Abstract
Background
Nasoenteric feeding tubes may easily become dislodged due to patient mental status, transfers, or positional changes. Nasal bridles were introduced to provide a better, more reliable system to secure these tubes. This meta-analysis was performed to evaluate the effectiveness of nasal bridles compared with the traditional method of adhesive tape alone in securing enteral feeding tubes.
Materials and Methods
Multiple databases were searched (October 2013). All studies that evaluated the use of nasal bridles in adult patients were included in the analysis. Meta-analysis for the outcomes from use of a nasal bridle vs the more traditional method of adhesive tape alone for securing nasoenteric tubes was analyzed by calculating pooled estimates of dislodgement, skin complications, and sinusitis. Statistical analysis was performed using RevMan 5.1.
Results
Six studies (n = 594) met the inclusion criteria. Use of a nasal bridle for securing enteral tubes resulted in a statistically significant reduction in tube dislodgement compared with traditional adhesive tape alone (odds ratio [OR], 0.16; 95% confidence interval [CI], 0.10–0.27; P < .01). The use of nasal bridles was associated with a higher rate of skin complications compared with traditional adhesive tape (OR, 4.27; 95% CI, 1.79–10.23; P < .01). Incidence of sinusitis was no different between the 2 groups (OR, 0.26; 95% CI, 0.03–2.28; P = .22).
Conclusion
Nasal bridles appear to be more effective at securing nasoenteric tubes and preventing dislodgement than traditional use of tape alone.
Keywords: enteral nutrition, feeding tubes, nasal bridles, nasogastric, nasojejunal
Nutrition plays an integral part in the care of all patients, especially those who are critically ill or severely malnourished.1 In patients unable to maintain adequate volitional intake, enteral access achieved through a variety of techniques becomes essential. For short-term nutrition supplementation, nasoenteric tubes (such as nasogastric, nasoduodenal, and nasojejunal) are used. These enteral access devices are readily used but may be difficult to keep in the proper position. Regardless of the location of the tube tip or level of infusion within the gastrointestinal tract, securing the nasoenteric tube is important. Tube dislodgement may lead to delays in enteral nutrition (EN), increased risk for aspiration or malposition of the tube at the time of replacement, and added cost (time spent replacing tubes, the new feeding tube itself, radiographic confirmation studies).
Traditionally, nasoenteric tubes have been kept in place by taping the tube to the face, nose, and forehead of the patient. Such practice, however, may be relatively ineffective, with a displacement rate as high as 62%.2,3 The adhesive tape itself may cause discomfort to the patient or nasal necrosis, lead to skin tears, cause cutaneous sensitivity reactions to the tape, or may interfere with endotracheal tubes, facial wounds, or other monitoring devices.
In 1980, Armstrong et al4 described a technique for securing nasoenteral feeding tubes by using a nasal bridle, whereby some type of anchor (extra feeding tube, umbilical tape, or red rubber tube) is placed around the vomer bone or nasal septum. The bridle is placed by a variety of methods, including via nares or mouth, with the end result being an anchor through 1 naris, around the nasal septum, and exiting the other naris. Both ends of the bridle are secured together to the nasoenteric tube near the nares. The advantage of the nasal bridle is that no taping is required. Anecdotally, the patients who are able to voice concerns do not seem to complain of increased discomfort with the bridle. With no tape on the nose, forehead, or cheeks, the nasal bridle is less likely to interfere with wounds, burns, orotracheal tubes, or oral airway devices.5–9
Many different types of anchors have been used with varying degrees of success.2,10–21 In 2009, Gunn et al18 described a new technique for a nasal bridle using a commercial magnetic retrieval system attached to 1/8-inch umbilical tape to place and secure the nasoenteric tube (Applied Medical Technology, Brecksville, OH). Given a limited number of small studies and a variety of techniques described,2,3,18–21 this meta-analysis was performed to examine the overall effectiveness of nasal bridles vs the traditional alternative of no bridle, using tape alone for securing nasoenteric tubes.
