Abstract
Backgrounds/Aims
Aging of population is leading to more operative treatments on elderly patients in various aspects. Growing numbers of patients are going through operations about cholecystitis in the same sense. We tried to survey them anew about remarkably increasing octogenarian patients and the outcome after operative management for cholecystitis seeking to improve treatment result.
Methods
For 5 years, from March 2007 to Febraury 2012, 57 octogenarian patients had cholecystectomy among total 380 cases. Patients were compared between total patients and octogenarians on perioperative follow-up findings in medical records.
Results
Underlying diseases were prevailing in octogenarian by more than 70% of cases. Severe acute cholecystitis was more often observed in octogenarians and procedures like endoscopic retrograde cholangiopancreaticography were more often performed preoperatively, showing more frequent conversion to open method from laparoscopic procedure. Complications such as peritonitis, sepsis, wound problem, including mortality were much more common in octogenarian cholecystectomy patients. When compared to total cholecystectomy patient group, octogenarian patients had more problems in every items significantly (p<0.05).
Conclusions
High rates of complications and mortality accompanying prolonged symptoms and examinations was inevitable for octogenarian patients after cholecystectomy. Operative treatment per se appears to be inevitable, thus it should make the patients be informed about risks with more attention to every aspect of care.
Keywords: Octogenarian, Cholecystitis, Cholecystectomy
INTRODUCTION
Octogenarians are the merging top topic in medical care by prolonging life expectancy and studies on geriatric patients are progressing nowadays as a specified field answering to increasing need for more scrupulous care of them.
Patients over age of eighty years were felt remarkably heavier in numbers while cholecystectomy was carried out recently, due to expanded life expectancy and followed increasing onset of cholecystitis from the silent gallbladder stones in elderly people.
We chose increasing octogenarian patients as our survey target, and reviewed their steeply elevated risks throughout the operative management, to seek out the chance to gather more attention in searching for improved care along their specified situation.
METHODS
Cholecystectomy patients from March 2007 to February 2012 were serially reviewed on its perioperative and postoperative clinical recordings of total 380 patients, and compared with 57 patients of octogenarians among them, and patients under age of eighty years also were separately described on table for reference during comparison.
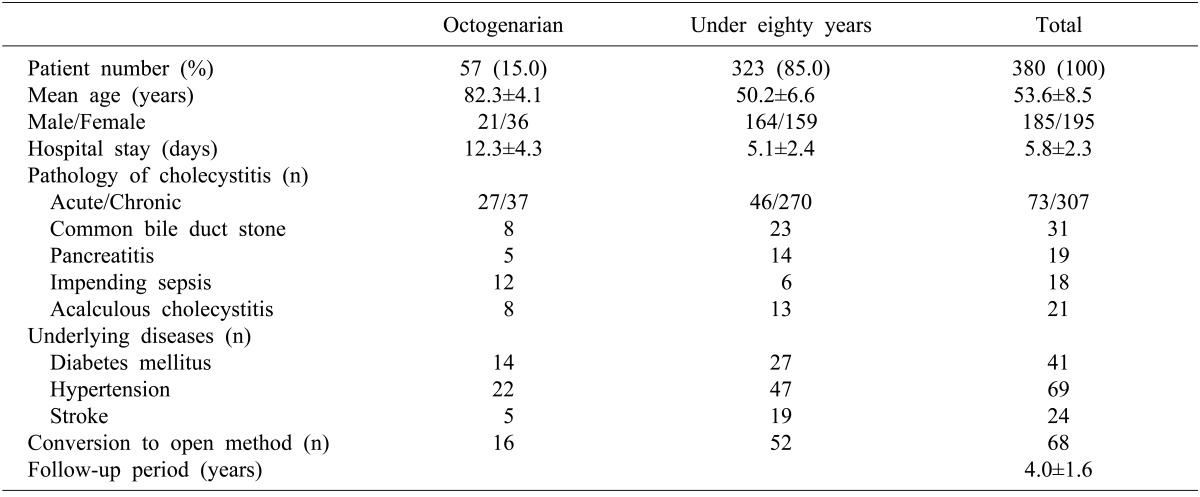
Baseline demography of the patients was illustrated in Table 1. Pathologic features of cholecystitis were reviewed through combined surgical pathology and clinical operative findings together. Associated common bile duct stone (CBD) stones, most of them were removed by endoscopic retrograde cholangiopancreaticography (ERCP) before laparoscopic or open cholecystectomy. Underlying health problems were also reviewed from medical records.
