Abstract
Purpose:
This study aimed to assess the prevalence of oral lesions among children with autism in Sana’a City, Yemen, and to evaluate their dental status.
Patients and Methods:
This case–control study included 42 children with autism, aged between 5 and 16 years, and 84 age- and gender-matched healthy children as controls. Oral lesions were assessed based on standardized criteria according to the World Health Organization (WHO) recommendations. Dental caries, gingival health, and oral hygiene status were assessed using dmft/DMFT index, Gingival Index (GI), and Plaque Index (PI), respectively. Chi-square test and Mann–Whitney's test were used to compare the groups.
Results:
Compared to controls, children with autism revealed higher proportion of fistulae (9.5% vs. 2.4%), ulcerative lesions (7.1% vs. 1.2%), gingival hyperplasia (4.8% vs. 0.0%), and cheilitis (4.8% vs. 2.4%); however, the differences were not statistically significant. The mean dmft score was significantly higher in children with autism than in controls (5.23 vs. 4.06; P < 0.001). Moreover, children with autism revealed poorer oral hygiene than controls, and the majority had gingivitis.
Conclusions:
Children with autism in Yemen have high prevalence of oral soft tissue lesions, caries, and gingivitis. Therefore, proper oral health education programs should be initiated and directed toward this special section of the society.
Keywords: Autism, dental caries, oral health, Yemen
INTRODUCTION
Autism is a neurodevelopmental condition characterized by impairment in social interaction, impaired communication, and restricted, repetitive, or stereotyped behaviors.[1] The prevalence of autism is estimated to be 1–2 per 1000, with about four times as many males as females.[2,3] Although the etiology of autism is still unknown, the common risk factors proposed include post-encephalitic infection and genetic and autoimmune factors. Family income, education, and lifestyle do not seem to affect the risk of autism.[4]
The oral health condition of disabled children may be influenced by age, severity of impairment, and living conditions. Individuals with special needs may have great limitations in oral hygiene performance due to their potential motor, sensory, and intellectual disabilities.[5,6,7,8] Children with autism have problems with language, behavior, and social skills. Such conditions may make the affected children more prone to oral diseases and complicate their dental care.[8] These children also commonly have damaging oral habits such as bruxism, tongue thrusting, picking at the gingiva, and lip biting.[8,9] Several studies have reported a higher prevalence of caries, gingivitis, and poorer oral hygiene in comparison with non-autistic individuals,[3,10,11,12,13,14] while others reported no differences in oral health status between autistics and controls;[9] in some cases, the prevalence of caries in children with autism may even be comparatively lower.[15,16] Furthermore, earlier reports on this group of individuals in our environment show that they have high unmet needs, especially periodontal treatment needs.[3,10,11,12,13,14]
To date, there has been no data available on the oral health status of children with autism in Yemen. Such information would enable dental professionals to plan and provide appropriate preventive protocol as well as effective treatment for these patients. Hence, the present study was planned and conducted to assess oral lesions and dental health status of children with autism in Sana’a city, Yemen, as compared to healthy controls.
PATIENTS AND METHODS
This case–control study was carried out over 3 months between September and November 2013 in Sana’a City, Yemen. A total of 124 children were included in the study (42 with autism and 84 healthy controls). Children with autism were recruited from Al-Yemen special center for rehabilitation and education of children with autism in Sana’a (the only available center in the city). Of the total 75 individuals in this center, only 42 met the study inclusion criteria. The inclusion criteria were defined before sample screening and consisted of the following: A diagnosis of autism, the understanding of at least very simple instructions and enough cooperation, and obtaining written informed consent from the parents of children for their participation in the study. Age- and gender-matched healthy controls were selected randomly from two public schools in the same neighborhood. Children with any other systemic disease known to cause dental problems and extremely uncooperative children were excluded from the study.
The study was approved by the Research and Ethics Committee, Faculty of Medicine and Health Sciences, Sana’a University, Yemen, and informed consents were obtained from relevant authorities and the participants’ parents.