Materials and Methods
Literature Search
A comprehensive literature search was performed from multiple databases using a 3-point system. First, multiple databases were searched, including PubMed/Medline, EMBASE, CINAHL, Scopus, and Cochrane Databases in October 2013. Second, abstracts from major conferences (Digestive Disease Week and American College of Gastroenterology national meetings from 2005–present and Clinical Nutrition Week national meeting from 2010–present) were searched. Third, references of the retrieved articles and reviews were manually searched for any additional articles. If data were incomplete, missing, or required clarification, authors were contacted and clarifications were made.
Data Extraction
All studies on adult patients that compared nasal bridle with traditional adhesive tape were included in the analysis. Two reviewers (M.L.B. and D.L.N.) independently assessed the trials and extracted the appropriate data to be included in the analysis. Any disagreements were evaluated and settled by consensus or a third party (L.B.P.).
Study Quality Assessment
The quality of studies was assessed using the Effective Public Health Practice Project model.22,23 This scale assesses study quality as strong, moderate, or weak based on criteria ratings for selection bias, study design, confounders, blinding, data collection methods, withdrawal and dropout descriptions, intervention integrity, and analysis. The quality of the study is based on the number of weak ratings identified per category (≥2 weak ratings = weak, 1 weak rating = moderate, and no weak ratings = strong).22,23
Statistical Analysis
Meta-analysis for the effect of nasal bridles vs traditional adhesive tape in adult patients with nasoenteric tubes was analyzed by calculating pooled estimates of the primary outcome (dislodgement) and secondary outcomes (skin complications and sinusitis). Skin complications consisted of a spectrum from skin erythema to ulceration. A subgroup analysis was performed in a similar fashion for those studies in which the bridle system involved used umbilical tape (instead of tubing). The results were reported using the odds ratio (OR) with a Mantel-Haenszel (fixed effects) model. Heterogeneity was analyzed by calculating the I2 measure of inconsistency and was considered significant if P < .10 or I2 > 50%. If heterogeneity was statistically significant, a sensitivity analysis was used to examine for heterogeneity when certain studies were excluded from the analysis. Statistical analysis was performed using RevMan 5.1 (ReviewManager [computer program], version 5.1, The Nordic Cochrane Centre, Copenhagen, Denmark). Publication bias was assessed by funnel plots.
Results
Article Search and Identification
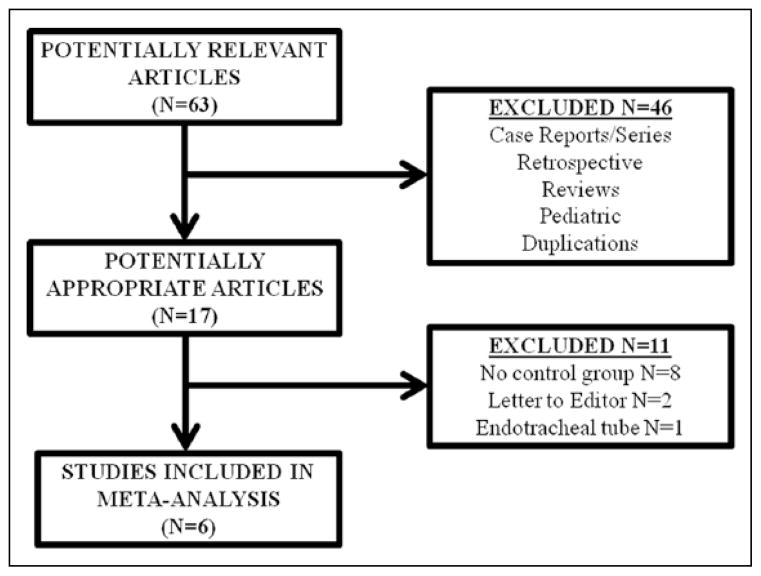
Sixty-three articles were identified upon initial search (Figure 1). Upon review of titles and abstracts, 46 articles and abstracts were excluded due to not meeting the inclusion criteria for this meta-analysis. Of the remaining 17 articles and abstracts, 6 studies (n = 594) met the inclusion criteria for this meta-analysis (Figure 1).2,3,18–21 These studies ranged in date from 1999–2013 and were reported by institutions at varying locations across the Midwest United States.2,3,18–21 The mean age of patients in these studies ranged from 48–66 years. The nasoenteric tubes ranged from 8–16 French in reporting studies. The details of these trials included in the meta-analysis are shown in Table 1. One study2 was deemed to be of strong methodologic quality, while the other 5 studies were designated as moderate quality.3,18–21 The details on quality assessment of included trials are summarized in Table 2.