Table 1.
Demography of total patients who underwent cholecystectomy
Underlying diseases were evaluated and described only for the most common three conditions such as diabetes, hypertension, and stroke. Underlying diseases from long-term steroid medication, smoking, Parkinsonism, osteoporoses and so on were excluded from study either for its relative small numbers in significance and for simplification of comparison.
Cholecystitis patients having operative management during the same hospitalization period were selected into study for even comparison. Preoperatively serious septic patient were ruled out from study considering varying chances of complication rates.
Laparoscopic cholecystectomy was routinely tried initially, but severe cholecystitis findings on preoperative imaging study or impending septic patients clinically with relevant laboratory data were operated by open method through right paramedian incision as conversion to open method (Table 1).
Under equal variance of 3 variables, data were compared about its significance on one-way ANOVA tests, and comparisons between two variables were executed using chi-square tests. Ordinal variables were compared using student t-test with confidence interval of 95%. A value <0.05 was considered to be statistically significant.
RESULTS
Patient population was composed of total 380 cholecystectomy cases during 5-years period from March 2007 to February 2012. Among them, 57 patients (15.0%) were eighty years or older ranging from 80 to 93 (82.3±4.1 years), while mean age of total patients were 53.6±8.5 years.
Female predominance was observed in octogenarian patients showing 63.16% (36/57) of cases, but female proportion in total patient was 48.7% (185/380) (p=0.038).
Octogenarian patient stayed in hospital much longer for 12.3 days than 5.8 days of total patients (p<0.001).
Pathologically and clinically, octogenarian patients presented acute cholecystitis symptoms more often in 47.4% (27/57), than in total patients of 23.8% (73/380), respectively (p<0.001).
Associated CBD stones, which were mostly managed by preoperative ERCP, were more common in 14.0% (8/57) of octogenarian patients, and 8.2% (31/380) of total patients had CBD stones (p=0.032).
Cholangitis (8/57) or pancreatitis (19/380) by migrating gallstone into CBD is more often associated in octogenarian meaningfully than in total patients.
Underlying diseases like diabetes, hypertension and stroke were prevailing among elderly patient, but more prominent in numbers in octogenarian patients at 71.9% (41/57) than in 35.3% (134/380) of total patients (p<0.001).
As can be expected from relatively many acute cholecystitis cases in octogenarian patient, conversion to open procedure was unavoidable in 28.1% (16/57), while totally in 17.9% (68/380) (p=0.025).
Operative morbidity and mortality after cholecystectomy was described in Table 2.
Table 2.
Morbidity and mortality profiles of cholecystectomy patients
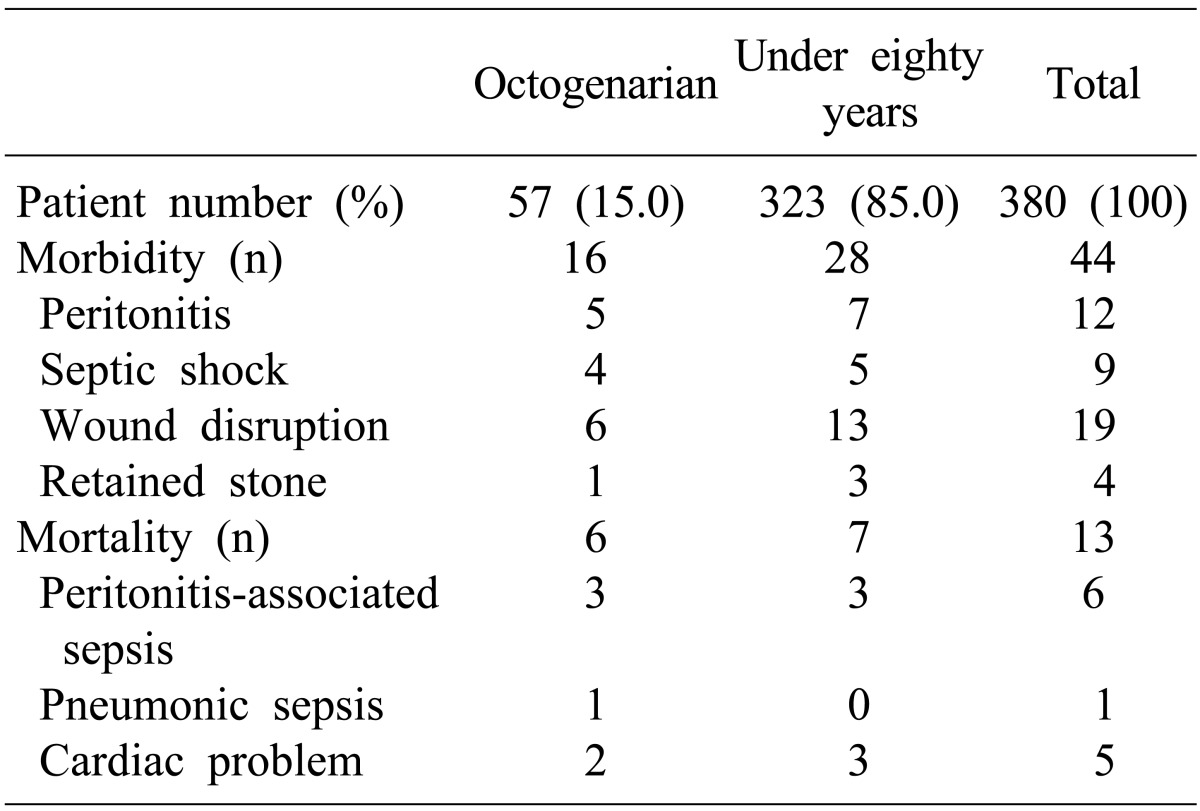