Demographic information such as age and gender were obtained for each subject prior to examination. The principal examiner (Al-Maweri, SA) was trained and calibrated before the start of the study. Clinical examination was conducted for both groups in the respective schools using electrical overhead light, mouth mirror, tweezers, dental explorer, gauze, and wooden tongue depressor. Oral lesions were evaluated using standard international diagnostic criteria. Dental status was evaluated using DMFT/dmft index according to the World Health Organization oral health surveys.[17] Met Need Index (MNI), an indication of treatment received by an individual, is determined using the ratio of mean missing (M) plus filled (F) teeth to mean decayed, missing, and filled teeth (DMF) [i.e. (M + F)/DMF]. Restorative Index (RI), which reflects the restorative care of those who have suffered the disease, is measured by the ratio of filled (F) to filled plus decayed teeth (F + D) percent [i.e. F/(F + D) percent] as described by Jackson.[18] Gingival health status was assessed using the Gingival Index (GI) of Loe and Silness,[19] while the Plaque Index (PI) of Sillness and Loe[20] was employed to ascertain the oral hygiene status.
The clinical findings were communicated to the parents/guardians and written referrals were given to dental clinics whenever it was necessary.
SPSS (SPSS Inc., Chicago, IL, USA) version 19.00 was used for data entry and analyses. Qualitative data were presented as frequencies and percentages, and the outcomes were analyzed by Chi-square or Fisher's exact tests. The quantitative data were presented as means and standard deviations; these outcomes were checked for normal distribution using Kolmogorov–Smirnov test. As these variables were not normally distributed, they were analyzed using the non-parametric Mann–Whitney's test. A P < 0.05 was considered to be statistically significant.
RESULTS
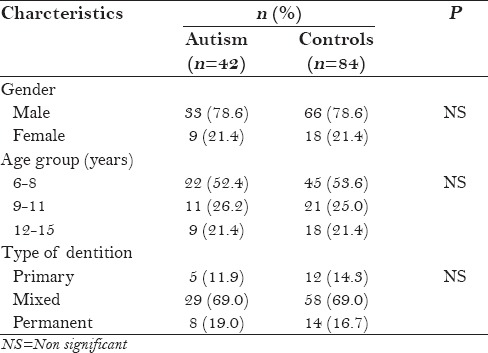
Majority of the children with autism were males (78.6%), with a male to female ratio of 3.7:1. Males dominated the controls also. The mean ages of the cases and controls were 8.45 and 8.6 years, respectively. More than half of children in both groups (52.4% of cases and 53.6% of controls) were in the 6–8 year age group. The demographic characteristics of both groups are presented in Table 1.
Table 1.
Demographic profile of the study subjects
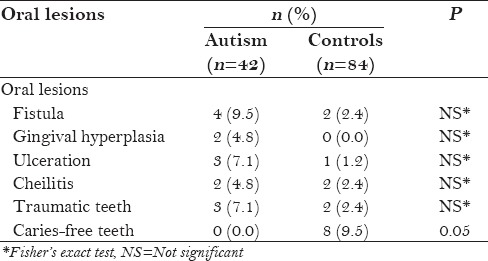
Four types of oral soft tissue lesions were identified among the study subjects. Compared to controls, children with autism revealed higher proportion of oral soft tissue lesions; however, these differences were not statistically significant (P > 0.05) [Table 2]. Also, although not significant, children with autism showed a higher proportion of traumatic teeth than the control group. The prevalence of dental caries was higher among children with autism compared with the control group (100% vs. 90.5%; P = 0.05) [Table 2].
Table 2.
Proportion of oral lesions, traumatic teeth, and caries-free teeth of both groups
The mean scores of DMFT were 2.00 ± 2.18 and 1.27 ± 1.77 for children with autism and controls, respectively, with no significant difference (P > 0.05). On the other hand, children with autism had significantly higher mean dmft scores (5.23 ± 2.34) compared with controls (4.06 ± 2.98; P < 0.001). A major fraction of caries experience in both groups is attributed to decayed teeth [Table 3].