Figure 1.
Article search algorithm in October 2013.
Table 1.
Details Described on the Studies Included in Meta-Analysis.
| Study | Institution | Data Collection Dates | Population | Bridle Material |
|---|---|---|---|---|
| Brandt and Mittendorf21 | Case Western Reserve University | May 1995–May 1997 | 66 | Excess tube |
| Gunn et al18 | University of Pittsburgh | May 2007–August 2007 | 90 | Red rubber catheter or umbilical tape |
| Seder et al19 | William Beaumont Hospital | November 2006–February 2007 | 234 | Umbilical tape |
| Seder et al2 | William Beaumont Hospital | January 2008–July 2008 | 80 | Umbilical tape |
| Parks et al20 | University of Kansas | NS | 50 | Umbilical tape |
| Hegazi et al3,a | University of Pittsburgh | January 2006–June 2007 | 74 | Umbilical tape |
NS, not specified.
Abstract publication.
Table 2.
Quality Assessment of the Studies Based on the Effective Public Health Practice Project Scale.
| Study | Study Design | Selection Bias | Confounders | Blinding | Data Collection Methods | Withdrawals and Dropouts | Intervention Integrity | Analyses | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Brandt and Mittendorf21 | Prospective cohort | Limited | Moderate | None | Strong | None | Strong | Strong | Moderate |
| Gunn et al18 | Prospective cohort | Limited | Moderate | None | Strong | None | Strong | Strong | Moderate |
| Seder et al19 | Prospective cohort | Limited | Limited | None | Strong | None | Strong | Strong | Moderate |
| Seder et al2 | Randomized controlled trial | Limited | Limited | None | Strong | None | Strong | Strong | Strong |
| Parks et al20 | Prospective cohort | Limited | Moderate | None | Moderate | None | Strong | Strong | Moderate |
| Hegazi et al3,a | Prospective cohort | Limited | Moderate | None | Moderate | None | Strong | Strong | Moderate |
Abstract publication.
Dislodgement of Nasoenteric Tube
Dislodgement of the nasoenteric tube was evaluated in 5 studies (n = 544).2,3,18,19,21 Dislodgement of the tube was noted in 40% (138/341) of those patients for whom the tube was secured in the traditional manner by tape alone but only 14% (28/203) of those patients for whom a nasal bridle was used. Thus, use of a nasal bridle in patients with nasoenteric tubes was associated with a statistically significant reduction in tube dislodgement (OR, 0.16; 95% confidence interval [CI], 0.10–0.27; P < .01) compared with the use of traditional adhesive tape (Figure 2). No statistically significant heterogeneity was observed across these studies (I2 = 0%, P = .66).
Figure 2.