Postoperative morbidities such as peritonitis (n=5), septic shock (n=4), wound disruption (n=6), and retained stone requiring reoperation (n=1) were representing complication rate of 28.1% (16/57) in octogenarian patients, and 11.6% (44/380) of complication arose from total patients (p<0.001).
Mortality was 10.5% (6/57) and 3.4% (13/380) respectively, from octogenarian and total patients (p<0.001).
DISCUSSION
Octogenarians, as the extremely old-aged population, surgical management on them has become a merging issue as census is aging especially from advanced countries. Naturally the most common surgical indication like cholecystitis is growing in patient numbers.
More frequent occurrence of acute cholecystitis in 47.4% of octogenarian cholecystitis patient than in 23.9% of total patients in our study can be interpreted as acute complications of gallstone, toward acute inflammation or to cholangitis or pancreatitis by migration of stone into CBD as times go by, in the shape of complicated gallstone disease rather than simple chronic cholecystitis.
Increasing necessity of emergent care about acutely complicated gallstone in old ages might be as natural like extreme age approaches spontaneously, but another guessing is that gallstones are conservatively managed in octogenarians, while younger patients are definitely treated even during chronic intervening form of cholecystitis before serious complication attack. What then will be safer between conservative care and operative management on octogenarians during chronic cholecystitis state? It is a matter to be followed up on large scale. But, we have opinion of aggressive operative management be given before complications come or before age come to octogenarian especially to the patients with underlying disease in an effort to enhance surgical results.
We found high morbidity rate of 28.1% and mortality of 10.5 from our 57 cases of octogenarian cholecystitis patients after cholecystectomy, but they were comparable or a bit higher to many other publications.1 It does not seem to be a matter of a rate of complications especially when a patient shows symptoms of acute complications. Can there be a high morbidity or mortality overriding efficiency of definite treatment to patients who will almost die without operation? Publications weighing options other than cholecystectomy has been proposed in various forms. Comparison between ERCP and conservative control of cholecystitis with surgical treatment in 80-mean-age-old patients by Targarona et al.2 were conducted, where surgery was supported in consideration of high recurrent symptoms of stones. Siegel and Kasmin3 presented preference of minimally invasive endoscopic decompression of biliary tract. Bergman et al.4 reported that patients were doing well under decreased surgical managements as getting older. Repeated symptomatic attack by gallbladder and gallstones left in position seemed to suggest drawback of options other than operation recently, except as life-saving bridge procedure as Trust et al.5 suggested that recurrence of symptom would return and need for cholecystectomy will also return making patients to suffer from the same disease as long as the stone and gallbladder remains in position.