Table 3.
Mean scores of DMFT and dmft and their components, RI and MNI, in both groups
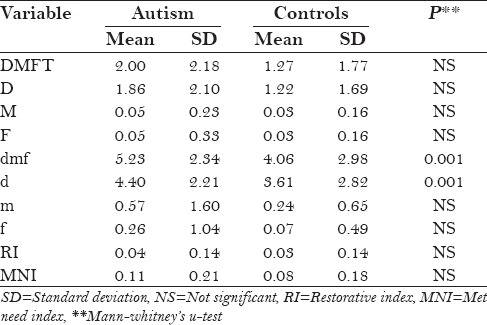
The mean scores of MNI and RI were generally low in both groups, with no significant difference between the two groups [Table 3].
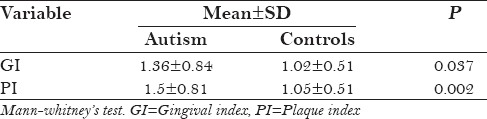
Tables 4 and 5 present the oral hygiene and gingival health status of both groups. Most children in both groups had mild to moderate plaque accumulation. However, children with autism had significantly higher mean PI as compared to controls (P = 0.002). Also, most of the children in both groups showed mild gingivitis; yet, children with autism scored higher mean GI than controls (P = 0.037).
Table 4.
Gingival health and oral hygiene status in both groups
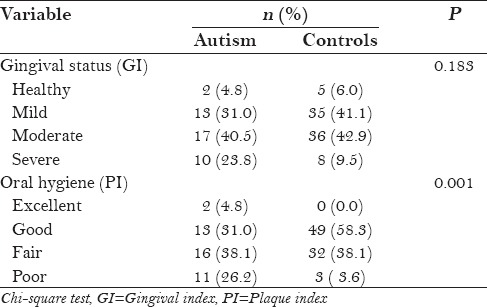
Table 5.
GI and PI in both groups
DISCUSSION
Information of the patterns of development of disease in a population is important because it can act as a database for the planning of public oral health policies.[3] Hence, this study was carried out to provide information on the oral health status of children with autism in Sana’a, Yemen.
The main limitation of the present study is the relatively small number of participants involved. Because of the limited number of special schools for autistic individuals in Sana’a, it was difficult to obtain a representative sample of these individuals. Therefore, generalization must be made carefully, as this study population may not reflect the autistic population in Yemen. Another limitation of the study is the fact that no data on the dietary habits and socio-economic status of the children were available (due to some cultural restrictions). Such data could have objectively explained the results and might have revealed some correlation between the study findings and the socio-demographic characteristics of the subjects. Nonetheless, despite these limitations, we believe that this study can provide valuable baseline information on the oral health status of children with autism in Yemen.
In the present study, most of the children with autism were males, with a male to female ratio of 3.7:1, reflecting a higher prevalence of such disorder among males. Previous studies reported similar higher prevalence among males.[3,12,14] Baron-Cohen et al.[21] attributed this to the high level of fetal testosterone which can potentially affect the genes and chromosomes.