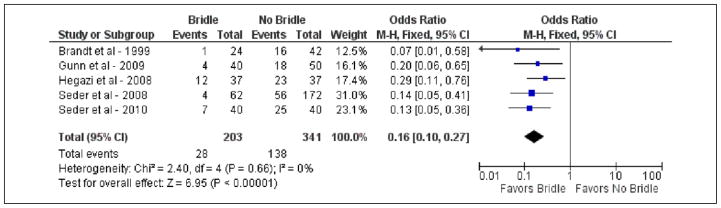
Forest plot demonstrating comparison of nasal bridle vs traditional adhesive tape in securing nasoenteric tubes for tube dislodgement. CI, confidence interval; M–H, Mantel-Haenszel.
Skin Complications
Four studies addressed the presence of skin complications, which ranged from erythema to frank ulcerations (n = 438).2,3,19,20 Skin complications were found in 13% (20/156) of those patients for whom a nasal bridle was placed compared with only 3% (9/282) of patients for whom traditional adhesive tape was used. Thus, use of a nasal bridle demonstrated an increased risk of skin complications (OR, 4.27; 95% CI, 1.79–10.23; P < .01) compared with tape alone (Figure 3). No statistically significant heterogeneity over these 4 trials was observed (I2 = 44%, P = .15). Seder et al19 found that using a red rubber catheter for the bridle resulted in a substantial increase in nasal ulcerations. After switching to 1/8-inch umbilical tape in the study, no further ulcerations were noted. However, even after excluding those patients for whom a red rubber tube was used, the correlation between use of a bridle and skin complications for all the studies remained statistically significant (OR, 3.19; 95% CI, 1.23–8.25, P = .02; I2 = 36%, P = .21).
Figure 3.
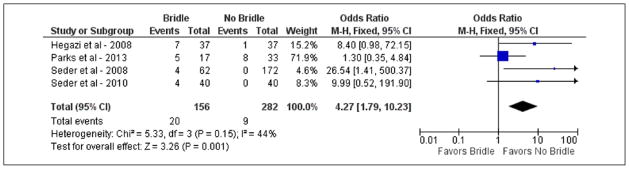
Forest plot demonstrating comparison of nasal bridle vs traditional adhesive tape in securing nasoenteric tubes for skin complications. CI, confidence interval; M–H, Mantel-Haenszel.
Sinusitis
Two studies examined both groups for the presence of sinusitis (n = 130).2,20 Five percent of patients (4/73) for whom adhesive tape was used to secure the tube developed sinusitis, whereas none of 57 patients for whom the nasal bridle was used reported this complication (a difference that did not reach statistical significance) (Figure 4).
Figure 4.
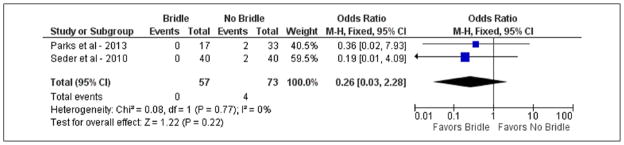
Forest plot demonstrating comparison of nasal bridle vs traditional adhesive tape in securing nasoenteric tubes for sinusitis. CI, confidence interval; M–H, Mantel-Haenszel.
Publication Bias
No publication bias was noted for any of the outcomes in this meta-analysis based on funnel plots.
Discussion
Enteral feeding tubes are the mainstay of delivery for EN in patients with inadequate volitional intake. Although effective, nasoenteric tubes are easily dislodged. Due to this problem, nasal bridles were developed to secure these tubes as an alternative to the traditional method of using adhesive tape alone.2–4,18–21 Since 1980, a variety of techniques and materials have been described for the placement of nasal bridles. In 1999, Brandt and Mittendorf21 found that nasal bridles, which were made from extra feeding tube that was cut into a bridle, decreased tube dislodgement in intensive care unit (ICU) patients with 8- or 10-Fr nasojejunal tubes. They also discovered that the use of a nasal bridle resulted in longer mean duration of tube use (23 vs 16 days; P < .05). Parks et al20 found that the use of a nasal bridle resulted in less mean tube replacements per day (0.26 vs 0.44; P < .05) and episodes of reported sinusitis (0% vs 6%; P < .05) compared with taping alone. In this meta-analysis, the use of nasal bridles to secure nasoenteric tubes resulted in fewer tube dislodgements than traditional use of adhesive tape alone. The incidence of reported sinusitis was not increased in those patients with nasal bridles. However, skin complications, consisting of skin erythema to ulceration, were increased in patients with nasal bridles.
