.11) |
Each column header reflects a dependent dichotomous outcome for which a multivariable logistic regression model was created with all variables shown in table rows included as independent predictor variables.
As compared to the method they used prior to seeking pregnancy testing from the study clinic.
Participants who completed surveys immediately after their clinic visit contributed data to this model from both the pre-intervention (n=95) and intervention (n=228) periods.
Participants who completed surveys 3-months after their enrollment clinic visit contributed data to this model from both the pre-intervention (n=71) and intervention (n=167) periods.
Data shown in this row reflects the odds of a change in the outcome specified by each column's header during the intervention period compared to the pre-intervention period. The comparison groups for the rows that follow are indicated in parentheses.
Table 4. Contraceptive dispensing to all patients who requested pregnancy testing from the study clinica.
| Pre-intervention period (n=453) % (n) | Intervention period (n=1005) % (n) | P-Value b | |
|---|---|---|---|
| Received EC | 5.5% (25) | 9.7% (97) | 0.007 |
| Prescribed contraception | 10.4% (47) | 23.1% (232) | <0.001 |
| IUD placed | 0.2% (1) | 1.1% (11) | 0.12 |
| Implant placed | 0.0%(0) | 0.0%(0) | - |
Data extracted from the electronic medical record do not allow determination of whether women desired pregnancy at the time they requested pregnancy testing from the study clinic. Women were only eligible to complete surveys as part of this study if they were wished to avoid pregnancy for at least 6 months at the time they sought pregnancy testing. Of women who visited the clinic during the intervention period, 25% completed surveys at the time of their clinic visit.
From chi-square tests and Fishers Exact test when any cell value <5.
Three months after visiting the study clinic, participants from the intervention period were more likely to be using an IUD, implant or injectable contraceptive (32% vs. 18% pre-intervention, p=0.03), and no less likely to use condoms (Table 2). After adjusting for potential confounders (Table 3), women who visited the clinic during the intervention period were more likely than those from the pre-intervention period to report at 3-month follow-up a method of contraception more effective than the method they used prior to seeking pregnancy testing from the study clinic (aOR=2.02, 95% CI 1.03-3.96).
Discussion
This study of women seeking walk-in pregnancy testing from an inner-city family planning clinic found that when clinic staff used a checklist to assess women's needs for other services and provided structured contraceptive counseling, women who did not want to become pregnant appeared significantly more likely to receive EC and to initiate use of more effective contraception. Of note, as women seeking pregnancy testing are often at risk of sexually transmitted infections (STI) which can be prevented by consistent condom use, providing this contraceptive counseling did not reduce condom use among study participants.
Although pregnancy testing is one of the most common services provided by family planning clinics,(9) there has been relatively little discussion of best practices in clinic-based pregnancy testing,(10) which according to Title X guidelines do not require an encounter with a clinical service provider. (11) Much of the prior literature on counseling women who have requested pregnancy testing has focused on how to counsel women who are found to be pregnant.(12) Less attention has been given to those who may remain at high risk of undesired pregnancy. This is unfortunate, as the large majority of women who seek walk-in pregnancy testing do not desire pregnancy and most are told their pregnancy test is negative.(7)
Prior work has found that most adolescents with negative pregnancy tests would welcome one-on-one counseling about contraception.(13) In addition, one previous study reported that reproductive health counseling offered with pregnancy testing provided benefits;(14) however, none of that study's participants used an IUD or subdermal implant. In contrast, the intervention we studied was designed specifically to promote use of these highly effective reversible contraceptives.
Although contraceptive counseling has been shown to be effective in multiple settings, structured contraceptive counseling (even when provided by staff without prior health care experience or clinical training) has been found to be even more effective.(15) Data from the National Survey of Family Growth shows that women who received any contraceptive counseling in the past year were much more likely to use contraception.(16) Additionally, women who report higher levels of contraceptive knowledge after receiving contraceptive counseling are more likely to initiate a new method of contraception. (17) However, for many women, the fragmentation of care which is produced when counseling is followed by referral to another clinic for desired contraceptive placement can be problematic.(18) For this reason, an important aspect of the intervention we studied was the offer of same-day initiation of any desired contraceptive, especially if the woman was interested in an IUD or subdermal implant.
Limitations of this study include the fact that survey data can be subject to both recall and social desirability bias. In addition, although we are not aware of any other local efforts to educate this population of women about IUDs or implants either prior to or during this study period, nationally, use of IUDs has been increasing,(19) and it is possible that the changes observed in this study simply reflect secular trends. Another limitation of this work is that we have no formal measures of how often clinic staff used the counseling script they were asked to use when patients requested pregnancy testing. However, medical record data indicate that responses to the checklist questions were documented for most women who received pregnancy testing during the intervention period. Finally, as a resident training clinic, the study clinic experienced considerable staff turnover during the course of this study which may have also affected the services women received.