Although statistically insignificant, children with autism revealed higher proportion of oral soft tissue lesions as compared to controls. This result is consistent with other studies which reported higher prevalence of oral lesions in these children than controls.[8,9] This high prevalence of oral soft tissue lesions among children with autism could be attributed to their poor oral hygiene, and drooling and xerostomia induced by medications.[8,9] Moreover, this group of people also commonly have damaging oral habits such as bruxism, tongue thrusting, picking at the gingiva, and lip biting, which might account for the high rate of self-inflicted oral lesions.[8,9] Similarly, the prevalence of traumatic teeth was also higher among children with autism as compared to the controls, which is consistent with other studies.[8,10]
None of the autistics was caries-free compared to 9.5% of controls, but there was no statistically significant difference. Previous studies have reported a high prevalence of dental caries in children with autism.[3,11,14] Murshid et al.[22] suggested that children with autism prefer soft and sweetened foods and they tend to pouch food inside the mouth instead of swallowing it, thereby increasing the susceptibility to caries. Furthermore, xerostomic medications such as Methamphetamine,[13] medications in the form of sweet syrup solution, and poor oral hygiene practices cannot be overlooked. On the contrary, some studies have reported a lower caries rate in autistic individuals as compared to healthy controls.[15,16]
The mean dmft was significantly higher in children with autism than in controls. This finding is consistent with many earlier reports.[3,11,14] However, this result differs from that of Nam et al.,[15] who found that children with autism had lower dmft than controls, and from that of DeMattei et al.,[9] who found no differences in dental caries between the autistics and controls. A high caries index among the children with autism in our study could be attributed to their poor oral hygiene and excessive consumption of sweets. The decay component was a major part for both dmft and DMFT indices, indicating a higher percentage of untreated caries and a greater need for dental treatment.
In the present study, the mean scores of MNI and RI were generally low in both groups, indicating poor access to restorative dental care and/or a negligible sign of preventive care. Similar to our results, many studies have reported that children with autism have more unmet dental needs and are difficult to treat.[3,10,12,15,23] This finding could be attributed to the limited access to the dental services for this group of children or to the difficulties in controlling these children. Moreover, parents frequently avoid taking these children for routine or even urgent dental examination because of their fear of dental procedures.
The oral hygiene of the children with autism examined in the present study was rather poor, and the majority of them were found to have gingivitis. The mean PI and GI scores were statistically higher in the children with autism than in the control group, which was in agreement with several previous reports.[3,10,12,13,14,23] This can be explained by the fact that autistic patients cannot brush as effectively as their normal counterparts. In a similar study by Luppanapornlap et al.,[24] they stated that poor hand coordination leads to difficulty in maintaining good oral hygiene in children with autism, thus increasing the incidence of gingival diseases. Another possible explanation for the presence of generalized gingivitis might be the side effects of medications which are used to control the manifestations of autism, such as psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics.[3,25]
CONCLUSION
In conclusion, children with autism in Yemen have shown a high prevalence of caries, gingivitis, and poor oral hygiene. This study suggests that oral health promotion programs should be introduced to special care schools with parental education as an integral component of such programs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Barbaresi WJ, Katusic SK, Voigt RG. Autism: A review of the state of the science for pediatric primary health care clinicians. Arch Pediatr Adolesc Med. 2006;160:1167–75. doi: 10.1001/archpedi.160.11.1167. [DOI] [PubMed] [Google Scholar]
- 2.Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE, et al. The epidemiology of autism spectrum disorders. Annu Rev Public Health. 2007;28:235–58. doi: 10.1146/annurev.publhealth.28.021406.144007. [DOI] [PubMed] [Google Scholar]