The potential risk for increased skin complications from nasal bridles may be reduced by using bridles only in those patients at high risk for dislodgement and performing proper technique at the time of placement. The umbilical tape used for the bridle has to be tied to the feeding tube around a clipping device. Excessive tension when tying the knot can cause pressure necrosis on the tissue, leading to ulceration. External traction on the tube itself can cause further strain and pressure necrosis on the posterior aspect of the nasal septum, such that the bridle can nearly erode through the entire septum.24 Careful external positioning of the tube and bridle in a tension-free manner should reduce the risk of skin complication. The complication of ulceration is likely increased the longer the tube is present. In addition to patient complications, skin complications are being monitored and reported by national agencies, giving extra incentive to reduce these complications. Earlier consideration of percutaneous or surgical gastrostomy placement in patients likely to require long-term feeding may also help limit these local complications.
As with any meta-analysis, strengths and weaknesses are present. One strength of this report is that it represents a variety of institutions in the United States. All studies were of moderate (most studies) or strong methodologic quality based on the Effective Public Health Practice Project assessment scale,22 with no heterogeneity or publication bias noted for any of the outcomes. However, most of the studies included in this meta-analysis were prospective cohort studies5 with only 1 randomized controlled trial.1 Also, limited data were available regarding secondary outcomes such as the subjective symptom of pain, erosion of the nasal septum, or complications arising from repeated nasoenteric tube placement (epistaxis, aspiration, etc).
According to this meta-analysis, nasal bridles appear to be more effective at securing nasoenteric tubes than use of traditional adhesive tape alone. While care and proper technique must be taken with bridles to avoid skin irritation, breakdown, and ulceration, such risk may be reduced by using umbilical tape, limiting pressure while tying the knot, and removing once clinically indicated. Use of a bridle may be considered following placement of a nasoenteric tube in patients at high risk for tube dislodgement as an effective strategy for access securement.
Footnotes
Financial disclosure: None declared.
References
- 1.McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) JPEN J Parenter Enteral Nutr. 2009;33:277–316. doi: 10.1177/0148607109335234. [DOI] [PubMed] [Google Scholar]
- 2.Seder CW, Stockdale W, Hale L, Janczyk RJ. Nasal bridling decreases feeding tube dislodgment and may increase caloric intake in the surgical intensive care unit: a randomized, controlled trial. Crit Care Med. 2010;38:797–801. doi: 10.1097/CCM.0b013e3181c311f8. [DOI] [PubMed] [Google Scholar]
- 3.Hegazi R, Rolniak S, Centa P, et al. Effects of a nasal tube retention device (AMT bridle) on frequency of nasojejunal feeding tube displacement [abstract] Nutr Clin Pract. 2008;23:223. [Google Scholar]
- 4.Armstrong C, Luther W, Sykes T. A technique for preventing extubation of feeding tubes: “the bridle” [abstract] JPEN J Parenter Enteral Nutr. 1980;3:603. [Google Scholar]
- 5.Meer JA. New nasal bridle for securing nasoenteral feeding tubes. JPEN J Parenter Enteral Nutr. 1989;13:331–334. doi: 10.1177/0148607189013003331. [DOI] [PubMed] [Google Scholar]
- 6.Barrocas A, Jastram C, St Romain C. The bridle: increasing the use of nasoenteric feedings. Nutr Support Serv. 1982;2:8–10. [Google Scholar]