In conclusion, this study demonstrates that a short checklist that reminds clinic staff to assess pregnancy intentions and need for EC when women request pregnancy testing and to provide scripted contraceptive counseling about IUDs and implants with the option of same-day placement appears to improve women's contraceptive knowledge and use three months after their clinic visit. Given the option of home pregnancy testing, many women do not come to clinics for pregnancy tests.(20) When women make the effort to seek pregnancy testing from a family planning clinic they deserve the added value that clinic staff can provide with the use of a three-item checklist.
Supplementary Material
Acknowledgments
The ECWIP Study team is grateful to Dr. Matthew Reeves, Dr. Caroline Moreau, and Dr. Candace McClure for serving on our data safety and monitoring committee. We also thank Sara Parisi, MPH, MS, for assistance with analysis of EMR data.
Funding: R01PG000859 (PI Schwarz) from Department of Health and Human Services Office of Population Affairs
Footnotes
Potential Conflicts of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Studies in family planning. 2008;39(1):18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 2.Services UDoHaH. Healthy People 2020 topics and objectives. US Department of helath and Human Services; 2010. [Google Scholar]
- 3.Finer LB, Zolna MR. Shifts in Intended and Unintended Pregnancies in the United States, 2001-2008. American journal of public health. 2013 doi: 10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frost JJ, Darroch JE, Remez L. Improving contraceptive use in the United States. Issues Brief (Alan Guttmacher Inst) 2008;(1):1–8. [PubMed] [Google Scholar]
- 5.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on sexual and reproductive health. 2006;38(2):90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 6.Lee JK, Parisi SM, Baldauf E, Rapkin RB, Updike GM, Schwarz EB. Asking for what she needs? Pregnancy testing or EC? Contraception. 2013;87(6):859–63. doi: 10.1016/j.contraception.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 7.Schwarz EB, Kavanaugh M, Douglas E, Dubowitz T, Creinin MD. Interest in intrauterine contraception among seekers of emergency contraception and pregnancy testing. Obstet Gynecol. 2009;113(4):833–9. doi: 10.1097/AOG.0b013e31819c856c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwarz EB, Papic M, Parisi SM, Baldauf E, Rapkin R, U G. Routine counseling about intrauterine contraception for women seeking emergency contraception. Contraception. 2014 doi: 10.1016/j.contraception.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Baker S, Barr M, B M. Family PACT Preliminary Program Report FY 2012-2013. 2013 [MArch 19, 2014]. 6]. Available from: http://bixbycenter.ucsf.edu/publications/files/FamPACTPreAR1213_508.pdf.
- 10.CDC. Providing Quality Family Planning Services. MMWR Recommendations and Reports. 2014;63(4) [PubMed] [Google Scholar]
- 11.Fowler CI, Gable J, Wang J, M E. Family Planning Annual Report: 2012 National Summary Research Triangle Park, NC RTI International. 2013 [March 19, 2014]. Available from: http://www.hhs.gov/opa/pdfs/fpar-national-summary-2012.pdf.
- 12.Stephenson JN. Pregnancy testing and counseling. Pediatr Clin North Am. 1989;36(3):681–96. doi: 10.1016/s0031-3955(16)36691-3. [DOI] [PubMed] [Google Scholar]
- 13.Drebitko CN, Sadler LS, Leventhal JM, Daley AM, Reynolds H. Adolescent girls with negative pregnancy tests. J Pediatr Adolesc Gynecol. 2005;18(4):261–7. doi: 10.1016/j.jpag.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Boise R, Petersen R, Curtis KM, Aalborg A, Yoshida CK, Cabral R, et al. Reproductive health counseling at pregnancy testing: a pilot study. Contraception. 2003;68(5):377–83. doi: 10.1016/j.contraception.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88(2):243–9. doi: 10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Upson K, Reed SD, Prager SW, Schiff MA. Factors associated with contraceptive nonuse among US women ages 35-44 years at risk of unwanted pregnancy. Contraception. 2010;81(5):427–34. doi: 10.1016/j.contraception.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 17.Harper CC, Brown BA, Foster-Rosales A, Raine TR. Hormonal contraceptive method choice among young, low-income women: How important is the provider? Patient Educ Couns. 2010 doi: 10.1016/j.pec.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dehlendorf C, Tharayil M, Anderson N, Gbenedio K, Wittman A, Steinauer J. Counseling About IUDs: A Mixed-Methods Analysis. Perspect Sex Reprod Health. 2014 doi: 10.1363/46e0814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007-2009. Fertil Steril. 2012;98(4):893–7. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baraitser P, Brown KC, Gleisner Z, Pearce V, Kumar U, Brady M. ‘Do it yourself’ sexual health care: the user experience. Sex Health. 2011;8(1):23–9. doi: 10.1071/SH10029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.