- 3.Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. 2011;19:212–7. doi: 10.1590/S1678-77572011000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muhle R, Trentacoste SV, Rapin I. The genetics of autism. Pediatrics. 2004;113:e472–86. doi: 10.1542/peds.113.5.e472. [DOI] [PubMed] [Google Scholar]
- 5.Nunn JH. The dental health of mentally and physically handicapped children: A review of the literature. Community Dent Health. 1987;4:157–68. [PubMed] [Google Scholar]
- 6.Oredugba FA, Akindayomi Y. Oral health status and treatment needs of children and young adults attending a day centre for individuals with special health care needs. BMC Oral Health. 2008;8:30. doi: 10.1186/1472-6831-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orellana LM, Silvestre FJ, Martínez-Sanchis S, Martínez-Mihi V, Bautista D. Oral manifestations in a group of adults with autism spectrum disorder. Med Oral Patol Oral Cir Bucal. 2012;17:e415–9. doi: 10.4317/medoral.17573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Sufyani GA, Al-Maweri SA, Al-Ghashm AA, Al-Soneidar WA. Oral hygiene and gingival health status of children with Down syndrome in Yemen: A cross-sectional study. J Int Soc Prev Community Dent. 2014;4:82–6. doi: 10.4103/2231-0762.139429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeMattei R, Cuvo A, Maurizio S. Oral assessment of children with an autism spectrum disorder. J Dent Hyg. 2007;81:65. [PubMed] [Google Scholar]
- 10.Subramaniam P, Gupta M. Oral health status of autistic children in India. J Clin Pediatr Dent. 2011;36:43–7. doi: 10.17796/jcpd.36.1.l6287842uj536x13. [DOI] [PubMed] [Google Scholar]
- 11.Desai M, Messer LB, Calache H. A study of the dental treatment needs of children with disabilities in Melbourne, Australia. Aust Dent J. 2001;46:41–50. doi: 10.1111/j.1834-7819.2001.tb00273.x. [DOI] [PubMed] [Google Scholar]
- 12.Vajawat M, Deepika PC. Comparative evaluation of oral hygiene practices and oral health status in autistic and normal individuals. J Int Soc Prev Community Dent. 2012;2:58–63. doi: 10.4103/2231-0762.109369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vishnu Rekha C, Arangannal P, Shahed H. Oral health status of children with autistic disorder in Chennai. Eur Arch Paediatr Dent. 2012;13:126–31. doi: 10.1007/BF03262858. [DOI] [PubMed] [Google Scholar]
- 14.Richa, Yashoda R, Puranik MP. Oral health status and parental perception of child oral health related quality-of-life of children with autism in Bangalore, India. J Indian Soc Pedod Prev Dent. 2014;32:135–9. doi: 10.4103/0970-4388.130967. [DOI] [PubMed] [Google Scholar]
- 15.Namal N, Vehit HE, Koksal S. Do autistic children have higher levels of caries? A cross-sectional study in Turkish children. J Indian Soc Pedod Prev Dent. 2007;25:97–102. doi: 10.4103/0970-4388.33457. [DOI] [PubMed] [Google Scholar]
- 16.Loo CY, Graham RM, Hughes CV. The caries experience and behavior of dental patients with autism spectrum disorder. J Am Dent Assoc. 2008;139:1518–24. doi: 10.14219/jada.archive.2008.0078. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. 4th ed. Geneva: World Health Organization; 1997. Oral Health Surveys: Basic Methods. [Google Scholar]
- 18.Jackson D. Measuring restorative dental care in communities. Br Dent J. 1973;134:385–8. doi: 10.1038/sj.bdj.4803007. [DOI] [PubMed] [Google Scholar]
- 19.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 20.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 21.Baron-Cohen S, Lombardo MV, Auyeung B, Ashwin E, Chakrabarti B, Knickmeyer R. Why are autism spectrum conditions more prevalent in males? PLoS Biol. 2011;9:e1001081. doi: 10.1371/journal.pbio.1001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murshid EZ. Diet, oral hygiene practices and dental health in autistic children in Riyadh, Saudi Arabia. Oral Health Dent Manag. 2014;13:91–6. [PubMed] [Google Scholar]
- 23.El Khatib AA, El Tekeya MM, El Tantawi MA, Omar T. Oral health status and behaviours of children with autism spectrum disorder: A case-control study. Int J Paediatr Dent. 2014;24:314–23. doi: 10.1111/ipd.12067. [DOI] [PubMed] [Google Scholar]
- 24.Luppanapornlarp S, Leelataweewud P, Putongkam P, Ketanont S. Periodontal status and orthodontic treatment need of autistic children. World J Orthod. 2010;11:256–61. [PubMed] [Google Scholar]
- 25.Friedlander AH, Yagiela JA, Paterno VI, Mahler ME. The neuropathology, medical management and dental implications of autism. J Am Dent Assoc. 2006;137:1517–27. doi: 10.14219/jada.archive.2006.0086. [DOI] [PubMed] [Google Scholar]