- 7.Levenson R, Dyson A, Turner W. Feeding tube anchor. Nutr Support Serv. 1985;5:40–42. [Google Scholar]
- 8.Popovich MJ, Lockrem JD, Zivot JB. Nasal bridle revisited: an improvement in the technique to prevent unintentional removal of small-bore nasoenteric feeding tubes. Crit Care Med. 1996;24:429–431. doi: 10.1097/00003246-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Popovich MJ. The bridle: path to improved enteral nutrition efficiency. Crit Care Med. 2010;38:984–985. doi: 10.1097/CCM.0b013e3181cc1197. [DOI] [PubMed] [Google Scholar]
- 10.Webb G, Gupta P, Fitchett J, Simmons J, De Silva A. Efficacy of nasal bridles in avoiding percutaneous endoscopic gastrostomy placement. Frontline Gastroenterol. 2012;3(2):109–111. doi: 10.1136/flgastro-2012-100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young A, Leedham L. Nasobridles as a retaining device to provide nutrition support [abstract] Gut. 2011;60:A52. [Google Scholar]
- 12.Gupta PK, Fitchett J, Simmons J, De Silva AN. Efficacy of nasal bridles in preventing nasogastric tube displacement: the Royal Berkshire experience [abstract] Gastroenterology. 2010;138(5):S234–S235. [Google Scholar]
- 13.Lang AP, Armitage HE, Weekes CE. The safety and effectiveness of nasal bridles as a method of securing nasogastric tubes in stroke and elderly care patients requiring enteral tube feeding [abstract] Cerebrovasc Dis. 2010;29:335. [Google Scholar]
- 14.Power S, Smyth N, Duggan S, Roddy M, Feehan S. The nasal bridle: a useful approach to prevent the dislodgement of feeding tubes. e-SPEN. 2010;5:e73–e76. [Google Scholar]
- 15.Cheung KT, Donaldson E, Earley T, Coulthurst P, Shaw T, Shields PL. Use of nasal bridles to secure nasogastric tubes improves delivery of enteral nutrition in at-risk patients [abstract] Gut. 2009;58:A81. [Google Scholar]
- 16.Bennell JA, Black S, Murray CD, Moore K. The nasal bridle effectively secures nasogastric feeding tubes and avoids unnecessary invasive enteral and parenteral nutrition [abstract] Gut. 2009;58:A81. [Google Scholar]
- 17.Popovich MJ, Lockrem JD, Zivot JB. Nasal bridle revisited: an improvement in the technique to prevent unintentional removal of small-bore nasoenteric feeding tubes. Crit Care Med. 1996;24:429–431. doi: 10.1097/00003246-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Gunn SR, Early BJ, Zenati MS, Ochoa JB. Use of a nasal bridle prevents accidental nasoenteral feeding tube removal. JPEN J Parenter Enteral Nutr. 2009;33:50–54. doi: 10.1177/0148607108321704. [DOI] [PubMed] [Google Scholar]
- 19.Seder CW, Janczyk R. The routine bridling of nasojejunal tubes is a safe and effective method of reducing dislodgement in the intensive care unit. Nutr Clin Pract. 2008;23:651–654. doi: 10.1177/0884533608326139. [DOI] [PubMed] [Google Scholar]
- 20.Parks J, Klaus S, Staggs V, Pena M. Outcomes of nasal bridling to secure enteral tubes in burn patients. Am J Crit Care. 2013;22:136–142. doi: 10.4037/ajcc2013105. [DOI] [PubMed] [Google Scholar]
- 21.Brandt CP, Mittendorf EA. Endoscopic placement of nasojejunal feeding tubes in ICU patients. Surg Endosc. 1999;13:1211–1214. doi: 10.1007/pl00009623. [DOI] [PubMed] [Google Scholar]
- 22.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1:176–184. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 23.Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract. 2012;18:12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 24.McClave SA, Chang WK. Complications of enteral access. Gastrointest Endosc. 2003;58:739–751. doi: 10.1016/s0016-5107(03)02147-3. [DOI] [PubMed] [Google Scholar]