Brunt et al.6 suggested 43.0% of cholecystitis patients over age of 80 were having synchronous CBD stones. Associated CBD stones causing cholangitis, pancreatitis, impending septic condition are frequently met in octogenarian patients as described above but reduced functional reserve resulting from extreme old age is additionally threatening patients before and after operative management. As being emphasized of highly increased operative risks by Loureiro et al.7, Marcari et al.8 would even named octogenarians extremely old and should be seen as a different group. Tambyraja et al.9 also published high rate of complication of 22.0%, from 24.0% acute form of cholecystitis in octogenarians to put emphasis on serious level of morbidities. Complications and mortality after cholecystectomy rose rapidly, which was observable at the practicing field before survey. Associated underlying disease in octogenarians might lead to that anticipation, as many wound agree on. Reduced functional reserve, and associated underlying diseases, is supposed to be related with high risks of octogenarian cholecystectomy.
High morbidity of 28.1 and mortality of 10.5% in our study was not strictly related to high underlying diseases in 71.9 or with American Society of Anesthesiologists (ASA) score when compared to other publications.1,6,9 Detailed interpretation on underlying disease or follow-up could not be satisfactory first, and comparison to other publications was beyond our scope to be carried out. But 8 cases of acalculous cholecystitis (14.0%), frequently associated with debilitating underlying diseases, and known as an indicator of worse prognoses after operative management, were associated with debilitating disease which we need more attention for better care or prevention in the future.
Opinion insisting no difference of complication or mortality in octogenarian cholecystectomy were also observed, presenting very low published rate of 16.7% complication and 0.0% mortality with low conversion rate of 4.8% by Marcari et al.8 counting severity of cholecystitis than chorological age. Most of publications were contrary to this viewpoint as our study showed high rates of complications.
When 6 patients in preoperatively septic condition requiring cholecystectomy, as a salvaging bridge procedure are included, the number of octogenarian cholecystectomy patient further increases in an incidence to 16.6% (63 of 380), facing more octogenarian patients.
In conclusion, many of cholecystitis patients in octogenarians were complicated than the other patients, and most of them were carrying underlying disease, which leads to higher complication and mortality rates after operative treatment on cholecystitis. Every aspect of medical and surgical problem should be meticulously arranged with further attention in order to improve surgical result by definite treatment of cholecystectomy.
ACKNOWLEDGEMENTS
This paper was partially supported by Wonkwang University research foundation.
References
- 1.Nikfarjam M, Yeo D, Perini M, et al. Outcomes of cholecystectomy for treatment of acute cholecystitis in octogenarians. ANZ J Surg. 2013 doi: 10.1111/ans.12313. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Targarona EM, Ayuso RM, Bordas JM, et al. Randomised trial of endoscopic sphincterotomy with gallbladder left in situ versus open surgery for common bileduct calculi in high-risk patients. Lancet. 1996;347:926–929. doi: 10.1016/s0140-6736(96)91413-0. [DOI] [PubMed] [Google Scholar]
- 3.Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433–435. doi: 10.1136/gut.41.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergman S, Sourial N, Vedel I, et al. Gallstone disease in the elderly: are older patients managed differently? Surg Endosc. 2011;25:55–61. doi: 10.1007/s00464-010-1128-5. [DOI] [PubMed] [Google Scholar]
- 5.Trust MD, Sheffield KM, Boyd CA, et al. Gallstone pancreatitis in older patients: Are we operating enough? Surgery. 2011;150:515–525. doi: 10.1016/j.surg.2011.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brunt LM, Quasebarth MA, Dunnegan DL, et al. Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc. 2001;15:700–705. doi: 10.1007/s004640000388. [DOI] [PubMed] [Google Scholar]
- 7.Loureiro ER, Klein SC, Pavan CC, et al. Laparoscopic cholecystectomy in 960 elderly patients. Rev Col Bras Cir. 2011;38:155–160. doi: 10.1590/s0100-69912011000300003. [DOI] [PubMed] [Google Scholar]
- 8.Marcari RS, Lupinacci RM, Nadal LR, et al. Outcomes of laparoscopic cholecystectomy in octogenarians. JSLS. 2012;16:271–275. doi: 10.4293/108680812X13427982376428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tambyraja AL, Kumar S, Nixon SJ. Outcome of laparoscopic cholecystectomy in patients 80 years and older. World J Surg. 2004;28:745–748. doi: 10.1007/s00268-004-7378-4. [DOI] [PubMed] [Google Scholar]


